Abstract
Cystic hygromas are the cystic variety of lymphangioma, common locations being cervico-facial regions and axilla. Respiratory distress, recurrent infections or cosmetic reasons are the main indications of the treatment. The ideal treatment is complete surgical excision; however, there is a gradual conversion towards sclerosant therapy. This article reviews the current literature and discusses the various problems encountered during the management of these lesions.
Keywords: Cystic hygroma, surgical excision, bleomycin, complications
INTRODUCTION
Hygroma in Greek means water-containing tumour. They are congenital malformations of lymphatic system. Cystic hygroma occurs more frequently as compared to other types of lymphangioma, and may compose of single or multiple macrocystic lesions having scarce communication with normal lymphatic channels.[1]
Lymphangiomas are usually classified as capillary, cavernous or cystic lymphangiomas. They may also be classified more conveniently, on the basis of size of the cysts contained, as microcystic, macrocystic and mixed lymphangiomas. Microcystic lymphangioma consists of cysts measuring less than 2 cm in size, whereas the size of cysts in case of macrocystic lymphangioma is more than 2 cm. The mixed lymphangioma is characterized by cysts of variable sizes, i.e. some cysts are more than 2 cm in size and others are less than 2 cm.[2,3]
Embryology
In the eighth week of gestation, six lymphatic sacs can be identified in the developing embryo. These lymphatic sacs are two jugular sacs, two iliac, one at the base of root of mesentery and one dorsal to the abdominal aorta (cysterna chyli). Jugular lymphatic sacs develop in the region of neck, whereas iliac sacs develop in the lumbar region. Later on, a network of lymphatics develops that communicate with lymphatics of various regions. During the ninth week of gestation, these sacs are invaded by connective tissue to form lymph nodes.[2]
There are a number of proposed mechanisms to explain the pathophysiology of cystic hygroma. Embryologically, these lesions are believed to originate from sequestration of lymphatic tissue from lymphatic sacs, during the development of lymphatico-venous sacs. These sequestered tissues fail to communicate with remainder of the lymphatic or venous system. Later on, dilatation of the sequestered lymphatic tissues ensues, resulting in the cystic morphology of these lesions.[2]
Location of cystic hygromas
Cystic hygromas can manifest anywhere in the body. The common locations are cervico-facial regions (especially posterior cervical triangle), axilla, mediastinum, groin and below tongue. Occasionally, these malformations occur in liver, spleen, kidney and intestine. Omental cyst in omentum and mesenteric cyst in the mesentery of intestine represents parallel lesions at these locations.[4–6]
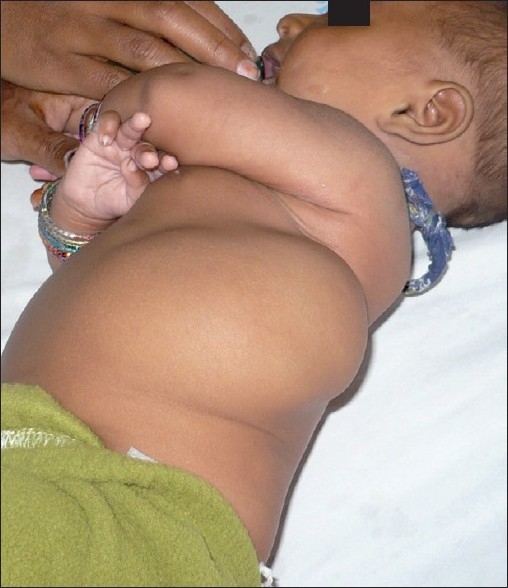
We have observed other rare sites of its occurrence especially at limbs, chest wall, cheek, lumbar region, supra-sternal area and over the shoulder or deltoid [Figures 1 and 2]. Though, usually isolated and single at these unusual occasions, cystic hygroma at multiple sites in the body have been observed.
Figure 1.

Cystic hygroma on the cheek
Figure 2.

