Abstract
Controversies existing over resurfacing the patella in total knee arthroplasty remain in the literature. The purpose of this review was to evaluate the effectiveness of resurfacing versus nonresurfacing the patella in total knee arthroplasty. We searched the Cochrane Library, MEDLINE and EMBASE for published randomised clinical trials relevant to patellar resurfacing. The relative risk of reoperation was significantly lower for the patellar resurfacing group than for the nonresurfacing group (relative risk 0.57, 95% confidence interval 0.38–0.84, P = 0.004). The overall incidence of postoperative anterior knee pain of the 1,421 knees included was 12.9% in the patellar resurfacing group and 24.1% in the nonresurfacing group. The existing evidence indicates that patellar resurfacing can reduce the risk of reoperation with no improvement in postoperative knee function or patient satisfaction over total knee arthroplasty without patellar resurfacing. Whether it can decrease the incidence of anterior knee pain remains uncertain.
Introduction
That it is controversial to resurface the patella in total knee arthroplasty (TKA) remains as a topic in the literature because of the higher incidence of anterior knee pain after TKA without patellar resurfacing [1, 2], which was reported to be between 5 and 47% of patients [3–7], and the general idea that the aetiology of anterior knee pain is related to the patellofemoral joint. Some authors recommend routinely resurfacing the patella [7–11], while others have reported no evidence to support routine patellar resurfacing. The patella complications were found more often in the resurfaced group than in the group without resurfacing [12–16]. Further authors suggested a selective decision based on factors such as the patella thickness, the presence of preoperative anterior knee pain, the severity of degenerative changes in the patella or rheumatoid arthritis and the experience of the surgeon [17–19].
Randomised controlled trials (RCT) represent the best study design to compare patellar resurfacing with patellar nonresurfacing. However, no consistent results had been provided in these published randomised trials. Four meta-analyses published over the past few years [21–23] failed to show clear superiority of patellar resurfacing or nonresurfacing, and the relatively small cumulative sample and more short-term follow-up RCTs included make it very difficult to draw a firm conclusion. Thus, whether to resurface the patella routinely is still uncertain. The purpose of this review was to compare the effectiveness of patellar resurfacing versus nonresurfacing in TKA, with a view to provide information for physicians in making a decision. The null hypothesis was that there was no difference in terms of clinical outcomes and patient satisfaction between patellar resurfacing and nonresurfacing after TKA.
Materials and methods
Criteria for considering studies for this review
All randomised controlled trials comparing patellar resurfacing with patellar nonresurfacing in TKA were eligible. Studies of bilateral total knee arthroplasties in which the patella was resurfaced in one knee and not in the other when the allocation of the two techniques to the operated knees was randomised were also included. All nonrandomised trials and quasi-randomised trials were excluded. The participants were limited to adults who were undergoing primary total knee replacement for osteoarthritis or rheumatoid arthritis. Any kind of prosthesis was considered for this review.
Search methods for identification of studies
We searched the Cochrane Central Register of Controlled Trials (in the Cochrane Library issue 2, 2009), MEDLINE (from 1970 to January 2009) and EMBASE (from 1970 to January 2009) for eligible trials. We also searched the review articles and bibliographies of other relevant studies to identify additional studies. We applied no language restriction and did not include data from review articles, case reports, abstracts or unpublished studies.
Outcome measures
The primary interests were the rate of reoperation for any reason and the incidence of anterior knee pain. According to the reasons for reoperation whether or not they were related to the patellofemoral joint, we further divided reoperation into two categories. One was reoperation related to the patellofemoral joint, including secondary resurfacing, revision surgery for patella component loosening, later additional procedures on the extensor mechanism and revision surgery for patella fracture and the other was reoperation unrelated to the patellofemoral joint, including revision surgery for tibiofemoral component loosening, infection or removal of loose bodies, internal fixation for tibial or femoral fracture and arthroscopic synovectomy. We also categorised primary outcomes as short term (under five years) and mid- to long term (over five years) for subgroup analysis. The secondary outcomes of interest were patient satisfaction and symptom and function scores such as the Knee Society score, the Hospital for Special Surgery score and the Bristol knee score.
Data extraction
Two review authors (Li SZ and Luo XP) independently extracted data of the outcomes using pre-designed standardised data abstraction forms without concealing the journal name and author details. Controversy was resolved by discussion. Reasons for excluding studies were recorded. Whenever studies belonged to the same patients at different follow-up periods, we respectively extracted the data for subgroup analysis comparing short-term with mid- to long-term follow-up trials, and selected the one with the longer duration of follow-up for the main analysis in order to avoid duplication of information. When the available published information was not adequate for the analysis, we communicated personally with the authors for additional information.
Quality assessment
The methodological quality of included trials was evaluated independently by the reviewers (Chen YP and Su W), using a specific tool for assessing risk of bias recommended by the Cochrane Collaboration to assess methodological quality of clinical trials. This comprises a description and judgment for each entry in a “risk of bias” table, where each entry addresses a specific feature of the study. The judgment for each entry involves answering a question, with answers “yes” indicating low risk of bias, “no” indicating high risk of bias and “unclear” indicating either lack of information or uncertainty over the potential for bias [24].
Data synthesis and analysis
The knee was the unit of the analysis. For each study, relative risks (RR) and 95% confidence intervals (CI) were calculated for dichotomous outcomes, and mean differences and 95% CI were calculated for continuous outcomes [25]. We also calculated the number of knees that needed to be treated to prevent a reoperation or postoperative anterior knee pain. When no heterogeneity existed among studies, fixed-effect [26] models were used to estimate the overall summary effect sizes, and if large between-study heterogeneity existed, random-effects [27] models were used. When necessary, the results of comparable groups of trials were pooled using both the fixed-effect and random-effects models. We tested heterogeneity between comparable trials using a chi-square test and considered P < 0.10 to be statistically significant [26], and quantified its extent with the I² statistic [28].
