Abstract
Background
Carpal tunnel syndrome (CTS) is the most commonly diagnosed compression neuropathy of the upper extremity. Current AAOS recommendations are to obtain a confirmatory electrodiagnostic test in patients for whom surgery is being considered. Ultrasound has emerged as an alternative confirmatory test for CTS; however, its potential role is limited by lack of adequate data for sensitivity and specificity relative to electrodiagnostic testing.
Questions/purposes
In this meta-analysis we determined the sensitivity and specificity of ultrasound in the diagnosis of CTS.
Methods
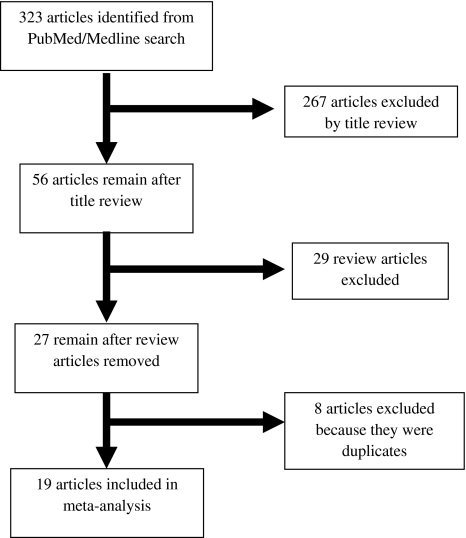
A PubMed/MEDLINE search identified 323 articles for review. After applying exclusion criteria, 19 articles with a total sample size of 3131 wrists were included for meta-analysis. Three groups were created: a composite of all studies, studies using clinical diagnosis as the reference standard, and studies using electrodiagnostic testing as the reference standard.
Results
The composite sensitivity and specificity of ultrasound for the diagnosis of CTS, using all studies, were 77.6% (95% CI 71.6–83.6%) and 86.8% (95% CI 78.9–94.8%), respectively.
Conclusions
The wide variations of sensitivities and specificities reported in the literature have prevented meaningful analysis of ultrasound as either a screening or confirmatory tool in the diagnosis of CTS. The sensitivity and specificity of ultrasound in the diagnosis of CTS are 77.6% and 86.8%, respectively. Although ultrasound may not replace electrodiagnostic testing as the most sensitive and specific test for the diagnosis of CTS given the values reported in this meta-analysis, it may be a feasible alternative to electrodiagnostic testing as the first-line confirmatory test.
Level of Evidence
Level III, systematic review of Level III studies. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
CTS is the most commonly diagnosed compression neuropathy of the upper extremity, with 500,000 decompressions performed annually in the United States and an estimated $30,000 lifetime cost for each injured worker [8, 11]. The incidence of CTS in the United States has been estimated at one to three cases per 1000 subjects per year, with a prevalence of approximately 50 cases per 1000 subjects [11]. CTS has a prevalence of 5% in the general population [14], and more than 3.8 million patients were seen by physicians regarding CTS in 2003 [11].
The recent AAOS Clinical Guidelines define CTS as a symptomatic compression neuropathy of the median nerve at the level of the wrist characterized physiologically by evidence of increased pressure in the carpal tunnel and decreased function of the nerve at that level [11]. Recommendations include obtaining confirmatory electrodiagnostic testing (EDX) in patients for whom surgery is being considered [11]. However, EDX is uncomfortable for patients, time consuming, and expensive (EDX is nearly twice as expensive as ultrasound at our institution). Studies also have questioned the value added by EDX in the diagnosis of CTS when compared with clinical diagnosis alone [6], and EDX studies are normal in 16% to 34% of patients with clinically defined CTS [9, 13, 29].
The current gold standard for the diagnosis of CTS [6, 7, 11] is a topic of debate. EDX traditionally has been used as the confirmatory test for the diagnosis of CTS; however, ultrasound has garnered interest as an alternative diagnostic test for CTS [2, 5, 12–14, 17, 22, 24, 27]. Studies have used either EDX [4, 15, 25, 28, 32] or clinical diagnosis [4, 12, 14, 15, 30] as the reference standard when determining the sensitivity and specificity of ultrasound in the diagnosis of CTS. The cutoff point used for determining abnormality in the measurement of nerve conduction is highly variable, making comparison between studies difficult [14].
