Abstract
The main objective of this study is to determine the prevalence of coronal abnormalities of the lumbar spine in a large population of patients with respect to their age and sex. Lumbar degenerative disease is associated with degenerative scoliosis. Degenerative scoliosis and lateral listhesis are important features to identify before decompressive surgery as deformity may not be seen on magnetic resonance imaging scans. Scoliosis and lateral listhesis may be important in the development of symptoms especially in an ageing population. All abdominal and plain kidney–ureter–bladder radiographs performed over a 10-month period were reviewed. 2,765 radiographs were assessed for scoliosis (Cobb angle greater then 10°), lateral listhesis and evidence of osteoarthritis. The prevalence of scoliosis, lateral listhesis and osteoarthritis of the lumbar spine increased with age. Scoliosis and lateral listhesis were significantly more prevalent in women. Deformity starts to occur after the age of 50 and steadily increases with age. By the ninth decade nearly a quarter of patients have evidence of scoliosis and lateral listhesis. As the adult lumbar spine ages, the prevalence of lateral listhesis and degenerative scoliosis increases. It is important to appreciate these coronal abnormalities in patients undergoing decompressive surgery for spinal stenosis. This increase in deformity may have a greater impact as the population continues to age.
Keywords: Prevalence, Degenerative lumbar scoliosis, Adult
Introduction
Adult scoliosis is defined as a spinal deformity in the skeletally mature adult with a Cobb angle of greater than 10° in the coronal plane [1]. The prevalence of adult scoliosis and other coronal plane deformities is not clear as published studies have reported contrasting results. Previous studies have looked at the prevalence of lumbar scoliosis in symptomatic and non-symptomatic groups. Prevalence has ranged from 1.4–68% [2–5]. The prevalence of spondylolisthesis in the sagittal plane has been investigated by other authors [6, 7] but coronal plane deformity, and in particular lateral listhesis, has not been well characterised.
Patients with adult scoliosis may be asymptomatic or severely disabled by the deformity [8]. Adult onset degenerative scoliosis often presents in the sixth decade [9, 10] with stenotic symptoms [9] from mechanical compression [11, 12], low back pain [10, 13] spondylolisthesis [14], rotational subluxation [14–17] and lumbar hypolordosis [14, 18]. The majority of adult onset degenerative scoliosis occurs in patients with no history of non-degenerative scoliosis [18–20].
The relationship between the presence and magnitude of scoliotic curves and the presence of pain is not clear. Higher Cobb angles and the development of new curves have been found to be related to the increased severity of pain [18, 20, 21]. Conversely others [5] found that whilst some radiographic parameters: lateral vertebral olisthy, L3 and L4 endplate obliquity angles, lumbar lordosis, and thoracolumbar kyphosis were significantly correlated with pain, the magnitude of the Cobb angle was not.
The United Kingdom (UK) has an ageing population with people living longer and with a greater proportion of the population over the age of 65 years [22]. In 2006, 16% of the UK population was aged over 65 years. This will rise to 22% by 2031. 2007 was the first year since records began that there were more people in the UK aged over 65 than under 16 [22]. Life expectancy is also increasing. In 1988 life expectancy for those aged 65 was 15.3 years for men and 18.8 years for women. By 2008 this had increased to 18.8 and 23.3 years, respectively [23]. These demographic changes mean that there will be more people with degenerative spinal deformity which may need treatment. Technology for treating such deformity, in the form of screws, cement and pelvic fixation, continues to evolve and has proven good results in selected patients.
Studies comparing operative and non-operative treatment in degenerative adult scoliosis [24–26] have shown improvement in Health Related Quality of Life (HRQOL) scores and improved walking ability in the operative groups.
It has been shown that there is a significant difference in the Scoliosis Research Society Quality of Life (SRS-QOL) scores between patients with adult onset spinal deformity and a control population [27]. Normative scores have also been established in unaffected patients [28]. Further, this work validates the SRS-QOL tool and allows other investigators to assess intervention in further studies in adult deformity patients.
The aim of this study was to assess the prevalence of coronal abnormalities of the lumbar spine in a large population of patients. Abdominal radiographs were used as they are a frequently performed investigation which demonstrate the lumbar spine well. The inclusion of formal lumbar spine radiographs, which are less frequently performed, would have introduced bias into our population as they are usually performed in patients in whom spinal pathology is suspected.
Materials and methods
We analysed all abdominal and kidney–ureter–bladder (KUB) radiographs performed at our institution, on patients over the age of 20 years, over the 10-month period from the introduction of a digital radiograph system (Centricity Enterprise—GE Medical). Patients who had multiple investigations were only included once. 2,765 radiographs were reviewed. KUB films image a greater area than abdominal radiographs but otherwise there is no difference between the techniques in obtaining either type of study.
