Abstract
The objective of the current study was to find out whether yoga practice was beneficial to the spine by comparing degenerative disc disease in the spines of long-time yoga practitioners and non-yoga practicing controls, using an objective measurement tool, magnetic resonance imaging. This matched case–control study comprised 18 yoga instructors with teaching experience of more than 10 years and 18 non-yoga practicing asymptomatic individuals randomly selected from a health checkup database. A validated grading scale was used to grade the condition of cervical and lumbar discs seen in magnetic resonance imaging of the spine, and the resulting data analyzed statistically. The mean number of years of yoga practice for the yoga group was 12.9 ± 7.5. The overall (cervical + lumbar) disc scores of the yoga group were significantly lower (indicating less degenerative disc disease) than those of the control group (P < 0.001). The scores for the cervical vertebral discs of the yoga group were also significantly lower than those of the control group (P < 0.001), while the lower scores for the yoga group in the lumbar group approached, but did not reach, statistical significance (P = 0.055). The scores for individual discs of yoga practitioners showed significantly less degenerative disease at three disc levels, C3/C4, L2/L3 and L3/L4 (P < 0.05). Magnetic resonance imaging showed that the group of long-term practitioners of yoga studied had significantly less degenerative disc disease than a matched control group.
Keywords: Yoga, Disc degenerative disease (DDD), Neck pain, Low back pain, MRI
Introduction
Yoga is an ancient discipline, originating in India, which involves meditation, breathing control and the maintenance of various body postures [1–4]. During a yoga session, a person assumes a series of prescribed stationary positions that utilize isometric contraction and relaxation of different muscle groups to create specific body alignments [5]. It has been estimated that in the USA, 20–30 million people practice some form of yoga [6]. Yoga has long been used to improve physical and emotional well-being, and to alleviate chronic pain, stress and anxiety [2, 7, 8].
Chronic back and neck pain are common in the general population [8–13], and yoga exercises have been reported to be effective in reducing such pain [3, 6, 14–17]. Yoga reduces chronic spinal pain; one reason might be that the stretching and positioning of the spine that occur during yoga exercises decrease the gradual disc degeneration that occurs with age. It might also be because the decreased weight bearing during yoga practice lessens the stress on the spine. Magnetic resonance imaging (MRI) is a well-documented diagnostic technique for the study of degenerative disc disease (DDD) [18–22]. To the best of our knowledge, there has been to date no original study using MRI to compare the spines of yoga practitioners and non-practitioners. Therefore, we conducted an MRI-based, case–control study of the extent of spine degeneration in yoga teachers in comparison to non-yoga practicing controls.
Methods
Study sample
Eighteen local yoga instructors with teaching experience of more than 10 years were invited to participate in our study. A control group was selected in the following way: 18 asymptomatic individuals were randomly selected from the health checkup database at our institution. The genders and ages of the individuals in this group were then compared to those of the yoga group using the chi-square and t tests, respectively. If there was a significant difference between the groups in either gender or age, the tentative control group was discarded and a new group randomly chosen and tested. This procedure was repeated until a group was found that did not differ significantly in age and gender from the yoga group. Written, informed consent was obtained from all participants.
No individual enrolled in either yoga or control group had ever experienced low back pain, soreness, painful sensation or other discomfort that required medication or medical consultation, and none had any systemic disease such as a cerebrovascular, craniospinal or cardiovascular disorders, or a malignancy that would have curtailed their physical activity. The BMI of all participants was within normal limits. No evidence of scoliosis was seen in any study participant, and no participant engaged in strenuous sports or employment involving heavy lifting. No individual in the control group had practiced yoga exercise prior to this study, and no other exercise that might have induced degenerative disc disease had been experienced in either group. All control subjects were non-smokers.
All individuals in both groups underwent MRI evaluation of their cervical and lumbar spines. The same MRI technique was used for both groups.
MRI protocol
The MRIs in the control group were performed as part of the general health checkup and not because of any complaint related to the spine.