Ultrasound has a sensitivity of as much as 94% and a specificity of as much as 98% for diagnosis of CTS, when measuring the cross-sectional area of the median nerve at the inlet of the carpal tunnel [3, 4, 15, 16, 25, 30, 32]. The cross-sectional area of the median nerve at the inlet of the carpal tunnel (at the level of the pisiform) is the most sensitive and specific ultrasound finding in patients with CTS [20, 28]. The wide variation of sensitivities and specificities reported in the literature has prevented meaningful analysis of ultrasound as a screening or confirmatory tool in the diagnosis of CTS. Although ultrasound may not replace EDX as the gold standard test for confirming the diagnosis of CTS, it may replace EDX as the first-line test depending on the cross-sectional area value chosen by the investigator.
Some studies have assumed the superiority of EDX over ultrasound for confirmation of a clinical diagnosis of CTS. However, a prospective analysis by Witt et al. [29] found nerve conduction studies to be normal in 25% of cases of clinically suspected CTS. Jablecki et al. [10], in a review of EDX for the American Association of Electrodiagnostic Medicine, found EDX missed the diagnosis of CTS in 16% to 34% of patients with clinically defined disease. EDX and ultrasound are highly operator dependent. These studies confirm the need to continually search for a better confirmatory test and emphasize the diagnostic gap between ultrasound and EDX is narrower than some might think.
In this meta-analysis, we attempt to answer the following questions: What are the sensitivity and the specificity of ultrasound for the diagnosis of CTS in the following three scenarios: (1) using all studies regardless of reference standard; (2) using all studies with EDX as the reference standard; and (3) using all studies with clinical diagnosis as the gold standard.
Search Strategy and Criteria
A PubMed/MEDLINE search was conducted using MeSH keywords “carpal tunnel syndrome” and “ultrasonography”; a keyword search using “carpal” and “tunnel” and “ultrasound”; and a keyword search using “median nerve” and “ultrasonography.” The references of all articles included in the meta-analysis also were reviewed for additional relevant articles. We identified 323 articles for review (Fig. 1). Articles were included in the meta-analysis if they reported the sensitivity and specificity of ultrasound in the diagnosis of CTS using either clinical diagnosis or EDX as the reference standard. EDX is defined as electromyography (EMG), nerve conduction studies (NCS), or a combination of the two. Studies were not included or excluded based on the type of EDX testing performed. Exclusion criteria included articles not published in the English language and review articles and studies that did not report sensitivity and specificity data. We excluded 267 articles based on a title review that determined the article did not address ultrasound of the median nerve in the diagnosis of CTS. We then excluded 29 review articles and eight duplicate articles. An additional eight articles were excluded after full article review revealed complete sensitivity and specificity data were not published. Application of the exclusion criteria left 19 articles to be included in the meta-analysis (Table 1). The studies included in the meta-analysis used a heterogeneous set of criteria to define positive EDX testing, including motor and sensory latencies and NCS findings. The studies also used heterogeneous criteria to define a cutoff value (mm2) for a positive ultrasound. Nearly all of the studies included in the meta-analysis excluded patients with diabetes, pregnancy, and other systemic disorders.
Fig. 1.
A flow diagram shows the inclusion and exclusion criteria of articles based on our systematic review of the literature.
Table 1.
