Abstract
Surgical treatment of most displaced proximal humerus fractures is challenging due to osteoporosis. Locking plates are intended to provide superior mechanical stability. In a prospective multicentre study 131 patients were treated with second generation locked plating (NCB-PH, Zimmer, Inc.). The open procedure (n = 78) was performed using a deltopectoral approach; the minimally invasive technique (n = 53) involved percutaneous reduction and an anterolateral deltoid split approach. Clinical and radiological follow-up was obtained. Improvement in function (ROM) was statistically significant. Fracture type (AO) had the most significant impact on the incidence of complications. The most frequent complications detected were intra-articular screw perforation (15%) and secondary displacement (8%). Complication rate and functional outcome of the NCB-PH are comparable to reports in the literature. Not all problems are likely to be solved by this new generation of implants, i.e. secondary dislocation still occurred in 8% of our patients.
Introduction
Fractures of the proximal humerus are a common injury and account for 5% of all fractures and 45% of all humerus fractures. It is a typical injury of the elderly patient and is mostly related to osteoporosis [1]. Surgical options for treatment are numerous, including anatomical reconstruction using extra- or intramedullary fixation techniques or hemiarthroplasty [2–4]. Besides anatomical reconstruction, a major goal of head-preserving procedures is to achieve high primary stability, allowing early functional rehabilitation. This is hard to achieve in osteoporotic bone which makes surgical treatment of these fractures a challenge [5, 6]. Failure of fixation is a common problem especially with conventional plating techniques [7–9].
Fixed-angle devices have been developed to enhance fracture stability [10]. Biomechanical in vitro studies confirmed the superior mechanical strength of these new devices compared to conventional implants [11, 12]. The clinical experience is rapidly growing [13–16]. A fixed-angle device of the second generation for treatment of proximal humeral fractures is the NCB® PH (non-contact-bridging for the proximal humerus) plate (Zimmer, Inc.) [17]. The system allows both open and minimally invasive (MI) application. Early clinical results in smaller populations have been promising [18, 19]. The objective of this prospective, multicentre study was to investigate the clinical outcome and complication rate of this device in a bigger population and to analyse the influence of the open and MI surgical techniques on the results.
Materials and methods
Implant and surgical technique
The titanium plate is anatomically precontoured and is available in two versions, either with four holes or five holes on the plate shaft. Screws can be inserted with a radius of 30° (polyaxial screw placement) and allow plate-to-bone compression for fracture reduction against the plate. Angular stability can be achieved by secondary insertion of a locking cap [17].
A radiolucent aiming system is available for MI plate insertion which defines a diverging screw position. The plate is attached to the handle bar and inserted sub-muscularly, maintaining the distal plate tip on the bone to protect the axillary nerve. The following steps are important for the MI technique. First, the screws should be inserted with a sleeve protection assembly and a drill guide. Second, after the stab incision in the skin, blunt dissection down to the plate is performed with scissors. Third, an oscillating drill technique is used [18].
In both open and MI techniques the patient is positioned in the beach-chair or supine position to allow two plane intraoperative C-arm image intensifier views. The C-arm is placed at the head of the operating table. For the open surgical technique, open reduction and internal fixation (ORIF) is performed using a standard deltopectoral approach. The MI technique uses a deltoid split approach starting at the anterolateral acromion [18]. Fracture reduction is performed percutaneously as described previously [17, 20].
In 92 cases the four-hole shaft version of the plate was used, and in 39 the five-hole shaft version.
Patients were immobilised postoperatively in a sling. The time of immobilisation and the exact rehabilitation scheme was at the discretion of the participating hospitals.
Patient population
The indication for surgery was based on the Neer criteria according to which fragment displacement of >1 cm or >0.5 cm for the greater tuberosity, shaft displacement of >10 mm, angular displacement of >45°, destruction of the medial metaphyseal column and an intraarticular step-off of >2 mm was always considered an indication for surgery [20, 21]. Exclusion criteria for the study were pathological fractures, open fractures, inability to give informed consent, pregnancy and age less than 18 years. Additionally, patients were excluded when operated upon by surgeons who had performed less than three cases using the implant. According to the criteria given above and after consent from the local ethics committees had been obtained, a total of 131 consecutive patients (91 women, 40 men) were included prospectively. These patients underwent surgery between October 2004 and December 2006 (27 months) in the orthopaedic trauma departments of five different hospitals (Ulm, Germany = ULM; St. Gallen, Switzerland = KSSG; Cremona, Italy = CREM; Tübingen, Germany = BGTUB; Dordrecht, Netherlands = DORD). Among the participating hospitals there were three level 1 trauma centres (ULM, KSSG and BGTUB) and two level 2 trauma centers (CREM and DORD). Seventy-eight patients (60%) were treated by open reduction and 53 (40%) with the MI technique.
