Abstract
Indirect reduction and fixation is not a new method in the treatment of thoracolumbar burst fractures but the indications and efficacy are controversial. The current study was designed to evaluate the efficacy of indirect reduction without fusion. Sixty-four patients with single-level thoracolumbar burst fractures were identified and treated by this method. The outcome was analyzed by the Frankel method, radiographic measurements, and at the latest follow-up the Denis Pain Scale and Oswestry disability index (ODI) were used to assess back pain and functional outcome. The average follow-up period was 40.1 months. The anterior vertebral height (AVH) was corrected from 55.2 to 97.2% post-operatively and decreased to 88.9% after hardware removal. The posterior vertebral height (PVH) increased from 88.9 to 99.1% post-operatively and decreased slightly after implant removal to 93.7%. The average pre-operative canal compromise was 41.4%, which decreased to 13.7% at last follow-up. Except for three paraplegic patients, neurological status significantly improved or stayed normal in the study’s remaining 61 patients. Fifty-two of sixty-four patients had excellent or good function. At latest follow-up the average ODI score was 16.7 and the Denis pain score improved in all patients but one. Indirect reduction and fixation can not only restore vertebral column structure but also, more importantly, patients’ functional outcome.
Keywords: Thoracic, Lumbar, Burst fracture, Indirect reduction, Treatment outcome
Introduction
Surgical treatments of thoracolumbar burst fractures have included a direct decompressive procedure in combination with fusion. These procedures are typically performed from an anterior, posterior, or combined approach. Additionally, many authors prefer multiple level fusion techniques [6, 13]. These surgical approaches can be traumatic for the patient but are necessary in the management of certain thoracolumbar burst fractures while conservative management may be necessary in yet other burst fractures.
Short-segment pedicle screw instrumentation and indirect reduction is not a new technique in the management of thoracolumbar burst fractures [2, 8, 11]. Recently, short-segment pedicle screw instrumentation has been used without fusion but the inclusion criteria in that study included only Dennis Type-B fractures [4, 5]. This study was designed to evaluate the outcome of thoracolumbar burst fractures managed with indirect reduction and posterior short-segment pedicle screw fixation, without laminectomy and fusion in patients with not only Dennis Type-B fractures but also any burst fracture involving the middle column and having an intact posterior longitudinal ligament (PLL).
Materials and methods
Patient data
From 1998 to 2005, 64 patients with thoracolumbar burst fractures were treated with indirect reduction without fusion. Patient inclusion in this retrospective study consisted of the following criteria: (1) compression of the anterior vertebral column with the vertebral body angle greater than 20° (2) thoracolumbar burst fractures that involved either two or three columns seen on X-ray and CT; and (3) an intact posterior longitudinal ligament. In terms of the AO classification system this included fractures A1.2, 1.3, 2.2, 2.3, 3.3, and C1.3 [9]. Also, A3.2, C1.1, and C1.2 were included if the vertebral body angle was greater than 20°. Patients were excluded if they fell under any of the following criteria: (1) the PLL was damaged, (2) they had previous spine pathology, or (3) they were obese. All patients were then treated by indirect reduction and posterior short-segment pedicle screw fixation without fusion and evaluated.
The patients had follow-ups that ranged from 16 to 108 months, with an average of 40.1 months; the large range of the follow-up period was due to the retrospective nature of the study in which some patients just recently had the procedure. There were 40 male and 24 female patients, ranging from 18 to 70 years in age with an average age of 42.1 years. Thirteen fractures were motor vehicle-related, 44 due to falls from a height, 5 from crush injuries, and 2 due to falling from the standing position. All 64 patients had single-level fractures, and consisted of 1 T11 level injury, 10 T12, 32 L1, 12 L2, 6 L3, and 3 L4 level injuries. Pre-operatively, 23 patients had neurological deficiency. Of these patients, the Frankel method classified three with A, eight with B, seven with C, and five with D. Additionally, 41 patients were classified as E (Table 1). All patients had radiographic studies: X-ray and CT scans. The time to operation after injury averaged 7 days.