We pre-specified characteristics in the protocol for later subgroup analyses in order to explore the between-study heterogeneity and to identify subgroup-specific differences in the effect of the intervention. The reoperation rate among patients undergoing patellar resurfacing versus nonresurfacing after TKA has been reported differently by various authors. In our review we defined the rate of reoperation as our primary outcome. However, because the category of reoperation mixed any operation for any reason and the confounders could affect the comparison of revision of the patellofemoral joint between patellar resurfacing and patellar nonresurfacing. We further divided reoperation into two categories for subgroup analysis [29]. Boyd et al. [7] reported that most complications occurred after the third or fourth year postoperatively, and based on this factor we categorised primary outcomes as short term (under five years) or mid- to long term(over five years) for subgroup analysis. Because different prostheses used in different trials may produce clinical heterogeneity, subgroup analysis may be conducted if observed substantive between-study heterogeneity exists in one outcome. Sensitivity analyses were performed to test the reliability of pooled results, and the results of sensitivity analyses were reported in a summary table. All analyses were done with RevMan5.0 software and the level of significance was set at P < 0.05. Funnel plots were used for detecting reporting bias in meta-analyses [30].
Results
Description of studies
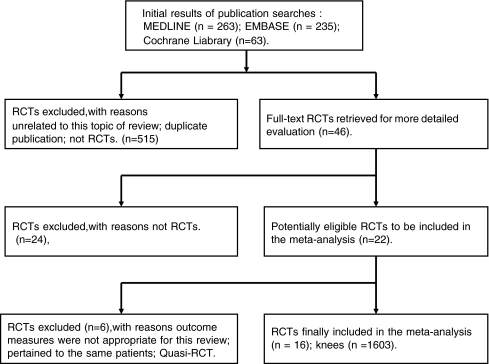
Studies from initial results of publication searches to final inclusion or exclusion are displayed in the flow chart (Fig. 1). A total of 14 trials (16 articles) were included in this review [9, 31–45]. There were 1,603 knees included in the 14 studies: 817 knees in the nonresurfaced group and 786 knees in the resurfaced group. The duration of follow-up ranged from one to ten years. The 14 included studies were published between 1990 and 2008: 12 in English, 1 in German [42] and 1 in Chinese [40]. Ten different prostheses were used. All included trials had compared the baseline preoperatively, and each had a similar baseline. More characteristics of the included studies are shown in Table 1. Of the 16 included trials, there are 12 studies with adequate random sequence generation and nine studies with adequate concealment of allocation [31–33, 35–38, 43–45]. Eight studies used at least observer blinding [9, 32–38, 40, 44]. The methods used to generate random sequence in the included trials were as follows: random number tables [9, 31, 36], computer-generated random numbers [37, 38, 42], randomised envelope [31–35, 43, 44], coin tossing [40, 42] and not reported [39, 41]. The methodological quality of the included trials can be seen in Table 2.
Fig. 1.
Flow chart of searches
Table 1.
Characteristics of included studies
| Author and publication date | Enrollment period | Indication | Number of knees enrolled | Number of knees analysed | Mean age (years) | Mean weight (kg) | Type of implant | Duration of follow-up (years) | Missing outcome data | Intention to treat analysis |
|---|---|---|---|---|---|---|---|---|---|---|
| PR/PN | PR/PN | PR/PN | PR/PN | |||||||
| Partio and Wirta (1995) | 1991–1992 | OA, RA | 100 (50/50) | 95 (47/48) | 67.5 | NR | PFC | 2.5 | 5 (5%) | No |
| Bourne et al. (1995)a | NR | OA | 100 (50/50) | 100 (50/50) | 72/68 | 84/86 | AMK | 2 | 0 (0%) | No |
| Feller et al. (1996) | 1990–1991 | OA | 40 (20/20) | 38 (19/19) | 70.5/71.1 | 86.1/78.6 | PCA | 3 | 2 (5%) | No |
| Kajino et al. (1997) | NR | RA | 70 (35/35) | 52 (26/26) | 56.1 | NR | YC | 6.5 | 18 (26%) | No |
| Barrack et al. (1997)b | 1992–1993 | OA | 121 | 118 (58/60) | 65.3/67.1 | NR | M-GII | 2.5 | 4 (3%) | Yes |
| Schroeder-Boersch et al. (1998) | NR | OA | 40 (20/20) | 40 (20/20) | 70.3/72.2 | 73.8/73.7 | Duracon | 24 | 0 (0%) | No |
| Barrack et al. (2001)b | 1992–1993 | OA | 121 | 93 (47/46) | 65.3/67.1 | NR | M-GII | 5.8 | 28 (23%) | Yes |
| Newman et al. (2000) | 1990–1992 | OA | 84 (42/42) | 71 (37/34) | 72. 0/71. 2 | 77. 3/74. 6 | Kinematic | 5 | 13 (15%) | No |
| Wood et al. (2002) | 1992–1996 | OA | 240 (106/13) | 220 (92/128) | 73.7/73.7 | 78.5/79.8 | M-GII | 4 | 41 (17%) | Yes |
| Waters and Bentley (2003) | 1992–NR | OA, RA | 514 | 474 (243./231) | 69.1/69.1 | 76.7/78.9 | PFC | 5.3 | 62 (12%) | Yes |
| Kordelle et al. (2003) | 1999–2000 | OA | 50 (25/25) | 50 (25/25) | NR | NR | NR | 1 | NR | NR |
| Gildone et al. (2005) | NR | OA | 56 (28/28) | 56 (28/28) | 74.6/73.6 | NR | NexGen | 2 | 0 (0%) | No |
| Burnett et al. (2004)a | 1991-NR | OA | 100 (50/50) | 90 (42/48) | 71/69 | 88/88 | AMK | 10 | 36 (36%) | Yes |
| Campbell et al. (2006) | 1991–1993 | OA | 100 (46/54) | 58 (30/28) | 71/73 | 88.4/77.5 | M-GII | 10 | 42 (42%) | No |
| Smith et al. (2008) | 1998–2002 | OA | 181 | 159 (73/86) | 71.9/71.2 | 86.1/82.2 | Profix | 4.3 | 22 (12%) | No |
| Huang et al. (2007) | 2000–2001 | OA | 117 | 107 (57/50) | 68.1/66.5 | NR | AMK | 2 | 10 (8%) | No |
PR patellar resurfacing, PN patellar nonresurfacing, OA osteoarthritis, RA rheumatoid arthritis, NR not reported, PFC Press-Fit Condylar prosthesis, AMK Anatomic Medullary Knee prosthesis, PCA PCA Modular prosthesis, YC Yoshino-Shoji total knee prosthesis, M-GII Miller-Galante II prosthesis
aBourne et al. [34] and Burnett et al. [35] reported the results of the same patients in different follow-up times
bBarrack et al. [32] and Barrack et al. [33] reported the results of the same patients in different follow-up times
Table 2.