Studies included in the meta-analysis and reported sensitivity and specificity
| Study | Reference standard | Cross-sectional area cutoff (mm2) | Number of wrists | Sensitivity (%) (95% CI) | Specificity (%) (95% CI) |
|---|---|---|---|---|---|
| Pinilla et al. [24] | Clinical | 6.5 | 70 | 90.0 (75.4–96.8) | 93.3 (76.5–98.8) |
| Pastare et al. [23] | Clinical | 9 | 84 | 62.1 (49.3–73.5) | 100 (78.1–00) |
| Altinok et al. [1] | Clinical | 9 | 80 | 65.0 (48.3–78.9) | 92.5 (78.5–8.0) |
| Padua et al. [22] | Clinical | 10 | 54 | 70.4 (56.2–81.6) | |
| Visser et al. [27] | Clinical | 10 | 305 | 78.0 (70.8–83.8) | 91.0 (84.9–95.2) |
| El Miedany et al. [5] | Clinical | 10 | 254 | 97.9 (92.0–99.6) | 100 (97.0–100) |
| Kwon et al. [14] | Clinical | 10.7 | 82 | 65.9 (49.3–79.4) | 63.4 (46.9–77.4) |
| Kele et al. [12] | Clinical | 11 | 110 | 74.0 (64.2–81.4) | 98.0 |
| Wong et al. [30] | EDX | 9 | 96 | 94.3 (85.3–98.2) | 65.4 (44.4–82.1) |
| Ziswiler et al. [32] | EDX | 9 | 101 | 85.9 (77.4–97.1) | 69.6 (47.0–85.9) |
| Wong et al. [30] | EDX | 9 | 124 | 80.0 (66.1–88.9) | 51.0 (39.3–63.4) |
| Duncan et al. [4] | EDX | 9 | 170 | 82.0 (73.3–88.9) | 97.0 (88.8–99.5) |
| Ashraf et al. [2] | EDX | 9 | 150 | 80.0 (68.4–88.3) | 77.5 (66.5–85.8) |
| Yesildag et al. [31] | EDX | 10.5 | 224 | 89.0 (82.8–93.5) | 95.0 (86.4–98.3) |
| Sarria et al. [25] | EDX | 11 | 105 | 74.6 (61.8–84.4) | 57.1 (41.1–71.9) |
| Wiesler et al. [28] | EDX | 11 | 130 | 90.9 (77.4–97.1) | 83.7 (73.9–90.5) |
| Moran et al. [17] | EDX | 12.3 | 70 | 62.0 (47.2–75.0) | 95.0 (73.1–99.7) |
| Nakamichi and Tachibana [20] | EDX | 13 | 822 | 57.0 (52.1–61.8) | 97.0 (94.8–98.4) |
| Lee et al. [15] | EDX | 15 | 100 | 88.0 (79.6–93.4) | 96.0 |
CI = confidence interval; EDX = electrodiagnostic testing.
The sensitivity, specificity, and likelihood ratios with 95% CIs were calculated separately for each study. Sensitivity indicates the true-positive rate and specificity indicates the true-negative rate. Sensitivity and specificity are characteristics of the diagnostic test and are not influenced by the incidence of the outcome. The positive likelihood ratio indicates the true-positive rate divided by the false-positive rate and the negative likelihood ratio indicates the true-negative rate divided by the false-negative rate. Likelihood ratios are useful in calculating post-test probabilities in the clinical setting.
A weighted random effects model was used to calculate composite sensitivity, specificity, and likelihood ratios from the combined studies. The weights applied to the analysis were based on the different sample sizes of the included studies. A random effects model was chosen to accommodate significant heterogeneity among the results of the individual studies (I2 = 93.7; p < 0.001). The weighted random effects composite sensitivity, specificity, and likelihood ratios were calculated along with 95% CIs.
Results
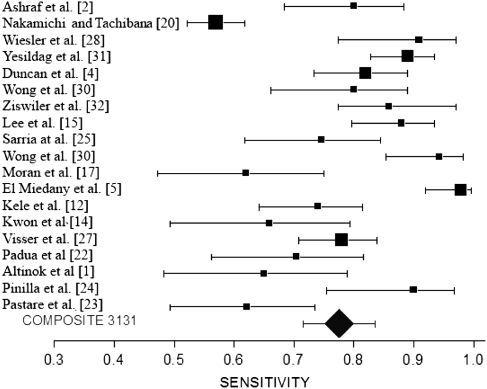
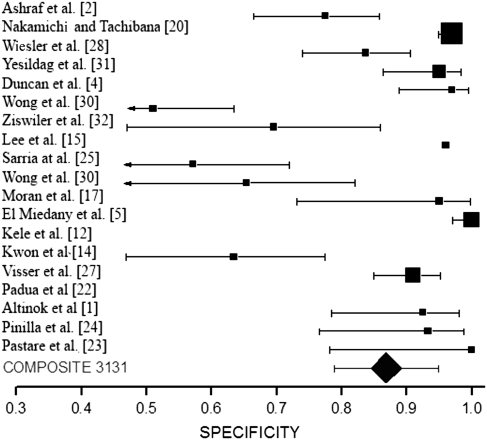
The composite pooled sensitivity and specificity (Table 2) of ultrasound for the diagnosis of CTS were 77.6% (95% CI 71.6%–83.6%) and 86.8% (95% CI 78.9%–94.8%), respectively. These values represent the pooled sensitivity and specificity of all articles included in the meta-analysis, regardless of the reference standard used. The 19 articles included in the meta-analysis had a total sample size of 3131 wrists for analysis (Table 1). Forest plots, which graphically show the sensitivity (Fig. 2) and specificity (Fig. 3), with 95% confidence intervals for each study and the composite sensitivity (Fig. 2) and specificity (Fig. 3), respectively, with 95% confidence intervals are shown. The size of the symbol reflects the sample size of each study and of the combined results. The sensitivity reported in these studies ranged from 57% to 98% and the specificity ranged from 63% to 100%. All studies included in the meta-analysis were prospective case series.