The distribution of patients among the five hospitals was 23 at ULM (n = 22 MI, n = 1 open), 50 at KSSG (n = 50 open), 25 at CREM (n = 18 MI, n = 7 open), 21 at BGTUB (n = 7 MI, n = 14 open), and 12 at DORD (n = 6 MI, n = 6 open). The average age was 67 years (range 18–93).
The most frequent type of fracture according to the AO classification system was type B (n = 54; 41%) [22]. There were 30 (23%) type A and 47 (36%) type C fractures. The left shoulder was affected in 68 (52%) and the right shoulder in 63 (48%) patients. In 71 (54%) patients the dominant arm was affected.
Follow-up
In total, 107 patients were included (75 women, 32 men; average age 66.1 years, range 18.5–91.8), with a follow-up rate of 82%. Twenty patients were lost to follow-up, because they could not be contacted using the documented telephone number and address or because the informed consent initially given was withdrawn. Four patients died due to causes unrelated to the fracture. Sixty-one patients (42 women, 19 men; average age 65 years, range 25.6–89.5) were treated by the open surgical technique, and 46 (33 women, 13 men; average age 67.6 years, range 18.5–91.8) were treated with the MI surgical technique. Data were collected at discharge, at six weeks, and at three, six and 12 months postoperatively. The mean follow-up period in this study was 9.5 months (range 6–12). Sixty-three patients were seen one year postoperatively.
At each follow-up, range of motion (ROM) was determined and an iADL score (instrumental activities of daily living) was applied. Additionally, this score was applied retrospectively for the preoperative situation. The iADL score questions eight activities of daily living (1, put on a coat; 2, sleeping on painful side; 3, washing the back/fastening a bra; 4, toilet hygiene; 5, combing hair; 6, reaching an overhead shelf; 7, lifting 5 kg above shoulder level; 8, throwing a ball). Each activity could be assigned three points maximum (3 for no problems, 2 for mild problems, 1 for very difficult, 0 for impossible). All items had the same weighting. The overall result for the iADL score was then divided by the number of items answered, which led to a maximum score of 3 points. The subjective outcome for pain and mobility was assessed using the visual analogue scale (VAS). A maximum of 10 points could be assigned for the two criteria, where 10 points was the score for maximum pain and also for optimal function. Standard X-rays in AP and transscapular view were obtained at each follow-up. The follow-up at each participating centre was conducted by one investigator.
Statistics
Statistics were performed using SPSS Software 16.0 (SPSS Inc., Chicago IL, USA). Mann-Whitney U-test was used for independent samples (open vs. MI). Wilcoxon signed-rank test was used for related samples. Results with p < 0.05 were considered statistically significant.
Results
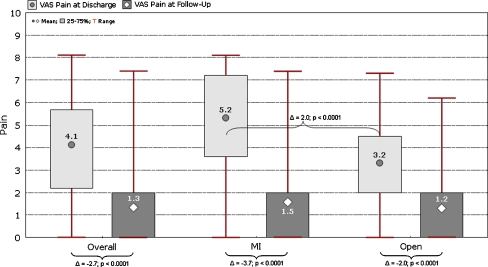
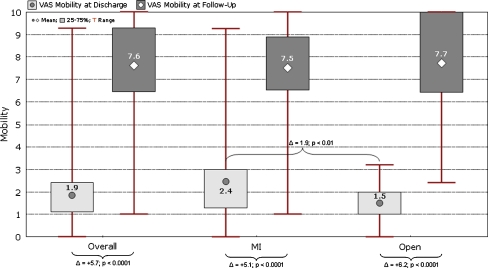
The average duration between trauma and surgery was 1.82 days (range 0–13). The patient with 13 days duration could not be operated upon earlier due to underlying medical conditions. Table 1 shows the results for operating room (OR) time, blood loss, X-ray time and duration of hospital stay. VAS for pain at discharge was 4.1 (range 0–8.1) and at the latest follow-up it was 1.3 (range 0–7.4) (Fig. 1). VAS for mobility at discharge was 1.9 (range 0–9.3) and at the latest follow-up 7.6 (range 1–10) (Fig. 2). The preoperative overall iADL score was 2.92 (range 0.14–3.00). For the open procedure, it was 2.96 (range 1.25–3.00), and for MI it was 2.86 (range 0.14–3.00) (p = 0.22). At the latest follow-up, overall iADL score was 2.10 (range 0–3.00). For the open procedure, it was 2.15 (range 0–3.00), and for MI it was 2.04 (range 0.25–3.00) (p = 0.47). The preoperative iADL was higher versus the latest follow-up for both groups (open and MI) (p < 0.001).