Assessments of risk of bias in included studies
| Included studies | Adequate sequence generation?a | Allocation concealmentb | Blinding?c | Incomplete outcome data addressed?d | Free of selective reporting?e | Free of other bias?f |
|---|---|---|---|---|---|---|
| Partio and Wirta (1995) | Unclear | Unclear | Unclear | Yes | Yes | Unclear |
| Bourne et al. (1995) | Unclear | Unclear | Yes | Yes | Yes | Yes |
| Feller et al. (1996) | Yes | Yes | Unclear | Yes | Unclear | Yes |
| Kajino et al. (1997) | Yes | Yes | Yes | Unclear | Yes | Yes |
| Barrack et al. (1997) | Yes | Yes | Yes | Yes | Yes | Yes |
| Schroeder-Boersch et al. (1998) | Unclear | Unclear | Unclear | Yes | Unclear | Unclear |
| Barrack et al. (2001) | Yes | Yes | Yes | No | Yes | Yes |
| Newman et al. (2000) | Yes | Yes | Unclear | Yes | Yes | Yes |
| Wood et al. (2002) | Yes | Yes | Yes | Unclear | Yes | Yes |
| Waters and Bentley (2003) | Yes | Unclear | Yes | Unclear | Yes | Yes |
| Kordelle et al. (2003) | Yes | Unclear | Unclear | Unclear | Unclear | Unclear |
| Burnett et al. (2004) | Yes | Yes | Yes | Unclear | Yes | Yes |
| Gildone et al. (2005) | Yes | Yes | Unclear | Yes | Yes | Yes |
| Campbell et al. (2006) | Yes | Yes | Yes | No | Yes | Yes |
| Huang et al. (2007) | Yes | Unclear | Yes | Unclear | Yes | Unclear |
| Smith et al. (2008) | Yes | Yes | Yes | Yes | Yes | Yes |
aWas the allocation sequence adequately generated?
bWas allocation adequately concealed?
cWas knowledge of the allocated interventions adequately prevented during the study?
dWere incomplete outcome data adequately addressed?
eAre reports of the study free of suggestion of selective outcome reporting?
fWas the study apparently free of other problems that could put it at a risk of bias?
Note: quoted from Cochrane handbook for systematic reviews for intervention. Version 5.0.0:191-195
Meta-analysis results
Reoperation
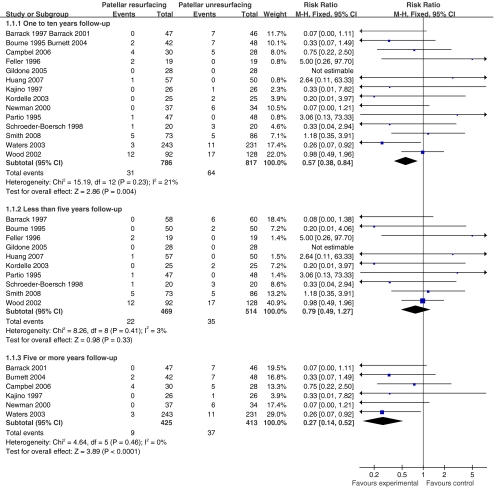
All included studies reported the results of reoperation. The results of a total of 1,603 knees showed a rate of reoperation for any reason in 31 of 786 (3.9%) knees in the resurfaced group and 64 of 817 (7.8%) knees in the nonresurfaced group during the period of one to ten years follow-up. When fixed-effects meta-analysis was used, the RR of reoperation for any reason was 0.57 (95% CI 0.38–0.84, P = 0.004), but when random-effects analysis was substituted, RR was 0.60 (95% CI 0.35–1.03, P = 0.06), indicating such results were unreliable. Sensitivity analysis showed similar summary effects. In subgroup analysis, either the RR or the risk differences (RD) showed no significant difference between the compared groups when we examined trials in which patients had been followed for less than five years (RR = 0.79, 95% CI 0.49–1.27, fixed-effects analysis; RD = −0.01, 95% CI −0.04 to 0.02, random-effects analysis). However, the pooled results of trials in which patients had been followed up for more than five years showed a significant difference between the compared groups. The RR in the patellar resurfacing arm was 0.27 times (95% CI 0.14–0.52, fixed-effects analysis) lower than that of the patellar nonresurfacing arm. The absolute risk was reduced by 0.08 (95% CI 0.14–0.02, random-effects analysis) in the resurfacing arm, indicating that one would need to resurface 13 patellae (95% CI 7–50) to avoid one reoperation. The rate of reoperation related to the patellofemoral joint calculated from 14 studies was 1.8% in the patellar resurfacing group and 6.2% in the patellar nonresurfacing group. The RR for reoperation related to the patellofemoral joint was 0.37 (95% CI 0.22–0.61, P = 0.0001, fixed-effects analysis), with no heterogeneity, implying there was a significant difference between the two groups. However, the RD was 0.03 in the summary effects and the number needed to treat (NNT) was 33, meaning that in order to prevent one case of reoperation related to the patellofemoral joint one would need to resurface 33 patellae. The summary effects indicated there was no significant difference between the resurfaced and the unresurfaced groups in terms of the rate of reoperation unrelated to the patellofemoral joint (RR = 1.33, 95% CI 0.68–2.63, P = 0.41, fixed-effects analysis) (Tables 3 and 4, Fig. 2).
