Abstract
POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, skin changes) syndrome is a rare haematological condition with a constellation of clinical features that can present to the clinician in a variety of ways. This case highlights how a seemingly uncomplicated myocardial infarction can herald the development of this rare haematological disorder. While knowledge of the pathophysiological mechanisms that underpin POEMS syndrome is developing, so too are the diagnostic and treatment strategies available to the clinician.
Background
The importance of this case relates to the unmasking of a rare haematological diagnosis with the expertise of numerous medical specialities. It also explores the role of novel treatments, such as stem cell transplantation, in treating this condition while understanding of the disease is itself continuing to evolve.
Case presentation
A previously healthy 49-year-old woman was admitted to her local hospital complaining of central crushing chest pain. At the time, her full blood count was abnormal with haemoglobin 16.9 g/dl, packed cell volume 0.5, white cell count 9.9×109/l and platelets 884×109/l. Her platelet count rose to greater than 1000×109/l during her admission.
A myocardial infarction was diagnosed on the basis of infero-lateral ischaemia on her ECG and an elevated troponin T (9.5ug/l). An echocardiogram showed an akinetic inferior wall with an ejection fraction of 51%. Her myocardial infarction was managed conservatively with cardiac catheterisation being postponed given her thrombocytosis.
A presumptive diagnosis of essential thrombocythaemia was made and she declined bone marrow examination. She was commenced on hydroxycarbamide, which normalised her platelet count.
Three months later she reported fatigue, peripheral oedema and paraesthesiae of her feet, spreading proximally to her knees, with associated unsteadiness and decreased exercise tolerance. She later reported distal upper limb dysfunction with weakness, sensory impairment and neuropathic pain. Inpatient investigations included electromyography, which was suggestive of demyelinating motor neuropathy. A brain and spinal column MRI was unremarkable and cerebrospinal fluid examination showed 1.06 g/l of protein. The differential diagnosis included chronic inflammatory demyelinating polyneuropathy; therefore, she received a course of intravenous immunoglobulin. This was of no benefit.
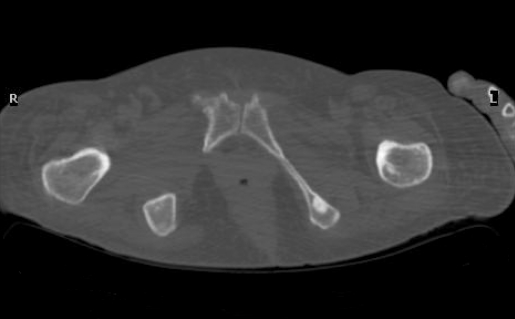
During the same admission, thyroid function tests were noted to be abnormal (thyroid stimulating hormone 4.35 mIU/l, free thyroxine 15.8 pmol/l), she had a borderline raised blood sugar at 7.2 mmol/l and her vitamin B12 levels were low at 128 ng/l. She was noted to be hirsute with hypertrichosis of her lower limbs and thickening of her skin. Protein electrophoresis showed an IgA lambda paraprotein of 4.6g/dl but her urine was negative for Bence Jones protein. A skeletal survey demonstrated osteosclerotic lesions of her pubic rami, the largest being 1.5 cm in diameter (figure 1). A diagnosis of POEMS syndrome was made and ultrasound scan of her abdomen did not reveal any organomegaly.
Figure 1.
Osteosclerotic lesion of the left pubic ramus.
Consequently, her hydroxycarbamide was discontinued. She then received radiotherapy to her osteosclerotic bone lesions, in preference to corticosteroids or alkylator treatment, given the severity of her neuropathy. Despite this treatment, her neurology rapidly progressed over the ensuing month so that she lost all power in her lower limbs with marked distal upper limb weakness. She was areflexic, with reduced pin-prick and fine touch sensation in both upper and lower limbs, and she was unable to sit up without assistance. She was mostly confined to her bed and required a hoist to transfer her from bed to wheelchair. At this time, serum vascular endothelial growth factor (VEGF) levels were measured and found to be >13 000 pg/mL (normal range up to 800 pg/mL).