All MRI studies were performed using a 1.5 Tesla superconducting system (Gyroscan NT 15, Philips Medical Systems, Best, Netherlands) with a spinal surface coil. The following pulse sequences were performed:
Sagittal T2-weighted turbo spin echo [4,700 ms (repetition time)/120 ms (echo time), 15 (echo train length), 4 mm (section thickness), 280 × 280 mm (field of view, FOV), 240 × 256 (matrix size), and one signal acquisition].
Sagittal T1-weighted spin echo [600 ms (repetition time)/14 ms (echo time), 15 (echo train length), 4 mm (section thickness), 280 × 280 mm (field of view, FOV), 240 × 256 (matrix size), and one signal acquisition].
Axial T2-weighted turbo spin echo over levels of intervertebral discs of the cervical and lumbar spine [4,500 ms (repetition time)/120 ms (echo time), 15 (echo train length), 4 mm (section thickness), 200 × 200 mm (field of view, FOV), 240 × 256 (matrix size), and one signal acquisition].
Imaging assessment
All MRI studies were evaluated by two of the authors (JCM and KCH), both experienced in reading spinal MRI. All images were assessed in a blinded fashion; neither of the two authors knew to which patient group each image belonged. The appearance of the intervertebral discs was graded using the system described below. In the cases where the grades of the two examiners differed, the final grade was reached through consensus after a further discussion of the image in doubt.
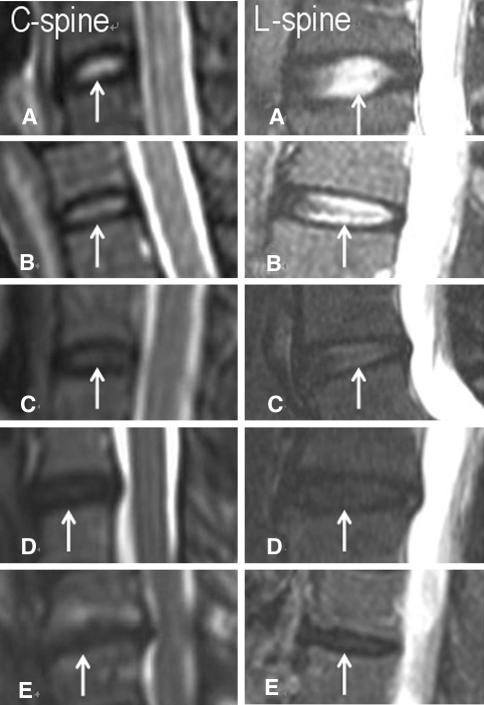
DDD was classified into five grades based on T2-weighted mid-sagittal images depending on the degenerative status of the nucleus. This grading system has been well documented [18, 19] as described below, and each grade is illustrated in Fig. 1.
Homogeneous hyperintense disc; normal disc height
Inhomogeneous hyperintense disc with focal hypointensity (gray); clear distinction between nucleus and annulus.
Inhomogeneous intermediate intensity disc with possible decreased height; unclear distinction between nucleus and annulus.
Inhomogeneous hypointense (dark) disc with decreased height; loss of distinction between nucleus and annulus.
Inhomogeneous hypointense (black) disc with collapsed disc space; loss of distinction between nucleus and annulus.
Fig. 1.
