Abstract
Background
Using comprehensive gait analysis and strength testing, we previously investigated the early (2-month) functional outcome after THA using two-incision and mini-posterior surgical approaches and found an advantage for the mini-posterior approach. Benefits included improved muscle strength, a less antalgic gait, and better hip function as reflected by changes in hip moments during level walking and stair climbing. We questioned how these differences in function would fare with longer followup.
Questions/purposes
We determined whether the observed early functional advantages for the mini-posterior technique over the two-incision technique were still present 1 year postoperatively.
Patients and Methods
We prospectively enrolled 22 patients with primary degenerative arthritis of the hip; of these, 21 completed gait and strength testing at 2 months, and 19 completed comprehensive gait and strength testing at 1 year (11 two-incision hips, eight mini-posterior hips). The 19 patients included 11 men and eight women with a mean age of 65 years (range, 40–85 years) and a mean (BMI) of 29 (range, 21–39).
Results
At 1 year postoperatively, the patients who had the mini-posterior THA had greater improvement in hip flexion strength and internal rotation strength, greater increase in hip flexor internal moment, and greater increase in single-leg stance time on level ground over the patients who had the two-incision THA.
Conclusions
Compared with the two-incision approach, patients undergoing mini-posterior THA had persistently better function, including hip flexor and internal rotator muscle strength, hip flexor internal moment, and single-leg stance during level walking.
Level of Evidence
Level II, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Using comprehensive gait analysis and strength testing, we previously investigated the early (2-month) functional outcome after THA with a subset of patients from a randomized clinical trial of the two-incision and mini-posterior surgical approaches and found an advantage for the mini-posterior approach [16]. Some surgeons have suggested any early differences in function attributable to a surgical approach would disappear with longer followup [8, 10, 11]. However, these studies did not use comprehensive gait analysis or quantitative strength testing.
In addition, some reports of the two-incision THA technique have been for selected series of patients [6, 7, 11, 20]. Without suitable controls, it is unclear whether the observed recovery in those reports was attributable to the two-incision technique or to some combination of patient selection, patient education, changes in perioperative analgesia protocols, or rapid rehabilitation protocols [12, 25, 26, 28]. Furthermore, there is a growing body of evidence of increased complication rates with the two-incision minimally invasive technique when compared with other methods [1, 31, 35]. This has persisted even beyond the learning curve of the individual surgeon [9, 27].
Proponents of the two-incision minimally invasive approach for THA have claimed the surgical technique can be performed without damaging any muscle or tendon, thereby making the recovery after that procedure dramatically better than after other methods of THA [4–6]. However, to our knowledge, no published reports on objective clinical strength data after minimally invasive THA exist. Further, few studies have been performed to compare gait analysis after THA to objectively assess recovery of function [2, 3, 37]. This prospective randomized study was designed to detect differences in muscle damage through isometric strength testing, differences in antalgic gait through changes in temporospatial parameters of gait, and differences in hip function through changes in hip kinetics during level walking and stair climbing.
We hypothesized any early (2-month) functional difference present between patients who had THAs with the mini-posterior and two-incision minimally invasive techniques no longer would be present at 1-year followup. Therefore, we sought to determine whether the observed changes from baseline that led to objective functional advantages for the mini-posterior technique at 2 months were still present at 1 year postoperatively when compared with baseline measurements, including changes in (1) hip muscle strength, (2) hip internal moments during level walking, and (3) temporospatial parameters of single-leg stance time and walking velocity during level walking and stair climbing.
Patients and Methods
This randomized clinical trial was conducted from November 2004 through January 2006. As part of a larger randomized trial [29], we prospectively enrolled 25 patients with primary degenerative arthritis of the hip in whom THA was planned. All patients gave written consent to participate in the study, and the study was approved by our institutional review board. The explicit inclusion criteria were patients aged 40 to 85 years presenting for THA with a diagnosis of primary degenerative arthritis of the hip. The explicit exclusion criteria were age younger than 40 years or older than 85 years; severe bone deformity about the hip such as Crowe Type III or IV dysplasia; osteomyelitis or prior intraarticular infection of the hip; substantial neurologic or musculoskeletal disorders that would adversely affect gait or early weightbearing after surgery; metastatic cancer; congenital, developmental, or other bone disease that would in the surgeon’s judgment interfere with survival of the THA; retained hardware around the hip; and arthrodesis of the affected hip.
