Abstract
Background:
Database studies have reported several associations between the diagnosis of idiopathic pulmonary arterial hypertension (IPAH) and mortality attributable to IPAH, including older age, black race, and diabetes.
Methods:
We investigated reported deaths and hospital discharges coded as IPAH and compared these with other forms of pulmonary hypertension. Three databases were used: the US National Center for Health Statistics database (1979-2006), queried for mortality data; the Nationwide Inpatient Sample database (1993-2007), queried for hospital discharge data; and the University of Texas Southwestern Hospital-Zale Lipshy discharge database (1999, 2002).
Results:
Marked increases in mortality attributable to IPAH and to pulmonary hypertension (all codes combined) generally were reported from 1979 until 2002 in the National Center for Health Statistics database. In 2003, reported IPAH mortality fell sharply while total pulmonary hypertension deaths increased. The Nationwide Inpatient Sample database showed a similar pattern of changes beginning approximately 2 years earlier. In both cases, the timing of these observations corresponded with changes made to the International Classification of Diseases (ICD) coding system in use for pulmonary hypertension in that particular database. Review of pulmonary hypertension discharge data from the University of Texas Southwestern Hospital-Zale Lipshy showed similar changes in diagnosis code use.
Conclusions:
Sudden shifts in reported IPAH mortality and hospital discharges were seen in all databases, likely related to coding changes. These findings raise questions about the accuracy of pulmonary hypertension diagnosis codes. Studies based on International Classification of Diseases, Ninth Revision and International Classification of Diseases, 10th Revision codes may have inadvertently included patients with other forms of pulmonary hypertension and should be reevaluated in this context. Validation studies of the IPAH diagnosis code are needed, and changes to the ICD coding system should be considered.
Idiopathic pulmonary arterial hypertension (IPAH) is a progressive, life-threatening condition of unknown cause. Prevalence has been estimated at between five and 25 cases per million population,1 often affecting women aged 20 to 50 years, but all ages and both sexes can be affected. In fact, recent registry studies suggested that the median age at initial diagnosis may be increasing.2 Because certain patient populations are less likely referred to pulmonary hypertension centers, the conclusions drawn from registry studies may or may not be accurate. An alternative approach used in recent years has been to evaluate medical information recorded in large electronic databases. Database studies are promoted as a cost-effective way to study medical conditions in large populations because information typically is extracted from preexisting sources such as death certificates, hospital discharge records, and managed care records.
Pulmonary hypertension diagnoses are recorded in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) as one of four specific diagnosis codes (Table 1).3‐6 Only two codes are commonly used: 416.0, primary pulmonary hypertension (synonymous with IPAH), and 416.8, chronic pulmonary heart disease. The current coding system appears to be using 416.8 for almost all types of pulmonary hypertension except IPAH, even though the medical literature defines the subtypes more distinctively. Some databases, including the National Center for Health Statistics (NCHS) database of US death certificates, have transitioned to the newer International Classification of Diseases, 10th Revision (ICD-10) coding system with similar but not identical descriptors. In this database only, a new code described as “other secondary pulmonary hypertension” was added in 2003.
Table 1.