Table 1.
OR (operating room) time, X-ray (XR) time, blood loss and hospital stay (MI minimally invasive, *p < 0.05, **p < 0.01, ***p < 0.001)
| Procedure | OR time (minutes) | XR time (minutes) | Blood loss (ml) | Hospital stay (days) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | Range | Mean | Range | Mean | Range | Mean | Range | |
| MI | 61.2 | 30–150 | 1.66 | 0.3–4.5 | 100 | 30–300 | 7.4 | 2–45 |
| Open | 85.5 | 34–170 | 1.79 | 0.3–4.6 | 195 | 30–1000 | 8.4 | 2–26 |
| All | 75.7*** | 30–170 | 1.72 | 0.3–4.6 | 157*** | 30–1000 | 8.0* | 2–45 |
Fig. 1.
Visual analogue scale (VAS) for pain at discharge and at latest follow-up
Fig. 2.
Visual analogue scale (VAS) for mobility at discharge and at latest follow-up
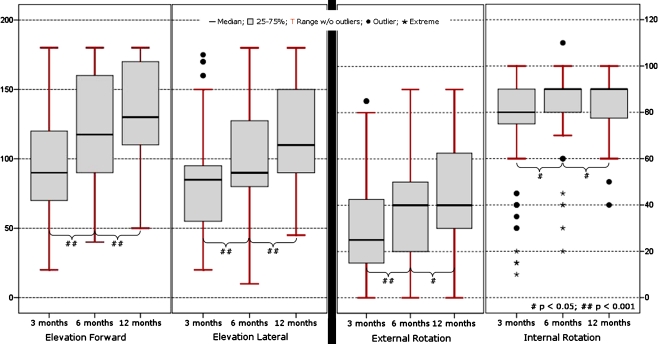
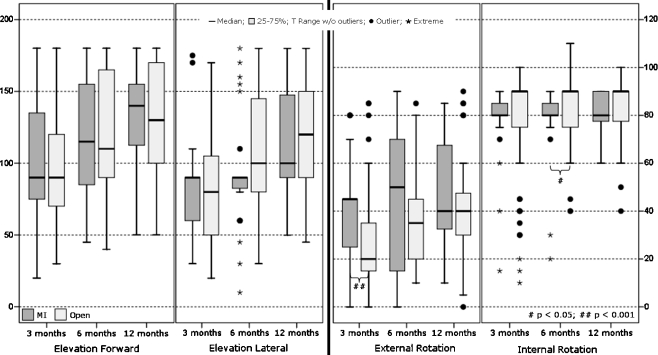
The results for ROM are shown in Fig. 3. The improvement during follow-up (three months versus six months, and six months versus twelve months) for moving in all directions was statistically significant (p < 0.05). Statistically significant differences between the two groups were seen preoperatively (elevation forward p < 0.05, external p < 0.001 and internal rotation p < 0.001), at six weeks (external rotation p < 0.01), three months (external rotation p < 0.001) and six months (internal rotation p < 0.01). The differences between open and MI at the 12-month follow-up were not statistically significant (Fig. 4).
Fig. 3.
Box plots for the four directions of range of motion (ROM)
Fig. 4.
Box plots comparing the range of motion (ROM) for both groups during follow-up (MI minimally invasive)
X-ray showed uneventful healing of the fracture after three months in 60 cases (57%), after six months in 88 cases (83%), and after 12 months in 103 cases (97%) (Fig. 5). The remaining fractures (n = 3) had not healed after 12 months and showed delayed (n = 2) or non-union (n = 1). In the one missing case, the patient had refused to undergo X-ray during follow-up several times. With regard to the technique, 52% of the open and 61% of the MI fractures had healed uneventfully after three months. After six months this was 79% (open) and 87% (MI), and after 12 months 97% (open) and 96% (MI).