The grading system of cervical and lumbar intervertebral discs based on sagittal T2-weighted images. a Grade I disc (arrow): a homogeneous hyperintense disc with normal height. b Grade II disc (arrow): a hyperintense disc with focal hypointensity. c Grade III disc (arrow): an inhomogeneous disc with unclear distinction between nucleus and annulus. d Grade IV disc (arrow): an inhomogeneous hypointense disc with decreased height. e Grade V disc (arrow): a collapsed hypointense disc
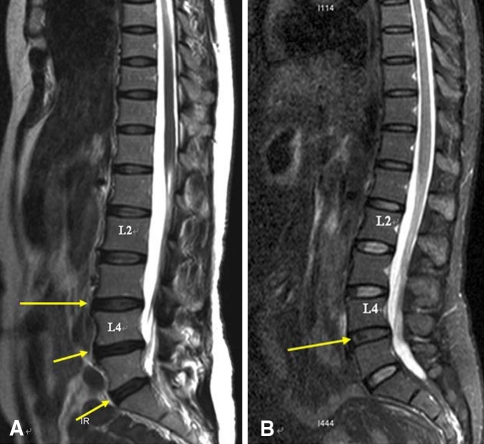
An example of the application of such grading system of the lumbar spine in a 50-year-old non-yoga office lady and a 51-year-old yoga teacher is illustrated in Fig. 2.
Fig. 2.
a Sagittal MRI of the lumbar spine of a 50-year-old female office lady without yoga experience. Findings: Grade III disc (an inhomogeneous disc with unclear distinction between nucleus and annulus) at L3–4 intervertebral disc (long arrow). Grade IV disc (an inhomogeneous hypointense disc with decreased height) at L4–5 and L5–S1 intervertebral discs (short arrows). b Sagittal MRI of the lumbar disc of a 51-year-old yoga teacher with 15 years of teaching experience. Findings: Grade III disc (an inhomogeneous disc with unclear distinction between nucleus and annulus) at L4–5 intervertebral disc (long arrow)
Statistical analysis
Continuous data were expressed as mean ± standard deviation (SD) or median (range) and compared using Student’s t test or Mann–Whitney test. Categorical data were expressed as frequencies and percentages and tested with the Fisher’s exact test. All statistical assessments were two sided and evaluated at the 0.05 level of significance. Statistical analyses were performed using SPSS 15.0 statistics software (version 15.0, SPSS Inc, Chicago, IL, USA). The primary objective was to compare results for the spine as a whole, the secondary objective to compare results for cervical and lumbar segments separately, and the tertiary objective to compare results at individual disc levels.
Results
Demographics
Table 1 shows age, gender and years of yoga practice for both yoga and control groups. The age (45.1 ± 10.6 years and 50.6 ± 8.5 years, respectively) and gender of the two groups were not significantly different. The mean number of years of yoga practice for the yoga group was 12.9 ± 7.5. The control group had never practiced yoga.
Table 1.
Descriptive characteristics of 36 subjects
| Yoga group n = 18 | Control group n = 18 | P value | |
|---|---|---|---|
| Agea | 45.1 ± 10.6 | 50.6 ± 8.54 | 0.378 |
| Sex (male/female)b | 3/15 | 5/13 | 0.345 |
| Yoga performing period (year) | 12.9 ± 7.5 | – | – |
Continuous data expressed as mean ± SD, and categorical data expressed as number
aStudent’s t test, bFisher’s exact test
MRI results
MRI results are shown in Table 2. The primary comparison, differences in the whole spine, showed the total score (cervical and lumbar discs, N = 180 for yoga and control) of the yoga group to be significantly lower (that is, to show less degenerative disc disease) than that of the control group (P < 0.001).
Table 2.