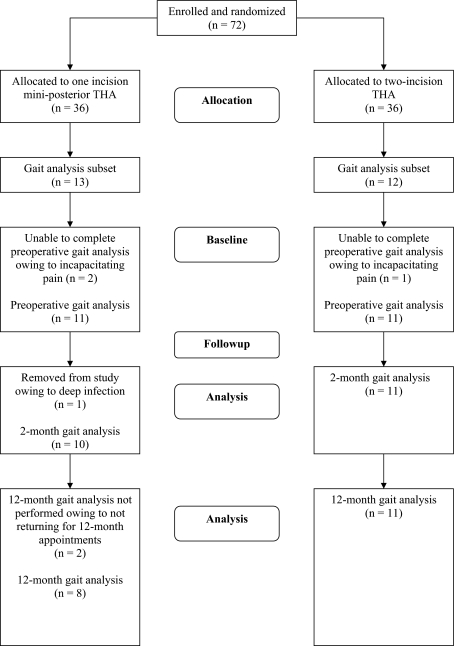
After patient enrollment, the randomization to the two-incision or the mini-posterior THA group was performed via a secure, web-based computerized process developed and implemented by our Department of Biostatistics, which dynamically balanced the groups based on age, gender, and BMI, and ensured similarity in these variables between the two groups. Randomization was done after the surgeon had completed the preoperative examination and discussion with the patient. The surgeon and patient were blinded regarding the group assignment before surgery but not during or after the procedure. On presentation to the gait laboratory preoperatively, three patients were unable to complete the comprehensive gait analysis because of incapacitating pain in the affected hip; at 2 months, one male patient was removed from analysis owing to deep prosthetic infection treated with débridement and retention of components; and at 1 year, two additional patients were unable to complete the gait analysis (Fig. 1). Of these two additional patients, one did not return for 1-year appointments but was doing well at his 2-year followup appointment. The other patient had Guillain-Barré syndrome and was unable to complete the 1-year analysis owing to profound weakness. Therefore, there were 21 patients with complete preoperative and 2-month postoperative gait analyses and strength testing, and 19 patients with complete preoperative and 1-year postoperative gait analyses and strength testing. The 19 patients included 11 men and eight women with a mean (± SD) age of 65 ± 12 years (range, 40–85 years) and a mean BMI of 29 ± 5 (range, 21–39). Eleven patients had the two-incision surgical technique and eight had the mini-posterior technique. There were no differences in age at the time of surgery, gender, or BMI between the two-incision and mini-posterior groups (Table 1). There were no differences in preoperative strength, temporospatial parameters, or hip kinetics between the two groups. Intention-to-treat analysis was followed during the study.
Fig. 1.
The diagram shows the flow of patients through the study.
Table 1.
Demographics of the study groups
| Characteristics | Mini-posterior (n = 8) | Two-incision (n = 11) | p Value |
|---|---|---|---|
| Age at surgery (years) | |||
| Mean (SD) | 64.50 (13.38) | 65.64 (12.11) | 0.84 |
| Median (range) | 65.5 (40, 80) | 66 (48, 85) | |
| Gender (number of patients) | |||
| Female | 4 (44%) | 4 (40%) | > 0.99 |
| Male | 5 (56%) | 6 (60%) | |
| Body mass index | |||
| Mean (SD) | 29.38 (6.52) | 28.45 (3.39) | 0.93 |
| Median (range) | 27.5 (21, 39) | 29 (24, 34) | |
The two-incision THAs were performed using a technique described previously through a 6-cm anterior incision using the Smith-Petersen interval to expose the hip, cut the femoral neck, and prepare and place the socket [4]. A second incision of 3.8 to 5 cm was made in the buttock to ream and broach the femur and place the real femoral component. For the mini-posterior technique, the surgical approach involved a 7- to 9.5-cm incision along the posterior aspect of the femur starting at the tip of the greater trochanter and proceeding distally [30]. The same femoral component design (Versys® Full-coat; Zimmer Inc, Warsaw, IN, USA) and the same acetabular component design (Trilogy® Modular Trabecular Metal; Zimmer Inc) were used in every case. All patients were treated with the same comprehensive multimodal anesthesia and analgesia protocol including peripheral nerve blocks [26]. There were no differences in analgesic medication requirements between the two groups. No patient-controlled analgesia pumps or other parenteral opioid medication were required by any of the patients in this study.