Radiographs were included if the lower border of T12 to the upper border of S1 vertebral bodies were visible. Radiographs were excluded if artefact precluded meaningful analysis of the vertebral column, e.g. contrast from intra-venous urograms, or if there was evidence of pre-existing lumbar surgery, e.g. metalwork. Figure 1 is an example of the type of radiograph included in the study. The lower border of T12 to the upper border of S1 is easily visualised and although there is a left sided ureteric stent in situ it does not obscure assessment of the spine and the radiograph could therefore be included.
Fig. 1.
Example abdominal radiograph
2,718 radiographs were suitable for inclusion. 47 were excluded; 37 radiographs were inadequate and in 10 metalwork was present.
The radiographs were analysed for the presence of a lumbar scoliosis and the presence and level of lateral listheses (slip of one vertebral end plate on another). The prevalence of osteoarthritis (OA) was determined by the presence of osteophytes. This was correlated with Grade III/IV osteoarthritis using the UCLA disc degeneration score. A scoliosis was defined as a Cobb angle of greater than 10°. Curves of less than 10° were recorded as “minor”. All radiographs were reviewed by two authors with separate measurement of Cobb angles and assessment of presence of OA and listhesis. Radiographs where there was disagreement (presence or not of listhesis or OA, difference in Cobb angles > 5°) were reviewed with the senior author.
Radiographs were grouped into 10 year age brackets by age on the day of the investigation. Radiographs in subjects older than 90 were grouped into one cohort. Subgroup analysis using the Chi-square test was performed according to the subject’s sex and age. Inadequate radiographs were not included in the analysis.
Results
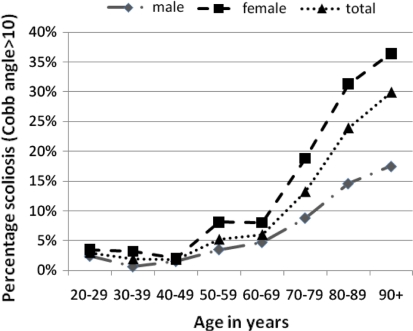
1,430 (52.6%) of subjects were male. In the population as a whole 9.5% subjects had a lumbar scoliosis of greater than 10° (women 13.5%, men 5.7%). Scoliosis was significantly more prevalent in women (p < 0.0001). Figure 2 shows the relationship between age, gender and prevalence of scoliosis. The average Cobb angle in patients with a curve greater than 10° was 16.9° (women 17.8°, men 14.8°). A further 10.2% had mild lumbar curves of less than 10° (women 9.5%, men 8.2%). The apex of the scoliotic curves greater than 10° was recorded in all patients over the age of 70 years. 60.6% of curves had the apex at L3 with a further 30.9% with apex L2. The sidedness of curves was not recorded.
Fig. 2.
The relationship between age, sex and prevalence of scoliosis (Cobb angle > 10o)
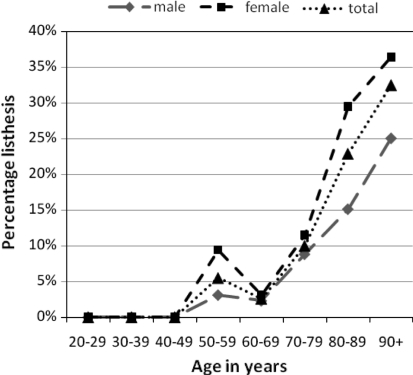
7.7% of subjects had evidence of lateral listhesis (women 10.0%, men 5.1%). Lateral listhesis was significantly more common in woman (p < 0.001). Figure 3 shows the relationship between age, gender and prevalence of listhesis. Ten patients had multi-level lateral listhesis. Table 1 shows the levels at which lateral listhesis occurred according to age. Lateral listhesis most commonly occurred at the L3/L4 junction in all age groups and in 48.1% of patients overall. This appears to correspond with the majority of curve apices being at L3.
Fig. 3.
The relationship between age, sex and prevalence of lateral listhesis
Table 1.