Comparison of the intervertebral disc degeneration between the yoga group and the control group
| Grading | Yoga group | Control group | P value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| C2/3 | 0 (0) | 11 (61.1) | 7 (38.9) | 0 (0) | 0 (0) | 0 (0) | 8 (44.4) | 9 (50.0) | 0 (0) | 1 (5.6) | 0.422 |
| C3/4 | 0 (0) | 14 (77.8) | 4 (22.2) | 0 (0) | 0 (0) | 1 (5.6) | 5 (27.8) | 11 (61.0) | 1 (5.6) | 0 (0) | 0.023* |
| C4/5 | 0 (0) | 14 (77.8) | 3 (16.6) | 1 (5.6) | 0 (0) | 0 (0) | 7 (38.9) | 9 (50.0) | 2 (11.1) | 0 (0) | 0.059 |
| C5/6 | 0 (0) | 15 (83.3) | 2 (11.1) | 1 (5.6) | 0 (0) | 0 (0) | 9 (50.0) | 5 (27.8) | 4 (22.2) | 0 (0) | 0.101 |
| C6/7 | 4 (22.2) | 10 (55.6) | 4 (22.2) | 0 (0) | 0 (0) | 0 (0) | 10 (55.6) | 8 (44.4) | 0 (0) | 0 (0) | 0.069 |
| Five C spine | 4 (4.5) | 64 (71.1) | 20 (22.2) | 2 (2.2) | 0 (0) | 1 (1.1) | 39 (43.3) | 42 (46.7) | 7 (7.8) | 1 (1.1) | <0.001* |
| L1/2 | 0 (0) | 16 (88.9) | 2 (11.1) | 0 (0) | 0 (0) | 0 (0) | 17 (94.4) | 1 (5.6) | 0 (0) | 0 (0) | 1.000 |
| L2/3 | 0 (0) | 16 (88.9) | 2 (11.1) | 0 (0) | 0 (0) | 0 (0) | 9 (50.0) | 8 (44.4) | 1 (5.6) | 0 (0) | 0.038* |
| L3/4 | 2 (11.1) | 6 (33.3) | 10 (55.6) | 0 (0) | 0 (0) | 0 (0) | 2 (11.1) | 14 (77.8) | 2 (11.1) | 0 (0) | 0.083 |
| L4/5 | 2 (11.1) | 2 (11.1) | 10 (55.6) | 4 (22.2) | 0 (0) | 0 (0) | 4 (22.2) | 11 (61.1) | 3 (16.7) | 0 (0) | 0.414 |
| L5/S1 | 2 (11.1) | 8 (44.5) | 4 (22.2) | 4 (22.2) | 0 (0) | 1 (5.6) | 6 (33.3) | 8 (44.4) | 3 (16.7) | 0 (0) | 0.553 |
| Five L spine | 6 (6.7) | 48 (53.3) | 28 (31.1) | 8 (8.9) | 0 (0) | 1 (1.1) | 38 (42.2) | 42 (46.7) | 9 (10.0) | 0 (0) | 0.055 |
| Total ten discs | 10 (5.6) | 112 (62.2) | 48 (26.7) | 10 (5.6) | 0 (0) | 2 (1.1) | 77 (42.8) | 84 (46.7) | 16 (8.9) | 1 (0.6) | <0.001* |
Data expressed as number (%) and tested with Fisher’s exact test
*Statistical significance, P < 0.05
The secondary comparison of the cervical and lumbar spinal segments separately, using groups of five disc levels in each segment, showed the scores of the yoga group (N = 90 for both yoga and control groups) to be significantly lower in the cervical spine (P < 0.001). When the same comparison was performed for the lumbar spine (N = 90 for both yoga and control groups also), the lower score in the yoga group approached, but did not reach, statistical significance (P = 0.055).
In the tertiary comparison, when yoga and control groups were compared at the individual disc level (N = 18 for yoga and control groups), the yoga group had significantly lower scores at three levels (C3/4, L 2/3 and L3/4) when this comparison was made using the Mann–Whitney test (Table 3) and at two levels (C3/4 and L2/3) when Fisher’s exact test was used for analysis (Table 2). The lower score of the yoga group at C3/4 and L2/3 is mainly due to a shift in the control group (compared to the yoga group) from Grade II to Grade III; that is, in the control group, the intensity of the MRI signal from the disc decreased, disc height in some cases was no longer normal, and the distinction between the interior of the disc and the surrounding ring was no longer clear.
Table 3.