All patients were moved from bed to a chair on the day of surgery and began walking with weightbearing as tolerated the morning after surgery. Two sessions of supervised physical therapy were performed each day the patient remained in the hospital. Patients were discharged from the hospital when they could move in and out of bed with minimal assistance, walk 100 feet using a walker or crutches, get up and down three stairs, and control their pain with oral medication. No attempt was made to perform the surgery on an outpatient basis. Traditional total hip dislocation precautions were not used. The only warning was for the patients who had the mini-posterior approach to avoid the combination of flexion greater than 100° and marked internal rotation of their hip; patients otherwise were encouraged to proceed with activities as tolerated, allowing their hip symptoms to be their guide, discontinue walking aids when they felt comfortable, and wean from pain medications as the pain diminished. They were not instructed to a specific time regarding when these events should occur, and there were no differences in long-term physical therapy between the two groups. The length of stay in the hospital was not different between the two groups, with a mean stay of 2.7 days for each group.
One examiner, blinded to the type of surgical approach, performed all gait and strength testing in the motion analysis laboratory. Blinding was assured by patients being cautioned not to reveal the type or number of incisions for their surgery and none of the markers used in the motion capture were located in the region(s) of the surgical incisions.
Three-dimensional gait data acquired from each patient during level walking, stair ascent, and stair descent preoperatively (1–3 days before surgery) and 8 weeks after surgery have been reported [16]. Data were obtained again 1 year postoperatively. We chose the 1-year end point in this study to evaluate whether any improved functional outcomes would persist a full year after surgery. Three-dimensional gait data were acquired using a 10-camera high-resolution motion capture system (Motion Analysis Corp, Santa Rosa, CA, USA) focused on a volume approximately 4 × 5 × 2 m. Within the volume, AMTI (Advanced Mechanical Technology, Inc, Watertown, MA, USA) and Kistler (Kistler Instrument Corp, Amherst, NY, USA) force platforms were embedded in the floor and a pair of AMTI force platforms were embedded in the third and fourth steps of a flight of seven steps. Data from three trials for each condition were processed and analysis performed including spatiotemporal distance parameters of gait velocity (measured in centimeters per second) and single-leg stance phase duration (measured as percent of gait cycle). Peak hip moments during the stance phase were calculated using OrthoTrak software (Motion Analysis Corp) yielding kinetics reported as internal moments normalized to body weight (Newton meters per kilogram) for hip abduction, adduction, flexion, extension, internal rotation, and external rotation.
Hip strength quantification was performed using a Biodex® machine (Biodex Medical Systems, Shirley, NY, USA). Peak torque (Newton meters) from three trials of isometric hip strength testing was used in the analysis of hip abduction, adduction, flexion, extension, internal rotation, and external rotation. Internal/external hip rotation was performed with subjects sitting with their hips flexed 45º, the dynamometer head aligned with the long axis of the femur, and the resistance arm attached proximal to the malleoli. Hip flexion and extension was performed with the patients supine and the hip flexed 30º with the dynamometer head centered through the femoral head and the resistance arm attached to the distal thigh. Hip abduction and adduction was performed with subjects in a side-lying position with the hip at 0º abduction and flexion, with the dynamometer head centered through the femoral head and the resistance arm attached to the distal thigh.
The current cohort of 19 patients with 1-year data is a subset of the 22 patients for whom the change from baseline to 2 months was reported [16]. For these patients, the primary outcome of interest was the change from baseline to 1 year in strength and gait parameters; a secondary outcome was the percent change from baseline. Evaluating the changes in outcome from baseline minimized any existing preoperative differences between the two groups. Results are reported as median (range), unless otherwise specified. Differences in strength and gait parameters between patients who had the mini-posterior and two-incision approaches were evaluated using the Wilcoxon rank sum tests owing to our small sample size. All statistical tests were one-sided and the alpha level set at 0.05 for statistical significance. All analyses were conducted using SAS® Version 9.1 (SAS Institute Inc., Cary, NC, USA). A post hoc power analysis was performed and outcomes that were found to be significant had adequate statistical power.
Parameters that were found to be significant at 2 months but not at 12 months had low statistical power to detect the observed differences as being significant. Specifically, the statistical powers to detect the observed differences as being significant for hip extension strength, hip flexor moment, hip extensor moment, and hip external rotator moment were 8%, 27%, 45%, and 39%, respectively.
