Abstract
The size of the femoral head and acetabular anteversion are crucial for stability in total hip replacements. This study examined the effects of head diameter and acetabular anteversion on the posterior instability after total hip replacement in an in vivo setting. The acetabular shell was inserted at 0–20° of anteversion at five degree intervals. By using different head sizes (28 mm, 32 mm, 36 mm), the degrees of dislocation were recorded by computer navigation. The 36-mm group consistently showed better stability compared with the 32- and 28-mm groups, regardless of the degree of cup anteversion. Within each group of head size, the hip was significantly more stable when the cup anteversion increased from 0° to 10°. The difference became insignificant when it increased from 15° to 20°.
Introduction
Dislocation after total hip replacement is one of the most common complications [1]. The reason is multifactorial. There are many risk factors, including the patient, surgical technique and prosthetic design. The choice of prosthesis and surgical technique are controllable factors. An in vitro study showed an increase in femoral head size of more than 32 mm improved hip range of motion and stability [2]. Clinical studies on the effects of femoral head size on stability were controversial [3–5]. In this study, the effect of femoral head size and anteversion of the acetabular cup on stability of hip is tested by means of computer navigation.
Material and methods
A cadaveric pelvis and a left whole femur from a known male adult Chinese donor were used. The cadaveric bone was denuded of soft tissue. On inspection, there was no gross pathology of the left hip. A cementless total hip system (Pinnacle shell, Summit stem; Depuy, Warsaw, IN) was used.
For reproducible registration of navigation landmarks, 3.5-mm screws were inserted at the pubic tubercles, anterior superior iliac spine, tip of the greater trochanter, and the medial and lateral epicondyles of the left femur. Two 4-mm Schanz screws were inserted into the left ilium and two 4-mm Schanz screws were inserted in the distal end of the left femur. VectorVision (BrainLAB AG, Munich) image-free navigation THR software was used for measurement. The trackers were assembled over the Schanz screws at the pelvis and left femur. The set-up is shown in Figs. 1 and 2. According to the software, the bony landmarks were registered using the recess of 3.5-mm screw heads. The centre of the femoral head was calculated by pivoting the hip. Morphing of the acetabular floor was performed. The femoral neck was osteotomised and the femoral canal was reamed sequentially. A size 3 trial stem that corresponded to the size of the medullary canal of the cadaveric femur was inserted at 15° anteversion of the femur, which was measured with reference to the posterior condylar line. The acetabulum was reamed sequentially to 52-mm when good stability of the trial cup was attained.
Fig. 1.
Study set-up
Fig. 2.
Assembly of the trial components and navigation trackers onto cadaveric bone
Another instrument tracker was connected to a holder of the acetabular trial shell. The exact position of the acetabular shell could be identified. The acetabular shell was inserted at 45° inclination and 0–20° anteversion at five degree intervals under the guidance of navigation. The trial insert with 10-degree elevated lip for a 28-mm femoral head was inserted. The elevated lip of the insert was placed at 2 o’clock. With the hip at 90° flexion and 0° adduction, the hip was gradually internally rotated. At the time of dislocation, there was an audible alarm from the software and the corresponding degree of internal rotation was recorded. The test was repeated ten times by one of the authors (JTZ) and monitored by another author (NFY). The test was repeated with the hip at 90-degree flexion and 30-degree adduction. The trial inserts accommodating 32-mm and 36-mm femoral trial heads were assembled similarly and the tests were conducted again.
Statistical analysis was performed by one-way analysis of variance (ANOVA) using SPSS (version 16.0; SPSS Inc., Chicago, IL, USA). Significance was taken at the 95% confidence interval.