Comparison of the intervertebral disc degeneration between the yoga group and the control group
| Grading | Yoga group | Control group | P value |
|---|---|---|---|
| C2/3 | 3 (2–5) | 2 (2–3) | 0.339 |
| C3/4 | 3 (1–4) | 2 (2–3) | 0.034* |
| C4/5 | 3 (2–4) | 2 (2–4) | 0.051 |
| C5/6 | 2.5 (2–4) | 2 (2–4) | 0.079 |
| C6/7 | 2 (2–3) | 2 (1–3) | 0.079 |
| L1/2 | 2 (2–3) | 2 (2–3) | 0.791 |
| L2/3 | 2.5 (2–4) | 2 (2–3) | 0.044* |
| L3/4 | 3 (2–4) | 3 (1–3) | 0.037* |
| L4/5 | 3 (2–4) | 3 (1–4) | 0.938 |
| L5/S1 | 3 (1–4) | 2 (1–4) | 0.563 |
Data expressed as median (range) and tested with Mann–Whitney Test
* Statistical significance, P < 0.05
Discussion
When individual disc level grades of yoga and control groups were compared, three of the ten disc level comparisons showed a lower score of the yoga group (that is, less disc degeneration) over the control group, which was of modest (P < 0.05) statistical significance. However, when the total disc grades for all cervical and lumbar disc levels were compared, the relative freedom from disc disease of the yoga group was highly significant (P < 0.001).
The high significance of the total score comparison compared to the modest or absent significance of the individual disc level comparisons is partly due to the difference in the size (180 and 18) of the data sets used. But it is also an expected result for the two populations. Our study was a comparison of two normal populations and individuals with symptomatic disc disease were excluded from the study. Therefore, the likelihood that there would be a highly significant difference between two asymptomatic groups at any one individual spinal level was remote, but small differences between groups at each individual level could easily add up to a total disc score difference of unquestionable significance.
This highly significant difference recorded here between the total disc scores of the two populations suggests that the long-term practice of yoga may have slowed somewhat the natural aging process that occurs in the intervertebral discs. It is possible that the somewhat older age of the control group influenced the results. However, the fact that the age difference was not statistically significant (P = 0.338) argues against this interpretation.
The intervertebral disc consists of an outer ring, the annulus fibrosis, that is made up primarily of type I collagen and fibrocyte/fibroblast-like cells. This composition gives the disc the ability to resist tensile forces. The inner core, the nucleus pulposis, contains type II collagen, proteoglycans and chondrocytes. The proteoglycans retain water, increase the stiffness of the disc and thus provide resistance to compression [13, 23].
As an individual ages, the number of chondrocytes in the nucleus pulposis decreases, less proteoglycan is synthesized, the water content of the disc decreases and it loses thickness. The disc becomes more fibrous and disorganized, and the visual distinction between the annulus and nucleus is lost (Grade III or higher of the MRI grading system is used here) [13].
The intervertebral disc is relatively avascular and receives nutrients through diffusion from the bone marrow across the cartilagenous endplate and through the annulus fibrosis from the surrounding blood vessels. It is possible, although speculative, that the various positions held by the spine during the yoga sessions retard disc degeneration by increasing the ability of nutrients to diffuse into the disc. It is also possible that the tension and compression of the disc during yoga exercises stimulate the synthesis of growth factors by the fibrocytes and chondrocytes residing in the disc and prevent their senescence.
The difference in total disc scores between the yoga and control group clearly shows that in this pilot study the long-term practice of yoga is associated with fewer age-related changes in the intervertebral discs. It is less easy to interpret the meaning of the other three statistically significant observations. At a few disc levels (C3/4, L2/3, and in the Mann–Whitney analysis L3/4), the yoga group showed significantly less disc degeneration than the control group. But at all except one of the other discs, the yoga group also showed less disc degeneration than the control group, although the difference did not reach statistical significance. The lesser disc degeneration seen in the yoga group, therefore, might be a general phenomenon and not limited to C3/4, L2/3 and L4/5. The difference in the statistical significance in the yoga/control comparison in the cervical and lumbar regions is seen because the control group has similar disc scores in both regions, but the yoga group does not and has higher scores (and therefore scores closer to control group scores) in the lumbar than in the cervical region.