Cystic hygroma of supra-sternal area
Diagnosis of cystic hygromas
In about 80% of instances, the location of cystic hygromas is cervico-facial region. Therefore, cystic hygroma should always be considered first in the preliminary differential diagnosis of cystic lesions with onset at birth, in the above-mentioned location. More than 60% of cystic hygromas have onset at birth and up to 90% become overt before the age of two years.[1,2,4–6]
The nascent appearance of cystic hygroma in adults has scarcely been reported in the literature. Some case reports depicted post-traumatic appearance (acquired cystic hygroma) of cystic hygroma in previously normal adults. These might represent the dormant variety of cystic hygromas that can appear at any age and trauma might be a coincidental event in those cases.[7–9]
The usual presentation of cystic hygroma apparent at birth is a painless mass with worries and queries of the parents about the lesion. The other modes of presentations are related to the complications or effects of cystic hygroma, such as respiratory distress, feeding difficulty, fever, sudden increase in the size and infection in the lesion.[1–3]
On clinical examinations, these lesions appear soft, compressible, non-tender, transluminant and without any bruit [Figures 3 and 4]. Ultrasound of the lesion usually features multicystic lesion with internal septations and no blood flow is detected on color doppler ultrasonographs. Other modalities like CT scan and MRI can be employed to delineate the lesion, in a better way. A CT scan demonstrates multicystic, homogeneous, non-invasive density with low attenuation [Figure 5]. These modalities are usually helpful in ascertaining the extent of the lesion and their association with nerves and vessels and are particularly useful, when surgical management of the lesion is contemplated.[1,10–12] These cysts may produce milky, serous, sero sanguinous or straw-coloured fluid, when aspirated with a wide-bore needle.[5]
Figure 3.
Cystic hygroma of lumbar region
Figure 4.

Transillumination is positive in the lumbar region cystic hygroma
Figure 5.

CT scan of a patient with cystic hygroma of neck
The prenatal diagnosis of cystic hygroma using ultrasound is well documented in the literature. This malformation is commonly localized in the nuchal region. An additional 20% are found in the axilla, while the remaining 5% are found in the mediastinum, retroperitoneum, abdominal viscera, groin, bones and scrotum. The characteristic sonographic appearance on antenatal ultrasonography is multiseptate, thin-walled cystic mass; occasionally the cystic mass may have a more complex echo texture with cystic and solid components. The foetus with cystic hygroma can be associated with other anomalies in about 62% of cases. The associated anomalies are Turner's syndrome, Down's syndrome, Trisomy 18, Trisomy 13, Noonan syndrome, etc.[13–16]
Sometimes biopsy correlation is needed for the precise diagnosis of the lesion occurring at unusual sites such as laryngeal, intra-oral and orbital lymphangiomas.[17,18]
Complications of cystic hygroma
Cystic hygromas are benign lesions; however, complications may arise. These lesions can get infected any time. The usual source of infection is seedling of microorganisms from a secondary focus of infection (respiratory tract infections), though they may get infected primarily also. During the course of infection, the cystic hygroma increases in size and becomes warm, red and tender. The patient may become febrile. The infection may involve entire cystic hygroma or a few of its cysts [Figure 6]. During active infection, it may not remain transluminant. Sometimes cystic hygroma turns into an abscess, which needs to be drained for amelioration of the symptoms. The treatment is conservative with antibiotics, antipyretics and analgesics.[1–5,19] It is our observation that in some instances, post-infection size of the cystic hygroma reduces remarkably.
Figure 6.

Cystic hygroma of neck and oral cavity. The lower portion of cystic hygroma was infected
The other most frequently reported and observed complication is spontaneous bleeding in the cyst. In this case, the cysts get tense and hard. On aspiration, they yield haemorrhagic fluid. Spontaneous haemorrhage in the scrotal lymphangioma may have to be dealt surgically to avoid testicular ischemia [Figure 7].[20] Kaur et al. reported spontaneous rupture, on the fourth day after birth, of a giant cystic hygroma of neck, necessitating urgent surgical intervention.[4]
Figure 7.

Spontaneous haemorrhage in a patient of scrotal lymphangioma
The other complications include respiratory difficulties and dysphagia, especially in cystic hygroma of neck and oral cavity. Sometimes, the cystic hygroma of neck and oral cavity occurs concurrently in the same patient; thus, creating a difficult situation for the management of respiratory distress and dysphagia. Lymph discharging sinus, resulting from infection or trauma is another rare complication.[1–4]
Management of cystic hygroma
The most preferred modality of treating cystic hygroma remains complete surgical excision; however, many recent case reports and case series have increasingly documented remarkable results for management of such lesions with sclerosant agents.[1–4,18–22] The other treatment modalities that have been employed with variable results include simple drainage, aspirations, radiation, laser excision, radio-frequency ablation and cauterization.[17,18,22]
Cystic hygromas are benign lesions and can remain asymptomatic in a patient for long duration. The indications of treatment are recurrent bouts of infection in the lesion, respiratory distress, dysphagia, haemorrhage inside cystic hygroma, sudden increase in the size of lesion, lymph discharging sinus and disfigurement. The respiratory distress can be of severe nature necessitating a tracheostomy due to complete or significant laryngeal or tracheal compressions by external and sometimes laryngeal lymphangiomas.[18–26] In our observation, a few patients showed partial self-regression of the lesion; however, complete spontaneous resolution has not been observed by us.