Table 1.
Pre-op and last f/u Frankel grade
| Pre-op | No. of cases | Latest f/u | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| A | 3 | 3 | ||||
| B | 8 | 3 | 3 | 2 | ||
| C | 7 | 3 | 4 | |||
| D | 5 | 5 | ||||
| E | 41 | 41 | ||||
| Total | 64 | 3 | 3 | 6 | 52 | |
Surgical technique
All patients underwent surgery in the prone position and under general anesthesia. The midline incision was centered at the injury level and completely exposed the injury and two adjacent levels. After insertion of the pedicle screws, the connecting rods were placed. Distraction of the levels above and below the fracture was used to create tension on the posterior longitudinal ligament, to reduce the fracture by ligamentotaxis. Pedicle screw insertion and reduction were guided by fluoroscopy, and the goal was to get the angles between the two pedicle screws and rods above a combined 180° in order to ideally restore correct lordosis and vertebral alignment. The screws were then tightened in a divergent manner.
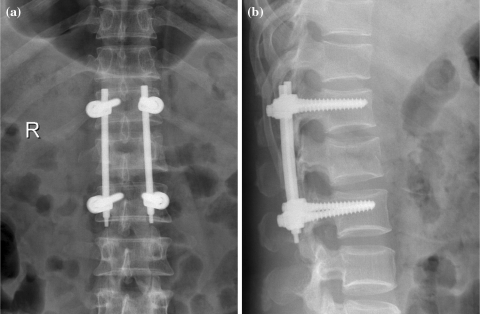
57 patients had instrumentation removal at 9–12 months post-operation. Before removal, X-ray verified the bone was healing, and the patient status was otherwise good (Figs. 1, 2, 3, 4). Healing bone was determined by comparing the density of the anterior column of the injured vertebral body to the adjacent normal vertebral bodies; if the density of the healing body was decreased then a CT was preformed to make sure there was no cavity.
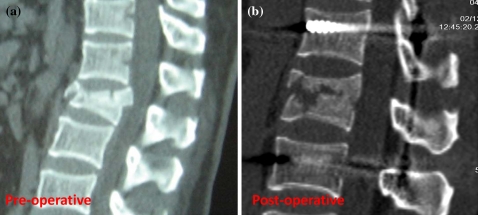
Fig. 1.
Post-operative sagittal CT (b) showing significant restoration of the posterior vertebral height (PVH) and anterior vertebral height (AVH) compared with the pre-operative sagittal CT (a)
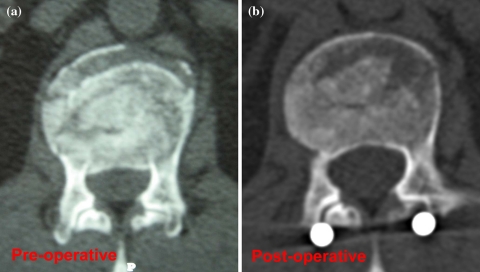
Fig. 2.
Post-operative axial CT view (b) showing significant canal decompression compared with the pre-operative axial CT view (a)
Fig. 3.
Pre-instrumentation removal AP (a) and lateral (b) X-ray views showing intact hardware, restored PVH, AVH, and the healed vertebrae fracture
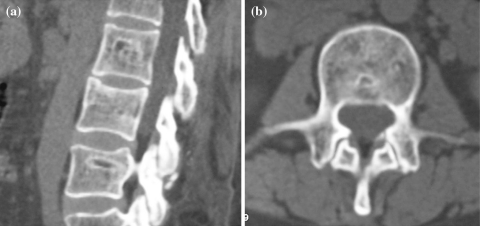
Fig. 4.