In a randomized controlled trial performed by others, yoga was found to be able to decrease kyphosis in senior women and men with adult-onset hyperkyphosis [24]. And as mentioned in our introduction, yoga exercises have been reported to be effective in reducing chronic back and neck pain [3, 6, 14–17]. Adults with pain, stenosis and idiopathic scoliosis have been shown to have better outcomes in the areas of pain relief, function and patient satisfaction with the surgical restoration of coronal and sagittal balance [25]. However, we do not know whether better preservation in sagittal balance occurs with long-term chronic yoga practice and whether it is a cause of the differences seen in cervical and lumbar scores in our study, because we cannot measure sagittal balance with MRI. The measurement of sagittal balance needs to be performed with 36-inch standing radiographs [26].
The effect of yoga on the spine described in this report is the result of long-term practice of yoga and cannot be directly responsible for the relief from back and neck pain experienced by some individuals after only a few yoga sessions. Back and neck pain are not only related to disc degeneration, but also to genetic factors, inflammation at the disc site and psychological and other factors. The relationship between disc degeneration and pain is not a “tight” one, and the majority of persons with disc degeneration are asymptomatic.
Our study has several limitations. First, yoga includes many types such as Ashtanga, Bhakti, Guru, Hatha, Iyengar, Jnana, Karma, Mantra, Raja and Tantra [3]. These have different posture practices related to the motion of the spine, and some are gentler than others [6]. Hatha yoga is the most common type practiced in the USA [5] and in Taiwan as well. Hatha is a slow-paced, gentle yoga. Other types may differ; for example, Asthanga is a fast, intense, very physically demanding yoga involving constant movement, and Iyengar stresses on precise positioning and these positions are held over long periods. Since all yoga instructors in our study practiced Hatha yoga, our results may not necessarily apply to other types of yoga.
Second, all participants in the yoga group of our study were yoga instructors with more than 10 years of experience. Thus, our results may not apply to the short-term practice of yoga in the general population.
The findings reported here are of interest for preventative medicine, a field that has become increasingly important as the population in many countries ages. They raise the question of whether long-term chronic practice of other types of exercises that involve changes in spinal conditioning retard or accelerate disc degeneration and, if this is the case, whether useful lifestyle guidelines to minimize age-related disc degeneration can be developed.
Conclusion
This pilot study shows a possible association between the long-term practice of yoga and a lessening of age-related disc degeneration that may be worth exploring. A larger prospective study controlled for other risk factors is needed to clarify the relationship between yoga and disc disease.
References
- 1.Guarracino JL, Savino S, Edelstein S. Yoga participation is beneficial to obesity prevention, hypertension control, and positive quality of life. Top Clin Nutr. 2006;21:108–113. [Google Scholar]
- 2.John PJ, Sharma N, Sharma CM, et al. Effectiveness of yoga therapy in the treatment of migraine without aura: a randomized controlled trial. Headache. 2007;47:654–661. doi: 10.1111/j.1526-4610.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 3.Breuner CC. Alternative and complementary therapies. Adolesc Med Clin. 2006;17:521–546. doi: 10.1016/j.admecli.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 4.Herrick CM, Ainsworth AD. Invest in yourself: Yoga as a self-care strategy. Nurs Forum. 2000;35(2):32–36. doi: 10.1111/j.1744-6198.2000.tb00996.x. [DOI] [PubMed] [Google Scholar]