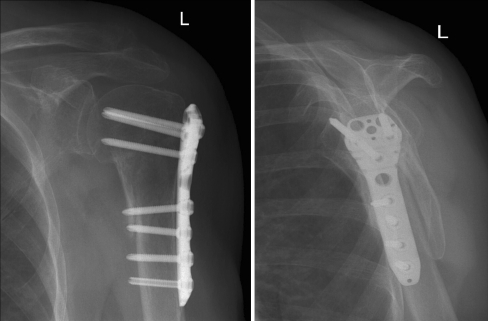
Fig. 5.
a, b X-ray of an AO 11-A2 fracture treated minimally invasively at 12 months
Complications
Complications were categorised into implant related (intra-articular screw perforation, proximal screw loosening, distal screw pull out and implant breakage) and “general” (secondary displacement, avascular necrosis [AVN], infection, frozen shoulder, impingement, non-union, delayed-union). The most frequent implant related complication was intra-articular screw perforation in 19 cases (15%; 10 open, 9 MI). The most frequent general complication was secondary displacement in ten cases (8%; 9 open, 1 MI). The implant related complication rate was 17% (open 15%, MI 19%), and the general complication rate was 21% (open 26%, MI 15%). Thirty-five patients (20 open, 15 MI ) were revised (27%; 26% open, 28% MI). In the MI group no clinical signs of axillary nerve lesion were detected. No case of implant breakage occurred. Table 2 shows a detailed description of the complications within this study. Analysing the fracture type (AO) as a risk factor, statistical significance could be shown (p < 0.001) (Table 3). Hence, the highest complication rate was seen for C-type fractures. Analysing age as a risk factor, there was a trend towards a higher complication rate with increasing age; however, it was not significant.
Table 2.
Description of complications
| Complications | Surgical technique | Complications within group (n) | Complication riska (%) | AO classification (number of cases and rateb) | Revisions including early removal of plate (% of overall patients within group) | ||
|---|---|---|---|---|---|---|---|
| A | B | C | |||||
| Implant related complications | MI | 10 | 18.9% | 2 (17%) | 2 (8%) | 6 (40%) | 8 (15%) |
| Open | 12 | 15.4% | 2 (11%) | 3 (11%) | 7 (22%) | 6 (8%) | |
| All | 22 | 16.8% | 4 (13%) | 5 (9%) | 13 (28%) | 14 (11%) | |
| Intra-articular screw perforation | MI | 9 | 17.0% | 2 | 1 | 6 | 7 |
| Open | 10 | 12.8% | 2 | 2 | 6 | 5 | |
| All | 19 | 14.5% | 4 | 3 | 12 | 12 | |
| Proximal screw loosening | MI | 1 | 1.9% | 0 | 1 | 0 | 1 |
| Open | 1 | 1.3% | 0 | 0 | 1 | 1 | |
| All | 2 | 1.5% | 0 | 1 | 1 | 2 | |
| Distal screw pull-out | MI | 0 | 0% | 0 | 0 | 0 | 0 |
| Open | 1 | 1.3% | 0 | 1 | 0 | 0 | |
| All | 1 | 0.8% | 0 | 1 | 0 | 0 | |
| Implant breakage | All | 0 | 0% | 0 | 0 | 0 | 0 |
| General complications | MI | 8 | 15.1% | 2 (17%) | 3 (12%) | 3 (20%) | 7 (13%) |
| Open | 20 | 25.6% | 3 (17%) | 3 (11%) | 14 (44%) | 14 (18%) | |
| All | 28 | 21.4% | 5 (17%) | 6 (11%) | 17 (36%) | 21 (16%) | |
| Secondary dislocation | MI | 1 | 1.9% | 0 | 0 | 1 | 1 |
| Open | 9 | 11.5% | 1 | 0 | 8 | 7 | |
| All | 10 | 7.6% | 1 | 0 | 9 | 8 | |
| AVN | MI | 3 | 5.7% | 1 | 0 | 2 | 3 |
| Open | 3 | 3.8% | 0 | 1 | 2 | 1 | |
| All | 6 | 4.6% | 1 | 1 | 4 | 4 | |
| Infection | MI | 2 | 3.8% | 0 | 2 | 0 | 2 |
| Open | 2 | 2.6% | 0 | 1 | 1 | 2 | |
| All | 4 | 3.1% | 0 | 3 | 1 | 4 | |
| Frozen shoulder | MI | 0 | 0% | 0 | 0 | 0 | 0 |
| Open | 3 | 3.8% | 0 | 1 | 2 | 3 | |
| All | 3 | 2.3% | 0 | 1 | 2 | 3 | |
| Impingement | MI | 1 | 1.9% | 0 | 1 | 0 | 1 |
| Open | 1 | 1.3% | 1 | 0 | 0 | 1 | |
| All | 2 | 1.5% | 1 | 1 | 0 | 2 | |
| Non-union | MI | 0 | 0% | 0 | 0 | 0 | 0 |
| Open | 1 | 1.3% | 1 | 0 | 0 | (1 planned) | |
| All | 1 | 0.8% | 1 | 0 | 0 | (1 planned) | |
| Delayed union | MI | 1 | 1.9% | 1 | 0 | 0 | 0 |
| Open | 1 | 1.3% | 0 | 0 | 1 | 0 | |
