Medicare spending on pharmaceuticals varies substantially among U.S. localities and hospital-referral regions, even after adjustment for variation in demographic characteristics, individual health status, and insurance coverage.1 If the drugs that are prescribed in high-spending regions are necessary and appropriate, the high spending may be justified by the health improvement they generate. But if such prescribing is not appropriate, the higher use could have serious adverse consequences. The elderly are twice as likely as people under the age of 65 years to have adverse events associated with drugs and almost seven times as likely to be hospitalized as a result.2 Although we have established that regions with higher drug spending do not seem to have offsetting reductions in medical spending (after adjustment for variation in medical risk),1 little is known about how, if at all, the quality of prescribing varies among regions and whether any of the variation in quality, rather than quantity, is associated with variation in medical spending.
To assess geographic variation in the management of medication in the elderly, we used two quality measures from the Health-care Effectiveness Data and Information Set (HEDIS): the use of medications that are considered to be high-risk for the elderly and potentially harmful drug–disease interactions.3 The former measure assesses whether a Medicare beneficiary received at least one drug that should be avoided in the elderly; these drugs include some antihistamines, long-acting benzodiazepines, thioridazine, and some skeletal muscle relaxants, among others (see the Supplementary Appendix, available with the full text of this article at NEJM.org). The latter measure assesses whether Medicare beneficiaries with evidence of one of three underlying diseases — dementia, a history of hip or pelvic fracture, or chronic renal failure — are given a prescription in an ambulatory care setting that is contraindicated for that condition.
We used pharmacy and medical claims data from a random sample of 5% of Medicare beneficiaries who were enrolled in stand-alone Medicare Part D plans in 2007.1 We restricted our sample to beneficiaries who were between 65 and 99 years of age in 2007, were alive on December 31, 2007, and were enrolled for the full year in Medicare Parts A and B and a stand-alone Part D plan. We assigned each person in the resulting sample of 533,170 beneficiaries to one of the 306 Dartmouth hospital-referral regions on the basis of the ZIP Code of residence.
To determine the amount of variation in the use of high-risk medications, we calculated the proportion of beneficiaries in each hospital-referral region who had received at least one high-risk drug in 2007. We assessed the potentially harmful drug–disease interactions for each of the three conditions separately and used a combination measure indicating the proportion of patients with at least one of the three conditions who were taking any potentially harmful drug. For instance, we first identified the earliest indication of dementia during 2007 and determined whether beneficiaries with such an indication had received any drug classified as potentially harmful for persons with dementia in 2007, at the time of or after the first indication. We then calculated the proportion of beneficiaries with dementia in each hospital-referral region who had received a potentially harmful drug in 2007. In our sample, 16% of beneficiaries had received a diagnosis of dementia, 5% had a history of hip or pelvic fracture, and 16% had chronic renal failure; 29% had one or more of these conditions.
To ensure that our results would not be influenced by measures from hospital-referral regions that had few beneficiaries, which could be subject to substantial sampling error, we focused on regions with at least 25 beneficiaries who could be included in analyses of a given measure. We therefore excluded 50 regions from our analysis of the hip-fracture measure but not from our analysis of the composite measure. However, we found that the inclusion of all 306 regions for all measures would not have changed our conclusions. Drugs with potentially harmful interactions with underlying diseases and high-risk drugs each accounted for less than 1% of total drug spending.