Table 2.
Sensitivity and specificity values for the three groups
| Reference standard | Sensitivity (%) (95% CI) | Specificity (%) (95% CI) |
|---|---|---|
| Clinical | 77.3 (62.1–84.6) | 92.8 (81.3–100) |
| EDX | 80.2 (71.3–89.0) | 78.7 (66.4–91.1) |
| Composite | 77.6 (71.6–83.6) | 86.8 (78.9–94.8) |
CI = confidence interval; EDX = electrodiagnostic testing.
Fig. 2.
A forest plot shows the sensitivity and 95% CI for each study and the composite sensitivity with the 95% CI. Symbol size reflects the sample size of each study and of the combined results. NCS = electrodiagnostic studies; C = clinical.
Fig. 3.
A forest plot shows the specificity for each study and the composite specificity with the 95% CI. Symbol size reflects the sample size of each study and of the combined results. NCS = electrodiagnostic studies; C = clinical.
Eight studies, with 1039 wrists, used clinical diagnosis as the reference standard. The definition of a positive clinical diagnosis was based on constellations of signs and symptoms, which varied among studies. The pooled sensitivity and specificity using clinical diagnosis as the reference standard were 77.3% (95% CI 62.1%–84.6%) and 92.8% (95% CI 81.3%–100%), respectively.
Eleven studies, with 2092 wrists, used EDX as the reference standard. The pooled sensitivity and specificity using EDX as the reference standard were 80.2% (95% CI 71.3%–89.0%) and 78.7% (95% CI 66.4%–91.1%), respectively.
Discussion
The shortfalls of EDX in the confirmation of the diagnosis of CTS have led physicians to search for an alternative method to confirm the diagnosis. Ultrasonographic measurement of the median nerve at the inlet of the carpal tunnel has emerged as a viable alternative to EDX. Although ultrasound is unable to evaluate proximal etiologies of carpal tunnel-like symptoms, it does have the ability to detect other causes of compression in the carpal tunnel such as space-occupying lesions and tenosynovitis [18, 19, 26]. Although some studies have confirmed the utility of ultrasound in the diagnosis of CTS, their small sample size and the heterogeneity of study design has made it difficult to draw definitive conclusions regarding the sensitivity and specificity of ultrasonographic measurement of the median nerve in the diagnosis of CTS [17, 22, 24]. In this meta-analysis, we determined the sensitivity and specificity of ultrasound as a diagnostic tool for CTS. The analysis included a large number of wrists (3131) in the statistical analysis. This represents a sample size 30 times larger than included in the majority of studies included in the meta-analysis [1, 2, 4, 12, 14, 15, 17, 22–25, 27, 28, 30–32] and nearly four times larger than in the largest series [20] available.
