Abstract
Background
Although the health-related quality of life (HRQL) for patients who are obese seems to improve after TKA, the magnitude of improvement and the associated factors remain controversial. We previously found body mass index was not associated with changes in HRQL after TKA.
Questions/purposes
The purposes of this secondary analysis were to determine which patient characteristics and surgical factors were associated with worse health status after TKA in patients who are severe or morbidly obese.
Methods
We assessed 60 patients (53 females; mean age, 70 years) 12 months after surgery. The mean number of comorbidities was 2.5. Mean lower limb anthropometric index scores were: suprapatellar, 1.6; infrapatellar, 2; and suprapatellar/infrapatellar, 1.2. Intraoperative difficulty (IOD) was Grade 0, 40%; Grade 1, 48%; and Grade 2, 12%. Ten patients (17%) had complications. We measured HRQL using the disease-specific WOMAC questionnaire. Patient characteristics (sociodemographic variables, BMI, comorbidity, lower limb anthropometry) and surgical factors (IOD, complications, postoperative medical data) were collected. Associations between WOMAC dimension scores at 12 months and patient characteristics and surgical factors were analyzed using linear regression models.
Results
Factors associated with worse WOMAC dimension scores in patients who were obese included the number of comorbidities, an infrapatellar index percentile less than 75, IOD Grade 2, and the number of complications after discharge.
Conclusions
For patients with knee osteoarthritis who were severe or morbidly obese, various lower limb anthropometric features, degree of IOD, and postoperative complications negatively influenced postoperative WOMAC scores.
Level of Evidence
Level II Prognostic Study. See Guidelines for a complete description of levels of evidence.
Introduction
As in other developed countries, increasing life expectancy in Spain has led to an increase in osteoarthritis (OA) [26]. At the same time, the incidence of obesity has increased [33], leading to greater morbidity. One study suggested a link between knee OA and obesity [19], which is reflected by the increased number of TKAs in individuals who are obese [6]. TKA can improve the HRQL of patients with knee OA, reducing pain and increasing functional capacity when conservative treatment fails [19]. Some suggest the greatest improvements in pain and function occur during the first 3 to 6 months after surgery [4, 14]. However, patient characteristics and surgical factors are important determinants of outcomes in TKA. Studies show that many factors are associated with HRQL after TKA but that not all are identified, none is decisive in itself, and controversy remains regarding their impact [10].
Some studies of TKA in patients who are severe and morbidly obese have concentrated on aspects such as surgical complications and mechanical failure [6, 9, 10, 13, 28]. Few short- or long-term studies have focused on health outcomes or HRQL and those that have are methodologically heterogeneous [6, 9, 10, 13, 27, 28].
In previous studies, attempts were made to standardize protocols and define variables according to their possible influence on TKA outcomes [24, 25]. Additionally, the patient’s perspective was incorporated in the evaluation of outcomes using HRQL measures [23, 24]. Disease-specific instruments focus on issues related to a particular health condition and can be used in therapeutic management [22]. In knee OA, the disease-specific WOMAC (LK 3.0) questionnaire is used for assessing functional outcomes in TKA [1] and often is used after total joint replacement to measure impairment, activity limitations, and participation restrictions [14]. Some studies suggest that condition- or limb-specific instruments are more sensitive to change [5, 14, 29].
In a case-control study (Núñez M, Lozano L, Núñez E, Sastre S, Luis Del Val J, Suso S. Good quality of life in severely obese total knee replacement patients: a case control study. Obes Surg. 2010. Submitted.), we found body mass index (BMI) did not influence HRQL (measured using the WOMAC) 12 months after TKA. HRQL improved substantially in the study group of 60 patients with a BMI of 35 or greater and in the control group of 60 patients with a BMI less than 35. Patients who were severe and morbidly obese and those who were not obese had similar change scores and TKA outcomes in terms of HRQL at 12 months after TKA. Patients who were obese had more intraoperative difficulties and more severe postoperative complications. We presumed identifying factors associated with worse outcomes in that original study group of patients who were severe or morbidly obese could help to identify patients requiring additional preoperative measures or a different surgical approach.