Results
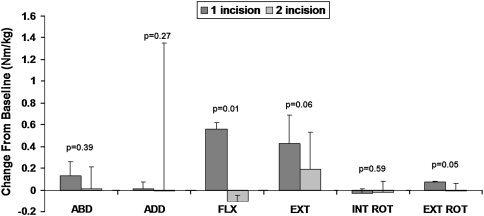
The advantage in hip muscle strength seen 2 months postoperatively for patients who had the mini-posterior THA over the patients who had the two-incision THA was maintained at 1 year postoperatively (Fig. 2). We previously reported, for isometric muscle strength testing at 2 months, the patients who had the mini-posterior approach had greater improvement in hip extension strength and a trend for improvement in hip flexor and hip internal rotation strength than patients who had the two-incision approach [16]. At 1 year postoperatively, the patients who had the mini-posterior approach showed greater improvement in hip flexion strength (p = 0.01) and hip internal rotation strength (p = 0.02) than the patients who had the two-incision approach (Table 2). Several patients who had the two-incision approach had worse hip flexion strength and worse internal rotation strength at 1 year than preoperatively. There were no differences in adduction (p = 0.22) or abduction strength (p = 0.32).
Fig. 2A–C.
(A) A graph shows the change in isokinetic muscle strength from preoperatively to 1-year postoperatively. The patients who had the mini-posterior approach showed greater improvement in hip flexion strength (p = 0.02) and hip internal rotation strength (p = 0.04) than the patients who had the two-incision approach. (B) Continued improvement in isokinetic muscle strength is evident before surgery, and 2 months and 1 year after surgery for the mini-posterior THA group, and (C) at 2 months and 1 year after surgery for the two-incision THA group. ABD = abduction; ADD = adduction; FLX = flexion; EXT = extension; INT ROT = internal rotation; EXT ROT = external rotation.
Table 2.
Changes from baseline to 12 months
| Parameter | Change from baseline to 12 months, median (range) | ||
|---|---|---|---|
| Mini-posterior (n = 8) | Two-incision (n = 11) | p Value (one-sided) | |
| Peak isometric strength measurements (Nm) | |||
| Hip abduction | 19.6 (−21.7 to 28.8) | 18.5 (−71.4 to 30.3) | 0.32 |
| Hip adduction | 46.7 (14.3 to 53.9) | 31.8 (−5.5 to 54.5) | 0.22 |
| Hip flexion | 31.6 (13.4 to 49.3) | 11.2 (−7.3 to 35.3) | 0.01 |
| Hip extension | 36.6 (1.5 to 53.9) | 48.6 (−26.5 to 78.7) | 0.57 |
| Hip internal rotation | 18.0 (2.4 to 39.9) | 5.6 (−13.2 to 31.6) | 0.02 |
| Hip external rotation | −2.0 (−11.8 to 2.0) | 0.90 (−9.7 to 22.2) | 0.82 |
| Peak internal hip moments during stance (Nm/kg) | |||
| Hip abductor | 0.13 (−0.13 to 0.30) | 0.01 (−0.48 to 0.09) | 0.39 |
| Hip adductor | 0.00 (−0.08 to 0.12) | −0.01 (−0.25 to 17.73) | 0.27 |
| Hip flexor | 0.56 (−0.1 to 1.96) | −0.10 (−0.16 to −0.06) | 0.01 |
| Hip extensor | 0.43 (−0.12 to 0.63) | 0.19 (−0.68 to 0.61) | 0.06 |
| Hip internal rotator | −0.03 (−0.06 to 0.07) | −0.02 (−0.22 to 10.06) | 0.59 |
| Hip external rotator | 0.07 (−0.14 to 0.16) | −0.01 (−0.17 to 0.09) | 0.05 |
| Temporospatial parameters of gait | |||
| Single-leg stance time (% of gait cycle) | |||
| Ascending | 5.0 (2.9 to 6.5) | 0.3 (−14.0 to 6.8) | 0.08 |
| Descending | 3.5 (−3.7 to 6.1) | 0.1 (−2.5 to 7.8) | 0.30 |
| Level ground | 5.0 (−1.3 to 9.5) | 2.2 (−0.5 to 6.6) | 0.035 |
| Walking velocity (cm/second) | |||
| Ascending | 10.8 (−8.2 to 13.0) | 7.0 (−1.3 to 26.1) | 0.50 |
| Descending | 8.3 (2.5 to 12.4) | 8.9 (−1.3 to 23.8) | 0.59 |
| Level ground | 30.0 (−3.7 to 62.9) | 23.3 (−2.8 to 55.0) | 0.26 |
Changes in hip internal moments indicated better hip function for the patients who had the mini-posterior approach than for patients who had the two-incision approach at 2 months postoperatively and remained present 1 year postoperatively. We previously reported, at 2 months postoperatively, the patients who had the mini-posterior approach had a greater increase in hip flexor internal moment and a trend for greater increase in hip extensor internal moment and hip external rotator internal moment than the patients who had the two-incision approach [16]. At 1 year, hip function remained better for patients who had the mini-posterior approach than for patients who had the two-incision approach as reflected by greater improvement in hip flexor internal moment (p = 0.01) (Fig. 3).