Results
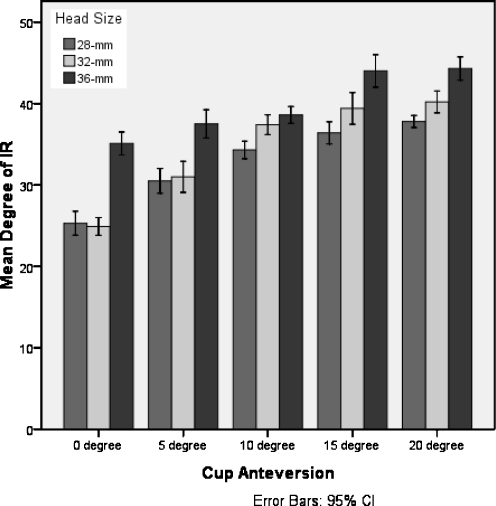
With the hip at 0° or 30° adduction, the degrees of internal rotation that led to posterior dislocation were plotted against the degrees of cup anteversion (Figs. 3 and 4, respectively). The 28-mm, 32-mm and 36-mm groups are shown in the graphs of Figs. 3 and 4.
Fig. 3.
With the hip at 90° flexion and 0° adduction, mean degree of internal rotation to dislocation was plotted against degree of cup anteversion using different sizes of femoral heads
Fig. 4.
With the hip at 90° flexion and 30° adduction, mean degree of internal rotation to dislocation was plotted against degree of cup anteversion using different sizes of femoral heads
Effect of cup anteversion
Within each group of femoral head size, when the cup anteversion varied from 0° to 15°, there was an increase in the degree of internal rotation to posterior dislocation (p < 0.05). There was no statistically significant difference between 15° anteversion and 20° anteversion.
Effect of femoral head size
With the hip at 90° flexion and 0° adduction, regardless of acetabular anteversion, the 36-mm group consistently showed a significantly higher degree of internal rotation to dislocation compared with the 28- and 32-mm groups, respectively (p < 0.005). The 32-mm group showed a significantly higher degree of internal rotation to dislocation compared with the 28-mm group when the acetabular anteversion was 10° or more (p < 0.05); the difference became statistically insignificant when the anteversion was less than 10°.
With the hip at 90° flexion and 30° adduction, regardless of acetabular anteversion, the 36-mm group also showed a significantly higher degree of internal rotation to dislocation compared with the 28- and 32-mm groups, respectively (p < 0.05). The 32-mm group showed a significantly higher degree of internal rotation to dislocation compared with the 28-mm group when the acetabular anteversion was 10° or more (p < 0.05); the difference became statistically insignificant when the anteversion was less than 10°.
Discussion
Dislocation after total hip replacement is annoying and recurrent dislocation is notoriously difficult to treat [6, 7]. The incidence of dislocation after primary total hip arthroplasty in large series varies from 0.4% to 5.8% [3, 8]. Berry et al. reported the cumulative risk of dislocation can be up to 6% at 20 years [4], suggestive that this vexing problem is not restricted to the early postoperative period. The risk of posterior dislocation was reportedly higher when the posterior approach was used.
One of the most important and controllable surgical factors is how the surgeon implants the prosthesis. In a classical paper Lewinnek et al. suggested that prosthesis insertion should be based on the “safe-zone” [9]. The dislocation rate for cup orientation with anteversion of 15 ± 10° and cup abduction angle of 40 ± 10° was 1.5%, while outside this “safe zone” the dislocation rate was 6.1%. However, this position of the “safe-zone” was deduced by measurement on postoperative plain X-rays and mathematical deduction. Many studies on the effect of position of prosthesis on dislocation of total hip replacement also depended on the postoperative X-rays [10]. Potential errors are present. CT assessment of the acetabular component has been studied [11], but artefacts may affect the reliability. With the use of computer navigation, the cup abduction angle and anteversion angle, and the exact degree of hip rotation, especially at the position when the hip is dislocated, can be accurately measured. In our study, the abduction angle was constant at 45° and this has been agreed upon by most experts. By means of computer navigation, the effect of anteversion of the acetabular component can be accurately determined. Our results showed that the optimal cup anteversion should be at least 15 to 20 degrees. This figure correlated very well to most clinical studies [12].