Table 3.
Summary of findings
| Outcome or subgroup | Studies | Participants | Test for heterogeneity | Statistical method | Effect estimate | P value | |
|---|---|---|---|---|---|---|---|
| Reoperation | 1–10 years follow-up | 14 | 1,603 | P = 0.23, I² = 21% | RR (M-H, fixed, 95% CI) | 0.57 (0.38, 0.84) | 0.004 |
| Less than 5 years follow-up | 10 | 983 | P = 0.41, I² = 3% | RR (M-H, fixed, 95% CI) | 0.79 (0.49, 1.27) | 0.33 | |
| 5 or more years follow-up | 6 | 838 | P = 0.46, I² = 0% | RR (M-H, fixed, 95% CI) | 0.27 (0.14, 0.52) | 0.0001 | |
| Reoperations related to the PFJ | 14 | 1,603 | P = 0.59, I² = 0% | RR (M-H, fixed, 95% CI) | 0.37 (0.22, 0.61) | 0.0001 | |
| Reoperations unrelated to the PFJ | 14 | 1,603 | P = 0.72, I² = 0% | RR (M-H, fixed, 95% CI) | 1.33 (0.68, 2.63) | 0.41 | |
| Postoperative anterior knee pain | 1–10 years follow-up | 10 | 1,421 | P = 0.00001, I² = 80% | RR (M-H, random, 95% CI) | 0.60 (0.32, 1.11) | 0.10 |
| Less than 5 years follow-up | 7 | 853 | P = 0.01, I² =63% | RR (M-H, random, 95% CI) | 0.55 (0.26, 1.15) | 0.11 | |
| 5 or more years follow-up | 5 | 786 | P = 0.00001, I² = 87% | RR (M-H, random, 95% CI) | 0.60 (0.23, 1.59) | 0.30 | |
| Knee Society score | Knee score | 4 | 621 | P = 0.30, I² = 17% | MD (IV, random, 95% CI) | 1.90 (−0.37, 4.18) | 0.10 |
| Functional score | 4 | 621 | P = 0.86, I² = 0% | MD (IV, random, 95% CI) | 2.58 (−0.96, 6.12) | 0.15 | |
| Patient satisfaction | 8 | 1,102 | P = 0.11, I² = 43% | RR (M-H, random, 95% CI) | 0.99 (0.93, 1.05) | 0.63 | |
PFJ patellofemoral joint, MD mean difference
Table 4.
Comparison of adverse events rate between the patellar resurfacing group and no resurfacing group after TKA
| Outcomes | Groups | Number of events | Number of knees analysed | Rate (%) | |
|---|---|---|---|---|---|
| Reoperation | 1–10 years follow-up | PR | 31 | 786 | 3.9 |
| PN | 64 | 817 | 7.8 | ||
| Less than 5 years follow-up | PR | 22 | 469 | 4.7 | |
| PN | 35 | 514 | 6.8 | ||
| 5 or more years follow-up | PR | 9 | 425 | 2.1 | |
| PN | 37 | 413 | 9.0 | ||
| Reoperations related to the PFJ | PR | 15 | 786 | 1.8 | |
| PN | 51 | 817 | 6.2 | ||
| Reoperations unrelated to the PFJ | PR | 16 | 786 | 2.0 | |
| PN | 13 | 817 | 1.6 | ||
| Postoperative anterior knee pain | 1–10 years follow-up | PR | 90 | 695 | 12.9 |
| PN | 175 | 726 | 24.1 | ||
| Less than 5 years follow-up | PR | 45 | 404 | 11.1 | |
| PN | 86 | 449 | 19.2 | ||
| 5 or more years follow-up | PR | 49 | 399 | 12.3 | |
| PN | 99 | 387 | 25.6 | ||
PFJ patellofemoral joint, PR patellar resurfacing, PN patellar nonresurfacing
Fig. 2.
Forest plot of RR with confidence intervals for reoperation for any reason
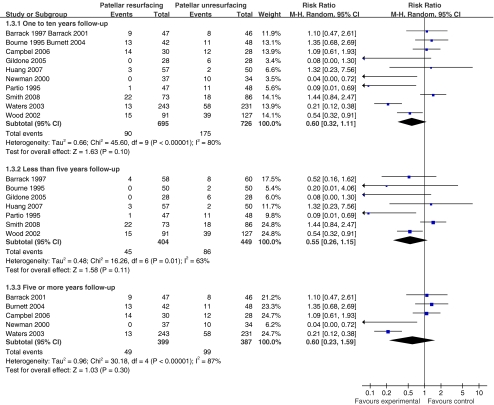
Postoperative anterior knee pain
Ten included studies had reported the results of postoperative anterior knee pain [7, 28–37, 40]; the incidence of postoperative anterior knee pain was 12.9% in the patellar resurfacing group and 24.1% in the patellar nonresurfacing group, and the RR of anterior knee pain was 0.56 (95% CI 0.45–0.70, fixed-effects analysis) with a significant difference (P < 0.00001). However, substantial heterogeneity was detected. We explored the heterogeneity by conducting subgroup analysis, characterised by different lengths of follow-up and different prostheses. Because the heterogeneity existed persistently and it was difficult to determine the causes, we presented the overall effects using random-effects meta-analysis. The RR of anterior knee pain of ten included studies was 0.60 (95% CI 0.32–1.11, P = 0.10, random-effects analysis) with no significant difference between the groups. In subgroup analysis, the RR of anterior knee pain in studies with less than or at least five years follow-up were 0.55 (95% CI 0.26–1.15) and 0.60 (95% CI 0.23–1.59) respectively, showing similar results (Fig. 3). When the analysis was limited to the high quality studies, the methodological quality of which met the criteria that the allocation sequence was generated randomly with adequate concealment and used at least observer blinding, no significant difference was detected among the resurfaced and nonresurfaced groups (RR = 1.03, 95% CI 0.69–1.52, I² = 50%, P = 0.90).
Fig. 3.