| All | 2 | 1.5% | 1 | 0 | 1 | 0 | |
| Total | MI | 18 (17 patients) | 32.1% | 4 (33%) | 5 (19%) | 9 (60%) | 15 (28%) |
| Open | 32 (30 patients) | 38.5% | 5 (28%) | 6 (21%) | 21 (66%) | 20 (26%) | |
| All | 50 (47 patients) | 35.9% | 9 (30%) | 11 (20%) | 30 (64%) | 35 (27%) | |
MI minimally invasive, AVN avascular necrosis
a Risk for patient to experience complication(s)
b Number of complications/patient
Table 3.
Cumulative incidences for experiencing at least one complication per fracture type
| Fracture type | Number of fractures at risk | Number of fractures with at least one complication related to a particular cause | Risk (%) | 95% CIa | pb |
|---|---|---|---|---|---|
| All fractures | <0.001 | ||||
| A | 30 | 9 | 30.0 | 12.6–47.4 | |
| B | 54 | 11 | 20.4 | 9.3–31.5 | |
| C | 47 | 27 | 57.4 | 42.8–72.1 | |
| MI | 0.08 (n.s.) | ||||
| A | 12 | 4 | 33.3 | 2.0–64.6 | |
| B | 26 | 5 | 19.2 | 3.0–35.5 | |
| C | 15 | 8 | 53.3 | 24.7–81.9 | |
| Open | 0.006 | ||||
| A | 18 | 5 | 27.7 | 4.9–50.7 | |
| B | 28 | 6 | 21.4 | 5.2–37.6 | |
| C | 32 | 19 | 59.4 | 41.4–77.4 | |
MI minimally invasive, n.s. not significant
a Confidence intervals for single-sample t-test
Difference among fracture types (Pearson's chi-square, 2-sided)
Implant removal
Implant removal was not performed in general, but only in patients who had clinical problems related to the implant (n = 15) or requested removal of the plate even without clinical problems (n = 15).
Discussion
Surgical treatment of most displaced proximal humerus fractures is challenging due to the fact that stable reduction is hard to achieve in the weak bone stock [2–5]. In the past, with the use of conventional implants, this led to high rates of fixation failure [2, 4, 5]. Implants of the latest generation use locking screws and act as internal fixators to create high stability. Many studies reporting results on these devices show good functional results [3, 5, 13, 14]. Only a very limited number of prospective, multicentre studies analysing the outcome of locked plating of proximal humerus fractures have been available until now [15, 22, 23]. In contrast to most of the other recent locking devices for the proximal humerus (PHILOS, LPHP, etc.), the NCB-PH combines secondary locking, polyaxial screw placement, and allows both open and MI technique with the same device [17–19].
This study shows that the MI technique required less OR time, caused less blood loss and a slightly shorter hospital stay. No difference could be detected for the X-ray time. The latter excludes a possible disadvantage of the MI technique, i.e. more X-ray exposure due to limited anatomical exposure and percutaneous fracture reduction. The functional outcome in our study was comparable to other recent studies [23, 24]. Full function was not regained at one-year follow-up compared to the healthy side (data not shown), which is in accordance with the literature. The technique (open/MI) had only inconsistently significant ROM or no significant influence on the functional results. Patients of the MI group reported more pain but better mobility (VAS). An explanation might be that patients of the MI group were more aggressively exposed to physical therapy because soft tissues were not that much of a limiting factor due to the limited incision. However, the main determinant for choosing the postoperative rehabilitation scheme should be the fracture pattern and the quality of reduction.
