Abstract
Background
Appraisal of the orientation of implants in THA dislocations currently is based on imaging done with the patient in the supine position. However, dislocation occurs in standing or sitting positions. Whether measured anteversion differs in images projected in the position of dislocation is unclear.
Questions/purposes
We compared measured acetabular cup orientations on axial CT scans taken with the patient in a supine position with those from CT sections at angles to the sacral slope reflecting standing and sitting positions.
Methods
We retrospectively reviewed the radiographs of 328 asymptomatic patients who had THAs. Anatomic acetabular anteversion (AAA) was measured from the plain CT scan (supine position, axial CT sections). The AAA also was measured on reformatted CT scans in which the orientation was adjusted individually to the sacral slope on lateral radiographs with patients in the standing and sitting positions.
Results
The mean/(SD) AAA changed from 24.2° (6.9°) in the supine position to 31.7° (5.6°) and 38.8° (5.4°) in simulated standing and sitting positions, respectively. The supine AAA correlated with the standing AAA (r = 0.857) but not with the sitting AAA (r = 0.484).
Conclusions
These data suggest measurement of the AAA on a plain CT scan used in current practice is biased. In patients with recurrent posterior dislocation from a sitting position, accounting for the functional variations in measurement of the position of the acetabular cup provides more relevant information regarding component positioning.
Introduction
Hip dislocation is a frequent mode of failure of THA with 0.5% to 10% dislocation rates reported for primary THA [3] and 10% to 25% after revision surgery [1]. The dislocation risk is multifactorial. In addition to infection, wear, issues with the quality of the surrounding soft tissue, and the type of prosthesis, the position of the implants plays a major role in the mechanical stability of a THA [5, 7, 10, 16, 19, 23, 25, 29, 30, 33]. The CT scan is the current gold standard for assessing the position of the implants in case of dislocation. Reference values with the common protocol have been reported for native hips [2, 15, 35, 37] and those with THAs [9, 20, 32, 36, 39].
However, the CT scan is done with the patient in the supine position, whereas the sitting position is where most posterior dislocations occur [12, 34]. Therefore, knowing the acetabular version in that position might be important, and measuring cup version of the patient in the supine position on a CT scan for hip dislocation, as most clinicians do, could result in misleading information as apparent acetabular anteversion increases 1° for every 2°-increase of pelvic tilt [18, 23, 25, 38].
Using an earlier protocol to adjust the plane of the CT scan to the subject’s sacral slope in standing and sitting positions, the AAA was obtained in simulated standing and sitting positions [22]. The measured value substantially changed from one position to the other with changes in lumbar spine lordosis and pelvic tilt.
We therefore compared measured acetabular cup orientations on axial CT scans taken with the patient in a supine position with those on CT sections at angles to the sacral slope reflecting standing and sitting positions.
Materials and Methods
We retrospectively reviewed the images of 328 selected asymptomatic patients who had undergone THAs. All patients had noncemented THAs with metal-backed acetabular implants and followups of 1 to 11 years (average, 4.3 years). Forty-eight percent were men and 52% were women. Their ages ranged from 60 to 79 years (average, 70.4 years). All patients had AP and lateral radiographs of the pelvis in the standing and sitting positions and a conventional low-dose CT scan of the pelvis in a supine position. Patients were checked for the absence of lower limb length differences and lumbosacral junction abnormalities (fusion, malformation, severe disc degeneration with substantial osteophytes, and disc space narrowing).
All measurements were made by two independent observers (JYL, MG). The abduction angle (AA) was measured on the AP view. On the lateral view, the sacral slope (SS) and acetabular sagittal inclination (ASI) were measured. The SS angle is formed by the tangent line to the upper end plate of S1 and the horizontal plane [24]. As a result of basic trigonometric relationships in three dimensions, the ASI has the same value as the operative anteversion, described by Murray [26], while being a different angle. The SS, AA, and ASI were measured with patients in the standing, sitting, and supine positions (Fig. 1). The standard radiographs were used for standing and sitting positions and CT topograms were used for the supine position.
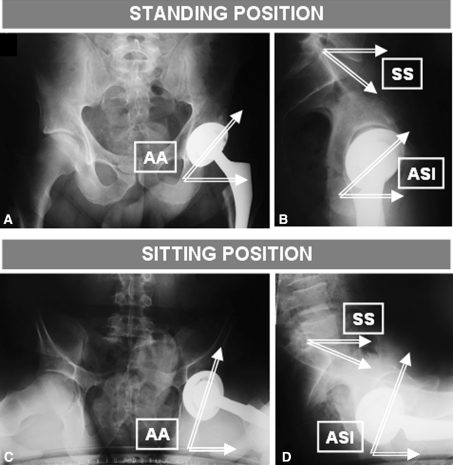
Fig. 1A–D.