Surgical excision of the complex cystic hygromas, involving deep and vital structures, is not an easy task. Extreme care has to be followed to avoid per-operative complications. The possible complications during surgery are damage to facial nerve, facial artery, carotid vessels, internal jugular vessels, thoracic duct and pleura, and incomplete excision in case of infiltration to the surrounding structures. The post-operative complications observed after surgical excision of cystic hygroma are wound infection, haemorrhage, hypertrophied scar and lymphatic discharge from the wound. In about 20 % of cases, there is recurrence even after apparent complete excision of the lesion.[1,18–26] Despite these possible complications, surgical excision of the cystic hygroma is still a preferred option in cases of life threatening lymphangiomas and wherein there is spontaneous bleeding. Intra-thoracic and intra-abdominal lesions are also preferably managed with surgical approach.[23]
Aspiration of the cystic hygroma can be performed as a temporary measure to reduce the size of the cystic hygroma, and thereby, reducing its pressure effects on the respiratory and feeding passages. A tracheostomy and feeding gastrostomy can be performed if the patient is not fit for any type of intervention, and especially in those with severe respiratory and feeding difficulties.[8,18]
As mentioned earlier, the other successful and popular treatment option for the management of cystic hygroma is sclerotherapy. Previously, sclerotherapy was carried out with sclerosant agents, such as boiling water, quinine, sodium morrhuate, urethane, iodine tenture, doxycycline and nitromin. However, sclerotherapy with the above-mentioned agents has been associated with low success rates and frequent complications.[16,20–24]
Sclerotherapy with intra-lesional bleomycin, as a primary treatment modality, for cystic hygroma, has been tried. Various case reports and original studies have documented good response to the therapy.[20–23] The other agent used as sclerosant is OK432, has more satisfactory results and less complications as compared to bleomycin.[20–24]
Bleomycin is a chemotherapeutic agent used in chemotherapy for a number of malignancies. Yura et al. used intra-lesional bleomycin as sclerosant agent for the first time.[21] It is a DNA synthesis inhibitor and its exact mechanism of action in cystic hygroma is not known; however, it is believed that it may produce a non-specific inflammatory process that results in the fibrosis of the cysts. In about 60% of patients treated with intra-lesional bleomycin, there was complete resolution of the lesion; and in about 30% patients, it caused remarkable reduction in size.[20–24] The same is true in our experience.
Bleomycin can be prepared as aqueous solution or as fat emulsion. Bleomycin is usually given according to the weight of the patient. The recommended dosage is 0.3 mg/kg to 3 mg/kg per session. However, many authors prefer giving bleomycin according to the size of the lesion and not the weight of the patient. Higher dosage is usually associated with complications.[20–24] In our experience, 0.5 mg/kg is a safer dose and can give excellent results. The recommended therapy schedule is fortnightly sessions with intra-lesional bleomycin, and 3-6 sessions have to be given for ultimate results. Some authors suggested weekly sessions for sclerotherapy with bleomycin.[20–24] However, we prefer a minimum interval of three weeks between sessions.
The reported complications of sclerotherapy with bleomycin are discolouration of the injection site, sudden increase in the size of cystic hygroma, fever, vomiting, cellulitis, interstitial pneumonia and pulmonary fibrosis. Pulmonary fibrosis is associated with high dosage of bleomycin. The safe upper limit for dosage of bleomycin in a single session is 30 mg/m2. In published case series, where small doses of bleomycin were used, there was no pulmonary fibrosis in any of their patients.[20–24] In some patients, we have observed an increase in the size of cystic hygroma after few hours of sclerotherapy with bleomycin [Figure 8]. Sometimes the cysts of the lesion reduced in size, but turned very tense and hard. Another cosmetic complication is the persistent firm hard residual lesion after disappearance of all the palpable cysts [Figure 9].
Figure 8.

Increase in the size of cystic hygroma after 2 weeks of intra-lesional bleomycin as sclerosant in a patient shown in Figure 2
Figure 9.