Lumbar spine abnormality according to age
| Age | n | Lumbar scoliosis | Lateral listhesis | Osteoarthritis |
|---|---|---|---|---|
| 20–29 | 197 | 6 (3.0%) | 0 | 0 |
| 30–39 | 319 | 6 (1.9%) | 0 | 0 |
| 40–49 | 399 | 7 (1.8%) | 0 | 101 (25.3%) |
| 50–59 | 420 | 22 (5.2%) | 23 (5.5%) | 306 (72.9%) |
| 60–69 | 419 | 25 (6%) | 11 (2.6%) | 353 (84.2%) |
| 70–79 | 432 | 57 (13.2%) | 43 (10.0%) | 430 (99.5%) |
| 80–89 | 185 | 99 (23.9%) | 95 (22.9%) | 185 (100%) |
| 90+ | 117 | 35 (29.9%) | 38 (32.5%) | 117 (100%) |
Lateral listhesis was significantly more prevalent in patients with a scoliosis (p < 0.001). Overall 7.7% of the population had a listhesis. In patients with a scoliosis 44.0% had a listhesis and in patients with no scoliosis just 3.8% had listhesis. This difference was present, and of a similar order of magnitude, in all age groups except the over 90-year-old where the difference, although still present, was much smaller.
63.4% of subjects had radiological signs of osteoarthritis (women 61.9%, men 64.0%). Table 2 shows the relationship between age and scoliosis, lateral listhesis and osteoarthritis.
Table 2.
Levels of lateral spondylolisthesis according to age (percentage)
| Age (years) | 50–59 | 60–69 | 70–79 | 80–89 | >90 | Overall average |
|---|---|---|---|---|---|---|
| Level (%) | ||||||
| L1/L2 | 4.3 | 0 | 2.3 | 13.7 | 10.5 | 9.0 |
| L2/L3 | 26.1 | 18.2 | 27.9 | 25.3 | 26.3 | 25.7 |
| L3/L4 | 30.4 | 63.6 | 58.1 | 46.3 | 47.4 | 48.1 |
| L4/L5 | 43.5 | 18.2 | 11.6 | 23.2 | 18.4 | 21.9 |
| L5/S1 | 0 | 0 | 0 | 0 | 2.6 | 0.5 |
As age increases so does the prevalence of all types of deformity. By the eighth decade 13% of people have a scoliosis of greater than 10°, one in ten have a lateral listhesis and nearly all patients have evidence of osteoarthritis. Deformity starts to appear after the age of 50 years. Tables 3 and 4 show the relationship between age, sex and scoliosis and lateral listhesis. In all age groups scoliosis is more common in women and the magnitude of the curves is greater in women. The prevalence of lateral listhesis is greater in women in all age groups.
Table 3.
The relationship between age, sex and prevalence of lateral listhesis and prevalence of listhesis in scoliotic and non-scoliotic patients
| Age | Male listhesis (%) | Female listhesis (%) | Overall listhesis (%) | Overall with scoliosis and listhesis (%) | Overall with no scoliosis and listhesis (%) |
|---|---|---|---|---|---|
| 20–29 | 0 | 0 | 0 | ||
| 30–39 | 0 | 0 | 0 | ||
| 40–49 | 0 | 0 | 0 | ||
| 50–59 | 3.1 | 9.4 | 5.5 | 45.5 | 3.2 |
| 60–69 | 2.3 | 3.1 | 2.6 | 20.0 | 1.5 |
| 70–79 | 8.8 | 11.5 | 10.0 | 38.6 | 5.5 |
| 80–89 | 15.1 | 29.1 | 22.9 | 65.7 | 9.2 |
| >90 | 25.0 | 36.4 | 32.5 | 34.3 | 31.3 |
| Overall | 5.1 | 10.6 | 7.7 | 44.4 | 3.8 |
Table 4.
The relationship between age and sex and the prevalence and magnitude of scoliosis
| Age | Male | Female | ||
|---|---|---|---|---|
| Scoliosis (%) | Average Cobb angle | Scoliosis (%) | Average Cobb angle | |
| 20–29 | 1.2 | – | 4.2 | – |
| 30–39 | 0.6 | 15.0 | 2.5 | 23.0 |
| 40–49 | 1.5 | 12.0 | 2.0 | 12.3 |
| 50–59 | 3.5 | 11.8 | 7.8 | 15.7 |
| 60–69 | 4.7 | 14.2 | 9.2 | 21.4 |
| 70–79 | 8.8 | 13.6 | 20.7 | 14.7 |
| 80–89 | 14.6 | 18.4 | 34.5 | 19.9 |
| >90 | 17.5 | 15.1 | 35.4 | 17.5 |
Discussion
The aim of this study was to assess the prevalence of coronal abnormalities of the lumbar spine in a population of random patients. This is a large study with all age groups numerically well represented. It shows a decade by decade increase, after the age of 50 years, in the prevalence of all types of coronal plane lumbar spine abnormality with a significant minority of the population affected. To our knowledge, it is the largest study in such a population looking at lateral listhesis as well as scoliosis. Previous studies have not related the findings of both types of deformity.