(A) AP and (B) lateral radiographs of a patient in a standing position, and (C) AP and (D) lateral radiographs of the same patient in the sitting position are shown. Measurement of the abduction angle (AA) on the AP radiograph and the acetabular sagittal inclination (ASI) and sacral slope (SS) is shown. Variations in orientation of the acetabular cup in the standing versus the sitting position can be seen.
In addition, the pelvic incidence (inclination) was measured on the lateral radiographs. The pelvic incidence is the angle between the line perpendicular to the S1 end plate and the line connecting the middle of the sacral plateau to the center of the femoral head. This parameter is related to the size of the pelvis in the sagittal plane and the offset between the lumbosacral junction and the hips [6]. As a morphometric parameter of bony structure, the pelvic incidence does not vary with the position of the pelvis (Fig. 2). The average radiation dose for the AP and lateral radiographs was 3 mGy and 4.6 mGy, respectively.
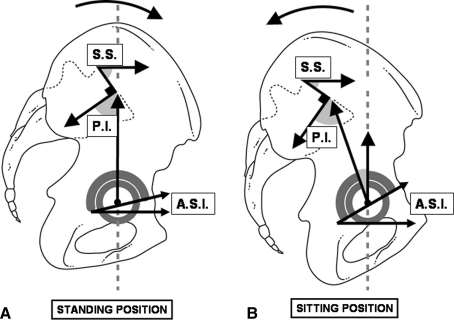
Fig. 2A–B.
Lateral schematics of the pelvis in (A) standing and (B) sitting positions show variations of the sacral slope (SS) and the acetabular orientation. The SS increases in the standing position, whereas the acetabular sagittal inclination (ASI) angle decreases. The SS decreases in the sitting position and the ASI angle increases. The pelvic incidence (PI) represents the offset between the lumbosacral junction and the hips. The PI is a constant anatomic parameter. It does not vary whatever the pelvic tilt is.
From the CT scan sections, the AAA was measured according to the usual routine protocol, with the patient in a supine position on the axial section, similar to the protocol described by Stem et al. [35] (Fig. 3A). Measurement of the AAA corresponding to standing and sitting positions required an adjustment of the sectional plane following the value of the SS on lateral radiographs with the patients in standing (Fig. 3C) and sitting positions [23] (Fig. 3C). Because the SS is a major parameter for assessing the position of the pelvis in the sagittal plane [31], the SS was used as a reference for the functional position of the pelvis. The radiation dose for the CT scan of the pelvis was 500 mGy · cm, which corresponds to 9.5 mSv using the conversion ratio from Hidajat et al. [13]. The standing AAA measured two times by the two observers showed a paired intraobserver difference of 2.53°. The intraobserver intraclass correlation coefficient (ICC) was 0.951. The paired interobserver difference was 3.25°. The interobserver ICC was 0.916.
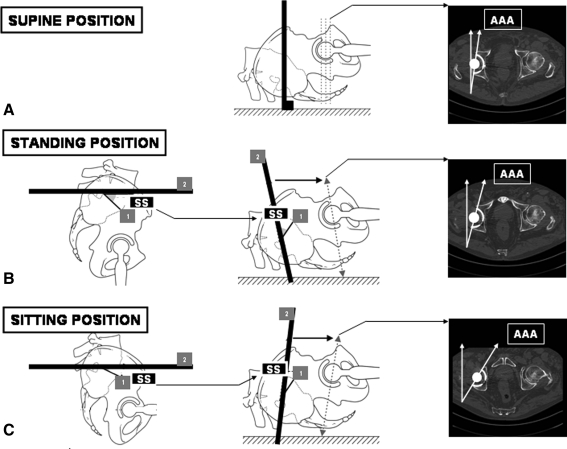
Fig. 3A–C.
(A) The standard CT scan protocol is performed with the patient in a supine position. It provides routine measurement of acetabular anteversion (AAA). (B) The proposed CT scan protocol includes an adjustment to the sacral slope, which replicates the standing position. First, the sacral slope (SS) is measured on the lateral radiograph in a standing position. Second, the sacral slope is transferred to the CT scan scout view (1 = sacral end plate; 2 = horizontal plane in a standing position). (C) Adjustment to the SS when measured on a lateral radiograph in a sitting position is shown. Changes of the measured AAA according to the plane of section can be seen.