Fig. 3.
A graph shows greater improvement in hip flexor internal moment for the patients who had the mini-posterior THA (p = 0.02) and trends for improved extensor internal moment (p = 0.12) and improved external rotator internal moment (p = 0.10) on level ground from preoperatively to 1 year postoperatively when compared with the patients who had the two-incision THA. ABD = abduction; ADD = adduction; FLX = flexion; EXT = extension; INT ROT = internal rotation; EXT ROT = external rotation
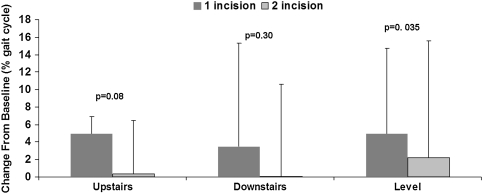
At 2 months postoperatively, there was a greater increase in single-leg stance time on level ground and a trend toward greater increase when ascending stairs for the patients who had the mini-posterior approach [16], and at 1 year, there was a greater (p = 0.035) increase in single-leg stance time on level ground for the patients who had the mini-posterior approach (Fig. 4). At 1 year postoperatively, there were no differences (p = 0.30) in single-leg stance time descending stairs. At 2 months postoperatively, the two groups had no differences in forward velocity, and at 1 year postoperatively, there remained no differences in forward walking velocity on level ground (p = 0.26) or when ascending (p = 0.50) or descending stairs (p = 0.59) (Table 2).
Fig. 4.
A graph shows trends toward greater improvement for the patients who had the mini-posterior THA in single-leg stance time on level ground (p = 0.07) and when ascending stairs (p = 0.15) from preoperatively to 1 year postoperatively
Discussion
Many theoretical advantages of minimally invasive approaches to THA have been proposed, including improved recovery and function [4, 6, 7, 13, 21, 36, 38]. However, relatively little direct objective comparison data have been published comparing minimally invasive THA techniques with one another or with an established THA technique [11, 18, 29]. Using comprehensive gait analysis and strength testing, we previously investigated the early (2-month) functional outcome after THA, with a randomized clinical trial of the two-incision and mini-posterior surgical approaches and found an advantage for the mini-posterior approach [16]. In the current study, we determined whether the 2-month objective functional advantages for the mini-posterior technique over the two-incision technique, were still present at 1 year postoperatively. We found that differences in selected hip muscle strength, hip internal moments, and the spatiotemporal gait parameter of single-leg stance during level walking at 1 year postoperatively continued to favor the patients who had the mini-posterior THA over the patients who had the two-incision THA.
This prospective randomized strength and gait analysis study of two approaches to THA has some limitations. First, the conclusions are limited by the relatively small sample size, which may be insufficiently powered to show all statistical differences. Thus, it is appropriate to consider this work a pilot study of these functional parameters of strength and gait after contemporary THA. Currently, the lack of substantial published data for expected improvements in strength or for gait analysis parameters made it impossible to perform an a priori power analysis [2, 3, 37]. A post hoc power analysis was performed and found significant outcomes had adequate statistical power. A second limitation is that we do not have sufficient followup at this time to assess the long-term results for these patients, particularly regarding the durability of THA done with either of these two minimally invasive approaches. A third limitation is that the patients included in this study were a subset of the 72 patients originally randomized. Of the 25 patients in the subset, those included in the analysis of gait and strength parameters at 1 year postoperatively were patients able to complete preoperative and 1-year postoperative gait analysis and strength testing. Of the 22 patients who were able to complete preoperative gait analysis, one was removed from the 2-month evaluation owing to a deep infection, and two did not return for the 1-year followup, possibly introducing some bias in 2-month, and more particularly, 1-year results. Fourth, a patient-based outcome was not correlated to the strength and gait analysis data. Therefore, it is difficult to interpret whether significant differences in the data presented represent true clinical differences.