The purpose of this secondary analysis therefore was to determine which patient characteristics and surgical factors were associated with changes in HRQL after TKA in patients who were severe and morbidly obese.
Patients and Methods
We retrospectively reviewed 68 patients with knee OA (according to Kellgren and Lawrence criteria [16]) and severe or morbid obesity (Class II BMI ≥ 35 and Class III BMI ≥ 40, respectively [19]) admitted for TKA between January 2006 and February 2007. We excluded patients with the following: functional illiteracy, inflammatory or other severe musculoskeletal conditions (eg, rheumatoid arthritis, sciatica), metabolic or neoplastic disease, and severe psychopathology or comorbidity (defined as a diagnosis, such as heart failure or respiratory disease severe enough to impede total participation in procedures). Using these criteria we excluded five patients (one with rheumatoid arthritis, two with neoplasia, one with severe heart failure, and one with renal failure with hemodialysis). Accepting an alpha risk of 0.05 and a beta risk of 0.20 in a bilateral contrast, 55 patients were needed to detect a difference of less than 10 points between mean preoperative and postoperative WOMAC scores [3], which we judged a clinically important difference [1, 27]. We assumed a standard deviation of 25. The sample was overestimated by 10% to allow for possible losses. Of the 63 patients recruited, three were lost to followup (one refused to attend hospital appointments and two could not be contacted). The remaining 60 patients completed the followup and were included in the final analysis. There were 53 women with a mean age of 70.2 years (± 6.7 years) (Table 1). The mean number of comorbidities was 2.5 (± 1.5). All patients were followed for 1 year. The study was approved by the hospital ethics committee and complied with current norms concerning data confidentiality. All patients gave written informed consent to participate in the study.
Table 1.
Baseline patient characteristics
| Age mean (SD) | 70.2 (6.7) |
| Male (%) | 7 (11.7) |
| Female (%) | 53 (88.3) |
| Number of preexisting comorbidities, mean (SD) | 2.5 (1.5) |
| Hypertension (%) | 42 (70) |
| Diabetes (%) | 14 (23.3) |
| Respiratory disease (%) | 12 (20) |
| Digestive disease (%) | 11 (18.3) |
| Psychiatric disease/depression (%) | 9 (15) |
| Heart disease (%) | 7 (11.7) |
| BMI mean (SD) | 39.9 (3.8) |
| Class II = 35–39.9 kg/m2 n (%) | 33 (55) |
| Class III = ≥ 40 kg/m2 n (%) | 27 (45) |
SD = standard deviation; N = number; BMI = body mass index (kg/m2).
Preoperatively we determined the lower limb suprapatellar, infrapatellar, and suprapatellar/infrapatellar indices [17]. Briefly, the suprapatellar circumference (measured at 4 cm proximal to the superior pole of the patella), infrapatellar circumference (measured at the anterior tibial tuberosity), and the length of the limb to be treated surgically (measured from the anterosuperior iliac crest to the center of the anterior face of the ankle) were determined. The same flexible, inelastic tape measure, calibrated in centimeters, was used for all measurements. The anthropometric indices calculated were the length of the limb/suprapatellar circumference ratio (suprapatellar index), length of the limb/infrapatellar circumference ratio (infrapatellar index), and the suprapatellar circumference/infrapatellar circumference ratio (suprapatellar/infrapatellar index). The mean scores were: suprapatellar, 1.6 (± 0.2); infrapatellar, 2 (± 0.2); and suprapatellar/infrapatellar, 1.2 (± 0.1). Six patients (10%) had deformities of two axes (varus, valgus) greater than 15°.
All surgeries were performed by the same surgeon (LL). The surgical technique was the same in all cases: an anteromedial approach without patellar resurfacing using a femoral and tibial intramedullary cutting guide. The femoral and tibial components were cemented. A standard (nonconstrained) prosthesis (Profix; Smith & Nephew Inc, Memphis, TN, USA) [31] was used in all patients.