The statistical analysis began with a study of the reproducibility and repeatability of measurement of the AAA of the cup of a THA on a CT scan because repeatability data of such measurement were not reported before. We then performed a descriptive analysis of the measured variables (mean ± SD). Normality of the variables was checked using the Shapiro-Wilk test. Paired t-tests were used to investigate differences among standing, sitting, and supine positions for each normally distributed variable. Using the Spearman correlation test, the relationships among the supine, sitting, and standing positions regarding the AAA, AA, and ASI were investigated. Finally, a linear regression analysis aimed at identifying the relevant parameters that influence the gain in AAA from the standing to the sitting position were identified among the pelvic incidence, the standing AAA, AA, ASI, and SS, and the variation. The SPSS 11.5 software package (SPSS Inc, Chicago, IL, USA) was used for the calculations with the significance level of p < 0.05 of the SS between the standing and sitting positions.
Results
The average (SD) pelvic incidence was 53.7° (13.6°); this anatomic parameter does not vary with the position of the pelvis. The SS decreased from the supine to the standing and the sitting positions. The frontal and sagittal inclinations and the anatomic anteversion increased from the supine to the standing and the sitting positions (Table 1).
Table 1.
Measured parameters*
| Parameter | Supine | Standing | Sitting | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| SS | 45.6 | 9.8 | 35.0 | 10.7 | 20.5 | 11.5 |
| AA | 46.3 | 3.6 | 49.4 | 4.0 | 56.7 | 7.1 |
| ASI | 25.5 | 8.4 | 36.0 | 8.2 | 50.6 | 11.2 |
| AAA | 24.2 | 6.9 | 31.7 | 5.6 | 38.8 | 5.4 |
* Variations between positions are statistically significant; SS = sacral slope; AA = acetabular frontal inclination; ASI = acetabular sagittal inclination; AAA = anatomic acetabular anteversion.
Measurement of anatomic anteversion with the CT scan correlated in the standing and supine positions but not between the sitting position and any other positions (Table 2). Similarly, the AA (Table 3) and the ASI (Table 4) correlated in the standing position and the supine position, but not in the sitting and or any other positions. The regression analysis showed a correlation coefficient of r = 0.943 and a coefficient of determination r2 = 0.889. The regression equation was:
 |
Table 2.
Spearman’s correlation matrix between CT images for AAA*
| AAA | Supine | Standing | Sitting | |||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| Supine | 1 | – | 0.857 | < 0.001 | 0.484 | < 0.001 |
| Standing | 1 | – | 0.551 | < 0.001 | ||
| Sitting | 1 | – | ||||
* There is a strong correlation between images in the supine and standing positions; AAA = anatomic acetabular anteversion.
Table 3.
Spearman’s correlation matrix between AP radiographs for AA*
| AA | Supine | Standing | Sitting | |||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| Supine | 1 | – | 0.864 | < 0.001 | 0.378 | < 0.001 |
| Standing | 1 | – | 0.403 | < 0.001 | ||
| Sitting | 1 | – | ||||
* There is a strong correlation between images of the supine and standing positions; AA = abduction angle.
Table 4.
Spearman’s correlation matrix between lateral radiographs for ASI*
| ASI | Supine | Standing | Sitting | |||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| Supine | 1 | – | 0.828 | < 0.001 | 0.374 | < 0.001 |
| Standing | 1 | – | 0.369 | < 0.001 | ||
| Sitting | 1 | – | ||||
* There is a strong correlation between images in the supine and standing positions; ASI = acetabular sagittal inclination.
Only the first three factors of the equation had significant p values. Their standardized coefficients were −0.786, −0.273, and − 0.151, respectively, showing that the gain in AAA from the standing to the sitting position was mostly the result of mobility in the lumbosacral junction.
Discussion
Because posterior dislocations of the hip mostly occur in the sitting position, and some anterior dislocations in the standing position, the rationale of our study was to investigate a novel protocol for measuring AAA on the CT scan with simulating the sitting and standing positions. We therefore compared measured acetabular cup orientations on axial CT scans taken with the patient in a supine position from those on CT sections at angles to the sacral slope reflecting standing and sitting positions.