—ICD-9-CM and ICD-10 PH Codes and Definitions3
| ICD-9-CM | ICD-10 | Current WHO Groups Included | Proposed ICD-10 Code Descriptors |
| 416.0 Primary PH. Idiopathic pulmonary arteriosclerosis. Pulmonary hypertension (essential) (idiopathic) (primary). | I27.0 Primary PH. Pulmonary (artery) hypertension(idiopathic) (primary). | ICD-9-CM and ICD-10: 1.1 Idiopathic PAH and 1.2 Heritable PAH. | Same, although the term “idiopathic pulmonary arterial hypertension” would be optimal. |
| 416.1 Kyphoscoliotic heart disease. | I27.1 Kyphoscoliotic heart disease. | ICD-9-CM and ICD-10: Does not correspond directly to a term in the clinical classification. | Rarely used. |
| … | I27.2 Other secondary PH.a | ICD-10: Unclear. Based on communication with the CDC, appears to include almost all nonidiopathic PH, including PAH, PH associated with left-sided heart failure, and PH with no modifier listed. | “Other pulmonary arterial hypertension.” Include all WHO group 1 PH except IPAH. |
| 416.8 Other chronic pulmonary heart disease. Pulmonary hypertension, secondary.b | I27.8 Other specified pulmonary heart disease. No description. | ICD-9-CM: Because there are no alternative codes for most forms of PH, it appears that the 416.8 code should be used for all forms of PH except IPAH and kyphoscoliotic PH. ICD-10: Unclear. This code would seem to overlap with the I27.2 code. | “Pulmonary hypertension, other specified.” Include WHO group 2-5 PH. The specific associated condition could then be coded using other codes (ie, left-sided heart failure, interstitial lung disease). |
| 416.9 Chronic pulmonary heart disease, unspecified. Chronic cardiopulmonary disease. Cor pulmonale (chronic) NOS. | I27.9 Pulmonary heart disease, unspecified. Chronic cardiopulmonary disease. Cor pulmonale (chronic) NOS. | ICD-9-CM and ICD-10: Any PH where the type is unknown or unspecified. Based on communication with the CDC, includes cor pulmonale if no other modifier is listed. | “Pulmonary hypertension, unspecified.” |
Terminology: chronic pulmonary heart disease and cor pulmonale have both been defined variably, usually as (1) PH related to lung disease or (2) PH from noncardiac causes, ie, all PH except when related to left-sided heart failure or congenital heart disease.5 CDC = Centers for Disease Control and Prevention; ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification; ICD-10 = International Classification of Diseases, Tenth Revision; IPAH = idiopathic pulmonary arterial hypertension; NOS = not otherwise specified; PH = pulmonary hypertension; WHO = World Health Organization.
2003 coding changes: “other secondary pulmonary hypertension” was added to the ICD-10. ICD-9-CM codes were used for US death certificate mortality data up until 1999 and continue to be used for hospital discharges in the United States. ICD-10 codes have been used for death certificates from 1999 to present and are used for hospital data in many other countries.
2001 coding changes: “hypertension, pulmonary” was switched from being indexed to the 416.0 code to being indexed to the 416.8 code in the ICD-9-CM.
Prior database studies describe an increasing number of deaths from IPAH7 and pulmonary hypertension (all codes combined).8 Trends in the use of specific pulmonary hypertension diagnosis codes other than IPAH have not been reported. In this study, we propose an evaluation of each individual pulmonary hypertension diagnosis code. We predicted that reported mortality from pulmonary hypertension in general (all codes combined) would continue to increase due to increases in disease recognition and that IPAH would make up a smaller percentage of the total pulmonary hypertension diagnoses due to increasing familiarity with the disease characteristics and more complete diagnostic evaluations.9
Materials and Methods
US National Center for Health Statistics Database
Mortality data were extracted from the NCHS database on June 3, 2009. This information is reported by the Centers for Disease Control and Prevention using International Statistical Classification of Diseases and Related Health Problems codes and is available at http://wonder.cdc.gov. Reported pulmonary hypertension mortality rates (all diagnosis codes, individually) were obtained by year (1979-2006) and by age group. Data are presented graphically as annual age-adjusted mortality rates using the 2000 US standard population and expressed as deaths per standard million population. Pulmonary hypertension-associated mortality was defined as a pulmonary hypertension diagnosis listed as the primary cause or contributor to immediate death.
From 1979 to 1998, ICD-9-CM codes were in use and included primary (idiopathic) pulmonary hypertension (416.0); kyphoscoliotic heart disease (416.1); other chronic pulmonary heart disease (416.8); and chronic pulmonary heart disease, unspecified (416.9). From 1999 to 2005, four ICD-10 codes also were used, with each code similar to the ICD-9-CM codes (ie, the same number was incorporated after the decimal). In other words, ICD-9-CM 416.0 (IPAH) is defined similarly in ICD-10 as I27.0 (IPAH). Additionally, in 2003, a new ICD-10 diagnosis code, other secondary pulmonary hypertension (I27.2), was added (Table 1).
Nationwide Inpatient Sample Database
Hospital discharge data were extracted from the Nationwide Inpatient Sample (NIS) database via http://hcupnet.ahrq.gov. This database is maintained by the US Department for Health and Human Services and is the largest all-payer database of hospital discharges. It provides a 20% stratified sample of all nonfederal hospitals and includes all patients discharged from member hospitals for the given year. The NIS database is weighted according to a complex scheme that allows for estimation of population parameters. The publicly-accessible databases (NCHS, NIS) were classified by the University of Texas Southwestern Institutional Review Board as institutional review board-exempt. The years 1993 to 2007 were included in this analysis; earlier years were excluded because the number of participating states was more limited, and it would have been difficult to accurately evaluate trends. Data are presented graphically and descriptively, showing the number of all discharges containing any pulmonary hypertension diagnosis code (416.0, 416.1, 416.8, and 416.9) and the percentage of discharges with the IPAH diagnosis code. The age distribution for the 416.0 code also is described.