Given the lack of standardized variables to determine the degree of IOD, we designed a multi-item questionnaire [22, 23] to identify possible surgical problems and degree of IOD presumed by the presence of more than one variable of surgical difficulty in the same operation. The six items were chosen for their relevance and use in other studies. Five senior orthopaedic surgeons (MN, LL, EN, JS, SS) evaluated all questionnaire items on an index of 1 to 5 for clarity, relevance, and importance. All items were scored at 4 or greater and no modifications were deemed necessary. The six variables of surgical difficulty selected were: (1) an approach requiring osteotomy of the tibial tuberosity, (2) bone defects requiring bone substitutes (staples, cement, prosthetic supplements), (3) severe intraoperative alteration of patellar tracking, (4) deformity of two axes (varus, valgus) greater than 15°, use of new techniques (minimally invasive surgery [MIS] or navigated surgery), (5) senior surgeon versus junior surgeon, and (6) surgical time longer than 105 minutes if any previous variables were present. The degree of IOD was defined as the number of the six variables present: 0 = no difficulty (ie, none of the above variables present), 1 = slight difficulty (1-2 problems during the intervention), 2 = medium difficulty (3-4 problems), and 3 = substantial difficulty (> 4 problems). The degrees of IOD were Grade 0, 40%; Grade 1, 48%; and Grade 2, 12%. Patients with Grade 1 required lateral release to balance patellar tracking or lateral and medial release for soft tissue balancing to correct central varus or valgus deviation greater than 15°. Patients with Grade 2 required lateral release in addition to lateral or medial soft tissue balancing to correct central varus or valgus deviation greater than 15° with a surgical time greater than 105 minutes. The mean hospital stay was 6.3 days (± 2.2 days). At discharge, patients received a booklet with advice regarding care of the wound and possible signs of complications.
Patients were hospitalized for 1 week, during which time they received physiotherapy to achieve flexion of 90° and autonomous walking using canes at discharge. Home rehabilitation lasted for 1 month. TKA, rehabilitation, and other treatments were standardized according to hospital protocols. Patients were treated with low molecular weight heparin as prophylaxis for thromboembolic events for 1 month and two doses of cefuroxime, 1.5 g, were administered as antibiotic prophylaxis.
Patients were seen 15 days after surgery to check the surgical wound and remove stitches. A followup at 3 months included radiography, including telemetry with lower limb loading, and a clinical evaluation. Additional clinical evaluations were obtained at 6 and 12 months.
Self-reported health status was measured by the Spanish version of the WOMAC questionnaire [1, 3], which contains three dimensions: pain, stiffness, and function. A total score combining the three dimensions may be used. WOMAC dimension scores were assessed at baseline and 12 months after surgery. All WOMAC data were normalized to a 0 to 100 scale (best to worst) for each WOMAC dimension [1, 3]. The number and type of major complications evaluated after discharge included: deformity of the lower limb, dislocation of TKA (femorotibial, femoropatellar), infection, pain, septic or aseptic loosening (patellar, tibial, femoral), extensor muscle failure, deep vein thrombosis, and others [20, 32].
One observer (JMS) evaluated alignment on long-leg coronal standing radiographs of the lower limb (varus-valgus ± 3° by goniometer). A descriptive analysis was made using univariable frequency tabulation for categorical variables, or mean values and standard deviation for continuous variables.
Differences between mean scores at baseline and 12 months in the WOMAC pain, stiffness, and function dimensions were evaluated using the Wilcoxon matched pairs signed ranks test. The effect size was calculated for the different outcome measures using the formula: effect size = mean change/standard deviation of preoperative results. The effect size is a standardized measure that provides information regarding the magnitude of change before and after TKA. An effect size of 0.8 or greater is considered large.
The postoperative influence of patient characteristics and surgical factors on HRQL was evaluated using an explanatory multiple linear regression model in which the dependant variable was WOMAC dimension scores at 12 months followup, and included independent variables that were significant in the univariable analysis; the infrapatellar index (coded as: 0 = < 75%, and 1 = ≥ 75%) and the IOD (coded as: 0 = Grades 0 and 1, and 1 = Grade 2) were dichotomized previously. The selection criterion for inclusion of variables in the multivariable model was forward-stepwise with an entry criterion of p < 0.05 and an exit criterion of p > 0.10. The 95% confidence intervals were measured when appropriate. The statistical analysis was performed using SPSS v16.0 for Windows program (SPSS Inc, Chicago, IL, USA).