Because of her steady deterioration despite radiotherapy, we proceeded to peripheral blood stem cell harvesting using cyclophosphamide (1.5 g/m2) and granulocyte-colony stimulating factor priming. She proceeded to autologous stem cell transplantation (ASCT), with melphlan (140 mg/m2) conditioning and stem cell rescue. She tolerated this well despite experiencing febrile neutropenia on day 11, which responded to antibiotic treatment and successfully engrafted on day 14.
Outcome and follow-up
Over the next 12 months her hirsutism resolved and her paraprotein became unquantifiable. Neurologically she made a marked improvement regaining near normal function of her upper limbs, transferring independently and walking with the aid of a gutter frame. She has further reclaimed some independence accessing public transport via her wheelchair, enabling her to resume a more active lifestyle, including swimming. It is now 3 years following her high-dose treatment and she is being followed up by her local physicians and physiotherapists where she continues to make good progress.
Discussion
POEMS syndrome is a rare condition related to a plasma cell dyscrasia, which frequently follows an indolent course. However, a minority of patients present with rapidly progressive disease, often dominated by the polyneuropathy, as illustrated in this case. POEMS is characterised by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes, and presents at an earlier age than multiple myeloma. Clinical features are protean, but patients frequently exhibit papilloedema, volume overload, sclerotic bone lesions (figure 1) and thrombocytosis.
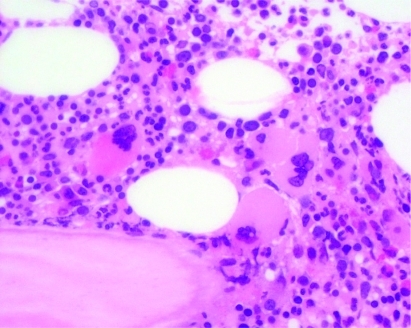
Approximately 50% of patients may present with thrombocytosis.1 Not infrequently this is mistaken for a myeloproliferative disorder, in the context of characteristic bone marrow findings, namely an increase in megakaryocytes (figure 2). Equally, ischaemic complications are well-recognised, with one series reporting 18 of 99 patients suffering from arterial events such as stroke, myocardial infarction and Budd Chiari Syndrome.2 Another study reported 20% of patients suffering with arterial occlusion,3 while an individual suffering with recurrent ischaemic strokes, in the absence of risk factors and despite anticoagulation, has also been reported.4
Figure 2.
Bone marrow trephine showing increased megakaryocytes.
The pathogenesis of POEMS is poorly understood but cytokines are believed to play an important role.5 VEGF in particular is often elevated at diagnosis and frequently normalises following successful treatment.6,7
VEGF is known to increase vascular permeability and plays an important role in angiogenesis. It has been postulated that VEGF is secreted from plasmacytomas,8 plasma cells6 and platelets9 possibly resulting in arterial obliteration. Indeed, VEGF is released from aggregated platelets in patients with POEMS9 and descriptions of closed lumina of endoneurial blood vessels raise the possibility of microthrombosis contributing to the polyneuropathy.6
Currently treatment options include radiotherapy to solitary plasmacytomas, which has been shown to be effective in approximately 50% of patients.2 Approximately 40% of patients will respond to alkylator treatment in combination with corticosteroids, while 15% may gain some benefit from corticostertoids alone.2 However, observational data strongly suggest that peripheral blood ASCT is the definitive treatment, with up to 87% of patients objectively reporting neurological improvement at 10.8 months in one study.2 Other authors cite continued improvement in neurological symptoms beyond 6 months following treatment.10
ASCT enables high-dose melphalan to be administered, followed by stem cell rescue, while allogeneic stem cell transplantation has not been reported in POEMS syndrome due to unacceptable transplant related mortality. An earlier report suggests the procedure related mortality of ASCT in POEMS patients is similar to those with multiple myeloma11 but more recently it has been recognised that there may be considerable peritransplant morbidity.12 Most notably, approximately 50% of patients are reported to experience engraftment syndrome, which manifests as fever, rash, diarrhoea, non-cardiogenic pulmonary oedema and weight gain within 96 h of neutrophil engraftment. It has been postulated that the clinical sequelae of engraftment syndrome are secondary to a cytokine burst with splenomegaly best predicting a complicated peritransplant course.12 It has been suggested that earlier and more aggressive use of corticosteroids may modulate this effect.12
Few patients have reported to have disease relapse following ASCT, with the exception of one individual we treated who developed marrow dysplasia 5 years following a reduced dose melphalan autologous stem cell transplant (110 mg/m2) and another individual who had a recurrence of sclerotic bony lesions some 7 years following transplantation.13
Learning points
POEMS syndrome is a rare haematological condition that can present with a myriad of clinical features.