Forest plot of RR with confidence intervals for postoperative anterior knee pain
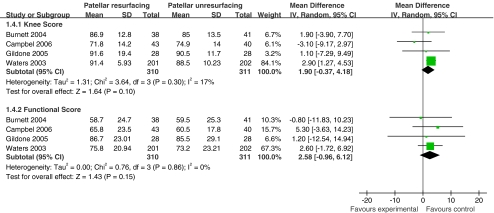
Knee scores
Three kinds of knee rating systems were used to assess the effects of TKA in 13 studies, including the Knee Society score (KSS, divided into knee score and functional score) [9, 32–39, 41, 42], the Bristol knee score [31] and the Hospital for Special Surgery score [40, 44, 45]. Nine studies used the KSS and only four studies provided adequate data for quantitative analyses. The mean difference of the knee score was 2.41 (95% CI 0.92–3.91, P = 0.002) when fixed-effects meta-analysis was used and was 1.9 (95% CI −0.37 to 4.18, P = 0.10) when random-effects meta-analysis was used with little heterogeneity (I² = 17%). The mean difference of the functional score was not significantly different between the groups regardless of whether fixed-effects or random-effects meta-analysis was used with no heterogeneity (I² = 0%). Other studies that cannot be extracted to quantitative analyses were descriptively analysed. Four studies [31, 40, 44, 45] reported that the two groups did not differ significantly with regard to the overall score. Two studies [37, 38] reported that both knee score and functional score were not significantly different between the groups compared, and only two studies [41, 42] reported that the difference between the resurfaced and nonresurfaced groups was significantly in favour of the resurfaced group (Fig. 4).
Fig. 4.
Forest plot of mean differences with confidence intervals for knee scores and functional scores
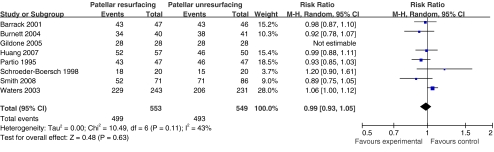
Patient satisfaction
Eight studies reported results of patient satisfaction [9, 32–35, 38–41, 43], but only seven studies were pooled. The summary effects demonstrated that there was no significant difference between the resurfaced and the nonresurfaced groups (RR = 0.99, 95% CI 0.93–1.05, random-effects analysis, P = 0.63). Wood et al. [37] reported the median and the interquartile range of satisfaction and showed no significant difference between the groups compared (P = 0.202) (Fig. 5).
Fig. 5.
Forest plot of mean differences with confidence intervals for patient satisfaction
Discussion
The issue of whether or not to resurface the patella in TKA has been disputed for more than two decades. Many randomised trials have provided inconclusive evidence regarding this problem due to small sample sizes. Therefore, several systematic reviews and meta-analyses have been performed in an attempt to clarify this issue. The meta-analysis by Parvizi et al. [23], which included 14 RCTs and quasi-RCTs, demonstrated that the rate of anterior knee pain (RR = 0.35, 95% CI 0.26–0.48, P < 0.00001, fixed-effects analysis) and patient satisfaction (RR = 0.12, 95% CI 0.07–0.17, P < 0.0001, fixed-effects analysis) significantly favoured patellar resurfacing; they observed no significant difference regarding the rate of reoperation between the patellar resurfacing group and patellar nonresurfacing group. Nizard et al. [21] performed a meta-analysis which pooled 12 RCTs and quasi-RCTs and reported that the RR for reoperation was 0.43 (95% CI 0.27–0.71, P = 0.0008, fixed-effects analysis) and the RR of significant anterior knee pain was 0.39 (95% CI 0.20–0.75, P = 0.005, random-effects analysis) in favour of resurfacing. Forster [20] published a systematic review including three RCTs and reported that the overall rate of reoperation for a patellofemoral problem was 0.7% in the resurfaced group and 12% in the nonresurfaced group (P = 0.003). Study data on clinical knee scores and anterior knee pain could not be analysed together as there was significant heterogeneity. The meta-analysis by Pakos et al. [22], which included ten RCTs, showed that the RR of revision favoured patellar resurfacing (RR = 0.48, 95% CI 0.30–0.75, fixed-effects analysis) and the RR of anterior knee pain favoured patellar resurfacing (RR = 0.40, 95% CI 0.19–0.85, fixed-effects analysis) in five trials. The standard mean differences (SMD) calculated for the knee scores were not significantly different between the compared arms with substantial heterogeneity.
Systematic reviews and meta-analyses are affected not only by the quality of the RCTs they collate but also by the methodology whereby RCTs are selected for inclusion [46]. Because the included RCTs and methods used in meta-analysis were different, the results of the above systematic reviews and meta-analyses were inconsistent. Boyd et al. [7] reported that complications of TKA occurred an average of three years postoperatively in the patellar resurfacing group and an average of four years postoperatively in the patellar nonresurfacing group, and secondary procedures for resurfacing of the patella were performed an average of 63 months after the index procedure. Moreover, some authors reported that the benefit of patellar resurfacing diminished with time [47]. Therefore, if one meta-analysis on this topic included more RCTs with short-term follow-up, the summary effects may not reflect the true effects of treatments. Compared with the above meta-analysis, relatively more RCTs with long-term follow-up had been included in our meta-analysis, which aggregated 838 knees with at least five years follow-up, and this will produce certain results different from those of the former. However, we believe the findings of our meta-analysis can represent the intervention effects in the mid- to long term.
