Abstract
A case of solitary bone metastasis from breast cancer, where MRI assessment of treatment response was inaccurate and whole-body fluorodeoxyglucose (18FDG) positron emission tomography with computed tomography (PET-CT) proved more reliable and objective, is presented.
Case presentation
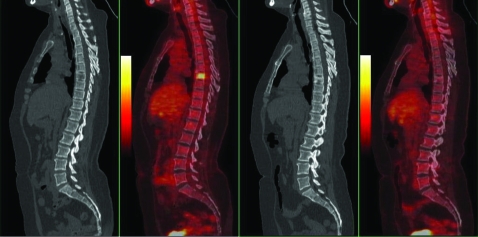
A fit, 54-year-old, postmenopausal woman presented with an upper outer quadrant left breast mass in October 2007, for which she underwent conservative surgery. Histology revealed a 27 mm, grade 3, oestrogen receptor (ER) positive, human epidermal growth factor receptor 2 (HER2) negative, invasive ductal cancer with involvement of 25 of 27 nodes (pT2 pN3). Staging investigations were requested and she was referred on to us for consideration of adjuvant treatment. The only positive finding was an area of focally increased tracer uptake in the L3 vertebral body on bone scan. This prompted further evaluation of her spine by MRI, which revealed no abnormality at L3 but unfortunately suggested a solitary metastatic deposit in the body of the T7 vertebra (figure 1). An interventional biopsy was not deemed feasible and an open biopsy was considered inappropriate. By consensus a positron emission tomography with computed tomography (PET-CT) scan was requested to evaluate the area further. This confirmed the presence of a 2 cm intensely hypermetabolic, lytic lesion in the body of T7 consistent with a metastatic deposit (figure 2). The patient was given an aromatase inhibitor (letrozole) and bisphosphonate (ibandronate) in January 2008.
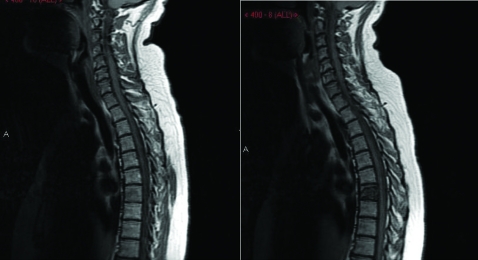
Figure 1.
MRI of the spine before (left panel) and after (right panel) treatment showing obvious deterioration in the appearance of the lesion in the T7 vertebra.
Figure 2.
Positron emission tomography with computed tomography (PET-CT) scans before (left panels) and after (right panels) treatment showing resolution of the intensely hypermetabolic deposit with treatment.
Outcome and follow-up
When reviewed in the clinic a month later, her backache had resolved. However, MRI of the spine 3 months after the initiation of treatment suggested progression of her disease with worsening destruction of T7 (figure 1). The incongruity between her symptomatic improvement and the MRI appearance prompted us to request a further PET-CT scan in May 2008, which in startling contrast to the MRI showed a complete metabolic response in the T7 vertebral lesion. The fluorodeoxyglucose (FDG) uptake had normalised and there was a sclerotic margin consistent with healing of the metastasis (figure 2). She continued treatment without side effects and stayed in remission until May 2009, when she was found to have multiple bone metastases.
Discussion
Bone metastases, unless lytic and accompanied by a soft tissue component, are non-measurable by Response Evaluation Criteria In Solid Tumors (RECIST) criteria. The objective evaluation of their response to non-surgical treatment is notoriously difficult and most clinicians rely primarily on the extent of symptomatic benefit to assess treatment response.
MRI has been recognised as the most sensitive imaging technique in the detection of bone metastases.1 Early publications suggested the use of T1-weighted sequences to evaluate response to treatment.2 However more recent publications have indicated that MRI scans may not be entirely reliable3 and multiple imaging modalities in combination are suggested.4
18FDG PET-CT is a relatively new hybrid imaging modality in the armamentarium of clinical oncologists. Its role in the staging of various malignancies and response assessment in lymphoma is well established. However, there is a dearth of information on its routine use in metastatic bone disease. In bone-dominant breast cancer use of PET scans (without CT correlation) to evaluate response to non-surgical treatments has been reported.5,6
This case illustrates the importance of carefully correlating clinical benefit with imaging results. It also highlights the limitations of MRI in the evaluation of treatment response in spinal metastasis. Despite apparent worsening of bony disease on MRI, our patient continued to be asymptomatic and in remission for over 13 months.
Accurate assessment of treatment response is vital to provide effective treatment as well as to avoid unnecessary treatment escalation. In this case PET-CT provided an effective tool to monitor treatment response in metastatic bone disease. Prospective trials in this area may prove useful.
Learning points
Bone metastases, unless lytic and accompanied by a soft tissue component, are non-measurable by Response Evaluation Criteria In Solid Tumors (RECIST) criteria.
MRI has been recognised as the most sensitive imaging technique in the detection of bone metastases, however to evaluate response to treatment it may not be reliable
A dearth of information exists on routine use of fluorodeoxyglucose (18FDG) positron emission tomography with computed tomography (PET-CT) in metastatic bone disease
18FDG PET-CT may provide an effective tool to monitor treatment response in metastatic bone disease.
It is important to carefully correlate imaging results with clinical benefit.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Husband JE, Padhani AR, eds. Metastatic bone tumours. : Recommendations for cross-sectional imaging in cancer management. London, UK: The Royal College of Radiologists, 2006: 108–10 [Google Scholar]
- 2.Husband JE, Johnson RJ, Reznek RH, eds. Bone metastases. : A guide to the practical use of MRI in oncology. Board of the Faculty of Clinical Radiology. London, UK: The Royal College of Radiologists, 1999: 31–3 [Google Scholar]
- 3.Vanel D, Husband JE, Padhani AR. Bone metastases. : Husband JE, Reznek RH, eds. Imaging in oncology. 2nd edn Oxford, UK: Taylor and Francis, 2004: 1041–58 [Google Scholar]
- 4.Hamaoka T, Madewell JE, Podoloff DA, et al. Bone imaging in metastatic breast cancer. J Clin Oncol 2004; 22: 2942–53 [DOI] [PubMed] [Google Scholar]
- 5.Stafford SE, Gralow JR, Schubert EK, et al. Use of serial FDG PET to measure the response of bone-dominant breast cancer to therapy. Acad Radiol 2002; 9: 913–21 [DOI] [PubMed] [Google Scholar]
- 6.Specht JM, Tam SL, Kurland BF, et al. Serial FDG-PET to monitor treatment of bone-dominant metastatic breast cancer predicts time to progression. Breast Cancer Res Treat 2007; 105: 87–94 [DOI] [PubMed] [Google Scholar]