University of Texas Southwestern Chart Review
Charts for all patients with an ICD-9-CM diagnosis code of pulmonary hypertension (416.0, 416.2, 416.8, and 416.9) in 1999 or in 2002 at the University of Texas Southwestern Hospital-Zale Lipshy (Dallas, Texas) were reviewed. University of Texas Southwestern IRB approval was obtained under IRB approval #052010-039. Zale Lipshy was chosen over the University of Texas Southwestern Hospital-St. Paul location (Dallas, Texas) because Zale does not have inpatient or outpatient congestive heart failure or pulmonary hypertension services or centers; therefore, we believed it better to represent the general use of these ICD-9 codes. The years 1999 and 2002 were chosen on the basis of our observations of the sudden decline in the use of the 416.0 code seen in 2000 and 2001 in the NIS database. Our goal was to understand how the 416.0 code was being used at both time points. A pulmonary hypertension specialist reviewed patient discharge records, and any prior work-up of pulmonary hypertension was noted. The reviewer assigned a probable diagnosis of IPAH if the treating physician believed that the patient had idiopathic (primary) pulmonary hypertension and if there was no evidence of connective tissue disease, congenital heart disease, advanced liver disease, left-sided heart failure, left-sided valvular heart disease, advanced pulmonary disease (interstitial lung disease, COPD, etc), chronic pulmonary emboli, or sarcoidosis. A diagnosis of probable pulmonary hypertension associated with another condition was made if there was evidence of one of these conditions, and IPAH (primary) was not specifically reported in the chart. Finally, if the treating physician specifically used the term “idiopathic” or “primary pulmonary hypertension,” but there was evidence of another condition, or if the more generic term “pulmonary hypertension” was used and the PH evaluation was not complete enough to rule out other conditions, then a diagnosis of possible IPAH was assigned.
Results
NCHS Database: 1979 to 2006
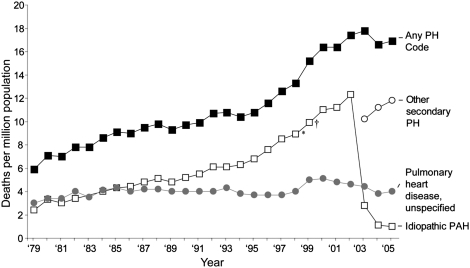
Reported pulmonary hypertension mortality from the NCHS database was evaluated for the years 1979 to 2006, using ICD-9-CM codes for 1979 to 1998 and ICD-10 codes for 1999 to 2006. Mortality rates by year for each pulmonary hypertension diagnosis code are shown graphically for all ages (Fig 1). In contrast to our initial hypothesis, reported deaths attributable primarily to IPAH increased more than other forms of pulmonary hypertension through most of the study period, accounting for 41% of all pulmonary hypertension deaths in 1979 and 71% of all reported pulmonary hypertension deaths in 2002. Beginning in 2003, mortality attributed to IPAH fell sharply, whereas total pulmonary hypertension mortality continued to increase. This decline began at the same time as a new ICD-10 diagnosis code was introduced: other secondary pulmonary hypertension (I27.2) (Table 2). The new code was used frequently, increasing to 73% of all pulmonary hypertension deaths in 2006, whereas IPAH diagnoses fell to 6% of total pulmonary hypertension deaths.
Figure 1.
Mortality from PH (death certificates), 1979 to 2005. The sudden decline in reported idiopathic PAH (IPAH) mortality in 2003 appears to relate to the addition of the new International Classification of Diseases, 10th Revision (ICD-10) code “other secondary PH.” * = updated PH classification system was published in 1988; † = ICD-10 was introduced in 1999; PAH = pulmonary arterial hypertension; PH = pulmonary hypertension.
Table 2.
