Abstract
Treatment of thoracolumbar fractures is still controversial. Several treatment options are reported to yield satisfactory results. There is no evidence indicating superiority of any treatment option. We have already presented radiological results of the use of PLIF/TLIF in trauma, which showed satisfactory results concerning intervertebral fusion and acceptable loss of correction. We examined 50 patients regarding loss of correction after implant removal and clinical outcome using a validated visual analogue score. The average time of follow-up (FU) was 35 months. We observed a total loss of correction of 4°. The pre-injury mean VAS score was 92. At FU, there was an average reduction of 17.2 points. Owing to the presented results, we suggest this method as an alternative to combined procedures.
Keywords: Thoracolumbar trauma, PLIF/TLIF, Intervertebral fusion, Single posterior approach
Introduction
Treatment of thoracolumbar fractures is still controversial. Several treatment options, such as posterior reduction and stabilization with or without posterolateral fusion, combined procedures using bony strut grafts or titanium implants with or without additional anterior plating for anterior reconstruction, isolated anterior procedures and conservative treatment with or without bracing are reported to yield satisfactory outcomes, typically in A3-type fractures [1, 7, 9, 13, 23, 28, 32, 34, 35, 49, 57, 61]. There is no evidence indicating superiority of any treatment option [4, 11, 14, 17, 19, 21, 26, 31, 45, 51–53, 56, 60, 61].
Combined procedures produce the best radiological results; however, the clinical results measured with different scores were not superior to posterior fixations alone and may, therefore, not be justified in many cases [26, 31, 45]. Guidelines based on the level 1 studies of when and how the anterior column should be additionally reconstructed surgically do not exist up to date [10, 19, 21, 36, 53–56, 59]. 360° fusions are considered to be necessary in cases with “unstable” burst fractures and more severe bony destruction [5, 11, 25, 26, 28, 31–33, 45, 47, 53, 58].
Regardless of an additional treatment of the anterior column, short segmented posterior reduction and stabilization is considered to be the first step in the vast majority of spinal trauma surgeries.
We have already presented first radiological results of a PLIF/TLIF technique in Trauma. With this technique, it is possible to restore the anterior column by a single posterior approach [48].
In this prospective observational study, we evaluated the mid-term results with regard to a possible radiological loss of correction some months after implant removal and clinical results using the VAS score.
Materials and methods
Between 2001 and 2005, 100 out of a total of 316 trauma patients were operated with this PLIF/TLIF-like technique. We enrolled patients with burst fractures (A3.1–A3.3) according to the classification of Magerl [39] that resulted in reduced resistance to compressive forces of the anterior column with or without injuries of the dorsal ligaments from Th11 to S1.
Eighteen patients were not traceable because they were tourists from other countries than Austria.
We followed 82 patients until implant removal (IR). Sixty-seven patients had a CT scan at this time and the rate of successful fusion has been measured and reported previously [51].
We could trace 50 of the initial 100 patients (13 females, 37 males) for this mid-term study in which X-rays and VAS scores were mandatory. All patients of this study had AP and lateral plain X-rays pre- and postoperatively, at implant removal (IR) and at minimum 4 months after IR. Follow-up (FU) X-rays were performed in standing position. Fractures were classified based on the X-rays and CT scans on first admission.
Forty-two out of these fifty patients had a CT scan at the time of IR completion.
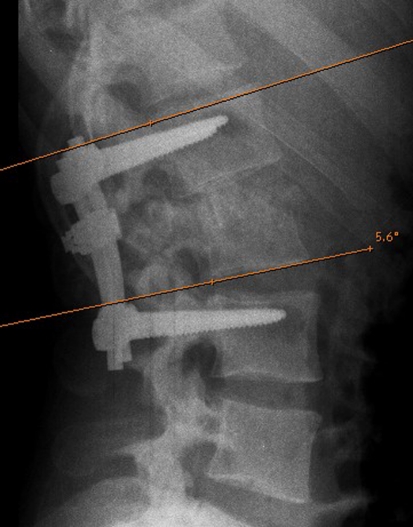
Monosegmental angles were measured as endplate angles between both endplates adjacent to the fused motion segment (Fig. 1) on lateral plain X-rays [28, 46, 51]. Positive values describe lordotic angles, whereas the negative values the kyphotic angles.
Fig. 1.
Segmental angle was measured between both endplates adjacent to the fused segment in the lateral view
Frankel/ASIA score was used to describe the neurological findings [2, 16].