Increasingly cytokine levels, particularly vascular endothelial growth factor, are being employed to monitor the disease activity.
A proportion of patients develop fulminant POEMS syndrome, with the clinical picture often being dominated by a rapidly progressive peripheral neuropathy.
Treatment options include radiotherapy, alkylator treatment and peripheral blood stem cell transplantation but need to be tailored to each individual’s disease.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Dispenzieri A, Kyle RA, Lacy MQ, et al. POEMS syndrome: definitions and long term outcome. Blood 2003; 101: 2496–506 [DOI] [PubMed] [Google Scholar]
- 2.Dispenzieri A. Hematology 2005. www.asheducationbook.hematologylibrary.org (accessed 30 March 2010) [Google Scholar]
- 3.Lesprit P, Authier FJ, Gherardi R, et al. Medicine, acute arterial obliteration: a new feature of POEMS syndrome? Medicine 1996; 75: 226–32 [DOI] [PubMed] [Google Scholar]
- 4.Forster A, Muri R. Recurrent cerebrovascular insult – manifestation of POEMS syndrome? Schweiz Med Wochenschr 1998. June 27; 128: 1059–64 [PubMed] [Google Scholar]
- 5.Rose C, Zandecki M, Copin MC, et al. POEMS syndrome: report on six patients with unusual clinical signs, elevated levels of cytokines, macrophage involvement and chromosomal aberrations of bone marrow plasma cells. Leukemia 1997; 11: 1318–23 [DOI] [PubMed] [Google Scholar]
- 6.Watanabe O, Maruyama I, Arimura K, et al. Overproduction of vascular endothelial growth factor/vascular permeability factor is causative in Crow-Fukase (POEMS) syndrome. Muscle Nerve 1998; 21: 1390–7 [DOI] [PubMed] [Google Scholar]
- 7.Soubrier M, Dubost JJ, Serre AF, et al. Growth factors in POEMS syndrome: evidence for marked increase in circulating vascular endothelial growth factor. Arthritis & Rheum 1997; 40: 786–7 [DOI] [PubMed] [Google Scholar]
- 8.Kuwabara S, Dispenzieri A, Arimura K, et al. Treatment for POEMS. Cochrane Database Systematic Database Review, Oct 2008 [DOI] [PubMed] [Google Scholar]
- 9.Hashiguchi T, Arimura K, Matsumuro K, et al. Highly concentrated vascular endothelial growth factor in platelets in Crow-Fukase syndrome. Muscle Nerve 2000; 23: 1051–6 [DOI] [PubMed] [Google Scholar]
- 10.Kuwabara S, Misawa S, Kinai K, et al. Neurologic improvement after peripheral blood stem cell transplantation in POEMS syndrome. Neurology 2008; 71: 1691–5 [DOI] [PubMed] [Google Scholar]
- 11.Peggs KS, Paneesha S, Kottaridis PD, et al. Peripheral blood stem cell transplantation for POEMS syndrome. Bone Marrow Transplant 2002; 30: 401–4 [DOI] [PubMed] [Google Scholar]
- 12.Dispenzieri A, Lacy MQ, Hayman SR, et al. Peripheral blood stem cell transplant for POEMS syndrome is associated with high rates of engraftment syndrome. Eur J Haematol 2008. May 1; 80: 397–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giglia F, Chiapparini L, Fariselli L, et al. POEMS syndrome; relapse after successful autologous peripheral blood stem cell transplantation. Neuromusc Disord 2007; 17: 980–2 [DOI] [PubMed] [Google Scholar]