—PH ICD-9-CM Codes vs Chart Review Diagnoses
| Chart Review |
|||
| Code, Year | No. | Expert-Reviewer Diagnosis | No. |
| ICD-9 code, 1999 | |||
| 416.0 Idiopathic PAH | 30 | IPAH | 2 (probable, 0; possible, 2) |
| Unclear | 3 | ||
| Not IPAH | 25 | ||
| PAH | 9 | ||
| Congenital heart disease | 6 | ||
| Connective tissue disease | 2 | ||
| Cirrhosis | 1 | ||
| Left-sided heart disease | 12 | ||
| Lung disease | 3 | ||
| Chronic pulmonary emboli | 1 | ||
| 416.8 Other chronic pulmonary heart disease | 2 | Not IPAH | 2 |
| Lung disease | 2 | ||
| 416.9 Pulmonary heart disease unspecified | 2 | Not IPAH | 2 |
| Left-sided heart disease | 1 | ||
| Lung disease | 1 | ||
| ICD-9 code, 2002 | |||
| 416.0 Idiopathic PAH | 3 | IPAH | 1 (probable, 0; possible, 1) |
| Not IPAH | 2 | ||
| Lung disease | 1 | ||
| Sarcoid | 1 | ||
| 416.8 Other chronic pulmonary heart disease | 22 | IPAH | 1 (probable, 0; possible, 1) |
| Unclear | 6 | ||
| Not IPAH | 15 | ||
| PAH | 3 | ||
| Congenital heart disease | 3 | ||
| Left heart disease | 5 | ||
| Lung disease | 5 | ||
| Chronic pulmonary emboli | 1 | ||
| Sarcoid | 1 | ||
| 416.9 Pulmonary heart disease unspecified | 2 | Not IPAH | 2 |
| PAH | 1 | ||
| Congenital heart disease | 1 | ||
| Lung disease | 1 | ||
Most patients coded as IPAH were found to have comorbidities, suggesting PH associated with another condition, including left-sided heart disease (n = 12), lung disease (n = 4), and congenital heart disease (n = 6), among others, with the years 1999 and 2002 combined. PAH = pulmonary arterial hypertension. See Table 1 legend for expansion of other abbreviations.
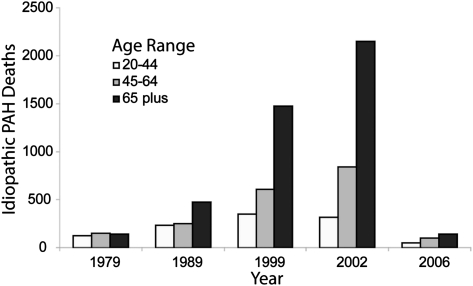
The > 400% increase in reported IPAH mortality between 1979 and 2002 was largely accounted for by an increasing number of deaths among patients aged > 65 years (Fig 2). For example, among patients aged 24 to 35 years, the mortality rate increased 71% over the 23-year period. In contrast, an increase of 947% was seen among patients aged ≥ 65 years, leading to a shift in reported age distribution. In 1979, most (66%) adult patients who died of IPAH were aged < 65 years, and only 3% were ≥ 85 years. In contrast, by 2002, only 35% of adult patients who died of IPAH were aged < 65 years, and 19% were ≥ 85 years. From 2003 to 2006 there was a slight reversal of this increasing age distribution, but patients aged > 65 years continued to account for more than one-half of all reported adult IPAH deaths.
Figure 2.
Mortality rate for IPAH by age group. The greatest increase in IPAH mortality occurred in patients aged > 65 years. See Figure 1 legend for expansion of abbreviation.
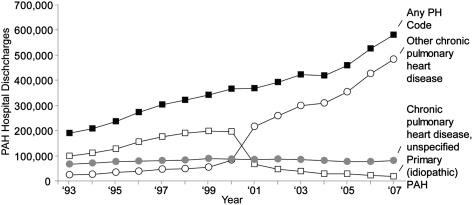
NIS Database: 1993 to 2007
Because of the marked decline in reported IPAH mortality in the NCHS database, we also investigated whether changes were observed in the frequency of reported pulmonary hypertension diagnoses among patients discharged from US hospitals between 1993 and 2007. Similar to the results from the NCHS database, reported pulmonary hypertension discharge diagnoses increased between 1993 and 2000 mainly because of increases in IPAH diagnoses. Then in 2001, 2 years before the decline in reported IPAH mortality in the NCHS database, there was a sharp decline in reported IPAH discharge diagnoses accompanied by a reciprocal increase in other chronic pulmonary heart disease (Fig 3). This was seen without any changes in coding terminology as US hospitals continued to use the ICD-9-CM (rather than ICD-10 codes), and no new codes had been added. There was, however, a change made in the ICD-9-CM index: The reference code in the index for the term “hypertension, pulmonary” was changed from IPAH (416.0) to other chronic pulmonary heart disease (416.8); the main entry for each pulmonary hypertension diagnosis code was not changed.