Sagittal CT view of a patient 3 years post-instrumentation removal showing a healed fracture and reconstruction of the AVH (a) axial CT view showing complete restoration of canal diameter and preservation of all elements of the posterior spinal column (b)
Seven patients did not have hardware removed between 9 and 12 months post-operatively. In these cases the patients did not want a second operation at that time, feeling satisfied with their function, and felt no significant discomfort from the installed hardware.
Imaging evaluation outcomes
The anterior vertebral height (AVH) and posterior vertebral height (PVH) were measured on lateral radiographs taken pre- and post-operatively, pre-removal, and at the latest follow-up (Table 2). The normal height of the fractured vertebra was determined by averaging the heights of vertebrae at adjacent levels. The vertebral body angle (VBA) was measured from the endplates of the injury level. The local kyphotic angle was found by measuring the difference in Cobb angle from the upper endplate of one vertebral level above the injury to the lower endplate of one vertebral level below the injury level. The sagittal index (SI), which measures kyphotic deformity, was determined by the method of Farcy [7]. Angles for the normal contour of the spine are 5° for thoracic spine, 0° for thoracolumbar, and −10° for lumbar spine. Sagittal index is determined by subtracting the normal angle of a specific spinal level from the deformed kyphotic angle [7]. Spinal canal diameter was measured on the axial cuts of CT scans at the injury level, pre and post-operatively (X). The calculated vertebral spinal canal diameter (Y) was determined by averaging spinal canal diameters of the adjacent vertebrae above and below the injury level (Y1 and Y2). The spinal canal narrowing percent (NR) was thus calculated as (Y − X)/Y × 100%.
Table 2.
Injury level vertebrae AVH and PVH reduction (average %, minimum to maximum)
| Pre-op | Post-op | Pre-removal | Latest | |
|---|---|---|---|---|
| AVH | 55.2 [15.4–83.7] | 97.2 [72.1–112.3] | 94.0 [71.2–107.6] | 88.9 [70.2–103.7] |
| PVH | 88.9 [71.4–98.4] | 99.1 [83.4–108.4] | 97.0 [75.2–106.8] | 93.7 [74.0–101.2] |
Neurological and lumbar function evaluation
The Frankel method, which grades neurological function impairment, was used to compare pre-operative and latest follow-up patient status [10]. The Frankel method is a scale used by the American Spine Injury Association (ASIA) and graded from A to E. ODI was used to determine lumbar function at latest follow-up with 0–25 being excellent, 26–50 good, 51–75 fair, and greater than 75 poor [12, 17]. All data analysis was done by SPSS. The paired t test was used for test statistics between continuous variables, and the accepted alpha-error was set at 0.05. Alpha values were adjusted based on the Bonferroni Correction when necessary.
Results
Of the total 64 patients, 57 patients had removal of instrumentation, and had an inclusive follow-up. The AVH, PVH, VBA, kyphotic angle reduction, and SI are presented in Tables 2 and 3 (Figs. 1, 5). Using paired t test significance testing, the differences between the pre-operative and post-operative numbers were all significant in all groups (P < 0.01). The difference between the pre-removal to latest follow-up numbers was also significant in all groups (P < 0.01). From this observation, there is a statistically significant increase in vertebral correction post-operatively. However, there is also a statistically significant decrease in vertebral correction after implant removal.
Table 3.
Vertebral body angle (VBA), local kyphotic angle (LKA), and sagittal index (SI) (average degrees, minimum to maximum)
| Pre-op | Post-op | Pre-removal | Latest | |
|---|---|---|---|---|
| VBA | 20.3 [4.7–37.8] | 2.6 [−5.4 to 13.3] | 4.6 [0–18.4] | 7.7 [0–21.6] |
| Local kyphotic angle | 18.9 [4.5–39.3] | 0.5 [−8.3 to 15.3] | 3.3 [−4.5 to 16.4] | 10.2 [4–19.2] |
| Sagittal index | 18.9 [0–35.9] | 2.1 [−12.1 to 16.6] | 4.1 [−10.5 to 18.6] | 9.8 [−10 to 24.9] |
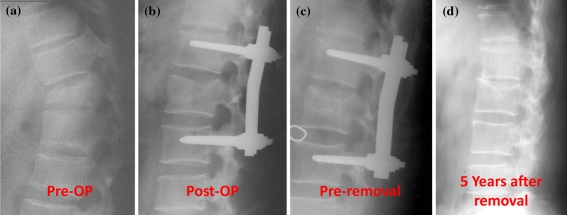
Fig. 5.