Within a week after the accident, patients were asked to complete VAS scoring to the best of their knowledge for the time before the injury. The same score was used at the last FU. We used a validated visual analogue scale that consists out of 19 questions (0–100, 100 best score, no pain, no complaints). The value used represents the mean value of all answered questions [30].
Surgical technique
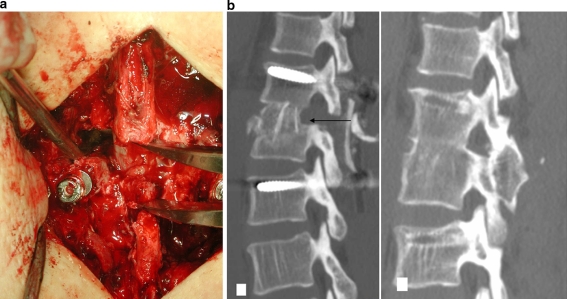
We performed a unilateral PLIF (below L2) or TLIF (at the thoracolumbar junction) procedure (Fig. 2). Displaced posterior wall fragments were removed or pushed forward to decompress the spinal canal. Following the partial resections of the intervertebral disc, monocortical strut graft and cancellous bone, harvested at the posterior iliac crest, are shaped and tapped in. Slight posterior shortening and compression of the posterior elements using an internal fixator (USS™ pedicle screw System, Synthes Medical, Oberdorf, Switzerland) was carried out to improve the contact between the grafts and the vertebral endplates and also to create the desired amount of reduction and segmental lordosis. Posterior fusion with autogenous bone was performed in all cases. If drainages are used, they are removed on the second day postoperatively, and the patient is mobilised without any brace.
Fig. 2.
a Intraoperative photo shows the interspinal spreader in position. The transforaminal approach to the disc space is lateral to the dural sac. The dura is to be seen in the distracted interspinal/laminar area of one segment only. b A incomplete cranial burst fracture (A3.1.1) of L1 is instrumented bisegmental. The arrow shows the transforaminal approach with the resection of the upper articular process and the posterior rim of the vertebral body. The monocortical bone graft is brought in longitudinal direction and shows good contact to the endplates. CT scan after the IR shows successful intervertebral and posterior fusion with satisfactory alignment
Statistics
SPSS 15.0 (SPSS, Chicago, IL, USA) was used for statistical analysis. For independent samples, a t test for independent samples or a non-parametric Mann–Whitney test was performed. For paired samples, a paired t test or a non-parametric Wilcoxon’s test was used. The Kolmogorov–Smirnov test was used for determination of the distribution form. The probability level was set at p < 0.05.
Results
Sport injuries (n = 23) were the predominant cause of injury, followed by falls from a height (n = 15), traffic accidents (n = 11) and one direct trauma. The mean time between trauma and operation was 3.5 days (range 0–28). All patients had acute fractures and were treated within 3 weeks, with the exception of one patient that had extensive pulmonary problems (trauma-op 28 days).
The mean age at the time of trauma was 31.8 (range 17–59) and the average FU time was 35 months (range 13–81).
There were three patients with a FU of 4 months after IR. Two of them had an entire FU period of 27 and 38 months. One patient was observed for 13 months alone. He had a complete paraplegia and we were not able to motivate him for further FU examinations.
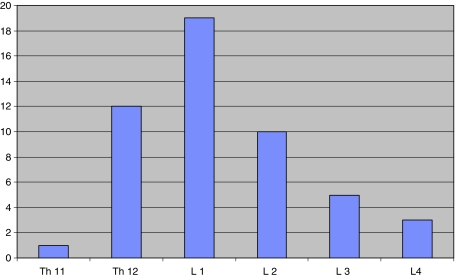
The first lumbar vertebra was affected in19 cases, followed by TH12 and L2 (Figs. 3, 4).
Fig. 3.
Diagram shows distribution of affected levels with a peak at L1
Fig. 4.
a–j A 41-year-old male patient who fell from a ladder. He suffered an incomplete cranial burst fracture of the first lumbar vertebra without any neurological lesions. We performed a PLIF procedure and could achieve physiological reduction. The CT scan after IR shows successful intervertebral bony bridging and dorsal fusion. The last XR in standing position presents lordotic alignment with minimal loss of correction of 2°
According to the classification of Magerl, we treated 17 A3.1, 30 A3.2 and 3 A3.3 fractures. Ten cases of them showed additional B-type lesions and two cases showed signs of a rotational injury (type C).