Figure 3.
Hospital discharges by year, 1993 to 2007. The fall in IPAH diagnoses in 2001 corresponded with a change in the ICD-9-Clinical Modification index in 2001. See Figure 1 legend for expansion of abbreviations.
University of Texas Southwestern Hospital-Zale Lipshy Chart Review
Medical records were reviewed for patients discharged from the University of Texas Southwestern Hospital-Zale Lipshy in either 1999 or 2002 with a reported diagnosis of pulmonary hypertension (all codes). In 1999, 34 patients were reported as having pulmonary hypertension at discharge, including 30 coded as IPAH (416.0) and four as either specified or unspecified chronic pulmonary heart disease (Table 2). Chart reviews of the patients assigned any of the ICD-9-CM diagnosis codes for pulmonary hypertension revealed that the use of the nonspecific term “pulmonary hypertension” without any modifier was most common. Only two charts of 30 specifically suggested possible IPAH, listed as primary pulmonary hypertension and as pulmonary hypertension, no evidence for a secondary cause. The remaining patients had a secondary condition listed that was very likely to be associated with pulmonary hypertension (n = 29), or there was too little information available to accurately evaluate (n = 3).
In contrast, in 2002, 27 patients were reported as having pulmonary hypertension, and only three were coded as IPAH. The remainder were coded as other chronic pulmonary heart disease (n = 22) or chronic pulmonary heart disease, unspecified (n = 2). Of the three patients coded as IPAH, the term “primary pulmonary hypertension” was used in one case. Upon review, this patient was believed to possibly have IPAH, but there was no evidence that a right-sided heart catheterization had been performed. The other patients had interstitial lung disease (n = 1) and sarcoidosis (n = 1) and were classified as pulmonary hypertension associated with another condition. The terminology used by physicians in 2002 was similar to that used in 1999; most continued to use the term “pulmonary hypertension” without listing a specific modifier or associated condition.
Discussion
Two main observations were made in this study. First, reported IPAH mortality increased markedly from 1979 to 2002, and most of the increase was reported for patients aged > 65 years. Second, sharp declines in both reported IPAH mortality (2003 and onward) and IPAH discharge diagnoses (2001 and onward) were seen during years where total pulmonary hypertension deaths and discharges increased. Combined with the results from our chart review, these findings suggest that most cases reported as IPAH in databases prior to between 2000 and 2003 (depending on the database) were unlikely to have had IPAH. These findings should lead to a review of any conclusions made about IPAH based on database studies from that era, including reports of an association found between black race and mortality from IPAH, an association reported between IPAH and increased prevalence of diabetes, and a trend showing increasing IPAH mortality throughout the 1990s.7,10,11
Changes in ICD-9-CM and ICD-10 Coding Manuals
The sudden changes in reported IPAH mortality and hospital discharges correspond to changes made in the coding systems. For the NCHS death certificate database, the term “other secondary pulmonary hypertension” was added in 2003, and the index order was changed, corresponding to the fall in reported IPAH mortality that began in 2003. A similar decline was seen in reported IPAH discharges from the NIS database from 2000 to 2001 after a change that involved the ICD-9-CM index. This change was more difficult to identify because the coding entries did not change. However, the 1999 ICD-9-CM Coordination and Maintenance Committee Meeting described plans for a switch in the default code for the term “pulmonary hypertension,” and we were able to confirm that this change was implemented in 2000, corresponding to the decline in IPAH hospital discharges in 2001.12
Studies using the Scottish Morbidity Record (SMR) indirectly suggest that pulmonary hypertension diagnosis code accuracy also may be low in databases in use outside the United States. In two studies of the SMR, inclusion and exclusion criteria were developed where patients were included if they were aged ≤ 65 years at diagnosis, had IPAH listed in the first or second coding position, and had no other explanatory diagnosis (code) listed, including connective tissue disease, parenchymal lung disease, heart failure, congenital heart disease, and others.13,14 The authors believed that patients meeting these criteria were likely to have IPAH, and they derived estimates of IPAH incidence and prevalence in Scotland from this subgroup. The remaining 96% of patients coded as IPAH were believed unlikely to truly have IPAH, and these patients were excluded. These results suggest that most patients coded as having IPAH likely had a different form of pulmonary hypertension.