Our meta-analysis of 1,603 randomised knees demonstrated that the rate of reoperation was lower in the patellar resurfacing group than that of the patellar nonresurfacing group. This finding was not significantly different in the subgroup of trials with a duration of follow-up less than five years. Nevertheless, in the subgroup analysis of trials with at least five years follow-up, the RR of reoperation for any reason was reduced by more than 70% and the absolute risk of reoperation was reduced by 8% in TKA with patellar resurfacing. In order to provide a more direct comparison with two treatment effects, we calculated the rate of reoperation related to the patellofemoral joint. The findings showed that the RR of the rate of reoperation related to the patellofemoral joint in the patellar resurfacing group was 0.37 times lower than that of the patellar nonresurfacing group, which means that patellar nonresurfacing in TKA can significantly reduce the rate of reoperation for patellofemoral joint problems. However, despite the large RR estimates, the absolute risk difference was small (3%). The NNT was 33, meaning that in order to prevent one case of reoperation related to the patellofemoral joint one would need to resurface 33 patellae. Although there were statistically significant differences between the two treatment effects with respect to reoperation, the clinical benefit may not be apparent based on the findings of our meta-analysis. Furthermore, the reluctance to revise a resurfaced patella may decrease the rate of reoperation in the patellar resurfacing group and lead to an overestimation of intervention effect, which has been discussed as a confounding variable in some studies [48]. As isolated revision of the patella component has been reported to be fraught with complications, there are fewer options available for the treatment of anterior pain in a knee with an already resurfaced patella [33]. Therefore, when we use the rate of reoperation as an outcome measure to assess the effectiveness of intervention, this should be taken into account.
The overall incidence of postoperative anterior knee pain in the 1,421 knees was 12.9% in the patellar resurfacing group and 24.1% in the patellar nonresurfacing group. For a pooled estimate, because of the observed large between-group heterogeneity, despite a significantly lower RR of anterior knee pain in the patients with patellar resurfacing when fixed-effects meta-analysis was used, attributing the effect to patellar resurfacing uniquely is inappropriate. When meta-analysis was limited to high quality studies, regardless of whether a fixed-effects method or random-effects method was used, the summary effect showed no significant differences between the two groups with moderate heterogeneity (I² = 50%). However, the results cannot be easily interpreted. Statistical heterogeneity is a consequence of clinical or methodological diversity, or both, among the studies [49]. In our review, the differences between studies in terms of methodological factors, such as use of blinding and concealment of allocation, and differences between studies in the way the anterior knee pain was defined and measured, may contribute to differences in the observed intervention effects. Clinical variation will also lead to heterogeneity, such as the specific implant design, surgical technique and patient characteristics. Burnett et al. [50] reported that underlying patient, implant or surgical factors substantially impact the presence of anterior knee pain, and despite resurfacing or nonresurfacing of the patella in TKA, the prevalence of anterior knee pain is approximately 17% ten years postoperatively. Component design influences patella tracking and conformity and may influence the presence of anterior knee pain [36, 51]. In this review, ten different prostheses were used in the included studies, which may be an important variable in the results of patellar resurfacing or nonresurfacing. Patient characteristics, such as weight, height, body mass index (BMI), gender, age and retinacular release, had been proved by some authors to have no relationship to the development of anterior knee pain [9, 35, 37, 38, 53]. Anterior knee pain before and after TKA has often been associated with a patellofemoral aetiology. However, it should be regarded as a syndrome, whose symptoms may be attributed to multiple causes [9, 51, 52], and is not necessarily related to preservation or replacement of the articular cartilage [29]. In view of the inadequate information about whether different studies compare the same aetiology, the current evidence indicated that the effectiveness of patellar resurfacing in reducing the incidence of postoperative anterior knee pain remains uncertain.
The variety of knee rating systems used in the studies made it difficult to compare the merits of patellar resurfacing or nonresurfacing. In our review, apart from two studies which reported that the difference between the resurfaced and the unresurfaced groups was significantly in favour of the resurfaced group, both the pooled estimate of four studies used KSS and the results of the other seven studies that cannot be included for meta-analysis demonstrated there was no significant difference between the two groups. Patient satisfaction was the same irrespective of whether the patella was resurfaced or not.
Based on the evidence presented, we draw a conclusion that patellar resurfacing in TKA can reduce the risk of reoperation with no benefit to postoperative knee function or patient satisfaction in TKA without patellar resurfacing, and whether it can decrease the incidence of anterior knee pain remains uncertain. Routinely resurfacing the patella lacks sufficient supporting evidence. The decision of whether or not to resurface the patella in TKA should be made based on the consideration of the situation of the patellofemoral joint, the design of the prosthesis [38, 53] and the experience of the surgeon, and it should integrate the patients’ values and preferences [54].
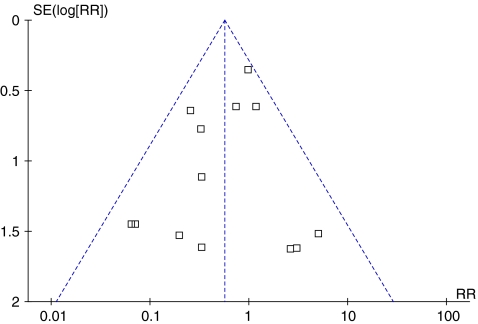
Several limitations were recognised in this review. First, we did not hand search journals and did not try to identify unpublished studies, making it possible that some related studies have been missed. We used funnel plots to detect the reporting biases (Fig. 6). However, because the tests typically have relatively low power, even when a test does not provide evidence of funnel plot asymmetry, bias (including publication bias) cannot be excluded [55]. Second, a higher proportion of attrition rate existed in some included studies with mid- to long-term follow-up, producing a high risk of bias. To test the stability and reliability of the results by sensitivity analysis is necessary. However, it was impossible to perform an intention to treat analysis, because the numbers randomised into each intervention group were not reported in some studies and we failed to obtain the extra information by contacting the authors. Finally, the knee rating systems used in some studies to assess the effects of TKA were different and some data were reported incompletely; therefore, we excluded those studies in meta-analysis, which may influence the summary estimate of the quantitative synthesis.
Fig. 6.
Funnel plots of RR of reoperations for any reason
Some attention should be paid to further research. In this review, the missing data reached 36–42% in two studies with at least ten years follow-up, most of which were due to death. Therefore, in order to observe the adverse events in the long term, the age of participants should be taken into consideration when enrolling eligible participants. Further research should describe randomisation methods and allocation in concealment in more detail, use at least blinded outcome assessors and report whether intention to treat analysis is used. Reporting that conforms to the Consolidated Standards of Reporting Trials (CONSORT) statement is necessary [56]. Because the economic burden is of concern to some patients, future trials should perform cost-effectiveness analysis.