Bisegmental instrumentation was performed in 27 patients, 20 patients were instrumented monosegmental and 3 tri-segmental. In all cases, PLIF procedure has been done monosegmentally.
The mean narrowing of the spinal canal on admission was 30% (0–100) as compared to the adjacent segments. After the decompression, we found 8% (0–50) of narrowing.
The mean monosegmental angle on admission was −12.8° (−39 to 13). The average postoperative angle was 2.6° (−12 to 18). The initial correction of the posttraumatic kyphosis was 15.5°. At the time of IR, we found a mean angle of 0° (−20 to 13) and at the last FU, the average angle was −1.4° (−20 to 14). Hence, there was a total loss of 4° (−20 to 24). This is a loss of 25% as compared to the initial reduction.
In fractures of the thoracolumbar junction (Th11–L1), the loss of correction was 3.6° (SD 4.4), in fractures of the second lumbar vertebra 4.2° (SD 3.4) and in fractures of L3 and L4 5° (SD 0.7).
Thus, the final result at the thoracolumbar junction was −4.7° (SD 6.2), at L2 1.2° (SD 4.8) and in L3 and L4 7.1° (SD 3.4) (Table 1).
Table 1.
The radiological course of the different fracture levels is presented, as well as the follow-up time and the VAS score at last FU
| Levels | n | Preop. | Radiological follow-up (°) | FU time (months) | FU VAS | ||
|---|---|---|---|---|---|---|---|
| Postop. | IR | FU | |||||
| Th11/Th12/L1 | 31 | −15 | −1 | −4.1 | −4.6 | 34 | 76.5 |
| L2 | 10 | −9.2 | 5.4 | 3.4 | 1.2 | 39.2 | 75 |
| L3/L4 | 9 | −6.3 | 12.2 | 8.7 | 7.1 | 34.4 | 68.2 |
| Total | 50 | −12.8 | 2.6 | −0.3 | −1.4 | 35 | 74.8 |
Monosegmentally, instrumented fractures lost mean 4.6°, bi-segmentally instrumented lesions loss mean 3.6° and tri-segmental instrumentations loss mean 3.2°. The difference between those groups did not reach any statistical difference.
CT scans at the time of the IR were available of 42 patients. There was a successful intervertebral fusion in 36 patients (85%). The posterior fusion rate was 95%. Fusion was defined using the criteria of McAfee et al. [40]. Patients with a successful anterior fusion lost mean 3.4° (SD 4.3) and those without fusion showed a loss of 5.5° (SD 4.2). No statistical difference could be reached (p ≥ 0.05). Two patients did not show a dorsal fusion and one of them did not show any ventral fusion too [51]. They lost mean at 14°.
The average time of surgery was 192 min (range 120–360), and mean blood loss was 790 ml (range 300–3,400 ml). There were 6 patients with blood loss >1,000 ml. All of them had a neurological impairment and, therefore, were decompressed acutely.
The pre-injury VAS score was 92 (74–100). At FU, there was a loss of 17.2 points to mean 74.9 (28–100). 21 patients scored higher than 80.
Forty-four patients were almost pain free or complained about mild/occasional problems at the donor site at the iliac crest. Four reported frequent, but mild complaints and two frequent and severe problems.
Nine patients showed an associated neurological deficit on admission. Two patients had a complete paraplegia (Frankel/ASIA A) that did not change till FU. Five patients suffered from an incomplete conus cauda syndrome scored as Frankel/ASIA D with bladder dysfunction. They all improved concerning their motor weakness, but two of them still complained about bladder and sexual dysfunction. Radicular lesions were seen in two patients that resolved completely after decompression.
In this series, we did not have any wound infections. One postoperative epidural haematoma has been revised immediately and remained uneventful. One patient with complete paraplegia suffered from persistent severe radicular pain that did not respond to injections and conservative treatment. In this case, we did a rhizotomy and the pain resolved. By this procedure, no additional motor weakness occurred.
Discussion
Main goals of the surgical treatment of spinal injuries are a definitive restoration of the spinal alignment [1, 11] with as short as possible instrumentations [1, 38, 41, 43], high fusion rates and the decompression of neural structures in case of narrowing to facilitate functional recovery.
Anterior or combined approaches with anterior decompression provide satisfactory decompression of the spinal canal, good reconstruction of the anterior column using tri-cortical strut grafts or cages and solid fusions [5, 26, 28, 31]. Biomechanical investigations have shown that 360° fusions provide better stability as compared to posterior instrumentations only [22, 25, 29, 47].