Our study patients who had the two-incision THA had poorer hip strength than patients who had the mini-posterior THA at 2 months postoperatively, and this persisted at 1 year. This is especially apparent when comparing hip flexion strength between the two groups. For the two-incision approach, the Smith-Petersen interval is used to expose the hip, cut the femoral neck, and prepare the acetabulum. Perrin et al. reported reduced tissue trauma with this two-incision technique [32]. However, in a cadaveric study using the anterior Smith-Petersen approach, measurable damage to the muscle of the direct head of the rectus femoris was observed in four of six specimens [22]. It is likely similar damage occurred in patients in the two-incision group of our study, either from retractors or insertion of instruments through this anteriorly based approach. The hips that had the mini-posterior approach avoided any potential damage to the hip flexors. In addition, detailed cadaveric study has shown measurable muscle damage with minimally invasive techniques [21]. Specifically, the two-incision technique has show there is greater injury of the gluteus minimus and medius muscles than with the mini-posterior approach [21]. Regarding hip abduction, there was no clinical difference in strength at 1 year between patients in either group. Although a previous cadaveric study found more injury to the gluteus medius muscle using the two-incision approach, there was no difference in damage to the gluteus medius tendon [21]. Further, a difference in muscle damage at the time of surgery may not translate to objective clinical differences, especially after 1 year of postoperative rehabilitation [24].
At 2 months postoperatively, the patients who had the mini-posterior THA had evidence of better hip function compared with patients who had the two-incision THA, as reflected by changes in gait kinematics, and this advantage persisted at 1 year postoperatively. Previous gait analysis has established traditional surgical approaches for THA influence the 6-month postoperative result, with anterolateral approaches showing greater characteristics of pathologic gait and less range of functional ability compared with posterior approaches [19, 39]. However, the literature is unclear regarding continued and long-term function of THA, with some studies showing no improvement with time [14, 32–34], and others showing additional improvement of gait characteristics after 2 years [15, 17]. Minimally invasive approaches previously have not shown a functional advantage postoperatively. In a prospective blinded study, there was no demonstrable benefit of a minimally invasive technique compared with a traditional THA technique as evaluated by changes in pelvic tilt, ROM in the sagittal plane, hip abduction and adduction, or rotation of the hip and foot [2]. Additionally, these gait kinetics are similar to those reported in a prospective analysis showing no difference in normalized abductor torque at midstance between three minimally invasive surgical approaches [23].
The patients who had the mini-posterior THA had less antalgic gait compared with patients who had the two-incision THA at 1 year postoperatively, as reflected by changes in single-leg stance time on level ground. That finding contrasts with a previously published gait study that compared minimally invasive surgical approaches (mini-posterior, anterolateral, and anterior Judet), and a traditional posterior approach, and found no difference for stride length, cadence, velocity, single-limb support time, or double-limb support time at 6 weeks or 3 months postoperatively [37]. The authors of that study suggested patients undergoing THA with any of these surgical approaches recover muscle function to preoperative levels within 6 weeks postoperatively [37]. Other authors have supported this contention that the ultimate results of two different surgical approaches in THAs are equivalent [8, 11]. In two separate prospective studies comparing minimally invasive approaches with standard approaches, the patients who underwent the minimally invasive THA limped less at early followup (6 months to 3 months), but this advantage disappeared by the 1-year followup [8, 11]. However, in these studies, gait analysis was not performed. Rather, limp was assessed on clinical examination as the only objective measure of gait [8, 11]. The detection of limp on clinical examination, used as the outcome measure of gait in the above two studies, is unlikely to be as sensitive as gait analysis to detect differences in hip function 1 year after surgery.
Our prospective randomized study using comprehensive gait analysis and strength testing found an early (2-month) and late (1-year) functional advantage of the mini-posterior THA over two-incision THA, including hip flexor and internal rotator muscle strength, hip flexor internal moment, and single-leg stance during level walking. The added technical complexity of the two-incision approach to THA was not rewarded with better function; instead, it was the patients who had a mini-posterior THA who had better hip function.
Acknowledgment
We thank Kristine M. Thomsen BA, for help in performing the statistical analysis.
Footnotes
One author (MWP) has received royalties from Zimmer, Inc (Warsaw, IN). Each of the other authors certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Mayo Clinic.