Footnotes
The authors contributed equally to the study.
References
- 1.Badhe N, Dewnany G, Livesley PJ. Should the patella be replaced in total knee replacement? Int Orthop. 2001;25(2):97–99. doi: 10.1007/s002640100225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patal K, Raut V. Patella in total knee arthroplasty: to resurface or not to-a cohort study of staged bilateral total knee arthroplasty. Int Orthop. 2010 doi: 10.1007/s00264-010-1063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levitsky KA, Harris WJ, McManus J, Scott RD. Total knee arthroplasty without patellar resurfacing. Clinical outcomes and long-term follow up evaluation. Clin Orthop Relat Res. 1993;286:116–121. [PubMed] [Google Scholar]
- 4.Fern ED, Winson IG, Getty CJ. Anterior knee pain in rheumatoid patients after total knee replacement. Possible selection criteria for patellar resurfacing. J Bone Joint Surg Br. 1992;74(5):745–748. doi: 10.1302/0301-620X.74B5.1527126. [DOI] [PubMed] [Google Scholar]
- 5.Lybäck CO, Lehto MU, Hämäläinen MM, Belt EA. Patellar resurfacing reduces pain after TKA for juvenile rheumatoid arthritis. Clin Orthop Relat Res. 2004;423:152–156. doi: 10.1097/01.blo.0000127118.98129.6d. [DOI] [PubMed] [Google Scholar]
- 6.Barrack RL, Wolfe MW. Patellar resurfacing in total knee arthroplasty. J Am Acad Orthop Surg. 2000;8(2):75–82. doi: 10.5435/00124635-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Boyd AD, Ewald FC, Thomas WH, Poss R, Sledge CB. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am. 1993;75(5):674–681. doi: 10.2106/00004623-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Levai JP, McLeod CH, Freeman MA. Why not resurface the patella? J Bone Joint Surg Br. 1983;65(4):448–451. doi: 10.1302/0301-620X.65B4.6874718. [DOI] [PubMed] [Google Scholar]
- 9.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85(2):212–217. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Insall JN, Tria AJ, Aglietti P. Resurfacing of the patella. J Bone Joint Surg Am. 1980;62(6):933–936. [PubMed] [Google Scholar]
- 11.Tabutin J, Banon F, Catonne Y, Grobost J, Tessier JL, Tillie B. Should we resurface the patella in total knee replacement? Experience with the Nex Gen prosthesis. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):534–538. doi: 10.1007/s00167-004-0571-z. [DOI] [PubMed] [Google Scholar]
- 12.Oh IS, Kim MK, You DS, Kang SB, Lee KH. Total knee arthroplasty without patellar resurfacing. Int Orthop. 2006;30(5):415–419. doi: 10.1007/s00264-006-0111-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasegawa M, Ohashi T. Long-term clinical results and radiographic changes in the nonresurfaced patella after total knee arthroplasty: 78 knees followed for mean 12 years. Acta Orthop Scand. 2002;73(5):539–545. doi: 10.1080/000164702321022811. [DOI] [PubMed] [Google Scholar]
- 14.Ogon M, Hartig F, Bach C, Nogler M, Steingruber I, Biedermann R. Patella resurfacing: no benefit for the long-term outcome of total knee arthroplasty. A 10- to 16.3-year follow-up. Arch Orthop Trauma Surg. 2002;122(4):229–234. doi: 10.1007/s00402-001-0364-5. [DOI] [PubMed] [Google Scholar]
- 15.Oztürk A, Bilgen S, Atici T, Ozer O, Bilgen OF. The evaluation of patients undergoing total knee arthroplasty with or without patellar resurfacing. Acta Orthop Traumatol Turc. 2006;40(1):29–37. [PubMed] [Google Scholar]
- 16.Hurson C, Kashir A, Flavin R, Kelly I. Routine patellar resurfacing using an inset patellar technique. Int Orthop. 2009 doi: 10.1007/s00264-009-0831-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Picetti GD, McGann WA, Welch RB. The patellofemoral joint after total knee arthroplasty without patellar resurfacing. J Bone Joint Surg Am. 1990;72(9):1379–1382. [PubMed] [Google Scholar]
- 18.Keblish PA, Varma AK, Greenwald AS. Patellar resurfacing or retention in total knee arthroplasty. A prospective study of patients with bilateral replacements. J Bone Joint Surg Br. 1994;76(6):930–937. [PubMed] [Google Scholar]
- 19.Kim BS, Reitman RD, Schai PA, Scott RD. Selective patellar nonresurfacing in total knee arthroplasty. 10 year results. Clin Othop Relat Res. 1999;367:81–88. [PubMed] [Google Scholar]
- 20.Forster MC. Patellar resurfacing in total knee arthroplasty for osteoarthritis: a systematic review. Knee. 2004;11(6):427–430. doi: 10.1016/j.knee.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 21.Nizard RS, Biau D, Porcher R, Ravaud P, Bizot P, Hannouche D, Sedel L. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432:196–203. doi: 10.1097/01.blo.0000150348.17123.7f. [DOI] [PubMed] [Google Scholar]
- 22.Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2005;87(7):1438–1445. doi: 10.2106/JBJS.D.02422. [DOI] [PubMed] [Google Scholar]
- 23.Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005;438:191–196. doi: 10.1097/01.blo.0000166903.69075.8d. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews for intervention. Version 5.0.0:180. (updated February 2008) The Cochrane Collaboration. Available via www.cochrane-handbook.org
- 25.Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews for intervention. Version 5.0.0:242-248. (updated February 2008) The Cochrane Collaboration. Available via www.cochrane-handbook.org
- 26.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127(9):820–826. doi: 10.7326/0003-4819-127-9-199711010-00008. [DOI] [PubMed] [Google Scholar]