Results
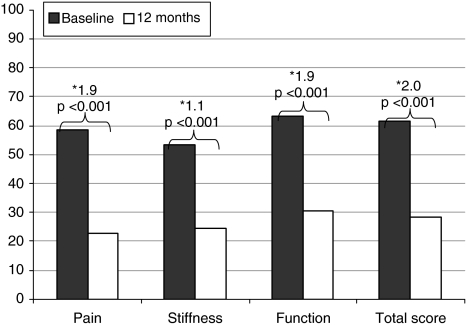
We observed improvements (p < 0.001) in the pain, stiffness, and functional WOMAC dimension scores at 12 months followup compared with baseline. WOMAC dimension scores, change scores, and effect size at baseline and after 12 months were compared (Fig. 1).
Fig. 1.
WOMAC dimension scores at baseline and 12 months after TKA are shown. The three WOMAC scales were normalized to a 0 to 100 scale for each separate WOMAC dimension, where 0 represents the best health status and 100 the worse health status. *Effect size; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index.
With respect to patient characteristics, the number of comorbidities was associated with higher (p = 0.012) scores in the WOMAC function dimension. An infrapatellar index percentile less than 75 was associated with higher scores in the WOMAC pain and function dimensions (p = 0.021 and 0.023, respectively) (Table 2).
Table 2.
Variables independently associated with WOMAC dimension scores at 12 months
| Independent variables | Dependent variables* WOMAC scores at 12 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pain | Stiffness | Function | |||||||
| R2 adjusted 0.369 | R2 adjusted 0.185 | R2 adjusted 0.307 | |||||||
| Coefficients | 95% CI | p Value | Coefficients | 95% CI | p Value | Coefficients | 95% CI | p Value | |
| Number of preexisting comorbidities | 5.4 | 1.2–9.6 | 0.012 | ||||||
| Infrapatellar index less than 75% | 22.4 | 8.2–36.5 | 0.021 | 14.9 | 2.2–27.6 | 0.023 | |||
| IOD (grade 2) | 15.5 | 2.5–28.4 | 0.021 | ||||||
| Number of complications after discharge | 28.5 | 13.1–43.9 | 0.001 | 25.79 | 9.94–41.64 | 0.002 | 23.0 | 9.1–36.8 | 0.002 |
SD = Standard deviation; CI = confidence interval; IOD = degree of intraoperative difficulty; *the coefficients of regression models indicate if an increase in the independent variables is related with worse (positive coefficient) or better (negative coefficient) WOMAC dimension score. R2 adjusted is the proportion of variance in the dependent variable explained by the relevant independent variables shown. N = number; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index. The three WOMAC scales were normalized to a 0–100 scale for each separate WOMAC dimension, where 0 represents the best health status and 100 the worse health status.
With respect to surgical factors, Grade 2 IOD was associated with (p = 0.021) the WOMAC pain dimension. At 12 months followup, 10 patients (16.7%) had major complications including tibial loosening (two patients), superficial infection (one patient), distal wound dehiscence (one patient), deep infection (three patients), reintervention for anterior knee pain (one patient), and reintervention for arthrolysis attributable to stiffness (two patients). The number of complications after discharge was associated with higher (p ≤ 0.002) scores in all WOMAC dimensions. The variables retained in each of the models explain between 18.5% and 36.9% (R2 adjusted) of the variability in each of the WOMAC dimensions (Table 2). Thirty-seven percent of the variability in the WOMAC pain dimension was explained by the infrapatellar index, IOD, and the number of complications after discharge. Likewise, 31% of the variability in the WOMAC function dimension was explained by the number of comorbidities, the infrapatellar index, and the number of complications.
Discussion
Given the increasing number of patients who are severe and morbidly obese who are undergoing TKA, we tried to identify some of the factors that could lead to worse outcomes in these patients using HRQL as a surrogate outcome measure to evaluate the success of surgery from the patient’s perspective. In a related case control study we found BMI was not associated with worse WOMAC total scores 12 months after TKA, although the effect size was lower in the study group (1.9 versus 2.2 in the WOMAC pain and function dimensions). Patients in the study group also had more intraoperative difficulties and more severe postoperative complications. Complications after discharge were associated with worse WOMAC total scores (B 26.09 in the study group and B 13.80 in the control group). Therefore, we asked which patient characteristics and surgical factors influenced the health status 12 months after TKA, to identify patients who might benefit from preoperative measures designed to improve outcomes.