Cystic hygroma resolved completely but a thickened area can be observed
In difficult patients, where cystic hygroma is compressing upon the respiratory passages and located very deep, we have used combined approach. The part of cystic hygroma, which can be excised without any damage to vital structures, is removed surgically and the remaining cysts were injected with injection bleomycin under vision. This has given excellent results with respect to recurrence.
OK-432 is another agent which has been tried, with good results with respect to the lesion resolution and complications25. It acts by causing migration of acute inflammatory cells into the cysts, which release cytokines, resulting in the damage of the endothelium of the cysts and an increase in its permeability and apoptosis. All these factors contribute to the reduction of size of the lesion.[25]
Katsuno et al[26] described successful surgical excision of the cystic hygroma after filling each cyst with hydrocolloid dental impression material. In their technique, they simultaneously aspirated the cyst fluid and injected the hydrocolloid dental impression material under direct vision after exposing the cysts surgically. This resulted in perfect delineation of each cyst all around and its complete excision became very easy. The prerequisite for the procedure is that the lesion should not involve major nerves and vessels.[26]
The other techniques recently introduced in the management of lymphangiomas are radio-frequency ablation and laser excision of the lymphangiomas. Laser has been increasingly used especially for laryngeal lymphangiomas. It causes point destruction of the lesion, thus avoiding damage to the adjacent vital structures.[8,27]
CONCLUSION
Cystic hygroma is a manageable lesion in paediatric population. Suitable treatment should be opted based upon case to case variation. Optimum treatment can be given by surgery alone, sclerotherapy alone or combined use of both. Recently invented treatment modalities such as laser and radiofrequency can also be used in selected patients.
Acknowledgments
We are thankful to Miss Attiya Bano for her help in retrieval of many articles from paid sites.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Manikoth P, Mangalore GP, Megha V. Axillary cystic hygroma. J Postgrad Med. 2004;50:215–6. [PubMed] [Google Scholar]
- 2.Fonkalsrud EW. Lymphatic disorders. In: Grosfeld JL, O'Neill JA Jr, Coran JA, Fonkalsrud EW, Caldamone AA, editors. Pediatric surgery. 6th ed. Chicago: Mosby Elsevier; 2006. pp. 2137–45. [Google Scholar]
- 3.Sanlialp I, Karnak I, Tanyel FC, Senocak ME, Buyukpamukcu N. Sclerotherapy for lymphangioma in children. Int J Pediatr Otorhynolaryngol. 2003;67:795–800. doi: 10.1016/s0165-5876(03)00123-x. [DOI] [PubMed] [Google Scholar]
- 4.Kaur N, Gupta A, Amratash , Singh N. Giant cystic hygroma of the neck with spontaneous rupture. J Indian Assoc Pediatr Surg. 2007;12:154–5. [Google Scholar]
- 5.Kocher HM, Vijaykumar T, Koti RS, Bapat RD. Lymphangioma of the chest wall. J Postgrad Med. 1995;41:89–90. [PubMed] [Google Scholar]
- 6.Dhrif AS, El Euch D, Daghfous M, Cherif F, Mokni M, Dhahri AB. Macrocystic lymphatic lymphangioma (cystic lymphangioma) of upper extremity: A case report. Arch Pediatr. 2008;15:1416–9. doi: 10.1016/j.arcped.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Antoniades K, Kiziridou A, Psimopoulou M. Traumatic cervical cystic hygroma. Int J Oral Maxillofac Surg. 2000;29:47–8. [PubMed] [Google Scholar]
- 8.Selz PA, Arjmand EM. Laryngeal lymphangioma: a case report of an uncommon entity. Otolaryngol Head Neck Surg. 1998;118:382–4. doi: 10.1016/s0194-5998(98)70320-1. [DOI] [PubMed] [Google Scholar]
- 9.Carpenter CT, Pitcher JD, Jr, Davis BJ, Gomez R, Schofield TD, Youngberg RA. Cystic hygroma of arm: A case report and review of literature. Skeletal Radiol. 1996;25:201–4. doi: 10.1007/s002560050064. [DOI] [PubMed] [Google Scholar]