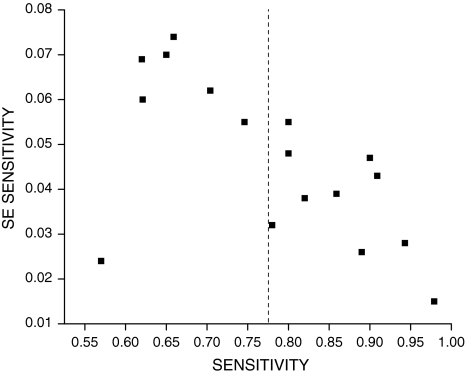
Our meta-analysis is not without limitations. The first limitation is related to the heterogeneity of the studies regarding their cross-sectional area cutoffs, criteria for clinical diagnosis, and criteria for EDX diagnosis of CTS. The authors of these studies have selected arbitrary cutoff values for the cross-sectional area of the median nerve, using receiver operating curves (ROCs), to optimize the sensitivity and specificity of the test. Our meta-analysis of the published data allowed a pooled composite of multiple cutoff values. Second, an inherent weakness of the studies using clinical diagnosis as the reference standard is the use of asymptomatic control subjects. Patients without clinical signs and symptoms of CTS may still have inflammation and thickening of the median nerve (only 4% of asymptomatic patients will have abnormal ultrasound examinations), but the changes have not yet caused clinical symptoms and signs [19]. Studies using EDX as the gold standard have substantial false-positive and false-negative rates [4, 9, 10, 14, 22–24]. Third, the use of ROCs to determine optimal cutoff values for the diagnosis of CTS also clouds the interpretation of data. Some authors have chosen to optimize the sensitivity and specificity [4, 5, 30]. However, if one wishes to use ultrasound as a confirmatory test, specificity could be optimized at the expense of sensitivity. By choosing a higher cutoff value, false negatives can be eliminated and the surgeon can have the confirmatory test that the AAOS has recommended. Fourth, a funnel plot (Fig. 4) of sensitivities indicated a trend in publication bias, with larger studies reporting higher sensitivities. The standard error for each study reflects the relative sample size and when plotted shows trends toward biased estimates. Usually larger studies have smaller standard errors. A sensitivity analysis was performed by stepwise removal of the two largest studies with recalculation of the composite sensitivity and specificity. Removal of these studies did not substantially alter the composite estimate of sensitivity and specificity.
Fig. 4.
A funnel plot of sensitivities indicated a trend in publication bias, with larger studies reporting higher sensitivities. The standard error (SE) reflects the variability and relative sample size of each study and when plotted shows trends toward biased estimates. The dotted line is provided as a reference to the composite estimate from the combined studies.
Eleven studies used EDX as the reference standard to determine the presence of CTS, with sensitivity ranging from 57% to 94% and specificity ranging from 51% to 97%. Four of the 11 studies [2, 4, 30, 32] used a cutoff point of 9 mm2, reporting sensitivities of 80% to 90% and specificities of 51% to 97%. The largest study included in the meta-analysis, by Nakamichi and Tachibana [21], reported on 822 wrists with a sensitivity of 57% and a specificity of 97% using a cutoff value of 13 mm2. The high specificity in their series shows the ability of ultrasound to rule in the diagnosis of CTS. Graham et al. [6, 7] and Keith et al. [11] also questioned the added value of EDX in patients with a high pretest likelihood of CTS. In patients with a pretest probability greater than 80%, EDX added little change of increasing the probability of diagnosis. This group of patients would be the perfect subset to undergo ultrasound diagnosis of CTS as a first-line test, rather than EDX.
Eight studies used a constellation of clinical findings as the reference standard to determine the presence of CTS [1, 5, 12, 14, 22–24, 27]. The sensitivity and specificity reported in these studies ranged from 62% to 98% and 63% to 100%, respectively. El Miedany et al. [5], in a series of 254 wrists, used a cutoff value of 10 mm2 to achieve a sensitivity of 98% and a specificity of 100%, the highest of any published series using clinical diagnosis as the reference standard. Kwon et al. [14], in a series of 82 wrists, reported sensitivity and specificity of 66% and 63%, respectively, and concluded ultrasound was not accurate enough to replace EDX as the preferred diagnostic study for CTS. However, the authors admitted their criteria for positive clinical diagnosis of CTS may have been too strict, thus biasing their results toward cases of advanced CTS.
The wide variation of sensitivities and specificities reported in various studies in the literature has prevented meaningful analysis of ultrasound as a screening or confirmatory tool in the diagnosis of CTS. In this meta-analysis, we calculated the sensitivity and specificity of ultrasound in the diagnosis of CTS to be 77.6% and 86.8%, respectively. The sensitivity and specificity when using EDX as the gold standard are 80.2% and 78.7%, respectively. The sensitivity and specificity of ultrasound when using clinical diagnosis as the gold standard are 77% and 93%, respectively, and compare favorably with the EDX sensitivity and specificity defined by Graham (69% and 97%, respectively) [6]. Although ultrasound may not replace EDX as the most sensitive and specific test for the diagnosis of CTS given the values reported in this meta-analysis, it potentially can be an alternative to EDX as the first-line confirmatory test. Additional research is necessary to determine the role of ultrasound for patients with clinical symptoms of CTS, but who have negative EDX studies.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
This work was performed at Temple University Hospital.