We acknowledge limitations to our study. First, we studied no patients with dislocations and therefore did not directly assess the importance of the proposed SS-adjusted CT protocol on the diagnosis and understanding of the mechanical dysfunction of unstable THAs. The normal ranges of the AAA, the AA, and the ASI, and the reproducibility of measurement of anatomic anteversion on the CT scan are presented in a large asymptomatic population, but it would be necessary to compare numerous dislocation cases with our data to define a predictive safety zone using the sacral slope-adjusted CT protocol. The safety limits for AAA would be the maximal value of the AAA above which there is a substantial risk of anterior dislocations and the minimum value of the AAA below which there is an increased risk of posterior dislocation. For now, the practical implication of the SS-adjusted CT scan protocol is limited to improving the examination of dislocations. Second, CT scans have substantial cost and radiation dose. However, the proposed protocol is based on only two additional lateral radiographs, which represent a little extra cost and radiation source, that substantially improve the results of the CT scans that already are widely performed in current practice for examining dislocations [17, 28]. It is likely that, in the future, the EOS® imaging system (EOS Imaging SA, Paris, France) could directly and accurately provide the three-dimensional orientation of the acetabulum in various postures with more efficiency and less radiation dose [8].
We confirmed that the AAA, frontal inclination, and sagittal inclination were functional parameters that varied substantially among the standing, sitting, and supine positions. We observed that the acetabular parameters in a supine position highly correlated with those in a standing position but poorly correlated with those in a sitting position. The amount of mobility in the lumbosacral junction accounted most for the variation in the AAA between the standing and sitting positions. The notion of a relationship between AAA and the position of the pelvis was suggested by Anda et al. [2] and Zilber et al. [40] in native hips (Table 5). Variations in the acetabular cup position after THA implantation as a function of the patient’s position were reported previously [22, 23]. The current study confirmed and numerically showed the functional relationship between the SS and the AAA: the SS increases while the AAA decreases from the sitting to standing positions and reciprocally the SS decreases and the AAA increases from the standing to sitting positions.
Table 5.
Studies of CT assessment of the AAA according to the position
| Study | THA or native hip | Conventional CT in supine position | CT in simulated standing position | CT in simulated sitting position |
|---|---|---|---|---|
| Current study | THA | 24.2° (SD 6.9°) | 31.7° (SD 5.6°) | 38.8° (SD 5.4°) |
| Lazennec et al. [23] | THA | 11.1° (SD 3.2°) | 13° (SD 2.4°) | 30.2° (SD 5.7°) |
| Swanson [36] | THA | 14.6° (SD NA) | NA | NA |
| Ryan et al. [32] | THA | 32° (SD 6.8°) | NA | NA |
| Kim [20] | THA | 26.9° (SD 4°) | NA | NA |
| Duwelius et al. [9] | THA | 18.4° (SD 7.9°) | NA | NA |
| Williams et al. [39] | THA | 15.5° (SD 5.5°) | NA | NA |
| Zilber et al. [40] | Native hip | 11° (SD 11°) | 26° (SD 7.2°) | 36° (SD 6.3°) |
| Tallroth and Lepisto [37] | Native hip (dysplasia) | 21° (SD 7°) | NA | NA |
| Stem et al. [35] | Native hips | 23° (SD 5°) | NA | NA |
AAA = anatomic acetabular anteversion; NA = not available.
We found a poor correlation between the supine and sitting AAA. This suggests that the usual CT scan protocol is biased and not fully appropriate for examination of a posterior THA dislocation, which occurs in hip flexion. On the contrary, the strong correlation observed between the supine and standing measurements, which were observed in all the acetabular parameters (AAA, AA, and ASI), suggests that the classic CT assessment of the AAA is still a relevant source of information in cases of anterior THA dislocation and subluxation. Few articles address this issue in the literature. One notices only that the correlation between the supine and standing positions is in agreement with the results presented by Nishihara et al., who reported less than 10° variation in orientation of the pelvis from a standing to a supine position in 90% of cases [27].
Lumbosacral junction mobility was the main parameter influencing the variations of AAA between the standing and sitting positions. The fact that the risk of dislocation increases cumulatively with time [4] and the fact that degenerative phenomena in the aging spine that induce progressive changes in sagittal balance with loss of lumbar lordosis and pelvic extension [11, 14, 31] support the idea of the major role of the function of the lumbosacral junction on function of the hip. In everyday practice, stiffness in the lumbar spine (eg, L5-S1 arthrodesis) is a risk factor for THA subluxation and dislocation resulting from the lack of variation in the AAA from a standing to a sitting position. To the best of our knowledge, this question has not been evaluated in the literature. This is not yet well defined, but our study suggests that taking spinal flexibility into account is important when planning a THA implantation or at least identifying outlier patients who have an abnormal pelvic (ie, acetabular) posture. Dual mobility cups could be specifically indicated for those patients [21].