However, anterior approaches yield a higher risk of surgical complications than posterior approaches [15, 26, 45] and isolated anterior fusions may fail in cases with disrupted posterior stabilizing elements [53].
The presented method achieves reduction, decompression and a “biological” anterior interbody fusion all from a posterior approach only.
After posterior instrumentation, we approach the anterior column via a partial hemilaminectomy and complete or partial resection of the articular process. The intervertebral disc is partially removed. Posterior wall fragments narrowing the spinal canal can be pushed forward or removed. The intervertebral space is filled with cancellous bone and monocortical strut grafts.
Our patient cohort is similar to other studies concerning gender ratio with 13 females and 37 males [14, 17, 20, 27, 44]. There is also a well-known distribution of affected levels with the peak at the first lumbar vertebra. All of our patients suffered from burst fractures according to Magerl [39]. The A3 type is the most common fracture type of the thoracolumbar transition and the lumbar spine. There were 10 B-type lesions and only 2 C-type lesions. Concerning the C-type lesion this is less than reported elsewhere, but the B-type distribution is comparable with other studies [27, 28, 44].
Our patients are younger (31.8a) than those reported by Reinhold et al. [44.] One explanation of this phenomenon could be the high amount of sports injuries (n = 23) in this group. Traffic injuries (n = 11) and falls from a height (n = 15) are less as compared to other reports [27, 44].
Eighteen percent of our patients showed a neurological deficit on admission. This is less than reported by Reinhold et al. (38.5%) [44], but comparable with Knop et al. (22%) [24, 27]. Seven of nine patients improved concerning their motor weakness. There is a tendency towards the reported recovery rates of Knop et al. [28]. The literature of recovery rates is inconsistent and varies between 0 and 100% [3, 6, 17, 18, 28, 31, 37].
In accordance with other authors, we favour immediate decompression of the spinal canal in presence of neurological deficits [26, 28, 56].
The need of 360° fusions is still under debate. Reports of unsatisfactory postoperative loss of correction after posterior procedures only compete with papers showing superior clinical results [26, 45]. Korovessis [31] recommends a combined procedure because of better radiological results although patients with a posterior fusion only rated better in the clinical scores VAS and SF-36 as compared to the combined group.
Our patients showed a normal age related pre-injury VAS score of 92 points. We found an average loss of 17.2 points at FU visit. This is comparable to the data of Lange et al. [33] and Knop et al. [28] after combined procedures. When compared with the results of Reinhold et al. [45], our patients scored better in the pre-injury score and had better end scores. Reinhold reported pre-injury scores in the combined group of only 74 points and FU scores of 55.3 points at the thoracolumbar junction and of 40.7 points in the lumbar region.
The initial correction of the posttraumatic deformity was mean 15.5°. The following loss of correction was 4°. Hence, this is comparable to the values of Lange et al. (2.3° loss of correction), Verlaan et al. (5.9°) and Reinhold et al. (3.6°) with combined procedures [28, 33, 45]. The achieved results with −4.7° at the thoracolumbar transition and 1.2° and 7.1° at L2–L4 are comparable with the results of Verlaan et al. [56] and Korovessis et al. [31]. The decompression of the spinal canal from 30 to 8% is effective. Esses et al. reported about 58% in anterior cases and 44.5% in posterior cases with better results of decompression in the anterior group. Reinhold et al. reported about an average posttraumatic narrowing of 34–42 and 9–19% postoperatively, with 19% in the single dorsal and combined group.
The rate of intervertebral anterior fusion in this group (n = 42) is 85% what is comparable to our previous report. The fusion rates in the literature vary widely from 73 to 100% [4, 8, 12, 26, 42, 56].
The largest strut graft, we have used was 25-mm long. In the CT scan after implant removal, we could see a certain amount of loss of volume as described by Morrison et al. [42], but we did not do any further investigations in this direction. We use more than one bone block and additionally fill up the intervertebral space with cancellous bone. Therefore, a precise measurement of the graft volume is not possible.
We did not see any correlation between graft size and failed fusion. The reasons of failure are more often inadequate graft endplate contact or graft bed irritation by screws [51].
The presented method offers some advantages especially in acute cases which need immediate stabilization and decompression. The dural sac and entrapped nerve roots can be decompressed under direct visualisation and dural tears can be addressed by suturing. Hence, the spinal canal is already explored and the disc space is identified. Only a few operative steps more are necessary to reconstruct the anterior column.