- 10.Oak SN, Redkar RG, Kapur VK. Posterior midline cervical fetal cystic hygroma. J Postgrad Med. 1992;38:93–6. [PubMed] [Google Scholar]
- 11.Mansingani S, Desai N, Pancholi A, Prajapati A, Vohra PA, Raniga S. A case of axillary cystic hygroma. Indian J Radiol Imag. 2005;15:517–9. [Google Scholar]
- 12.Arora A, Narula MK, Sonkar P, Chadha R. Cystic hygroma of chest wall. Indian J Radiol Imag. 2003;13:120–1. [Google Scholar]
- 13.Descamps P, Jourdian O, Paillet C, Toutain A, Guichet A, Pourcelot D. Etiology, prognosis and management of nuchal cystic hygroma: 25 new cases and literature review. Europ J Obstet Gyenecol Reprod Biolog. 1997;71:3–10. doi: 10.1016/s0301-2115(96)02590-0. [DOI] [PubMed] [Google Scholar]
- 14.Gustavii B, Ecivall H. First trimester diagnosis of cystic nuchal hygroma. Acta Obstet Gynecol Scand. 1984;63:377–80. doi: 10.3109/00016348409155537. [DOI] [PubMed] [Google Scholar]
- 15.Zanotti SD, LaRusso S, Coulson C. Prenatal sonographic diagnosis of axillary cystic lymphangiomas. J Clin Ultrasound. 2001;29:112–5. doi: 10.1002/1097-0096(200102)29:2<112::AID-JCU1009>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim AH, Kandeel A, Bazeed MF. Successful non surgical management of a huge life threatening cervicomediastinal cystic hygroma case report and review of the literature. J Pediatr Surg Specialt. 2009;3:48–50. [Google Scholar]
- 17.Sheila S, Nazarian-Mobin, Simms K, Urata MM, Tarczy-Hornoch K, Jeffrey A. Misleading presentation of an orbital lymphangioma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:82–5. doi: 10.1016/j.tripleo.2009.08.042. [DOI] [PubMed] [Google Scholar]
- 18.Sobol SE, Manoukian JJ. Acute airway obstruction from a laryngeal lymphangioma in a child. Int J Pediatr Otorhynolaryngol. 2001;58:255–7. doi: 10.1016/s0165-5876(01)00433-5. [DOI] [PubMed] [Google Scholar]
- 19.Ameh EA, Nmadu PT. Cervical cystic hygroma: Pre, intra and postoperative morbidity and mortality in Zaria, Nigeria. Pediatr Surg Int. 2001;17:342–3. doi: 10.1007/s003830000558. [DOI] [PubMed] [Google Scholar]
- 20.Mahajan JK, Bharathi V, Chowdhary SK, Samujh R, Menon P, Rao KL. Bleomycin as intralesional sclerosant for cystic hygromas. J Indian Assoc Pediatr Surg. 2004;9:3–7. [Google Scholar]
- 21.Yura J, Hashimoto T, Tsuruga N. Bleomycin treatment for cystic hygroma in children. Arch Jpn Chir. 1977;46:607–14. [PubMed] [Google Scholar]
- 22.Okada A, Kubota A, Fukuzawa M, Imura K, Kamata S. Injection of bleomycin as a primary therapy of cystic lymphangioma. J Pediatr Surg. 1992;27:440–3. doi: 10.1016/0022-3468(92)90331-z. [DOI] [PubMed] [Google Scholar]
- 23.Orford J, Barker A, Thonell S, King P, Murphy J. Bleomycin therapy for cystic hygroma. J Pediatr Surg. 1995;30:1282–7. doi: 10.1016/0022-3468(95)90485-9. [DOI] [PubMed] [Google Scholar]
- 24.Zhong PQ, Xhi FX, Li R, Xue JL, Shu GY. Long-term results of intratumorous bleomucin-A5 injection for head and neck lymphangioma. Oral Surg Oral Med Oral Pathol Oral Radiol Endodnone. 1998;86:139–44. doi: 10.1016/s1079-2104(98)90115-9. [DOI] [PubMed] [Google Scholar]
- 25.Ogita S, Tsuto T, Nakamura K, Deguchi E, Tokiwa K, Iwai N. OK-432 therapy for lymphangioma in children: Why and how does it work? J Pediatr Surg. 1996;31:477–80. doi: 10.1016/s0022-3468(96)90478-9. [DOI] [PubMed] [Google Scholar]
- 26.Katsuno S, Ezawa S, Minemura T. Excision of cervical cystic lymphangioma using injection of hydrocolloid dental impression material, a technical case report. Int J Oral Maxillofac Surg. 1999;28:295–6. [PubMed] [Google Scholar]
- 27.Bozkaya S, Ugar D, Karaka I, Ceylan A, Uslu S, Baris E, et al. The treatment of lymphangioma in the buccal mucosa by radiofrequency ablation: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28–31. doi: 10.1016/j.tripleo.2006.03.007. [DOI] [PubMed] [Google Scholar]