The classic measurement of AAA on CT scans uniquely taken with patients in the supine position seems insufficient to determine the actual position of the acetabular cup from a functional standpoint. In our opinion, the plain measurement is biased specifically in the case of posterior dislocation, because the supine AAA is poorly correlated with the adjusted AAA of the sitting position of dislocation. Therefore, when a CT scan is indicated for patients undergoing THA with problems of recurrent THA dislocation who need revision arthroplasty, we recommend adjusting the CT sectional plane to the SS that corresponds to the position of interest. This protocol would be more standardized and more efficient for measuring orientation of the acetabular cup than the plain CT scan with the patient in a supine position with a random position of the pelvis on the machine. Based on our observations, we suspect mobility of the lumbosacral junction plays a crucial role in the mechanical function and stability of a THA. Therefore, we also recommend doing dynamic lateral radiographs of the lumbosacral junction in the standing and sitting positions for primary THA in patients who have some abnormal features in their lumbosacral spine, for example, in the elderly population [31].
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery, La Pitié–Salpétrière Hospital, Assistance Publique–Hopitaux de Paris, Paris, France.
References
- 1.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84:1788–1792. [PubMed] [Google Scholar]
- 2.Anda S, Terjesen T, Kvistad KA. Computed tomography measurements of the acetabulum in adult dysplastic hips: which level is appropriate? Skeletal Radiol. 1991;20:267–271. doi: 10.1007/BF02341662. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Berry DJ, Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 5.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 6.Boulay C, Tardieu C, Hecquet J, Benaim C, Mitulescu A, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J. Anatomical reliability of two fundamental radiological and clinical pelvic parameters: incidence and thickness. Eur J Orthop Surg. 2005;17:197–204. doi: 10.1007/s00590-005-0239-5. [DOI] [Google Scholar]
- 7.Chen E, Goertz W, Lill CA. Implant position calculation for acetabular cup placement considering pelvic lateral tilt and inclination. Comput Aided Surg. 2006;11:309–316. doi: 10.1080/10929080601090516. [DOI] [PubMed] [Google Scholar]
- 8.Dubousset J, Charpak G, Skalli W, Kalifa G, Lazennec JY. EOS stereo-radiography system: whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose [in French] Rev Chir Orthop Reparatrice Appar Mot. 2007;93(6 suppl):141–143. doi: 10.1016/s0035-1040(07)92729-4. [DOI] [PubMed] [Google Scholar]
- 9.Duwelius PJ, Burkhart RL, Hayhurst JO, Moller H, Butler JB. Comparison of the 2-incision and mini-incision posterior total hip arthroplasty technique: a retrospective match-pair controlled study. J Arthroplasty. 2007;22:48–56. doi: 10.1016/j.arth.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 10.Eddine TA, Migaud H, Chantelot C, Cotten A, Fontaine C, Duquennoy A. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for CT measurement of position of a prosthetic cup. Surg Radiol Anat. 2001;23:105–110. doi: 10.1007/s00276-001-0105-z. [DOI] [PubMed] [Google Scholar]
- 11.Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976). 1995;20:1351–1358. [PubMed] [Google Scholar]
- 12.Hamilton WG, McAuley JP. Evaluation of the unstable total hip arthroplasty. Instr Course Lect. 2004;53:87–92. [PubMed] [Google Scholar]
- 13.Hidajat N, Maurer J, Schroder RJ, Nunnemann A, Wolf M, Pauli K, Felix R. Relationships between physical dose quantities and patient dose in CT. Br J Radiol. 1999;72:556–561. doi: 10.1259/bjr.72.858.10560337. [DOI] [PubMed] [Google Scholar]
- 14.Itoi E. Roentgenographic analysis of posture in spinal osteoporotics. Spine (Phila Pa 1976). 1991;16:750–756. doi: 10.1097/00007632-199107000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Jacobsen S, Romer L, Soballe K. Degeneration in dysplastic hips: a computer tomography study. Skeletal Radiol. 2005;34:778–784. doi: 10.1007/s00256-005-0019-7. [DOI] [PubMed] [Google Scholar]