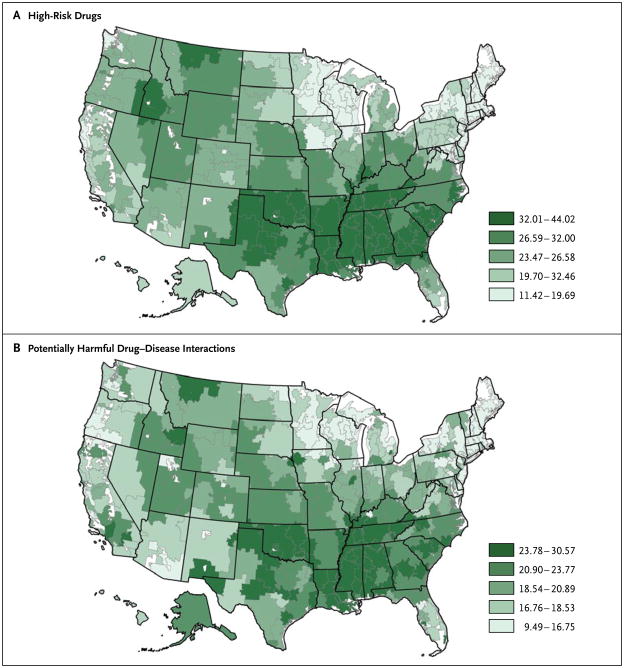
The table shows the variation among hospital-referral regions in drug spending and in the two HEDIS measures (lower utilization of potentially dangerous drugs is considered a sign of higher-quality care), and the maps show how performance on the quality measures vary across hospital-referral regions. Our analysis offers three key messages.
First, hospital-referral regions vary substantially in terms of HEDIS measures of the quality of prescribing. Indeed, performance on these measures varies considerably more than spending does, whether variation is measured in terms of the coefficient of variation or the ratio of spending at the 75th percentile to that at the 25th percentile.1 The hospital-referral region with the largest proportion of elderly beneficiaries taking high-risk drugs is Alexandria, Louisiana, where 44% of elderly beneficiaries received them — four times the 11% who received them in the Bronx, New York, the best-performing hospital-referral region on this measure. The ratio of the 75th to the 25th percentile for the use of high-risk medication was 1.49, and the coefficient of variation was 0.27. The two quality measures were positively correlated across hospital-referral regions; that is, regions generally scored well on both measures or poorly on both, with correlations for all the individual measures both positive and significant (for details, see the Supplementary Appendix).
Second, after adjustment for demographic variables and level of health risk, performance on the two measures was positively but very weakly related to overall drug spending. The coefficient for the correlation between the proportion of the population receiving high-risk drugs and total spending on all other drugs was only 0.02 (P = 0.78), and the coefficient for the correlation between the proportion receiving drugs with potentially harmful interactions with their diseases and total spending on all other drugs was 0.10 (P = 0.07). In other words, regions in which beneficiaries were more likely to be given prescriptions for potentially harmful or high-risk drugs did not necessarily spend more on drugs overall than regions in which beneficiaries were less likely to use such drugs.
Third, both markers of low-quality prescribing were positively associated with higher medical spending, excluding drug spending (r = 0.30 for the proportion taking high-risk drugs; r = 0.25 for the proportion taking drugs with potentially harmful interactions with their underlying diseases [P<0.001 for both correlations] (see the Supplementary Appendix). In other words, the regions in which nondrug medical spending per beneficiary was higher were also the regions in which beneficiaries were more likely to be given prescriptions for potentially harmful or high-risk drugs — a finding that does not support the premise that higher medical spending leads to higher-quality prescription use. Our measures were adjusted for patients’ risk scores, but because similar patients appear to be coded as sicker in high-spending areas than in lower-spending areas,4 we also examined the correlation between the quality measures and medical or drug spending without adjusting for patients’ risk scores. Analyzed in this way, the correlations between spending and the prevalence of low-quality prescribing were even stronger and more highly significant than they were with risk adjustment and thus are not an artifact of risk-coding practices.
In sum, according to HEDIS measures of potentially dangerous prescribing patterns, the quality of prescribing for the elderly varies substantially among local markets — substantially more, in fact, than does spending on drugs overall. Our results do not support the theory that high-spending areas simply use more of everything, including inappropriate drugs, since the association between overall drug spending and inappropriate prescribing is weak. In addition, because spending on nondrug medical care is positively associated with a greater use of potentially harmful drugs, our results also do not suggest that more medical spending is associated with better health care overall. Our results are consistent, however, with an association between lower-quality prescription patterns and more adverse drug events that may require additional expense to treat.