The complication rate in our study is comparable to the literature, where the most recent studies report complication rates between 32 and 50% [13, 22–26]. These results suggest that locking plates have not, as yet, turned out to be a panacea for the treatment of these osteoporotic fractures, though most studies show that they are a true benefit. This is supported by the results of our study, i.e. secondary displacement and intraarticular screw perforation being the most frequent complications detected. The severity of fracture (AO) turned out to be the most important predictive factor for the incidence of complications. This was also the case when analysing the two subgroups: open and MI. The higher overall complication rate within the open group can be explained by the fact that more C-type fractures were treated with the open technique. In summary, none of the two techniques should be labelled “better” or “worse”, but it is rather a question of the correct indication. Based on our experience we recommend that complex fractures (three to four parts) with no medial support of the head fragment are best treated with the open technique, as the reconstruction of the medial metaphyisis seems particularly difficult with percutaneous techniques.
There are some limiting factors in our study. First, no randomisation between the open and MI techniques was performed, which is critical. However, comparable studies have recently been published [16]. The follow-up period is too short to obtain more definitive results and the study protocol did not provide a standard procedure for the postoperative treatment protocol, which may impact functional outcome and complication rate.
Conclusion
In this multicentre study a second generation locking device was shown to be a suitable method for the routine treatment of proximal humerus fractures. Complication rate and functional outcome are comparable to those in the literature. The system used allows both the open and minimally invasive (MI) techniques. In complex fracture patterns, where anatomical reduction is unlikely to be achieved by percutaneous reduction, a thorough preoperative diagnostic workup should identify those fractures, which must be treated with the open surgical technique.
Acknowledgments
Conflict of interest The institutions received financial reimbursement from Zimmer, Inc. for conducting this follow-up. None of the authors received financial reimbursement or anything of value for conducting this follow-up. The first and fourth authors are instructional lecturers for Trauma Courses by the Zimmer Institute.
References
- 1.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 2.Helmy N, Hintermann B. New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res. 2006;442:100–108. doi: 10.1097/01.blo.0000194674.56764.c0. [DOI] [PubMed] [Google Scholar]
- 3.Lill H, Hepp P, Rose T, et al. The angle stable locking-proximal-humerus-plate (LPHP®) for proximal humeral fractures using a small anterior-lateral-deltoid-splitting-approach—technique and first results. Zentralbl Chir. 2004;129:43–48. doi: 10.1055/s-2004-44870. [DOI] [PubMed] [Google Scholar]
- 4.Lill H, Josten C (2001) Conservative or operative treatment of humeral head fractures in the elderly? Chirurg 72:1224–1234 (in German) [DOI] [PubMed]
- 5.Plecko M, Kraus A. Internal fixation of proximal humerus fractures using the locking proximal humerus plate. Oper Orthop Traumatol. 2005;17:25–50. doi: 10.1007/s00064-005-1120-8. [DOI] [PubMed] [Google Scholar]
- 6.Wijgman AJ, Roolker W, Patt TW, et al. Open reduction and internal fixation of three and four-part fractures of the proximal part of the humerus. J Bone Jt Surg. 2002;84-A(11):1919–1925. [PubMed] [Google Scholar]
- 7.Kwon BK, Goertzen DJ, O’Brien PJ, et al. Biomechanical evaluation of proximal humeral fracture fixation supplemented with calcium phosphate cement. J Bone Jt Surg. 2002;84-A:951–961. doi: 10.2106/00004623-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Cofield RH. Comminuted fractures of the proximal humerus. Clin Orthop. 1988;230:49–57. [PubMed] [Google Scholar]