Another important and controllable factor is the femoral head diameter. Theoretically, a larger femoral head diameter improves the head-to-neck ratio, increases the range of motion without prosthetic impingement, requires greater jump distance before dislocation and better constraint by soft tissue envelope [1]. In the past, a smaller diameter of femoral head was chosen to reduce volumetric wear rate [13]. However, a long-term large series study showed that smaller head size was associated with higher cumulative dislocation rate in comparison to larger diameters [4]. With the advances in the wear resistance of the new bearing surfaces, large diameter heads may not be associated with higher wear rate. Bartz et al. showed that the site of impingement varied with the head diameter [14]. With the 22-mm head, impingement occurred between the femoral prosthesis and acetabular liner. With the 32-mm head, impingement occurred between femur and pelvis. In this study, bone-on-bone impingement always occurred in the 36-mm group. The advantage of avoiding component-on-component impingement is even more important in ceramic-on-ceramic and metal-on-metal articulations.
In this study, the posterior stability depended on the anteversion of the acetabular cup and the size of the femoral head. When the acetabular anteversion was 20° and a femoral head of 28 mm was used, the degree of internal rotation to posterior dislocation was 44° when the hip was at 90° flexion and 0° adduction. If a femoral head of 36 mm was used, dislocation occurred only when internal rotation was more than 56°. When the acetabular anteversion was 0° and a femoral head of 28-mm was used, the degree of internal rotation to posterior dislocation was 25° when the hip was at 90° flexion and 30° adduction. If a femoral head of 36 mm was used, dislocation occurred only when internal rotation was more than 35°.
Unco-operative patients, neuromuscular and post-traumatic diseases, and revision situations are common clinical conditions when stability of total hip replacement is intrinsically jeopardised. In revision settings when the host bone contact is inferior, the anteversion of the acetabular cup may be sacrificed to allow stability. Therefore, a large femoral head is favourable.
Nonetheless, a large femoral head is not always the answer. One must be cautious about the scenarios when a large femoral head does not offer better stability. Sariali et al. used mathematical evaluation and reported that jumping distance decreased as the cup abduction angle increased [15]. As a result, the theoretical advantage of using a large femoral head became negligible. Even worse, Crowninshield et al. reported that the vertical acetabular component resulted in elevated stress within the polyethylene and led to implant failure [16]. An experimental study by Prietzel et al. showed that apart from using a large femoral head, capsular repair after total hip replacement is important to improve stability [17]. In the absence of the hip abductor mechanism, the dislocation rate using a large femoral head did not significantly decrease [18].
In our previous study in young Chinese patients, it was noted that the size of acetabular cup in our population is often 50- to 52-mm or less [19]. As a result, a 36-mm head may not be used in all patients because most of the manufacturers only provide 36-mm heads when the acetabular shell is more than or equal to 50 mm. In this situation, we suggest using a 32-mm head because a 32-mm head still shows better results than the 28-mm head. However, the cup anteversion must be increased in order to attain good stability. One must bear in mind that excessively increasing the degree of cup anteversion may increase the chance of anterior dislocation even when the hip is posteriorly approached [20].
There are a few limitations to this study. The effects of standard and different neck lengths compared with high offset femoral components were not studied. The results from only one cadaveric specimen may not extrapolate our results to all clinical situations. There was absence of soft tissue action in the cadaveric model. In this study, we steadily increased the degree by one investigator and another investigator monitored the whole procedure. In order to minimise the chance of error, each set of data was repeated ten times and the average degree of dislocation was then calculated. A hip simulator would be a more reliable means to apply a preset direction and speed of force for dislocation. In future, we will consider using a hip simulator for this.
In conclusion, the posterior stability after total hip replacement in this cadaveric specimen improves with the size of femoral head and degree of cup anteversion. When the clinical condition is unfavourable for stability, for example, acetabular anteversion is suboptimal, the use of a large femoral head is justified.