L2 fracture ASIA E with anterior column compression treated with indirect reduction and fixation without fusion pre-operatively (a), post-operatively (b), pre-instrumentation removal (c) and 5 years after instrumentation removal (d)
The average calculated normal canal diameter at the injury level (Y) was 18.3 mm. The corresponding pre-operative value was (X1) 11.0 mm, for a spinal canal narrowing percent (NR1) of 41.4%. The latest follow-up values showed that the canal diameter was restored, on average, to 16.1 mm at the injury level (X2). At this follow-up, the canal was compromised (NR2), in AP diameter, about 13.7%. On average, the middle sagittal diameter increased 5.1 mm with reduction. The narrowing ratio (NR) reduction was 27.6% (Fig. 2). Comparisons between pre-operative and latest follow-up values were both significant at P < 0.01.
At latest follow-up, 64 cases were neurologically assessed. Of these cases, 3 were ASIA A, 0 B, 3 C, 6 D, and 52 ASIA E grades. 12 patients, who were graded lower than E, were noted to have bowel or bladder disturbances. The three patients with a pre-operative neurological status of ASIA A had no improvement at latest follow-up, but all other patients had improvement of at least one ASIA grade (Table 1).
Of the patients with Frankel E neurological status, 52 had the Oswestry index functional evaluation at latest follow-up. The functional disorders index mean score was 16.7 ± 18.5 and was graded as excellent in 41, good in 7, and poor in 4 patients. Of these 52 patients, 76.9% had excellent or good function.
Pre-operatively all patients were graded as P4 on the Denis pain scale. At latest follow-up there was pain reduction in all patients but one: 28 P1, 29 P2, 6 P2, and 1 P4. The one patient with a P4 rating was found to have a disk herniation at latest follow-up.
In this series of 64 patients, there were no infections, no neurological deterioration, and no deep venous thrombosis (DVTs). A total of 57 patients had hardware removal. Two patients had implant failure at 10 months, one patient had failure at 12 months and another patient, who did not want hardware removal, was incidentally found to have broken hardware at 48 months. Of these four patients with hardware failure, none reported any pain.
At latest follow-up four screws were not in the ideal location. Three screws had broken the medial wall, but no patient reported any neurological problems. One screw was found to have broken out laterally, but this patient also did not have any neurological problems. After these fractures healed, the screws were removed without any sequelae.
Additionally, after 10–12 months four screws were found to be broken. This included one cranial level screw failure caused by fatigue in two patients and one patient with both cranial screws broken at 12 months.
Discussion
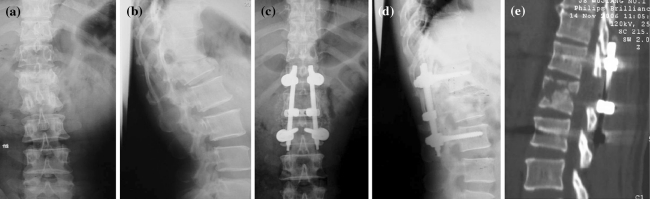
Indirect reduction and fixation without fusion for the treatment of thoracolumbar burst fractures is not considered the standard of care because of the belief that it is not strong and stable enough; however, other authors have reported good results [4, 14, 15] This method of indirect reduction with short pedicle screw fixation without fusion provides another treatment option in managing thoracolumbar burst fractures in which there is an intact PLL and injury to the anterior and middle columns or to the anterior, middle, and posterior columns (Figs. 5, 6). Such a case can be treated by conventional decompression, reduction, fixation, and fusion, either by anterior or posterior approaches, or both, but this may be an overly aggressive technique in a patient with an intact posterior longitudinal ligament and without neurological deficiency.