- 9.Esser RD. Treatment of three and four part fractures of the proximal humerus with a modified cloverleaf plate. J Orthop Trauma. 1994;8:15–22. doi: 10.1097/00005131-199402000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Chudik SC, Weinhold P, Dahners LE. Fixed-angle plate fixation in simulated fractures of the proximal humerus: a biomechanical study of a new device. J Shoulder Elbow Surg. 2003;12(6):578–588. doi: 10.1016/S1058-2746(03)00217-9. [DOI] [PubMed] [Google Scholar]
- 11.Siffri PC, Peindl RD, Coley ER, et al. Biomechanical analysis of blade plate versus locking plate fixation for a proximal humerus fracture: comparison using cadaveric and synthetic humeri. J Orthop Trauma. 2006;20(8):547–554. doi: 10.1097/01.bot.0000244997.52751.58. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein DM, Bratton DR, Ciccone WJ, et al. Locking plate improves torsional resistance in the stabilization of three part proximal humeral fractures. J Shoulder Elbow Surg. 2006;15(2):239–243. doi: 10.1016/j.jse.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Agueldo J, Schürmann M, Stahel P, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plate. J Orthop Trauma. 2007;21(10):676–681. doi: 10.1097/BOT.0b013e31815bb09d. [DOI] [PubMed] [Google Scholar]
- 14.Frankenhauser F, Boldin C, Schnippinger G, et al. A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res. 2005;430:176–181. doi: 10.1097/01.blo.0000137554.91189.a9. [DOI] [PubMed] [Google Scholar]
- 15.Laflamme GY, Rouleau DM, Berry GK, et al. Percutaneous humeral plating of fractures of the proximal humerus: results of a prospective multicenter clinical trial. J Orthop Trauma. 2008;22(3):153–158. doi: 10.1097/BOT.0b013e3181694f7d. [DOI] [PubMed] [Google Scholar]
- 16.Hepp P, Theopold J, Voigt C, et al. The surgical approach for locking plate osteosynthesis of displaced proximal humeral fractures influences the functional influences the outcome. J Shoulder Elbow Surg. 2008;17(1):21–28. doi: 10.1016/j.jse.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 17.Röderer G, Gebhard F, Erhardt J, et al. The non-contact bridging plate: a new fixed angle device for the minimally-invasive treatment of fractures of the proximal humerus—technique and preliminary results. Unfallchirurg. 2007;110(6):505–512. doi: 10.1007/s00113-006-1227-x. [DOI] [PubMed] [Google Scholar]
- 18.Röderer G, Abouelsoud M, Gebhard F, et al. Minimally-invasive application of the non-contact bridging plate to the proximal humerus. An anatomical study. J Orthop Trauma. 2007;21(9):621–627. doi: 10.1097/BOT.0b013e318157f0cd. [DOI] [PubMed] [Google Scholar]
- 19.Erhardt JB, Röderer G, Grob K, et al. Early results in the treatment of proximal humeral fractures with a polyaxial locking plate. Arch Orthop Trauma Surg. 2009;129(10):1367–1374. doi: 10.1007/s00402-009-0924-7. [DOI] [PubMed] [Google Scholar]
- 20.Resch H, Hübner C, Schwaiger R. Minimally invasive reduction and osteosynthesis of articular fractures of the humeral head. Int J Integr Care. 2001;32S-A:25–32. doi: 10.1016/s0020-1383(01)00058-4. [DOI] [PubMed] [Google Scholar]
- 21.Neer CS., 2nd Four-segment classification of proximal humeral fractures: purpose and reliable use. J Shoulder Elbow Surg. 2002;11:389–400. doi: 10.1067/mse.2002.124346. [DOI] [PubMed] [Google Scholar]
- 22.Müller ME, Nazarin S, Koch P. Classification AO des fractures: les os logs. Berlin Heidelberg New York: Springer Verlag; 1987. [Google Scholar]
- 23.Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23(3):163–172. doi: 10.1097/BOT.0b013e3181920e5b. [DOI] [PubMed] [Google Scholar]
- 24.Südkamp N, Bayer J, Hepp P, et al. Open reduction and internal fixation of proximal humeral fractures with the use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Jt Surg. 2009;91-A(6):1320–1328. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 25.Solberg BD, Moon CN, Franco DP, et al. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg. 2009;91-A(7):1689–1697. doi: 10.2106/JBJS.H.00133. [DOI] [PubMed] [Google Scholar]
- 26.Bahrs C, Badke A, Rolauffs B et al (2009) Long-term results after non-plate head-preserving fixation of proximal humeral fractures. Int Orthop. doi:10.1007/s00264-009-0848-4 [DOI] [PMC free article] [PubMed]