Age Distribution
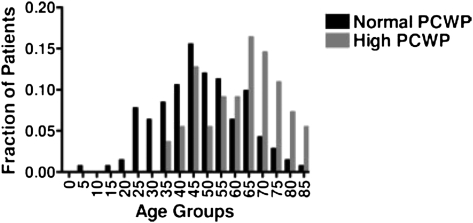
The other trend of note in the NCHS database was the almost 10-fold increase in reported IPAH mortality among patients aged > 65 years that was seen between 1979 and 2002. Potential contributors to this increase include longer survival for patients with IPAH in general, increased detection rates in older patients, and a real change in the age distribution for IPAH. Alternatively, misdiagnosis and miscoding also could have contributed to the changing age distribution. Our study most strongly suggests miscoding, but we suspect that misdiagnosis also may contribute. Other studies have found that older patients with otherwise unexplained pulmonary hypertension are more likely to have elevated wedge pressures at cardiac catheterization compared with younger patients (56% vs 19%; P < .05) (Fig 4)15,16 and are more likely to have comorbidities that are associated with diastolic congestive heart failure, such as diabetes, hypertension, and obesity.17 These findings emphasize the importance of a complete work-up prior to making an IPAH diagnosis in older patients.
Figure 4.
PCWP among patients with unexplained PH at a referral center. Older patients with otherwise unexplained PH after a noninvasive work-up are more likely to have an elevated wedge pressure at the time of cardiac catheterization compared with younger patients. Republished with permission of American College of Chest Physicians.15 PCWP = pulmonary capillary wedge pressure. See Figure 1 legend for expansion of other abbreviation.
Potential Modifications
Consideration should be made to updating the coding system to reflect the widely used clinical classification system (Tables 1, 3).18 For nonidiopathic World Health Organization group 1 pulmonary arterial hypertension (ie, connective tissue disease, HIV, congenital heart disease), we suggest a separate code with the descriptor other pulmonary arterial hypertension. For World Health Organization group 2-5 pulmonary hypertension, we suggest a code with the descriptor pulmonary hypertension, other specified. We would avoid the nonspecific and outdated term “secondary” in describing either group. Additionally, coding system changes will only be effective if physician documentation includes appropriate, descriptive pulmonary hypertension diagnoses. On the basis of our chart review results, additional physician training in the differential diagnosis for pulmonary hypertension also is needed.
Table 3.
—Updated Clinical Classification of PH18
| Primary Code | Secondary Code |
| 1. PAH | 1.1 Idiopathic PAH |
| 1.2 Heritable | |
| 1.2.1 BMPR2 | |
| 1.2.2 ALK1, endoglin (with or without hereditary hemorrhagic telangiectasia) | |
| 1.3 Drug and toxin induced | |
| 1.4 Associated with | |
| 1.4.1 Connective tissue diseases | |
| 1.4.2 HIV infection | |
| 1.4.3 Portal hypertension | |
| 1.4.4 Congenital heart disease | |
| 1.4.5 Schistosomiasis | |
| 1.4.6 Chronic hemolytic anemia | |
| 1.5 Persistent pulmonary hypertension of the newborn | |
| 1′ pulmonary venoocclusive disease and/or pulmonary capillary hemangiomatosis | |
| 2. PH owing to left-sided heart disease | 2.1 Systolic dysfunction |
| 2.2 Diastolic dysfunction | |
| 2.3 Valvular disease | |
| 3. PH owing to lung disease and/or hypoxia | 3.1 COPD |
| 3.2 Interstitial lung disease | |
| 3.3 Other pulmonary diseases with mixed restrictive and obstructive pattern | |
| 3.4 Sleep-disordered breathing | |
| 3.5 Alveolar hypoventilation disorders | |
| 3.6 Chronic exposure to high altitude | |
| 3.7 Developmental abnormalities | |
| 4. Chronic thromboembolic PH | |
| 5. PH with unclear multifactorial mechanisms | 5.1 Hematologic disorders: myeloproliferative disorders, splenectomy |
| 5.2 Systemic disorders: sarcoidosis, pulmonary Langerhans cell histiocytosis: lymphangioleiomyomatosis, neurofibromatosis, vasculitis | |
| 5.3 Metabolic disorders: glycogen storage disease, Gaucher disease, thyroid disorders | |
| 5.4 Others: tumoral obstruction, fibrosing mediastinitis, chronic renal failure on dialysis |
Conclusions
IPAH is a diagnosis of exclusion that cannot be made without thorough clinical evaluation. In contrast to pulmonary hypertension related to left-sided heart disease and to other medical conditions, IPAH is rare and should not have been the most common type of pulmonary hypertension reported. Earlier database studies that relied on the IPAH diagnosis code need to be reevaluated because it is likely that patients with other types of pulmonary hypertension were inadvertently included in the analyses and that many of these results are inaccurate (Table 4).7,8,10,11,13,14,19 Combinations of specific diagnosis codes could be more accurate, such as the inclusion and exclusion criteria used in the SMR studies, but this strategy needs to be validated. Our findings reinforce the importance of validation studies when using ICD codes in epidemiologic studies and support the value of prospectively collected data in IPAH, including ongoing registries and cohort studies.