Intraoperative bleeding due to the fractured vertebra and torn epidural veins have to be addressed using cell saving systems and carefully dissection and coagulation. In most cases, the bleeding stops at the moment the retropulsed fragment is pushed anteriorly.
In non-emergency cases without the need of spinal canal decompression, there is a risk of iatrogenic lesions of the dural sac and nerve roots as well as epidural bleeding. We always try to work as far as lateral as possible to avoid complications with the neural structures that we have under direct visualisation. After the presented results, we think that it is a feasible approach to the anterior column.
Sassani et al. [50] and Haiyun et al. [19] reported about three column reconstruction using expandable and non-expandable cages via a single dorsal approach.
The results of this method concerning loss of correction and VAS score are comparable to combined procedures and, therefore, we suggest this as an alternative procedure, especially in A3.1–A3.2 fractures. Complete burst fractures or bi-segmental lesions should be treated dorsoventrally, as well as fractures with bone defects that need grafts longer than 25 mm.
Our experience with “osteoporotic patients” is marginal. In the first paper with more than 80 patients, there were only 3 older than 65 years. However, we do not believe that this technique is recommendable for patients with poor bone quality, as we need corticocancellous bone blocks that are able to withstand the load exerted through the anterior column with the posterior instrumentation in place.
There are some limitations of our paper: there is a lack of a comparison group and only half of the initially included patients were seen personally and evaluated for mid-term FU.
References
- 1.Aebi M, Etter C, Kehl T, Thalgott J. The internal skeletal fixation system. A new treatment of thoracolumbar fractures and other spinal disorders. Clin Orthop Relat Res. 1988;227:30–43. [PubMed] [Google Scholar]
- 2.American Spinal Injuries Association (1992) ASIA Classification. Standards for neurological and functional classification of spinal cord injury. Chicago
- 3.An HS, Vaccaro A, Cotler JM, Lin S. Low lumbar burst fractures. Comparison among body cast, Harrington rod, Luque rod, and Steffee plate. Spine (Phila Pa 1976) 1991;16:S440–S444. [PubMed] [Google Scholar]
- 4.Been HD, Bouma GJ. Comparison of two types of surgery for thoraco-lumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir (Wien) 1999;141:349–357. doi: 10.1007/s007010050310. [DOI] [PubMed] [Google Scholar]
- 5.Beisse R. Endoscopic surgery on the thoracolumbar junction of the spine. Eur Spine J. 2006;15:687–704. doi: 10.1007/s00586-005-0994-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blauth M, Tscherne H, Haas N. Therapeutic concept and results of operative treatment in acute trauma of the thoracic and lumbar spine: the Hannover experience. J Orthop Trauma. 1987;1:240–252. doi: 10.1097/00005131-198701030-00009. [DOI] [PubMed] [Google Scholar]
- 7.Briem D, Linhart W, Lehmann W, Bullinger M, Schoder V, Meenen NM, Windolf J, Rueger JM. Investigation of the health-related quality of life after a dorso ventral stabilization of the thoracolumbar junction. Unfallchirurg. 2003;106:625–632. doi: 10.1007/s00113-003-0627-4. [DOI] [PubMed] [Google Scholar]
- 8.Briem D, Rueger JM, Linhart W. Osseous integration of autogenous bone grafts following combined dorso-ventral instrumentation of unstable thoracolumbar spine fractures. Unfallchirurg. 2003;106:195–203. doi: 10.1007/s00113-002-0508-2. [DOI] [PubMed] [Google Scholar]
- 9.Cantor JB, Lebwohl NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine (Phila Pa 1976) 1993;18:971–976. doi: 10.1097/00007632-199306150-00004. [DOI] [PubMed] [Google Scholar]
- 10.Dai LY, Jiang SD, Wang XY, Jiang LS. A review of the management of thoracolumbar burst fractures. Surg Neurol. 2007;67:221–231. doi: 10.1016/j.surneu.2006.08.081. [DOI] [PubMed] [Google Scholar]