References
- 1.Altinok T, Baysal O, Karakas HM, Sigirci A, Alkan A, Kayhan A, Yologlu S. Ultrasonographic assessment of mild and moderate idiopathic carpal tunnel syndrome. Clin Radiol. 2004;59:916–925. doi: 10.1016/j.crad.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 2.Ashraf AR, Jali R, Moghtaderi AR, Yazdani AH. The diagnostic value of ultrasonography in patients with electrophysiologicaly confirmed carpal tunnel syndrome. Electromyogr Clin Neurophysiol. 2009;49:3–8. [PubMed] [Google Scholar]
- 3.Buchberger W, Judmaier W, Birbamer G, Lener M, Schmidauer C. Carpal tunnel syndrome: diagnosis with high-resolution sonography. AJR Am J Roentgenol. 1992;159:793–798. doi: 10.2214/ajr.159.4.1529845. [DOI] [PubMed] [Google Scholar]
- 4.Duncan I, Sullivan P, Lomas F. Sonography in the diagnosis of carpal tunnel syndrome. AJR Am J Roentgenol. 1999;173:681–684. doi: 10.2214/ajr.173.3.10470903. [DOI] [PubMed] [Google Scholar]
- 5.El Miedany YM, Aty SA, Ashour S. Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: substantive or complementary tests? Rheumatology (Oxford) 2004;43:887–895. doi: 10.1093/rheumatology/keh190. [DOI] [PubMed] [Google Scholar]
- 6.Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2008;90:2587–2593. doi: 10.2106/JBJS.G.01362. [DOI] [PubMed] [Google Scholar]
- 7.Graham B, Regehr G, Naglie G, Wright JG. Development and validation of diagnostic criteria for carpal tunnel syndrome. J Hand Surg Am. 2006;31:919–924. [PubMed] [Google Scholar]
- 8.Hanrahan LP, Higgins D, Anderson H, Smith M. Wisconsin occupational carpal tunnel syndrome surveillance: the incidence of surgically treated cases. Wis Med J. 1993;92:685–689. [PubMed] [Google Scholar]
- 9.Jablecki CK, Andary MT, Floeter MK, Miller RG, Quartly CA, Vennix MJ, Wilson JR; American Association of Electrodiagnostic Medicine; American Academy of Neurology; American Academy of Physical Medicine and Rehabilitation. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002;58:1589–1592. [DOI] [PubMed]
- 10.Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve. 1993;16:1392–1414. doi: 10.1002/mus.880161219. [DOI] [PubMed] [Google Scholar]
- 11.Keith MW, Masear V, Chung KC, Maupin K, Andary M, Amadio PC, Watters WC, III, Goldberg MJ, Haralson RH, III, Turkelson CM, Wies JL, McGowan R. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91:2478–2479. doi: 10.2106/JBJS.I.00643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kele H, Verheggen R, Bittermann HJ, Reimers CD. The potential value of ultrasonography in the evaluation of carpal tunnel syndrome. Neurology. 2003;61:389–391. doi: 10.1212/01.wnl.0000073101.04845.22. [DOI] [PubMed] [Google Scholar]
- 13.Koyuncuoglu HR, Kutluhan S, Yesildag A, Oyar O, Guler K, Ozden A. The value of ultrasonographic measurement in carpal tunnel syndrome in patients with negative electrodiagnostic tests. Eur J Radiol. 2005;56:365–369. doi: 10.1016/j.ejrad.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 14.Kwon BC, Jung KI, Baek GH. Comparison of sonography and electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Hand Surg Am. 2008;33:65–71. doi: 10.1016/j.jhsa.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 15.Lee D, Holsbeeck MT, Janevski PK, Ganos DL, Ditmars DM, Darian VB. Diagnosis of carpal tunnel syndrome: ultrasound versus electromyography. Radiol Clin North Am. 1999;37:859–872. doi: 10.1016/S0033-8389(05)70132-9. [DOI] [PubMed] [Google Scholar]
- 16.Leonard L, Rangan A, Doyle G, Taylor G. Carpal tunnel syndrome: is high-frequency ultrasound a useful diagnostic tool? J Hand Surg Br. 2003;28:77–79. doi: 10.1054/jhsb.2002.0869. [DOI] [PubMed] [Google Scholar]
