Abstract
A 14-year-girl presented with solitary exuberant warty plaque over her right great toe since the age of 4 years. Ten years ago, an excisional biopsy was performed by a surgeon, and a histopathological diagnosis of angiokeratoma was made. A wide local excision of the lesion followed by a plantar digital artery flap in a V-Y fashion adjacent and just proximal to the excision wound was performed. This procedure has not only led to complete growth removal, but also a well-preserved digit with an excellent color and contour match.
Keywords: Flaps, verrucous hemangioma, graft, wide excision
INTRODUCTION
Verrucous hemangioma is a rare variety of angiomatous nevi usually involving the, lower extremities. It has been reported under a diversity of names such as angiokeratoma circum-scriptum neviforme, unilateral verrucous heman-gioma, keratotic hemangioma etc.
They are best treated by excision while still small, as they enlarge with body growth and do not regress spontaneously. In contrast to angiokeratomas, which respond to various means of therapy (e.g., cryotherapy, electrocautery, and argon laser), verrucous hemangiomas require a large, deep excision as a superficial therapeutic approach would be unsuccessful because of the deep angiomatous proliferation.[1]
CASE REPORT
A 14-year-old girl presented with an exuberant warty brownish growth on her right great toe. History revealed that when she was 4 years old, she had a small similar lesion, a part of which was biopsied by a general surgeon and was reported as angiokeratoma. The patient was then lost for follow-up. Over the next 10 years, the lesion recurred and continued to grow in a slow but progressive manner to the present size without any treatment.
Examination revealed a solitary hyperpigmented, hyperkeratotic plaque consisting of closely set warty papules measuring 20 × 25 mm2 involving the pulp space of the right great toe. Surface of the lesion was firm and verrucous with no ulceration, bleeding, or atrophy. The lesion was noncompressible, and diascopy was negative. Regional lymph nodes were not enlarged. Systemic examination was normal. Routine laboratory investigations and X-ray chest were also normal.
We considered a clinical differential diagnosis of tuberculosis verrucosa cutis and angiokeratoma [Figure 1]. The entire growth was excised by a wide excision resulting in a defect that involved one-third of the pulp space of the great toe extending till the bone. A plantar digital artery flap was designed in a V-Y fashion adjacent and just proximal to the excision wound. An initial exploring incision was taken, and the digital neurovascular bundle was identified. Skeletonizing this pedicle permitted the elevated flap to advance and cover the excision defect completely with sensate, glabrous plantar skin without any contour defect.
Figure 1.

Hyperpigmented verrucous plaque over the pulp space of the great toe
The excised material was subjected to histological examination. H and E stained sections of the specimen showed marked hyperkeratosis, parakeratosis, papillomatosis, and elongation of the rete ridges. Extending from the dermo-epidermal junction into the deeper dermis, there were numerous small to large vascular channels lined by flattened endothelial cells and filled with blood. A final diagnosis of verrucous hemangioma was confirmed.
DISCUSSION
Verrucous hemangioma is a rare variety of angiomatous nevus usually involving the lower extremities.[1] Lesions are mostly seen at birth or appear during childhood. Initially, they are soft, bluish-red vascular lesions, but with time they enlarge and develop keratotic and verrucous features.[2]
Secondary bleeding and infection are frequent complications, which often result in reactive papillomatosis and hyperkeratosis and thus the older lesions acquire a warty surface.[3] Unlike other angiomatous nevi, they do not involute spontaneously.[4]
Clinically, verrucous hemangioma mimicks angiokeratoma, but histopathologically they can be clearly differentiated as the former involves the dermis and subcutaneous fat and the latter involves only the papillary dermis.[1] Hence, deep excisional surgery is the proper treatment for verrucous hemangioma[5] as a superficial therapeutic approach would be unsuccessful because of the deep angiomatous proliferation.[6] Superficial ablative procedures such as electrocautery, cryosurgery, and laser ablation almost invariably lead to recurrence of the lesion. A combined approach using surgery and erbium laser have been reported with good results.[4]
In our case, as the large defect size would not permit a direct primary closure, either a skin graft or a flap was needed. A skin graft would have had disadvantages such as; (a) uncertain acceptance on the bare bone with risk of delayed healing, (b) a sunken appearance resulting in poor aesthesis causing social anxiety, and (c) poor tolerance to wear and tear. Although conventional local flaps would heal the wound reliably, loss of the toe contour and the skin graft needed on the flap donor area would leave obvious cosmetic deformity on the young girl's toes.
Therefore, we performed a wide local excision of the growth and closed the defect with a plantar digital artery flap designed in a V-Y fashion[7] just proximal to the excision wound. The donor defect was closed primarily without compression of underlying structures. Excellent color, contour match as well as preservation of sensation in 2 weeks ensured a good aesthetic reconstruction. The digit shape was also preserved to the satisfaction of the patient [Figures 2a–d]
Figure 2.
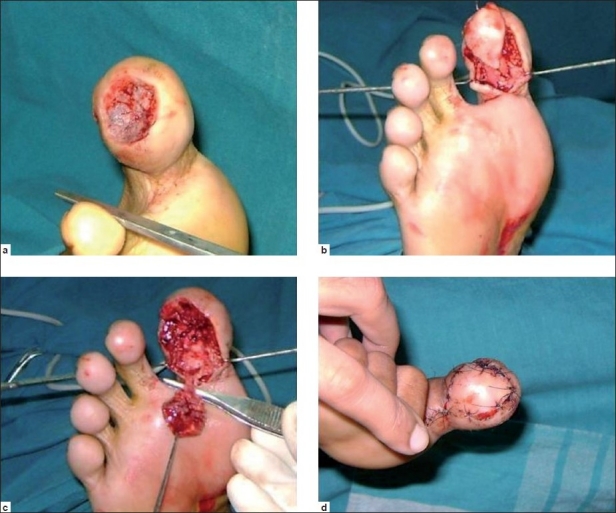
(a) Verrucous growth excised by a wide local excision. (b) A plantar digital artery flap was designed in a V-Y fashion adjacent and just proximal to the excision wound. (c) The pedicle was skeletonized permitting the flap to advance by about 1 cm to cover the entire excision defect. (d) Excised area was then sutured.