- 11.Daniaux H, Seykora P, Genelin A, Lang T, Kathrein A. Application of posterior plating and modifications in thoracolumbar spine injuries: indication, techniques, and results. Spine. 1991;16:S125–S133. doi: 10.1097/00007632-199103001-00018. [DOI] [PubMed] [Google Scholar]
- 12.Defino HL, Rodriguez-Fuentes AE. Treatment of fractures of the thoracolumbar spine by combined anteroposterior fixation using the Harms method. Eur Spine J. 1998;7:187–194. doi: 10.1007/s005860050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Denis F, Armstrong GW, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984;184:142–149. [PubMed] [Google Scholar]
- 14.Dickman CA, Yahiro MA, Lu HT, Melkerson MN. Surgical treatment alternatives for fixation of unstable fractures of the thoracic and lumbar spine. A meta-analysis. Spine. 1994;19:2266S–2273S. doi: 10.1097/00007632-199410151-00003. [DOI] [PubMed] [Google Scholar]
- 15.Esses SI, Botsford DJ, Kostuik JP. Evaluation of surgical treatment for burst fractures. Spine. 1990;15:667–673. doi: 10.1097/00007632-199007000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 17.Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine. 1992;17:528–540. doi: 10.1097/00007632-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Haas N, Blauth M, Tscherne H. Anterior plating in thoracolumbar spine injuries. Indication, technique, and results. Spine. 1991;16:S100–S111. doi: 10.1097/00007632-199103001-00015. [DOI] [PubMed] [Google Scholar]
- 19.Haiyun Y, Rui G, Shucai D, Zhanhua J, Xiaolin Z, Xin L, Xue W, Gongyi L, Jiankun L. Three-column reconstruction through single posterior approach for the treatment of unstable thoracolumbar fracture. Spine (Phila Pa 1976) 2010;35:E295–E302. doi: 10.1097/BRS.0b013e3181c392b9. [DOI] [PubMed] [Google Scholar]
- 20.Hebert JS, Burnham RS. The effect of polytrauma in persons with traumatic spine injury. A prospective database of spine fractures. Spine. 2000;25:55–60. doi: 10.1097/00007632-200001010-00011. [DOI] [PubMed] [Google Scholar]
- 21.Hitchon PW, Torner J, Eichholz KM, Beeler SN. Comparison of anterolateral and posterior approaches in the management of thoracolumbar burst fractures. J Neurosurg Spine. 2006;5:117–125. doi: 10.3171/spi.2006.5.2.117. [DOI] [PubMed] [Google Scholar]
- 22.Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997;79:69–83. doi: 10.2106/00004623-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Knight RQ, Stornelli DP, Chan DP, Devanny JR, Jackson KV. Comparison of operative versus nonoperative treatment of lumbar burst fractures. Clin Orthop Relat Res. 1993;293:112–121. [PubMed] [Google Scholar]
- 24.Knop C, Bastian L, Lange U, Blauth M. Transpedicular fusion of the thoraco-lumbar junction. Clinical, radiographic and CT results. Orthopade. 1999;28:703–713. doi: 10.1007/s001320050400. [DOI] [PubMed] [Google Scholar]
- 25.Knop C, Blauth M. Bisegmental stability and Synex. Unfallchirurg. 2003;106:259–261. doi: 10.1007/s00113-003-0588-7. [DOI] [PubMed] [Google Scholar]
- 26.Knop C, Blauth M, Buhren V, Arand M, Egbers HJ, Hax PM, Nothwang J, Oestern HJ, Pizanis A, Roth R, Weckbach A, Wentzensen A. Surgical treatment of injuries of the thoracolumbar transition–3: follow-up examination. Results of a prospective multi-center study by the “Spinal” Study Group of the German Society of Trauma Surgery. Unfallchirurg. 2001;104:583–600. doi: 10.1007/s001130170089. [DOI] [PubMed] [Google Scholar]
- 27.Knop C, Blauth M, Buhren V, Hax PM, Kinzl L, Mutschler W, Pommer A, Ulrich C, Wagner S, Weckbach A, Wentzensen A, Worsdorfer O. Surgical treatment of injuries of the thoracolumbar transition. 1: Epidemiology. Unfallchirurg. 1999;102:924–935. doi: 10.1007/s001130050507. [DOI] [PubMed] [Google Scholar]