Table 4.
—PH Studies Using ICD Codes
| Study/Year Range | Database | Strategy | Select Reported Findings |
| Lilienfeld and Rubin7/1979-1996 | NCHS | ICD-9 code 416.0 | Mortality rates for IPAH increased in the United States from 1979-1996. Some portion of this increase may be related to anorexigens. |
| Rothman19/1990-1997 | NCHS | ICD-9 code 416.0 limited to only age 20-54 y | Letter after Lilienfeld paper: There is no evidence of an epidemic around the peak years of fenfluramine use in the age groups most likely to have used anorexigens. |
| Movahed et al10/1990-2000 | VA | ICD-9 code 416.0 | Patients with diabetes mellitus have significantly higher prevalence of IPAH, independent of coronary artery disease, hypertension, congestive heart failure, or smoking (OR, 1.53; P < .05). |
| Hyduk et al8/1980-2002 | Multiple | All PH codes combined | The number of deaths from PH (all forms) increased from 1980-2002, and older women represent the majority of decedents. |
| Peacock et al13/1986-2001 | SMR | ICD-9 416.0 or ICD-10 I27.0 plus exclusion strategy | Prevalence of PAH may be higher than previously reported. This may be due to underestimation by the centers or overestimation by hospital data. |
| Davis et al11/1994-1998 | NCHS | ICD-9 416.0 | Blacks with PH exhibit a substantially increased mortality compared with whites, particularly black women. |
| Carrington et al14/1986-2001 | SMR | Same as Peacock et al13 | Mortality rates for PH are lower in the current era, particularly for patients with connective tissue disease-related PAH. |
Six studies investigated trends or associations with IPAH (ICD-9 code 416.0), either using all IPAH diagnoses or using a strategy to identify patients more likely to truly have IPAH. One study evaluated all forms of PH combined (ICD-0 code 416.x) but did not look at the individual diagnosis codes. NCHS = National Center for Health Statistics Database; SMR = Scottish morbidity record; VA = Veterans Administration Hospitals. See Table 1 and 2 legends for expansion of other abbreviations.
Acknowledgments
Author contributions: Dr Link: contributed to study design, manuscript revision, and final approval of the manuscript.
Dr Glazer: contributed to manuscript revision.
Dr Torres: contributed to manuscript revision.
Dr Chin: contributed to study design, manuscript revision, and final approval of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Torres has received consulting and speakers fees from Actelion, Pfizer, Novartis, Gilead, United Therapeutics, the National Institutes of Health, Bayer, and MedTronics; Dr Chin has received consulting and speakers fees from Gilead, United Therapeutics, and Actelion. Drs Link and Glazer have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Abbreviations
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD-10
International Classification of Diseases, 10th Revision
- IPAH
idiopathic pulmonary arterial hypertension
- NCHS
US National Center for Health Statistics
- NIS
Nationwide Inpatient Sample
- SMR
Scottish Morbidity Record
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (http://www.chestpubs.org/site/misc/reprints.xhtml).
Funding/Support: This work was supported by a National Institutes of Health grant [UL1RR024982] titled “North and Central Texas Clinical and Translational Science Initiative.”