- 27.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 29.Calvisi V, Camillieri G, Lupparelli S. Resurfacing versus nonresurfacing the patella in total knee arthroplasty: a critical appraisal of the available evidence. Arch Orthop Trauma Surg. 2009;129(9):1261–1270. doi: 10.1007/s00402-008-0801-9. [DOI] [PubMed] [Google Scholar]
- 30.Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–1055. doi: 10.1016/S0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 31.Newman JH, Ackroyd CE, Shah NA, Karachalios T. Should the patella be resurfaced during total knee replacement? Knee. 2000;7(1):17–23. doi: 10.1016/S0968-0160(99)00033-2. [DOI] [Google Scholar]
- 32.Barrack RL, Wolfe MW, Waldman DA, Milicic M, Bertot AJ, Myers L. Resurfacing of the patella in total knee arthroplasty. A prospective, randomized, double-blind study. J Bone Joint Surg Am. 1997;79(8):1121–1131. doi: 10.2106/00004623-199708000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am. 2001;83(9):1376–1381. [PubMed] [Google Scholar]
- 34.Bourne RB, Rorabeck CH, Vaz M, Kramer J, Hardie R, Robertson D. Resurfacing versus not resurfacing the patella during total knee replacement. Clin Orthop Relat Res. 1995;321:156–161. [PubMed] [Google Scholar]
- 35.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res. 2004;428:12–25. doi: 10.1097/01.blo.0000148594.05443.a3. [DOI] [PubMed] [Google Scholar]
- 36.Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM. Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88(6):734–739. doi: 10.1302/0301-620X.88B6.16822. [DOI] [PubMed] [Google Scholar]
- 37.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK. Patellar resurfacing in total knee arthroplasty: a prospective, randomized trial. J Bone Joint Surg Am. 2002;84(2):187–193. doi: 10.2106/00004623-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Smith AJ, Wood DJ, Li MG. Total knee replacement with and without patellar resurfacing: a prospective, randomised trial using the profix knee system. J Bone Joint Surg Br. 2008;90(1):43–49. doi: 10.1302/0301-620X.90B1.18986. [DOI] [PubMed] [Google Scholar]
- 39.Partio E, Wirta J. Comparison of patellar resurfacing and nonresurfacing in total knee arthroplasty: a prospective randomised study. J Orthop Rheumatol. 1995;8:69–74. [Google Scholar]
- 40.Huang ZF, Weng XS, Qiu GX, Jing J, Lin J, Yang XY. The influence of patellar retention or resurfacing on total knee arthroplasty. J Pract Orthop. 2007;13(8):449–452. [Google Scholar]
- 41.Schroeder-Boersch H, Scheller G, Fischer J, Jani L. Advantages of patellar resurfacing in total knee arthroplasty. Two-year results of a prospective randomized study. Arch Orthop Trauma Surg. 1998;117:73–78. doi: 10.1007/BF00703446. [DOI] [PubMed] [Google Scholar]
- 42.Kordelle J, Schleicher I, Kaltschmidt I, Haas H, Grüner MR. Patella resurfacing in patients without substantial retropatellar knee pain symptoms? Z Orthop Ihre Grenzgeb. 2003;141(5):557–562. doi: 10.1055/s-2003-42850. [DOI] [PubMed] [Google Scholar]
- 43.Gildone A, Manfredini M, Biscione R, Faccini R. Patella resurfacing in posterior stabilised total knee arthroplasty: a follow-up study in 56 patients. Acta Orthop Belg. 2005;71:445–451. [PubMed] [Google Scholar]
- 44.Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78(5):226–228. [PubMed] [Google Scholar]
- 45.Kajino A, Yoshino S, Kameyama S, Kohda M, Nagashima S. Comparison of the results of bilateral total knee arthroplasty with and without patellar replacement for rheumatoid arthritis. A follow-up note. J Bone Joint Surg Am. 1997;79(4):570–574. doi: 10.1302/0301-620X.79B4.7238. [DOI] [PubMed] [Google Scholar]
- 46.Jüni P, Altman DG, Egger M. Systematic reviews in healthcare: assessing the quality of controlled clinical trials. BMJ. 2001;323:42–46. doi: 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71(3):262–267. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 48.Burnett S, Bourne RB. Indications for patellar resurfacing in total knee arthroplasty. J Bone Joint Surg Am. 2003;85(2):728–745. [Google Scholar]
- 49.Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews for intervention. Version 5.0.0:269. (updated February 2008) The Cochrane Collaboration. Available via www.cochrane-handbook.org
- 50.Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007;464:65–72. doi: 10.1097/BLO.0b013e31812f783b. [DOI] [PubMed] [Google Scholar]
- 51.Ma MH, Lu YC, Kwok TG, Ho FY, Huang CY, Huang CH. The effect of the design of the femoral component on the conformity of the patellofemoral joint in total knee replacement. J Bone Joint Surg Br. 2007;89(3):408–412. doi: 10.1302/0301-620X.89B3.18276. [DOI] [PubMed] [Google Scholar]
- 52.Brander V, Stulberg SD, Adams AD, Harden RN, Bruehl S, et al. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res. 2003;416:27–36. doi: 10.1097/01.blo.0000092983.12414.e9. [DOI] [PubMed] [Google Scholar]
- 53.Tanzer M, McLean CA, Laxer E, Casey J, Ahmed AM. Effect of femoral component designs on the contact and tracking characteristics of the unresurfaced patella in total knee arthroplasty. Can J Surg. 2001;44(2):127–133. [PMC free article] [PubMed] [Google Scholar]
- 54.Haynes RB, Devereaux PJ, Guyatt GH. Clinical expertise in the era of evidence-based medicine and patient choice. ACP J Club. 2002;136(2):A11–A14. [PubMed] [Google Scholar]
- 55.Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews for intervention. Version 5.0.0:310. (updated February 2008) The Cochrane Collaboration. Available via www.cochrane-handbook.org
- 56.Moher D, Schulz KF, Altman DC. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001;357(9263):1191–1194. doi: 10.1016/S0140-6736(00)04337-3. [DOI] [PubMed] [Google Scholar]