Fig. 6.
L1 burst fracture ASIA B showing pre-operative AP (a) and lateral (b) X-rays, post-operative AP (c) and lateral (d) X-rays, and a sagittal reconstructed post-operative CT (e) showing an almost normal AVH and PVH
Determination of an intact PLL is difficult to obtain directly from imaging studies; however, a fracture displaced out of the canal, a facet joint that has jumped to another vertebral level, or rotation of the fracture suggests damage to the PLL [16]. Also, determination of an intact PLL can be made while attempting reduction via ligamentotaxis. Pedicle screw insertion parallel to the end plate in the vertebrae above and below the fractured vertebrae and fixation achieved with connecting rods should produce tension on the PLL and subsequent reduction of the fracture by ligamentotaxis. If the fracture does not reduce with this technique it may be because the PLL is damaged and will not provide the tension needed for reduction. Consequently, the traditional method of treatment should be used.
Standard methods of repairing thoracolumbar burst fractures involve laminectomy, which can result in further spinal instability [12, 17]. Indirect reduction both eliminates the possibility of soft tissue scarring, which could compress spinal nerves, and the need for laminectomy, without compromising results as compared with conventional methods such as those utilizing direct reduction, decompression, and fusion. Additionally, fusion methods may result in long-term adjacent level disease [1, 3]. In this study fusion was not done, and after removing instrumentation, the patient had better restored spinal motion and thus a reduced risk of adjacent level disease. Moreover, this method is relatively less invasive and less complicated than conventional anterior approaches.
For patients with neurological deficiency it is routinely thought that direct decompression must occur before reduction of the fracture, but the current results demonstrate that the neurological status does not worsen with indirect reduction without fusion. Furthermore, Yang et al. has previously confirmed the immediate improvement of canal diameter achieved by indirect reduction with short-segment pedicle screw fixation without fusion within 2 weeks post-operatively [16].
Thoracolumbar burst fracture treatment with short-segment pedicle screw fixation has its limitations. Cases in which this technique cannot be used include a ruptured posterior longitudinal ligament or when the vertebral disc has entered the injury level vertebral body. An additional shortcoming of this technique is the need for a second operation to remove hardware.
Also, a few patients had instrumentation failure. A few safety measures can prevent such failure from occurring. First, instrumentation should be removed as soon as healed bone is verified on radiograph. Second, a cooperating patient should be advised to take precaution during weight bearing and daily activities. Third, improved instrument design can help against such failure. This technique should not be used for treating obese patients because there is a risk of hardware failure.
There are other prospective studies, which have reported on short-segment pedicle screw fixation without fusion [4, 14]. Those studies do show beneficial clinical and technical outcomes, as does this study, but they are not without limitations. The first study had a limited number of patients, only 15, and used hydroxyapatite grafting in addition to short-segment pedicle screw fixation [14]. The other study, randomized and controlled, only compared patients with Denis Type B fractures [4]. This study consisted of 64 patients and included all thoracolumbar burst fractures involving the middle column, not just Denis Type B fractures, so even though this study is retrospective it expands on the current knowledge of this treatment.
In most of the burst fractures presented in this paper there was adjacent disk injury both cephalad and caudal to the injury but especially cephalad. Although there was adjacent disk injury, if the disk was not completely herniated into the vertebral canal or vertebral body then this method could still be used. Also, adjacent disk injury does not influence reduction as long as the longitudinal ligament is intact. However, after hardware removal these adjacent disks do degenerate quickly, but clinical outcome is still acceptable.