Our findings are of importance to spinal surgeons as fixation with decompression rather than decompression alone may be indicated. Previous studies have shown good results for operative treatment in selected patients with degenerative lumbar scoliosis [25, 26]. In patients with lateral subluxations that may be ‘open’ or ‘closed’ [17] predictable patterns of stenosis exist. Furthermore, failure to appreciate this or the fact that any deformity is present at all may lead to injudicious decompression with subsequent recurrence of the problem or a failure to adequately decompress at the time of surgery. The most common fault is to fail to decompress in the foramen or to think that one has done so adequately in the prone position only to have recurrence on mobilisation. This is borne out by results from recent studies [25, 26].
Unfortunately many patients undergoing spinal surgery may only have supine MRI of their spine. Supine MRI does not show deformity well and in particular subluxations in the coronal plane. Standing MRI is an advance but does not show bony anatomy well, and is not widely available and the sequence times are not well tolerated by patients. It is our practice to perform standing radiographs of the spine in: (1) patients with clinical deformity, (2) patients with an MRI suggestive of possible deformity, (3) patients with a history suggestive of nerve compression but a “normal” MRI and (4) all patients over 50 years of age undergoing decompressive surgery. Coronal plane deformity may or may not need to be addressed if patients with spinal symptoms are felt likely to benefit from surgery. The deformity associated with spinal stenosis needs to be recognised and explained to the patient as part of the consent process. It may not need to be addressed but it may have implications for current or future treatments that are not within the scope of this article.
The study has only assessed the spine in the coronal plane and all the radiographs were of supine patients. This means that the study has probably underestimated the prevalence of deformity. For example in the 60–69 year old age bracket where 6% of patients had curves greater than 10° a further 13% had curves of less than 10°. We do not know how many of these subjects would have significant curves on standing radiographs and no work has been done to allow an estimation of this. We set out to investigate lumbar spine coronal abnormalities and have not considered possible associated deformity of the thoracic spine.
This is an anonymised radiographical study and we have no clinical data on the subjects included. Previous studies have been contradictory on the relationship between scoliosis and symptoms [4, 17, 19, 20]. We have not set out to and are not able to make any comment on the relationship between the presence of deformity and symptoms. Our results are supported by the findings of other studies [27] which found similar levels of deformity which started to appear in the fifth and sixth decade and were more common in women. However, they studied a smaller number of patients all presenting with low back pain. They concluded that patients with lumbar scoliosis should be considered a distinct sub-group within the low back pain population.
Osteoporosis, degenerative disc disease, osteoarthritic changes, stenosis, endochondreal abnormalities, compression fractures, facet tropism and lateral listhesis have all been implicated in the pathogenesis of lumbar scoliosis but none have been shown to be causally related [10]. Around half of the lateral listhesis in our study were at the L3/L4 level whilst three in five of curves apices were at L3. While we cannot prove any causal association this would support the idea of lateral listhesis driving further deformity.
As the population continues to age and the number of people with degenerative spinal deformity increases, further well-designed studies are needed to investigate operative intervention and outcome in this group of patients. This study does not aim to influence surgical decision making, but in demonstrating the increasing prevalence with age we do maintain that the assessment of coronal plane deformity is a necessary consideration.
Conflict of interest
No funds were received in support of this study.