- 28.Knop C, Kranabetter T, Reinhold M, Blauth M. Combined posterior-anterior stabilisation of thoracolumbar injuries utilising a vertebral body replacing implant. Eur Spine J. 2009;18:949–963. doi: 10.1007/s00586-009-0970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knop C, Lange U, Bastian L, Blauth M. Three-dimensional motion analysis with Synex. Comparative biomechanical test series with a new vertebral body replacement for the thoracolumbar spine. Eur Spine J. 2000;9:472–485. doi: 10.1007/s005860000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knop C, Oeser M, Bastian L, Lange U, Zdichavsky M, Blauth M. Development and validation of the Visual Analogue Scale (VAS) Spine Score. Unfallchirurg. 2001;104:488–497. doi: 10.1007/s001130170111. [DOI] [PubMed] [Google Scholar]
- 31.Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2–L4) burst fractures. Spine. 2006;31:859–868. doi: 10.1097/01.brs.0000209251.65417.16. [DOI] [PubMed] [Google Scholar]
- 32.Kossmann T, Ertel W, Platz A, Trentz O (1999) Combined surgery for fractures of the thoraco-lumbar junction using the inlay-span method [Die kombinierte Operation von Frakturen des thorakolumbalen Ubergangs mit der Inlay-Span-Technik]. Orthopade 28:432–440 [DOI] [PubMed]
- 33.Lange U, Edeling S, Knop C, Bastian L, Krettek C, Blauth M. Titanium vertebral body replacement of adjustable size. A prospective clinical trial. Unfallchirurg. 2006;109:733–742. doi: 10.1007/s00113-006-1090-9. [DOI] [PubMed] [Google Scholar]
- 34.Leferink VJ, Keizer HJ, Oosterhuis JK, Sluis CK, ten Duis HJ. Functional outcome in patients with thoracolumbar burst fractures treated with dorsal instrumentation and transpedicular cancellous bone grafting. Eur Spine J. 2003;12:261–267. doi: 10.1007/s00586-002-0518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leferink VJ, Zimmerman KW, Veldhuis EF, ten Vergert EM, ten Duis HJ. Thoracolumbar spinal fractures: radiological results of transpedicular fixation combined with transpedicular cancellous bone graft and posterior fusion in 183 patients. Eur Spine J. 2001;10:517–523. doi: 10.1007/s005860100319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liao JC, Fan KF, Keorochana G, Chen WJ, Chen LH. Transpedicular grafting after short-segment pedicle instrumentation for thoracolumbar burst fracture: calcium sulfate cement versus autogenous iliac bone graft. Spine (Phila Pa 1976) 2010;35:1482–1488. doi: 10.1097/BRS.0b013e3181c176f8. [DOI] [PubMed] [Google Scholar]
- 37.Liljenqvist U, Mommsen U (1995) Surgical treatment of thoracolumbar spinal fractures with internal fixator and transpedicular spongiosa-plasty [Die operative Behandlung thorakolumbaler Wirbelsaulenverletzungen mit dem Fixateur interne und transpedikularer Spongiosaplastik] Unfallchirurgie 21:30–39 [DOI] [PubMed]
- 38.Lindsey RW, Dick W. The fixateur interne in the reduction and stabilization of thoracolumbar spine fractures in patients with neurologic deficit. Spine (Phila Pa 1976) 1991;16:S140–S145. doi: 10.1097/00007632-199103001-00020. [DOI] [PubMed] [Google Scholar]
- 39.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 40.McAfee PC, Boden SD, Brantigan JW, Fraser RD, Kuslich SD, Oxland TR, Panjabi MM, Ray CD, Zdeblick TA. Symposium: a critical discrepancy—a criteria of successful arthrodesis following interbody spinal fusions. Spine. 2001;26:320–334. doi: 10.1097/00007632-200102010-00020. [DOI] [PubMed] [Google Scholar]
- 41.McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1993;75:162–167. doi: 10.2106/00004623-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 42.Morrison RH, Thierolf A, Weckbach A. Volumetric changes of iliac crest autografts used to reconstruct the anterior column in thoracolumbar fractures: a follow-up using CT scans. Spine. 2007;32:3030–3035. doi: 10.1097/BRS.0b013e31815cdeae. [DOI] [PubMed] [Google Scholar]
- 43.Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine (Phila Pa 1976) 2000;25:1157–1170. doi: 10.1097/00007632-200005010-00018. [DOI] [PubMed] [Google Scholar]
- 44.Reinhold M, Knop C, Beisse R, Audige L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Buhren V, Blauth M (2008) Operative treatment of traumatic fractures of the thoracic and lumbar spinal column: Part I: Epidemiology. Unfallchirurg 112:33–42, 44, 45 [DOI] [PubMed]