We acknowledge limitations in our study. First, our data arise from one tertiary reference center and the findings may reflect only this particular group of patients and may not be generalizable to other areas or countries. Second, although the low proportion of male subjects included meant that gender differences could not be interpreted, this is typical of this kind of study and type of patient and we believe it did not affect the results [18]. Third, we did not study the influence of each comorbidity separately. Finally, we did not measure other factors such as range of movement at 12 months or the effect of possible component malposition. As our aim was to report the patient’s perspective of their TKA, we do not believe these factors would have changed our observations. In addition, in previous studies [8, 10, 20] of patients who were obese we found that malpositioning was not a problem, as we used a tibial endomedullary or extramedullary guide in the frontal and sagittal planes that ensures correct alignment in both planes using either type of guide.
We found comorbidities and lower limb anthropometric features were independently associated with worse postoperative WOMAC scores at 12 months. Other studies have reported an independent negative effect of comorbidities on function [7, 15, 23], suggesting that treatment and active control should be considered. Patients with severe and morbid obesity reportedly have more associated comorbidities and longitudinal studies provide evidence of a relationship between comorbidity and functional limitations [2, 20, 21]. Jones et al. reported comorbidity was associated with poorer short-term functional results in patients undergoing TKA [13]. Fisher et al. evaluated the influence of patient-specific factors on TKA outcomes using the Knee Society Score and found that diabetes mellitus, respiratory disease, and depression (among the most frequent comorbidities in our patients) were associated with poor results after TKA [7].
In a previous study [17], we found that although a suprapatellar index less than 1.6 predicts more difficult surgery, an infrapatellar index less than 1.75 predicts worse WOMAC functional and pain domain scores at 12 months, and an infrapatellar index percentile less than 75 indicated a knee with more difficulties in prosthesis implantation, regardless of the BMI, although patients with a BMI greater than 35 had greater surgical difficulties. Therefore we chose to use the infrapatellar index [17] in the current study. We found that an infrapatellar index less than 75% was associated with worse pain and function.
The degree of IOD and complications after discharge negatively influenced WOMAC dimension scores. Greater IOD (Grade 2) was associated with more pain at 12 months. Several studies suggest obesity complicates the technical aspects of surgery [10, 17, 27]. Patients who are severe or morbidly obese who are undergoing TKA have more IOD, leading to poorer results [8, 20, 25, 32]. This suggests that our IOD index, which we have used in previous studies [22, 23], may be useful in estimating the short-term influence of intraoperative difficulties on TKA outcomes, and may be considered an indirect instrument for quality control of the surgical procedure. We currently are validating this index in various patient groups with the objective of standardizing methods.
We found the percentages of major complications after TKA were similar to the numbers reported in other studies [10, 20, 25, 32]. Patients who are obese who are undergoing TKA have more postoperative complications and worse results, including worse functional scores. Gillespie and Porteous found that heavier patients are at greater risk of having complications and there is a well-established increased risk of complications [10]. However, other studies have had contrasting results [11, 12, 30], with a low frequency of complications in patients who are obese. Additionally, reports emphasize that, as in our study, complications are defined by each study, and the exact nature of the complication often cannot be determined adequately, making comparisons difficult [15, 28]. As suggested in previous studies, homogenous criteria should be developed to measure TKA outcomes and make more accurate comparisons between series possible [27, 28].
In practical terms, our observations suggest that, in addition to the BMI, the anthropometric index of the knee can help identify patients requiring a different surgical approach designed to minimize complications. This might include the use of special prosthetic models with supplementary tibial components to avoid early loosening, more surgical staff during the operation, tapered (conical) lower leg tourniquets, and additional supports in the surgical table to support the patient’s weight and to fasten the knee. We believe the surgical technique should ensure accurate placement of the implant using a tibial endomedullary guide, and correct equilibrium of extensor mechanism of the knee to achieve good patellar tracking and thereby prevent postoperative anterior knee pain. Likewise, evaluation of comorbidities can identify patients requiring greater preoperative control to reduce surgical risks. Finally, informed consent for surgery should include information regarding the possible difficulties that surgery may entail for a patient who is obese.