For editorial comment see page 482
References
- 1.Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006;173(9):1023–1030. doi: 10.1164/rccm.200510-1668OC. [DOI] [PubMed] [Google Scholar]
- 2.Thenappan T, Shah SJ, Rich S, Gomberg-Maitland M. A USA-based registry for pulmonary arterial hypertension: 1982-2006. Eur Respir J. 2007;30(6):1103–1110. doi: 10.1183/09031936.00042107. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed February 17, 2010.
- 4.Rubin LJ. Primary pulmonary hypertension. Chest. 1993;104(1):236–250. doi: 10.1378/chest.104.1.236. [DOI] [PubMed] [Google Scholar]
- 5.Thomas AJ. Chronic pulmonary heart disease. Br Heart J. 1972;34(7):653–657. doi: 10.1136/hrt.34.7.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chronic cor pulmonale Report of an expert committee. Circulation. 1963;27(4):594–615. [PubMed] [Google Scholar]
- 7.Lilienfeld DE, Rubin LJ. Mortality from primary pulmonary hypertension in the United States, 1979-1996. Chest. 2000;117(3):796–800. doi: 10.1378/chest.117.3.796. [DOI] [PubMed] [Google Scholar]
- 8.Hyduk A, Croft JB, Ayala C, Zheng K, Zheng ZJ, Mensah GA. Pulmonary hypertension surveillance—United States, 1980-2002. MMWR Surveill Summ. 2005;54(5):1–28. [PubMed] [Google Scholar]
- 9.McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association: developed in collaboration with the American College of Chest Physicians, American Thoracic Society, Inc., and the Pulmonary Hypertension Association. Circulation. 2009;119(16):2250–2294. doi: 10.1161/CIRCULATIONAHA.109.192230. [DOI] [PubMed] [Google Scholar]
- 10.Movahed MR, Hashemzadeh M, Jamal MM. The prevalence of pulmonary embolism and pulmonary hypertension in patients with type II diabetes mellitus. Chest. 2005;128(5):3568–3571. doi: 10.1378/chest.128.5.3568. [DOI] [PubMed] [Google Scholar]
- 11.Davis KK, Lilienfeld DE, Doyle RL. Increased mortality in African Americans with idiopathic pulmonary arterial hypertension. J Natl Med Assoc. 2008;100(1):69–72. doi: 10.1016/s0027-9684(15)31177-9. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics Coordination and Maintenance Committee ICD-9-CM Coordination and Maintenance Committee Meeting, May 13, 2009, Summary. http://www.cdc.gov/nchs/data/icd9/icdm599.pdf. Accessed November 28, 2008.
- 13.Peacock AJ, Murphy NF, McMurray JJV, Caballero L, Stewart S. An epidemiological study of pulmonary arterial hypertension. Eur Respir J. 2007;30(1):104–109. doi: 10.1183/09031936.00092306. [DOI] [PubMed] [Google Scholar]
- 14.Carrington M, Murphy NF, Strange G, Peacock A, McMurray JJ, Stewart S. Prognostic impact of pulmonary arterial hypertension: a population-based analysis. Int J Cardiol. 2008;124(2):183–187. doi: 10.1016/j.ijcard.2006.12.045. [DOI] [PubMed] [Google Scholar]
- 15.Shapiro BP, McGoon MD, Redfield MM. Unexplained pulmonary hypertension in elderly patients. Chest. 2007;131(1):94–100. doi: 10.1378/chest.06-1571. [DOI] [PubMed] [Google Scholar]
- 16.Rich S. How do we explain unexplained pulmonary hypertension in the elderly? Chest. 2007;131(1):5–6. doi: 10.1378/chest.06-2329. [DOI] [PubMed] [Google Scholar]
- 17.Robbins IM, Newman JH, Johnson RF, et al. Association of the metabolic syndrome with pulmonary venous hypertension. Chest. 2009;136(1):31–36. doi: 10.1378/chest.08-2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simonneau G, Robbins IM, Beghetti M, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2009;54(1) suppl:S43–S54. doi: 10.1016/j.jacc.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 19.Rothman RB. The age-adjusted mortality rate from primary pulmonary hypertension, in age range 20 to 54 years, did not increase during the years of peak “phen/fen” use. Chest. 2000;118(5):1516–1517. doi: 10.1378/chest.118.5.1516. [DOI] [PubMed] [Google Scholar]