References
- 1.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 2.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. 2005;32:1082–1085. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 3.Kostuik J, Bentivoglio J. The prevalence of low back pain in adult scoliosis. Spine. 1981;6:268–273. doi: 10.1097/00007632-198105000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Schwab F, Benchick el Fegoun A, Gamez L, et al. A lumbar classification of scoliosis in the adult patient: preliminary approach. Spine. 2005;30:1670–1673. doi: 10.1097/01.brs.0000170293.81234.f0. [DOI] [PubMed] [Google Scholar]
- 5.Schwab F, Smith V, Biserni M, et al. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27:387–392. doi: 10.1097/00007632-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 6.Vogt MT, Rudin DA, Palermo L, et al. Lumbar spine listhesis in older African American women. Spine J. 2003;3(4):255–261. doi: 10.1016/S1529-9430(03)00024-X. [DOI] [PubMed] [Google Scholar]
- 7.Vogt MT, Rubin DA, San Valentin R, et al. Degenerative lumbar listhesis and bone mineral density in elderly women. The study of osteoporotic fractures. Spine. 1999;24(23):2536–2541. doi: 10.1097/00007632-199912010-00016. [DOI] [PubMed] [Google Scholar]
- 8.Glassman S, Berven S, Bridwell K. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30(6):682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 9.Grubb S, Lipscomb H, Coonrad R. Degenerative adult onset scoliosis. Spine. 1988;13:241–245. doi: 10.1097/00007632-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Tribus C. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003;11:174–183. doi: 10.5435/00124635-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Aaro S, Dahlbohn M, Svensson L. Estimation of vertebral rotation in structural scoliosis by computerised tomography. Spine. 1981;6:460–467. doi: 10.1097/00007632-198109000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Aaro S, Dahlbohn M. Estimation of vertebral rotation and the spinal and rib-cage deformity in scoliosis by computerised tomography. Spine. 1985;10(9):806–811. doi: 10.1097/00007632-198511000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Daffner S, Vaccaro A. Adult degenerative lumbar scoliosis. Am J Orthop. 2003;32(2):77–82. [PubMed] [Google Scholar]
- 14.Lowe T, Bervern S, Schwab F, et al. The SRS classification for adult deformity: building on the King/Moe and Lenke classification systems. Spine. 2006;31(19s):s119–s125. doi: 10.1097/01.brs.0000232709.48446.be. [DOI] [PubMed] [Google Scholar]
- 15.Ploumis A, Transfledt E, Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J. 2007;7:428–436. doi: 10.1016/j.spinee.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 16.Toyone T, Tanaka T, Kato D, et al. Anatomic changes in lateral spondylolisthesis associated with adult lumbar scoliosis. Spine. 2005;30(22):671–675. doi: 10.1097/01.brs.0000186581.44715.df. [DOI] [PubMed] [Google Scholar]
- 17.Garner ROE, Chaudhury E, Baker R, Harding IJ. An analysis of the appearance on supine MRI of open and closed subluxations of the lumbar spine. J Bone Joint Br Proc. 2009;91-B:494–495. [Google Scholar]
- 18.Murata Y, Takahashi K, Hanaoka E, et al. Changes in scoliotic curvature and lordotic angle during the early phase of degenerative lumbar scoliosis. Spine. 2002;27:2268–2273. doi: 10.1097/00007632-200210150-00016. [DOI] [PubMed] [Google Scholar]
- 19.Benner B, Ehni G. Degenerative lumbar scoliosis. Spine. 1979;4(6):548–552. doi: 10.1097/00007632-197911000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Prichett J, Bortel D. Degenerative symptomatic lumbar scoliosis. Spine. 1993;18:700–703. doi: 10.1097/00007632-199305000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Robin G, Span Y, Steinberg R, et al. Scoliosis in the elderly: a follow up study. Spine. 1982;7:355–359. doi: 10.1097/00007632-198207000-00005. [DOI] [PubMed] [Google Scholar]
- 22.UK Statistics Authority (2009) Population Ageing (UK National Statistics website). http://www.statistics.gov.uk/cci/nugget.asp?ID=949. Accessed 04 February 2009
- 23.UK Government Actuary Department (2009) Period and cohort expectation of life tables (UK Government Actuary Department website). http://www.gad.gov.uk/Demography_Data/Life_Tables/Eoltable06.asp. Accessed 04 February 2009
- 24.Kluba T, Dikmenli G, Dietz K, et al. Comparison of surgical and conservative treament for degenerative lumbar scoliosis. Arch Orthop Trauma Surg. 2009;129:1–5. doi: 10.1007/s00402-008-0673-z. [DOI] [PubMed] [Google Scholar]
- 25.Bridwell KH, Glassman S, Horton W, et al. Does treatment (non-operative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine. 2009;34(20):2171–2178. doi: 10.1097/BRS.0b013e3181a8fdc8. [DOI] [PubMed] [Google Scholar]
- 26.Smith JS, Shaffrey CI, Berven S. Improvement of back pain with operative and non-operative treatment in adults with scoliosis. Neurosurgery. 2009;65(1):86–93. doi: 10.1227/01.NEU.0000347005.35282.6C. [DOI] [PubMed] [Google Scholar]
- 27.Perennou D, Marcelli C, Herisson C, et al. Adult lumbar scoliosis: epidemiologic aspects in a low-back pain population. Spine. 1994;19:123–128. doi: 10.1097/00007632-199401001-00001. [DOI] [PubMed] [Google Scholar]
- 28.Baldus C, Bridwell KH, Harrast J, et al. Age-gender matched comparison of SRS instrument scores between adult deformity and normal adults: are all SRS domains disease specific? Spine. 2008;33(20):2214–2218. doi: 10.1097/BRS.0b013e31817c0466. [DOI] [PubMed] [Google Scholar]