Acknowledgments
We thank F. Segura, G. Navarro, and D. Buss for help and advice.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at: Hospital Clínic, Barcelona (Spain)
References
- 1.Bellamy N. WOMAC: a 20-year experimental review of a patient-centered self-reported health status questionnaire. J Rheumatol. 2002;29:2473–2476. [PubMed] [Google Scholar]
- 2.Deshmukh RG, Hayes JH, Pinder IM. Does body weight influence outcome after total knee arthroplasty? A 1-year analysis. J Arthroplasty. 2002;17:315–319. doi: 10.1054/arth.2002.30776. [DOI] [PubMed] [Google Scholar]
- 3.Escobar A, Quintana JM, Bilbao A, Azkarate J, Guenaga JI. Validation of the Spanish version of the WOMAC questionnaire for patients with hip or knee osteoarthritis: Western Ontario and McMaster Universities Osteoarthritis Index. Clin Rheumatol. 2002;21:466–471. doi: 10.1007/s100670200117. [DOI] [PubMed] [Google Scholar]
- 4.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Ethgen O, Vanparijs P, Delhalle S, Rosant S, Bruyere O, Reginster JY. Social support and health-related quality of life in hip and knee osteoarthritis. Qual Life Res. 2004;13:321–330. doi: 10.1023/B:QURE.0000018492.40262.d1. [DOI] [PubMed] [Google Scholar]
- 6.Fehring TK, Odum SM, Griffin WL, Mason JB, McCoy TH. The obesity epidemic: its effect on total joint arthroplasty. J Arthroplasty. 2007;22(6 suppl 2):71–76. [DOI] [PubMed]
- 7.Fisher DA, Dierckman B, Watts MR, Davis K. Looks good but feels bad: factors that contribute to poor results after total knee arthroplasty. J Arthroplasty. 2007;22(6 suppl 2):39–42. [DOI] [PubMed]
- 8.Foran JR, Mont MA, Rajadhyaksha AD, Jones LC, Etienne G, Hungerford DS. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty. 2004;19:817–824. doi: 10.1016/j.arth.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466:2597–2604. doi: 10.1007/s11999-008-0428-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gillespie GN, Porteous AJ. Obesity and knee arthroplasty. Knee. 2007;14:81–86. doi: 10.1016/j.knee.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Griffin FM, Scuderi GR, Insall JN, Colizza W. Total knee arthroplasty in patients who were obese with 10 years followup. Clin Orthop Relat Res. 1998;356:28–33. doi: 10.1097/00003086-199811000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D. Health-related quality of life after knee replacement. J Bone Joint Surg Am. 1998;80:163–173. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Jones CA, Beaupre LA, Johnston DW, Suarez-Almazor ME. Total joint arthroplasties: current concepts of patient outcomes after surgery. Rheum Dis Clin North Am. 2007;33:71–86. doi: 10.1016/j.rdc.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 14.Jones DL, Westby MD, Greidanus N, Johanson NA, Krebs DE, Robbins L, Rooks DS, Brander V. Update on hip and knee arthroplasty: current state of evidence. Arthritis Rheum. 2005;53:772–780. doi: 10.1002/art.21465. [DOI] [PubMed] [Google Scholar]
- 15.Kane RL, Saleh KJ, Bershadsky B, Cross WW 3rd, MacDonald RM, Rutks I. Total knee replacement. Evidence Report/Technology Assessment No. 86 (Prepared by Minnesota Evidence-based Practice Center, Minneapolis, Minnesota). AHRQ Publication No. 04-E006-1. Rockville, MD: Agency for Healthcare Research and Quality. November 2003. Available at: http://www.ahrq.gov/clinic/epcsums/kneesum.pdf. Accessed December 2003.