- 5.Oken BS, Kishiyama S, Zajdel D, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62:2058–2064. doi: 10.1212/01.wnl.0000129534.88602.5c. [DOI] [PubMed] [Google Scholar]
- 6.Taylor MJ. Yoga therapeutics: an ancient, dynamic systems theory. Tech Orthop. 2003;18:115–125. doi: 10.1097/00013611-200303000-00017. [DOI] [Google Scholar]
- 7.Chen K, Tseng WS, Ting LF, et al. Development and evaluation of a yoga exercise programme for older adults. J Adv Nurs. 2007;57:432–441. doi: 10.1111/j.1365-2648.2007.04115.x. [DOI] [PubMed] [Google Scholar]
- 8.Katz JN, Simmons BP. Carpal tunnel syndrome. N Engl J Med. 2002;346:1807–1812. doi: 10.1056/NEJMcp013018. [DOI] [PubMed] [Google Scholar]
- 9.Devereaux MW. Anatomy and examination of the spine. Neurol Clin. 2007;25:331–351. doi: 10.1016/j.ncl.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Hogg-Johnson S, Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine. 2008;33:S39–S51. doi: 10.1097/BRS.0b013e31816454c8. [DOI] [PubMed] [Google Scholar]
- 11.Hazard RG. Low-back and neck pain diagnosis and treatment. Am J Phys Med Rehabil. 2007;86:S59–S68. doi: 10.1097/PHM.0b013e31802ba50c. [DOI] [PubMed] [Google Scholar]
- 12.Schenk P, Laubli T, Hodler J, et al. Magnetic resonance imaging of the lumbar spine findings in female subjects from administrative and nursing professions. Spine. 2006;31:2701–2706. doi: 10.1097/01.brs.0000244570.36954.17. [DOI] [PubMed] [Google Scholar]
- 13.Roh JS, Teng AL, Yoo JU, et al. Degenerative disorders of the lumbar and cervical spine. Orthop Clin N Am. 2005;36:255–262. doi: 10.1016/j.ocl.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 14.Levin KH. Nonsurgical interventions for spine pain. Neurol Clin. 2007;25:495–505. doi: 10.1016/j.ncl.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Sherman KJ, Cherkin DC, Erro J, et al. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143:849–856. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 16.Hurwitz EL, Carragee EJ, Velde G, et al. Treatment of neck pain: noninvasive interventions: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine. 2008;33:S123–S152. doi: 10.1097/BRS.0b013e3181644b1d. [DOI] [PubMed] [Google Scholar]
- 17.Dillard JN, Knapp S. Complementary and alternative pain therapy in the emergency department. Emerg Med Clin N Am. 2005;23:529–549. doi: 10.1016/j.emc.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Fujiwara A, Tamai K, Yamato M, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pappou IP, Cammisa FP, Girardi FP. Correlation of end plate shape on MRI and disc degeneration in surgically treated patients with degenerative disc disease and herniated nucleus pulposus. Spine J. 2007;7:32–38. doi: 10.1016/j.spinee.2006.02.029. [DOI] [PubMed] [Google Scholar]
- 20.Pfirrmann CWA, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 21.Peterson CK, Gatterman B, Carter JC, et al. Inter-and intraexaminer reliability in identifying and classifying degenerative marrow (Modic) changes on lumbar spine magnetic resonance resonance scans. J Manipulative Physiol Ther. 2007;30:85–90. doi: 10.1016/j.jmpt.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Miyanji F, Furlan JC, Aarabi B, Arnold PM, Fehlings MG. Acute cervical traumatic spinal cord injury: MR imaging findings correlated with neurologic outcome—prospective study with 100 consecutive patients. Radiology. 2007;243:820–827. doi: 10.1148/radiol.2433060583. [DOI] [PubMed] [Google Scholar]
- 23.Modic MT, Ross JS. Lumbar degenerative disk disease. Radiology. 2007;245:43–61. doi: 10.1148/radiol.2451051706. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro GS, Taira G, Boachie-Adjei O. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes. Spine. 2003;28:358–363. doi: 10.1097/00007632-200302150-00009. [DOI] [PubMed] [Google Scholar]
- 25.Greendale GA, Huang MH, Karlamangla AS, et al. Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57(9):1569–1579. doi: 10.1111/j.1532-5415.2009.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]