- 45.Reinhold M, Knop C, Beisse R, Audige L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Buhren V, Blauth M. Operative treatment of traumatic fractures of the thoracic and lumbar spinal column: Part III: Follow up data. Unfallchirurg. 2009;112:294–316. doi: 10.1007/s00113-008-1539-0. [DOI] [PubMed] [Google Scholar]
- 46.Reinhold M, Knop C, Beisse R, Audige L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Buhren V, Blauth M (2009) Operative treatment of traumatic fractures of the thorax and lumbar spine: Part II: Surgical treatment and radiological findings. Unfallchirurg 112(2):149–167 [DOI] [PubMed]
- 47.Reinhold M, Schmoelz W, Canto F, Krappinger D, Blauth M, Knop C (2009) A new distractable implant for vertebral body replacement: biomechanical testing of four implants for the thoracolumbar spine. Arch Orthop Trauma Surg [DOI] [PubMed]
- 48.Rene S, Dietmar K, Peter S, Michael B, Anton K. PLIF in thoracolumbar trauma: technique and radiological results. Eur Spine J. 2010;19(7):1079–1086. doi: 10.1007/s00586-010-1362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Resch H, Rabl M, Klampfer H, Ritter E, Povacz P (2000) Surgical vs. conservative treatment of fractures of the thoracolumbar transition [Operative vs. konservative Behandlung von Frakturen des thorakolumbalen Ubergangs] Unfallchirurg 103:281–288 [DOI] [PubMed]
- 50.Sasani M, Ozer AF. Single-stage posterior corpectomy and expandable cage placement for treatment of thoracic or lumbar burst fractures. Spine (Phila Pa 1976) 2009;34:E33–E40. doi: 10.1097/BRS.0b013e318189fcfd. [DOI] [PubMed] [Google Scholar]
- 51.Schmid R, Krappinger D, Seykora P, Blauth M, Kathrein A (2010) Erratum to: PLIF in thoracolumbar trauma: technique and radiological results. Eur Spine J [DOI] [PMC free article] [PubMed]
- 52.Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, Rommens PM, ten Duis HJ, Patka P. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 2006;31:2881–2890. doi: 10.1097/01.brs.0000247804.91869.1e. [DOI] [PubMed] [Google Scholar]
- 53.Vaccaro AR, Lim MR, Hurlbert RJ, Lehman RA, Jr, Harrop J, Fisher DC, Dvorak M, Anderson DG, Zeiller SC, Lee JY, Fehlings MG, Oner FC. Surgical decision making for unstable thoracolumbar spine injuries: results of a consensus panel review by the Spine Trauma Study Group. J Spinal Disord Tech. 2006;19:1–10. doi: 10.1097/01.bsd.0000180080.59559.45. [DOI] [PubMed] [Google Scholar]
- 54.Roer N, Bruyne MC, Bakker FC, Tulder MW, Boers M. Direct medical costs of traumatic thoracolumbar spine fractures. Acta Orthop. 2005;76:662–666. doi: 10.1080/17453670510041745. [DOI] [PubMed] [Google Scholar]
- 55.Roer N, Lange ES, Bakker FC, Vet HC, Tulder MW. Management of traumatic thoracolumbar fractures: a systematic review of the literature. Eur Spine J. 2005;14:527–534. doi: 10.1007/s00586-004-0847-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Verlaan JJ, Diekerhof CH, Buskens E, Tweel I, Verbout AJ, Dhert WJ, Oner FC. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine. 2004;29:803–814. doi: 10.1097/01.BRS.0000116990.31984.A9. [DOI] [PubMed] [Google Scholar]
- 57.Vieweg U, Solch O, Kalff R. Vertebral body replacement system Synex in unstable burst fractures of the thoracic and lumbar spine—a retrospective study with 30 patients. Zentralbl Neurochir. 2003;64:58–64. doi: 10.1055/s-2003-40373. [DOI] [PubMed] [Google Scholar]
- 58.Whitesides TE., Jr Traumatic kyphosis of the thoracolumbar spine. Clin Orthop Relat Res. 1977;128:78–92. [PubMed] [Google Scholar]
- 59.Wild MH, Glees M, Plieschnegger C, Wenda K. Five-year follow-up examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg. 2007;127:335–343. doi: 10.1007/s00402-006-0264-9. [DOI] [PubMed] [Google Scholar]
- 60.Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V, Butterman G. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:773–781. doi: 10.2106/00004623-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 61.Yi L, Jingping B, Gele J, Baoleri X, Taixiang W (2006) Operative versus non-operative treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev CD005079 [DOI] [PubMed]