- 16.Kellgren JH, Lawrence JS. Atlas of Standard Radiographs: The Epidemiology of Chronic Rheumatism. Oxford, England: Blackwell Scientific Publications; 1996. [Google Scholar]
- 17.Lozano LM, Nunez M, Segur JM, Macule F, Sastre S, Nunez E, Suso S. Relationship between knee anthropometry and surgical time in total knee arthroplasty in severely and morbidly obese patients: a new prognostic index of surgical difficulty. Obes Surg. 2008;18:1149–1153. doi: 10.1007/s11695-008-9481-3. [DOI] [PubMed] [Google Scholar]
- 18.Lozano LM, Segur JM, Macule F, Nunez M, Torner P, Castillo F, Suso S. Intramedullary versus extramedullary tibial cutting guide in severely obese patients undergoing total knee replacement: a randomized study of 70 patients with body mass index > 35 kg/m2. Obes Surg. 2008;18:1599–1604. doi: 10.1007/s11695-008-9564-1. [DOI] [PubMed] [Google Scholar]
- 19.Mason JB. The new demands by patients in the modern era of total joint arthroplasty: a point of view. Clin Orthop Relat Res. 2008;466:146–152. doi: 10.1007/s11999-007-0009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miric A, Lim M, Kahn B, Rozenthal T, Bombick D, Sculco TP. Perioperative morbidity following total knee arthroplasty among obese patients. J Knee Surg. 2002;15:77–83. [PubMed] [Google Scholar]
- 21.Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20(7 suppl 3):46–50. [DOI] [PubMed]
- 22.Nunez M, Lozano L, Nunez E, Segur JM, Sastre S, Macule F, Ortega R, Suso S. Total knee replacement and health-related quality of life: factors influencing long-term outcomes. Arthritis Rheum. 2009;61:1062–1069. doi: 10.1002/art.24644. [DOI] [PubMed] [Google Scholar]
- 23.Nunez M, Nunez E, del Val JL, Ortega R, Segur JM, Hernandez MV, Lozano L, Sastre S, Macule F. Health-related quality of life in patients with osteoarthritis after total knee replacement: factors influencing outcomes at 36 months of follow-up. Osteoarthritis Cartilage. 2007;15:1001–1007. doi: 10.1016/j.joca.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 24.Nunez M, Nunez E, Segur JM, Macule F, Quinto L, Hernandez MV, Vilalta C. The effect of an educational program to improve health-related quality of life in patients with osteoarthritis on waiting list for total knee replacement: a randomized study. Osteoarthritis Cartilage. 2006;14:279–285. doi: 10.1016/j.joca.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 25.Peersman G, Laskin R, Davis J. Peterson M: Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res. 2001;392:15–23. doi: 10.1097/00003086-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Pla de Salut de Catalunya 2002–2005. Generalitat de Catalunya Departament de Salut. Available at: http://www.gencat.net/salut/depsan/units/sanitat/html/ca/plasalut/index.html. Accessed January 2002.
- 27.Rajgopal V, Bourne RB, Chesworth BM, MacDonald SJ, McCalden RW, Rorabeck CH. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008;23:795–800. doi: 10.1016/j.arth.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 28.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG: Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51:428–436. [PMC free article] [PubMed]
- 29.Singh J, Sloan JA, Johanson NA. Challenges with health-related quality of life assessment in arthroplasty patients: problems and solutions. J Am Acad Orthop Surg. 2010;18:72–82. [PMC free article] [PubMed] [Google Scholar]
- 30.Spicer DD, Schaper LA, Pomeroy DL, Badenhausen WE, Jr, Curry JI, Suthers KE, Smith MW. Cementless cup fixation in total hip arthroplasty after 5–8 years. Int Orthop. 2001;25:286–289. doi: 10.1007/s002640100265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whiteside LA, Nakamura T. Effect of femoral component design on unresurfaced patellas in knee arthroplasty. Clin Orthop Relat Res. 2003;410:189–198. doi: 10.1097/01.blo.0000063605.67412.4d. [DOI] [PubMed] [Google Scholar]
- 32.Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am. 1998;80:1770–1774. doi: 10.2106/00004623-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation.WHO Technical Report Series. No. 894. Geneva, Switzerland: World Health Organization; 2000. [PubMed]