In conclusion, the management of thoracolumbar burst fractures ranges from simple conservative management to anterior and posterior surgical decompression with fixation. Indirect reduction with short pedicle screw fixation falls somewhere in the middle of the management spectrum. Because of the limitations of the few studies on this treatment we advocate for a more thorough investigation. Furthermore, the technique described is not intended to replace known management techniques, but instead, adds another therapeutic option in burst fracture care.
References
- 1.Aiki H, Ohwada O, Kobayashi H, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci. 2005;10(5):490–495. doi: 10.1007/s00776-005-0919-3. [DOI] [PubMed] [Google Scholar]
- 2.Butt MF, Farooq M, Mir B, et al. Management of unstable thoracolumbar spinal injuries by posterior short segment spinal fixation. Int Orthop. 2007;31(2):259–264. doi: 10.1007/s00264-006-0161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheh G, Bridwell KH, Lenke LG, et al. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine. 2007;32(20):2253–2257. doi: 10.1097/BRS.0b013e31814b2d8e. [DOI] [PubMed] [Google Scholar]
- 4.Dai L, Jiang L, Jiang S. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. A five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009;91(5):1033–1041. doi: 10.2106/JBJS.H.00510. [DOI] [PubMed] [Google Scholar]
- 5.Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res. 1984;189:65–76. [PubMed] [Google Scholar]
- 6.Esses S, Botsford D, Kostuik J. Evaluation of surgical treatment for burst fractures. Spine. 1990;15(7):667–673. doi: 10.1097/00007632-199007000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Farcy J, Weidenbaum M, Glassman S. Sagittal index in management of thoracolumbar burst fractures. Spine. 1990;15(9):958–965. doi: 10.1097/00007632-199009000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Maciejczak A, Barnas P, Dudziak P, et al. Posterior keyhole corpectomy with percutaneous pedicle screw stabilization in the surgical management of lumbar burst fractures. Neurosurgery. 2007;60(4 Suppl 2):232–241. doi: 10.1227/01.NEU.0000255399.08033.B3. [DOI] [PubMed] [Google Scholar]
- 9.Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 10.Maynard FM, Jr, Bracken M, Creasey G, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord. 1997;35(5):266–274. doi: 10.1038/sj.sc.3100432. [DOI] [PubMed] [Google Scholar]
- 11.Muller U, Berlemann U, Sledge J, et al. Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: Bisegmental Stabilization with Monosegmental Fusion. Eur Spine J. 1999;8(4):284–289. doi: 10.1007/s005860050175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roland M, Fairbank J. The Roland–Morris disability questionnaire and the Oswestry disability questionnaire. Spine. 2000;25(24):3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 13.Singn K, Kim D, Vaccaro AR. Thoracic and lumbar spinal injuries. In: Herkowitz H, Garfin S, Eismont F, Bell G, Balderston R, editors. Rothman–Simeone the spine. Philadelphia: Saunders Elsevier; 2006. pp. 1132–1156. [Google Scholar]
- 14.Toyone T, Tanaka T, Kato D, et al. The treatment of acute thoracolumbar burst fractures with transpedicular intracorporeal hydroxyapatite grafting following indirect reduction and pedicle screw fixation: a prospective study. Spine. 2006;31(7):E208–E214. doi: 10.1097/01.brs.0000208161.74286.ad. [DOI] [PubMed] [Google Scholar]
- 15.Verlaan J, Diekerhof C, Buskens E, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine. 2004;29(7):803–814. doi: 10.1097/01.BRS.0000116990.31984.A9. [DOI] [PubMed] [Google Scholar]
- 16.Yang H, Shi J, Liu J, et al. Fluoroscopically-guided indirect posterior reduction and fixation of thoracolumbar burst fractures without fusion. Int Orthop. 2009;33(5):1329–1334. doi: 10.1007/s00264-008-0626-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoganandan N, Maiman D, Pintar F, et al. Biomechanical effects of laminectomy on thoracic spine stability. Neurosurgery. 1993;32(4):604–610. doi: 10.1227/00006123-199304000-00017. [DOI] [PubMed] [Google Scholar]