Supplementary Material
Figure 1. Quintiles of Performance on HEDIS Measures of the Quality of Drug Prescribing, According to Hospital-Referral Region in 2007.
Measures on HEDIS (Healthcare Effectiveness Data and Information Set) range from 11.4 to 44.0% for use of high-risk drugs (Panel A) and from 9.5 to 30.6% for potentially harmful drug–disease interactions (Panel B). Lower scores indicate better quality.
Table 1.
Variation in Annual Pharmacy Spending and HEDIS Quality Measures Related to Medication Use among Elderly Beneficiaries in Different Hospital-Referral Regions.*
| Variable | Lowest Value† | 25th Percentile | Median | 75th Percentile | Highest Value | Mean | Ratio of Highest Value to Lowest Value | Ratio of 75th to 25th Percentile | Coefficient of Variation |
|---|---|---|---|---|---|---|---|---|---|
| 2007 dollars | |||||||||
|
Drug spending‡ | |||||||||
| Annual gross spending per beneficiary | 1,851 | 2,274 | 2,413 | 2,537 | 3,026 | 2,410±204 | 1.63 | 1.12 | 0.08 |
| percent | |||||||||
|
HEDIS quality measure§ | |||||||||
| Use of high-risk medication | 11.4 | 20.6 | 24.9 | 30.6 | 44.0 | 25.8±6.9 | 3.85 | 1.49 | 0.27 |
| Potentially harmful drug– disease interactions | |||||||||
| Dementia | 11.2 | 21.0 | 24.3 | 29.0 | 45.7 | 25.1±6.0 | 4.09 | 1.38 | 0.24 |
| Hip or pelvic fracture | 4.5 | 15.4 | 19.0 | 22.6 | 38.4 | 19.1±5.5 | 8.62 | 1.47 | 0.29 |
| Chronic renal disease | 3.2 | 11.2 | 13.4 | 16.0 | 24.9 | 13.8±3.8 | 7.80 | 1.43 | 0.27 |
| ≥1 condition | 9.5 | 17.3 | 19.7 | 22.8 | 30.6 | 20.2±4.2 | 3.22 | 1.31 | 0.21 |
Plus–minus values are means ±SD.
The lowest-value category shows data for the hospital-referral region that was lowest within each category among hospital-referral regions in which the measure applied to at least 25 beneficiaries.
Gross drug spending, which is reported in 2007 dollars, includes out-of-pocket spending by beneficiaries, subsidy amounts paid by the government, and spending by Medicare Part D plans before rebates. Values for adjusted annual gross drug spending per beneficiary differ slightly from those in our previous study1 because we used an improved measure of the number of people receiving the low-income subsidy; this change does not affect the conclusions of the previous study.
Lower scores on each of the quality measures in the Healthcare Effectiveness Data and Information Set (HEDIS) represent better quality. A total of 256 hospital-referral regions were included in the analysis of the proportion of elderly beneficiaries with hip or pelvic fracture who were receiving potentially harmful drugs. All other analyses included 306 hospital-referral regions.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Zhang Y, Baicker K, Newhouse JP. Geographic variation in Medicare drug spending. N Engl J Med. 2010;363:405–9. doi: 10.1056/NEJMp1004872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The State of Health Care Quality. Washington, DC: National Committee for Quality Assurance; 2009. ( http://www.ncqa.org/Portals/0/Newsroom/SOHC/SOHC_2009.pdf) [Google Scholar]
- 3.The Healthcare Effectiveness Data and Information Set (HEDIS) Washington, DC: National Committee for Quality Assurance; 2010. ( http://www.ncqa.org/tabid/59/default.aspx) [Google Scholar]
- 4.Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES. Regional variations in diagnostic practices. N Engl J Med. 2010;363:45–53. doi: 10.1056/NEJMsa0910881. [Erratum, N Engl J Med 2010; 363:198.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.