- 17.Moran L, Perez M, Esteban A, Bellon J, Arranz B, del Cerro M. Sonographic measurement of cross-sectional area of the median nerve in the diagnosis of carpal tunnel syndrome: correlation with nerve conduction studies. J Clin Ultrasound. 2009;37:125–131. doi: 10.1002/jcu.20551. [DOI] [PubMed] [Google Scholar]
- 18.Nakamichi K, Tachibana S. The use of ultrasonography in detection of synovitis in carpal tunnel syndrome. J Hand Surg Br. 1993;18:176–179. doi: 10.1016/0266-7681(93)90100-T. [DOI] [PubMed] [Google Scholar]
- 19.Nakamichi K, Tachibana S. Unilateral carpal tunnel syndrome and space-occupying lesions. J Hand Surg Br. 1993;18:748–749. doi: 10.1016/0266-7681(93)90236-9. [DOI] [PubMed] [Google Scholar]
- 20.Nakamichi KI, Tachibana S. Enlarged median nerve in idiopathic carpal tunnel syndrome. Muscle Nerve. 2000;23:1713–1718. doi: 10.1002/1097-4598(200011)23:11<1713::AID-MUS7>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 21.Nakamichi KI, Tachibana S. Ultrasonographic measurement of median nerve cross-sectional area in idiopathic carpal tunnel syndrome: diagnostic accuracy. Muscle Nerve. 2002;26:798–803. doi: 10.1002/mus.10276. [DOI] [PubMed] [Google Scholar]
- 22.Padua L, Pazzaglia C, Caliandro P, Granata G, Foschini M, Briani C, Martinoli C. Carpal tunnel syndrome: ultrasound, neurophysiology, clinical and patient-oriented assessment. Clin Neurophysiol. 2008;119:2064–2069. doi: 10.1016/j.clinph.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 23.Pastare D, Therimadasamy AK, Lee E, Wilder-Smith EP. Sonography versus nerve conduction studies in patients referred with a clinical diagnosis of carpal tunnel syndrome. J Clin Ultrasound. 2009;37:389–393. doi: 10.1002/jcu.20601. [DOI] [PubMed] [Google Scholar]
- 24.Pinilla I, Martin-Hervas C, Sordo G, Santiago S. The usefulness of ultrasonography in the diagnosis of carpal tunnel syndrome. J Hand Surg Eur Vol. 2008;33:435–439. doi: 10.1177/1753193408090396. [DOI] [PubMed] [Google Scholar]
- 25.Sarria L, Cabada T, Cozcolluela R, Martinez-Berganza T, Garcia S. Carpal tunnel syndrome: usefulness of sonography. Eur Radiol. 2000;10:1920–1925. doi: 10.1007/s003300000502. [DOI] [PubMed] [Google Scholar]
- 26.Vugt RM, Dalen A, Bijlsma JW. The current role of high-resolution ultrasonography of the hand and wrist in rheumatic diseases. Clin Exp Rheumatol. 1998;16:454–458. [PubMed] [Google Scholar]
- 27.Visser LH, Smidt MH, Lee ML. High-resolution sonography versus EMG in the diagnosis of carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 2008;79:63–67. doi: 10.1136/jnnp.2007.115337. [DOI] [PubMed] [Google Scholar]
- 28.Wiesler ER, Chloros GD, Cartwright MS, Smith BP, Rushing J, Walker FO. The use of diagnostic ultrasound in carpal tunnel syndrome. J Hand Surg Am. 2006;31:726–732. doi: 10.1016/j.jhsa.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 29.Witt JC, Hentz JG, Stevens JC. Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve. 2004;29:515–522. doi: 10.1002/mus.20019. [DOI] [PubMed] [Google Scholar]
- 30.Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: diagnostic usefulness of sonography. Radiology. 2004;232:93–99. doi: 10.1148/radiol.2321030071. [DOI] [PubMed] [Google Scholar]
- 31.Yesildag A, Kutluhan S, Sengul N, Koyuncuoglu HR, Oyar O, Guler K, Gulsoy UK. The role of ultrasonographic measurements of the median nerve in the diagnosis of carpal tunnel syndrome. Clin Radiol. 2004;59:910–915. doi: 10.1016/j.crad.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 32.Ziswiler HR, Reichenbach S, Vogelin E, Bachmann LM, Villiger PM, Juni P. Diagnostic value of sonography in patients with suspected carpal tunnel syndrome: a prospective study. Arthritis Rheum. 2005;52:304–311. doi: 10.1002/art.20723. [DOI] [PubMed] [Google Scholar]