References
- 1.Bal BS, Haltom D, Aleto T, Barrett M. Early complications of primary total hip replacement performed with a two-incision minimally invasive technique. J Bone Joint Surg Am. 2005;87:2432–2438. doi: 10.2106/JBJS.D.02847. [DOI] [PubMed] [Google Scholar]
- 2.Bennett D, Ogonda L, Elliott D, Humphreys L, Beverland DE. Comparison of gait kinematics in patients receiving minimally invasive and traditional hip replacement surgery: a prospective blinded study. Gait Posture. 2006;23:374–382. doi: 10.1016/j.gaitpost.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Bennett D, Ogonda L, Elliott D, Humphreys L, Lawlor M, Beverland D. Comparison of immediate postoperative walking ability in patients receiving minimally invasive and standard-incision hip arthroplasty: a prospective blinded study. J Arthroplasty. 2007;22:490–495. doi: 10.1016/j.arth.2006.02.173. [DOI] [PubMed] [Google Scholar]
- 4.Berger RA. Total hip arthroplasty using the minimally invasive two-incision approach. Clin Orthop Relat Res. 2003;417:232–241. doi: 10.1097/01.blo.0000096828.67494.95. [DOI] [PubMed] [Google Scholar]
- 5.Berger RA, Duwelius PJ. The two-incision minimally invasive total hip arthroplasty: technique and results. Orthop Clin North Am. 2004;35:163–172. doi: 10.1016/S0030-5898(03)00110-X. [DOI] [PubMed] [Google Scholar]
- 6.Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 7.Berry DJ, Berger RA, Callaghan JJ, Dorr LD, Duwelius PJ, Hartzband MA, Lieberman JR, Mears DC. Minimally invasive total hip arthroplasty: development, early results, and a critical analysis. J Bone Joint Surg Am. 2003;85:2235–2246. [PubMed] [Google Scholar]
- 8.Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP. Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:139–144. doi: 10.1016/j.arth.2004.09.061. [DOI] [PubMed] [Google Scholar]
- 9.Desser DR, Mitrick MF, Ulrich SD, Delanois RE, Mont MA. Total hip arthroplasty: comparison of two-incision and standard techniques at an AOA-accredited community hospital. J Am Osteopath Assoc. 2010;110:12–15. [PubMed] [Google Scholar]
- 10.DiGioia AM, 3rd, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18:123–128. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 11.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty: a prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89:1153–1160. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 12.Duwelius PJ, Dorr LD. Minimally invasive total hip arthroplasty: an overview of the results. Instr Course Lect. 2008;57:215–222. [PubMed] [Google Scholar]
- 13.Huo MH, Brown BS. What’s new in hip arthroplasty. J Bone Joint Surg Am. 2003;85:1852–1864. doi: 10.2106/00004623-200309000-00041. [DOI] [PubMed] [Google Scholar]
- 14.Isobe Y, Okuno M, Otsuki T, Yamamoto K. Clinical study on arthroplasties for osteoarthritic hip by quantitative gait analysis: comparison between total hip arthroplasty and bipolar endoprosthetic arthroplasty. Biomed Mater Eng. 1998;8:167–175. [PubMed] [Google Scholar]
- 15.Komistek RD, Dennis DA, Ochoa JA, Haas BD, Hammill C. In vivo comparison of hip separation after metal-on-metal or metal-on-polyethylene total hip arthroplasty. J Bone Joint Surg Am. 2002;84:1836–1841. doi: 10.2106/00004623-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Krych AJ, Pagnano MW, Wood KC, Meneghini RM, Kaufmann K. No benefit of the two-incision THA over mini-posterior THA: a pilot study of strength and gait. Clin Orthop Relat Res. 2010;468:565–570. doi: 10.1007/s11999-009-0780-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kyriazis V, Rigas C. Temporal gait analysis of hip osteoarthritic patients operated with cementless hip replacement. Clin Biomech. (Bristol, Avon) 2002;17:318–321. doi: 10.1016/S0268-0033(02)00024-4. [DOI] [PubMed] [Google Scholar]
- 18.Lugade V, Klausmeier V, Jewett B, Collis D, Chou LS. Short-term recovery of balance control after total hip arthroplasty. Clin Orthop Relat Res. 2008;466:3051–3058. doi: 10.1007/s11999-008-0488-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madsen MS, Ritter MA, Morris HH, Meding JB, Berend ME, Faris PM, Vardaxis VG. The effect of total hip arthroplasty surgical approach on gait. J Orthop Res. 2004;22:44–50. doi: 10.1016/S0736-0266(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 20.Malik A, Dorr L. The science of minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2007;463:74–84. doi: 10.1097/BLO.0b013e3181468766. [DOI] [PubMed] [Google Scholar]