References
- 1.Soong M, Rubash H, Macaulay W. Dislocation after total hip arthroplasty. J Am Acad Orthop Surg. 2004;12:314–321. doi: 10.5435/00124635-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Burroughs BR, Hallstrom B, Golladay GJ, Hoeffel D, Harris WH. Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes. J Arthroplasty. 2005;20:11–19. doi: 10.1016/j.arth.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Woo R, Morrey B. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 4.Berry DJ, Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 5.Geller JA, Malchau H, Bragdon C, Greene M, Harris WH, Freiberg AA. Large diameter femoral heads on highly cross-linked polyethylene. Clin Orthop Relat Res. 2006;447:53–59. doi: 10.1097/01.blo.0000218742.61624.80. [DOI] [PubMed] [Google Scholar]
- 6.Beaule PE, Schmalzried TP, Udomkiat P, Amstutz HC. Jumbo femoral head for the treatment of recurrent dislocation following total hip replacement. J Bone Joint Surg Am. 2002;84:256–263. doi: 10.2106/00004623-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Bosker BH, Ettemma HB, Verheyen CCPM, Castelein RM. Acetabular augmentation ring for recurrent dislocation of total hip arthroplasty: 60% stability rate after an average follow-up of 74 months. Int Orthop. 2009;33:49–52. doi: 10.1007/s00264-007-0456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Etienne A, Cupic Z, Charnley J. Postoperative dislocation after Charnley low friction arthroplasty. Clin Orthop Relat Res. 1978;132:19–23. [PubMed] [Google Scholar]
- 9.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip replacement arthroplasty. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 10.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Pierchon F, Pasquier G, Cotton A, Fontaine C, Clarisse J, Duquennoy A. Causes of dislocation of total hip arthroplasty: CT study of component alignment. J Bone Joint Surg Br. 1994;76:45–48. [PubMed] [Google Scholar]
- 12.Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, Nunoda D. Study of hip joint dislocation after total hip arthroplasty. Int Orthop. 2006;30:26–30. doi: 10.1007/s00264-005-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Livermore J, Ilstrup D, Morrey B. Effect of femoral head size on wear of polyethylene of the polyethylene acetabular component. J Bone Joint Surg Am. 1990;72:518–528. [PubMed] [Google Scholar]
- 14.Bartz RL, Noble PC, Kadakia NR, Tullos HS. The effect of femoral component head size on posterior dislocation of the artificial hip joint. J Bone Joint Surg Am. 2000;82:1300–1307. doi: 10.2106/00004623-200009000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Sariali E, Lazennec JY, Khiami F, Catonne Y. Mathematical evaluation of jumping distance in total hip arthroplasty: influence of abduction angle, femoral head offset, and head diameter. Acta Ortho. 2009;80:277–282. doi: 10.3109/17453670902988378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crowninshield RD, Maloney WJ, Wentz DH, Humphrey SM, Blanchard CR. Biomechanics of large femoral heads. Clin Orthop. 2004;429:102–107. doi: 10.1097/01.blo.0000150117.42360.f9. [DOI] [PubMed] [Google Scholar]
- 17.Prietzel T, Richter KW, Salis-Soglio G. The stabilizing effect of atmospheric pressure (AP) on hip joint subject to traction force—an experimental study. Z Orthop Unfall. 2007;145:468–475. doi: 10.1055/s-2007-965255. [DOI] [PubMed] [Google Scholar]
- 18.Kung PL, Ries MD. Effect of femoral head size and abductors on dislocation after revision THA. Clin Orthop Rel Res. 2007;465:170–174. doi: 10.1097/BLO.0b013e318159a983. [DOI] [PubMed] [Google Scholar]
- 19.Chiu KY, Tang WM, Ng TP. Cementless total hip arthroplasty in young Chinese patients. J Arthroplasty. 2001;16:863–870. doi: 10.1054/arth.2001.25505. [DOI] [PubMed] [Google Scholar]
- 20.Ng TP, Yau WP, Tang WM, Chiu KY. Anterior dislocation following primary total hip replacement by posterior approach—aetiology and treatment. Hong Kong J Orthop Surg. 2003;7:14–18. [Google Scholar]