- 16.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 17.Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup: accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58:294–300. doi: 10.1016/j.ejrad.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Kalteis TA, Handel M, Herbst B, Grifka J, Renkawitz T. In vitro investigation of the influence of pelvic tilt on acetabular cup alignment. J Arthroplasty. 2009;24:152–157. doi: 10.1016/j.arth.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 20.Kim YH. Comparison of primary total hip arthroplasties performed with a minimally invasive technique or a standard technique: a prospective and randomized study. J Arthroplasty. 2006;21:1092–1098. doi: 10.1016/j.arth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Langlais FL, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop Relat Res. 2008;466:389–395. doi: 10.1007/s11999-007-0047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lazennec JY, Riwan A, Gravez F, Rousseau MA, Mora N, Gorin M, Lasne A, Catonne Y, Saillant G. Hip spine relationships: application to total hip arthroplasty. Hip Int. 2007;17(suppl 5):S91–S104. [PubMed] [Google Scholar]
- 23.Lazennec JY, Charlot N, Gorin M, Roger B, Arafati N, Bissery A, Saillant G. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat. 2004;26:136–144. doi: 10.1007/s00276-003-0195-x. [DOI] [PubMed] [Google Scholar]
- 24.Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 26.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 27.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140–151. doi: 10.1097/01.blo.0000069891.31220.fd. [DOI] [PubMed] [Google Scholar]
- 28.Nishii T, Sugano N, Miki H, Koyama T, Takao M, Yoshikawa H. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of total hip arthroplasty. J Arthroplasty. 2004;19:162–166. doi: 10.1016/j.arth.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 30.Pierchon F, Pasquier G, Cotten A, Fontaine C, Clarisse J, Duquennoy A. Causes of dislocation of total hip arthroplasty: CT study of component alignment. J Bone Joint Surg Br. 1994;76:45–48. [PubMed] [Google Scholar]
- 31.Rousseau MA, Lazennec JY, Boyer P, Mora N, Gorin M, Catonné Y. Optimization of total hip arthroplasty implantation: is the anterior pelvic plane concept valid? J Arthroplasty. 2009;24:22–26. doi: 10.1016/j.arth.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 32.Ryan JA, Jamali AA, Bargar WL. Accuracy of computer navigation for acetabular component placement in THA. Clin Orthop Relat Res. 2010;468:169–177. doi: 10.1007/s11999-009-1003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seki M, Yuasa N, Ohkuni K. Analysis of optimal range of socket orientations in total hip arthroplasty with use of computer-aided design simulation. J Orthop Res. 1998;16:513–517. doi: 10.1002/jor.1100160418. [DOI] [PubMed] [Google Scholar]
- 34.Sierra RJ, Raposo JM, Trousdale RT, Cabanela ME. Dislocation of primary THA done through a posterolateral approach in the elderly. Clin Orthop Relat Res. 2005;441:262–267. doi: 10.1097/01.blo.0000194308.23105.f4. [DOI] [PubMed] [Google Scholar]
- 35.Stem ES, O’Connor MI, Kransdorf MJ, Crook J. Computed tomography analysis of acetabular anteversion and abduction. Skeletal Radiol. 2006;35:385–389. doi: 10.1007/s00256-006-0086-4. [DOI] [PubMed] [Google Scholar]
- 36.Swanson TV. Early results of 1000 consecutive, posterior, single-incision minimally invasive surgery total hip arthroplasties. J Arthroplasty. 2005;20(7 suppl 3):26–32. doi: 10.1016/j.arth.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 37.Tallroth K, Lepisto J. Computed tomography measurement of acetabular dimensions: normal values for correction of dysplasia. Acta Orthop. 2006;77:598–602. doi: 10.1080/17453670610012665. [DOI] [PubMed] [Google Scholar]
- 38.Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467:32–42. doi: 10.1007/s11999-008-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams SL, Bachison C, Michelson JD, Manner PA. Component position in 2-incision minimally invasive total hip arthroplasty compared to standard total hip arthroplasty. J Arthroplasty. 2008;23:197–202. doi: 10.1016/j.arth.2006.12.045. [DOI] [PubMed] [Google Scholar]
- 40.Zilber S, Lazennec JY, Gorin M, Saillant G. Variations of caudal, central, and cranial acetabular anteversion according to the tilt of the pelvis. Surg Radiol Anat. 2004;26:462–465. doi: 10.1007/s00276-004-0254-y. [DOI] [PubMed] [Google Scholar]