Skin lesions needing excisions very often cannot be closed primarily or tension of primary closure results in unacceptable distortion of adjacent anatomic landmarks. While the former problem may present in any area of the body, the latter usually presents on vital areas such as face, hand, foot, or genitals.
When wound healing alone is the concern, simple skin grafts-either partial/split (STSG) or full thickness (FTSG) may suffice. However, these are usually associated with problems of function (unable to tolerate wear and tear, inadequate sensation or contraction of graft) or aesthesis (color or texture mismatch, contour defect).[8]
In this case, there was the additional uncertainty of poor acceptance of the graft on bare bone with the risk of delayed healing. It is in such situations that local flaps are suitable. Although conventional local flaps would heal the wound reliably, loss of the toe contour and the skin graft needed on the flap donor area would leave obvious stigmas on the young girl's toes. This final problem can also be avoided by careful design and dissection of the flap to permit direct closure of flap donor areas, as demonstrated in our case [Figures 3a and b].
Figure 3.

(a) Postoperative status of the great toe with acceptable contour. (b) Postoperative picture with acceptable contour and good aesthetic reconstruction of the great toe
Yang and Ohara reported 14 patients presenting with small, localized lesions that were cured by one session of surgery without recurrence, while the 9 patients with wider and more extensive lesions required combination therapy in several stages for optimal results.[9] Achar et al.[10] reported a case of verrucous hemangioma over the lateral aspect of left leg of a 19-year-old girl, treated with multiple sessions of electrocautery, which healed with scarring and hyperpigmentation.
Sclerotherapy has also been used to make these lesions amenable to easy excision. Roy et al.[11] used percutaneous injection of N-butyl cyanoacrylate (NBCA) prior to excision of the lesion which on contact with tissue fluid, causes inter compartmental tissue adhesion, thereby causing cessation of blood flow into the vascular malformation tissue. After few injections, the whole mass forms a solid polymer, which is then excised. During excision, there is remarkably minimum bleeding.[11]
When dimensions permit, local flaps are far better than distant flaps in vital areas, on grounds of better function and aesthesis. The limit for local flap dimensions in critical areas is reached when the donor area cannot be closed primarily and is likely to need a skin graft. In areas with axial pattern blood supply, flaps can be islanded and creatively designed to permit larger donor areas to be closed primarily. This ensures the best of wound healing, function, and aesthesis with minimal scars, which is called aesthetic reconstruction.[8]
Ability to restore the toe virtually back to normal permits a fearless and wide excision needed for definitive cure of the disease. This makes aesthetic reconstruction a useful tool in dermatosurgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Imperial R, Helwig EB. Verrucous Hemangioma- A clinicopathologic study of 21 cases. Arch Dermatol. 1967;96:247–53. doi: 10.1001/archderm.96.3.247. [DOI] [PubMed] [Google Scholar]
- 2.Loria PR, Derbes VJ, Krafchuk JD. Keratotic haemangioma. Arch Dermatol. 1958;77:216–9. doi: 10.1001/archderm.1958.01560020070008. [DOI] [PubMed] [Google Scholar]
- 3.Wang G, Li C, Gao T. Verrucous hemangioma. Int J Dermatol. 2004;43:745–6. doi: 10.1111/j.1365-4632.2004.02261.x. [DOI] [PubMed] [Google Scholar]
- 4.Yasar A, Ermertcan AT, Bilac C, Bilac DB, Temiz P, Ozturkcan S. Verrucous hemangioma. Indian J Dermatol Venereol Leprol. 2009;75:528–30. doi: 10.4103/0378-6323.55415. [DOI] [PubMed] [Google Scholar]
- 5.Utta W, Rudolf H. Linear verrucous hemangioma. J Am Acad Dermatol. 2000;42:516–8. doi: 10.1016/s0190-9622(00)90232-9. [DOI] [PubMed] [Google Scholar]
- 6.Niechajev IA, Sternby NH. Cutaneous keratotic hemangioma. Scand J Plast Reconstr Surg. 1983;17:153–4. doi: 10.3109/02844318309013112. [DOI] [PubMed] [Google Scholar]
- 7.Flint MH, Harrison SH. A Local neurovascular flap to repair the digit pulp. Br J Plast Surg. 1965;18:156–63. doi: 10.1016/s0007-1226(65)80020-0. [DOI] [PubMed] [Google Scholar]
- 8.Mathes SJ. Flap classifications and applications. In: Mathes SJ, editor. Textbook of plastic Surgery. 2nd ed. Philadelphia: Elsevier and Saunders; 2006. pp. 365–482. [Google Scholar]
- 9.Yang CH, Ohara K. Successful surgical treatment of verrucous hemangioma: A combined approach. Dermatol Surg. 2002;28:913–9. doi: 10.1046/j.1524-4725.2002.02061.x. [DOI] [PubMed] [Google Scholar]
- 10.Achar A, Biswas SK, Maity AK, Naskar B. Verrucous hemangioma treated with electrocautory. Indian J Dermatol. 2009;54:51–2. [Google Scholar]
- 11.Roy AK, Majumdar BK, Majumdar S. Management of unresolved hemangiomas and venous malformations by N-butyl cyanoacrylate. Indian J Plast Surg. 2007;40:8–11. [Google Scholar]