- 21.Mardones R, Pagnano MW, Nemanich PJ, Trousdale RT. The Frank Stinchfield Award: Muscle damage after total hip arthroplasty done with the two-incision and mini-posterior techniques. Clin Orthop Relat Res. 2005;441:63–67. doi: 10.1097/01.blo.0000194727.55372.04. [DOI] [PubMed] [Google Scholar]
- 22.Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453:293–298. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- 23.Meneghini RM, Smits SA, Swinford RR, Bahamonde RE. A randomized, prospective study of 3 minimally invasive surgical approaches in total hip arthroplasty: comprehensive gait analysis. J Arthroplasty. 2008;23(6 suppl 1):68–73. [DOI] [PubMed]
- 24.Müller M, Tohtz S, Winkler T, Dewey M, Springer I, Perka C. MRI findings of gluteus minimus muscle damage in primary total hip arthroplasty and the influence on clinical outcome. Arch Orthop Trauma Surg. 2010;130:927–935. doi: 10.1007/s00402-010-1085-4. [DOI] [PubMed] [Google Scholar]
- 25.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes: a prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701–710. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 26.Pagnano MW, Hebl J, Horlocker T. Assuring a painless total hip arthroplasty: a multimodal approach emphasizing peripheral nerve blocks. J Arthroplasty. 2006;21(4 suppl 1):):80–84. doi: 10.1016/j.arth.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Pagnano MW, Leone J, Lewallen DG, Hanssen AD. Two-incision THA had modest outcomes and some substantial complications. Clin Orthop Relat Res. 2005;441:86–90. doi: 10.1097/01.blo.0000191275.80527.d6. [DOI] [PubMed] [Google Scholar]
- 28.Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Patients preferred a miniposterior THA to a contralateral two-incision THA. Clin Orthop Relat Res. 2006;453:156–159. doi: 10.1097/01.blo.0000238858.38992.2d. [DOI] [PubMed] [Google Scholar]
- 29.Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:1000–1006. doi: 10.2106/JBJS.G.00804. [DOI] [PubMed] [Google Scholar]
- 30.Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: surgical technique . J Bone Joint Surg Am. 2009;91(suppl 2 pt 1):50–73. doi: 10.2106/JBJS.H.01531. [DOI] [PubMed] [Google Scholar]
- 31.Palutsis RS, Sheridan KC, Wasielewski RC. One surgeon’s experience with the 2-incision technique for total hip arthroplasty. J Arthroplasty. 2008;25:71–75. doi: 10.1016/j.arth.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 32.Perrin T, Dorr LD, Perry J, Gronley J, Hull DB. Functional evaluation of total hip arthroplasty with five- to ten-year follow-up evaluation. Clin Orthop Relat Res. 1985;195:252–260. [PubMed] [Google Scholar]
- 33.Perron M, Malouin F, Moffet H, McFadyen BJ. Three-dimensional gait analysis in women with a total hip arthroplasty. Clin Biomech.(Bristol, Avon) 2000;15:504–515. doi: 10.1016/S0268-0033(00)00002-4. [DOI] [PubMed] [Google Scholar]
- 34.Sicard-Rosenbaum L, Light KE, Behrman AL. Gait, lower extremity strength, and self-assessed mobility after hip arthroplasty. J Gerontol A Biol Sci Med Sci. 2002;57:M47–M51. doi: 10.1093/gerona/57.1.m47. [DOI] [PubMed] [Google Scholar]
- 35.Tanavalee A, Jaruwannapong S, Yuktanandana P, Itiravivong P. Early outcomes following minimally invasive total hip arthroplasty using a two-incision approach versus a mini-posterior approach. Hip Int. 2006;16(suppl 4):17–22. doi: 10.1177/112070000601604S05. [DOI] [PubMed] [Google Scholar]
- 36.Waldman BJ. Minimally invasive total hip replacement and perioperative management: early experience. J South Orthop Assoc. 2002;11:213–217. [PubMed] [Google Scholar]
- 37.Ward SR, Jones RE, Long WT, Thomas DJ, Dorr LD. Functional recovery of muscles after minimally invasive total hip arthroplasty. Instr Course Lect. 2008;57:249–254. [PubMed] [Google Scholar]
- 38.Wenz JF, Gurkan I, Jibodh S. Mini-incision total hip arthroplasty: a comparative assessment of perioperative outcomes. Orthopedics. 2002;25:1031–1043. doi: 10.3928/0147-7447-20021001-14. [DOI] [PubMed] [Google Scholar]
- 39.Whatling GM, Dabke HV, Holt CA, Jones L, Madete J, Alderman PM, Roberts P. Objective functional assessment of total hip arthroplasty following two common surgical approaches: the posterior and direct lateral approaches. Proc Inst Mech Eng H. 2008;222:897–905. doi: 10.1243/09544119JEIM396. [DOI] [PubMed] [Google Scholar]