Abstract
Background
Hip fractures in the elderly are associated with high 1-year mortality rates, but whether patients with other lower extremity fractures are exposed to a similar mortality risk is not clear.
Questions/purposes
We evaluated the mortality of elderly patients after distal femur fractures; determined predictors for mortality; analyzed the effect of surgical delay; and compared survivorship of elderly patients with distal femur fractures with subjects in a matched hip fracture group.
Patients and Methods
We included 92 consecutive patients older than 60 years with low-energy supracondylar femur fractures treated between 1999 and 2009. Patient, fracture, and treatment characteristics were extracted from operative records, charts, and radiographs. Data regarding mortality were obtained from the Social Security Death Index.
Results
Age-adjusted Charlson Comorbidity Index and a previous TKA were independent predictors for decreased survival. Congestive heart failure, dementia, renal disease, and history of malignant tumor led to shorter survival times. Patients who underwent surgery more than 4 days versus 48 hours after admission had greater 6-month and 1-year mortality risks. No differences in mortality were found comparing patients with native distal femur fractures with patients in a hip fracture control group.
Conclusions
Periprosthetic fractures and fractures in patients with dementia, heart failure, advanced renal disease, and metastasis lead to reduced survival. The age-adjusted Charlson Comorbidity Index may serve as a useful tool to predict survival after distal femur fractures. Surgical delay greater than 4 days increases the 6-month and 1-year mortality risks. Mortality after native fractures of the distal femur in the geriatric population is high and similar to mortality after hip fractures.
Level of Evidence
Level II, prognostic study. See the guidelines online for a complete description of evidence.
Introduction
Fractures of the distal femur occur most frequently either as high-energy injuries in young men or low-energy fractures in elderly women [33]. In elderly patients, distal femur fractures are the second most frequent fragility fractures of the femur following those of the hip [1, 35, 36], and these patients are at elevated risk for complications, given the high prevalence of medical comorbidities [8, 12, 36].
Numerous studies regarding treatment of distal femur fractures focus on orthopaedic outcomes, such as nonunion, malunion, and infection [6, 23, 27–29, 31, 40, 44, 48]. Despite affecting a high-risk population, data regarding postoperative mortality are limited. Of the few studies analyzing mortality, one randomized controlled trial reported a 30-day mortality rate of 10%, whereas a prospective case series reported 6-month and 1-year mortality rates of 17% and 30%, respectively [9, 18]. These outcomes have been compared with historical mortality rates published for fractures of the hip, but a direct comparison has not been performed.
Mortality after fractures of the hip has been studied extensively. Patients sustaining a hip fracture have a higher mortality rate than uninjured age- and gender-matched patients [2, 3, 5, 7, 13, 14, 45]. Given the similarity in age and gender distribution of patients with low-energy distal and proximal femur fractures and based on the limited published data, we hypothesized patients with distal femur fractures would have a mortality rate similar to that of patients with fractures of the hip.
Our specific aims were to assess a cohort of elderly patients with distal femur fractures treated during a 10-year period to (1) calculate overall, 30-day, 6-month, and 1-year mortality rates in elderly patients with distal femur fractures; (2) determine the existence of variables that influence survivorship; (3) evaluate the importance of surgical delay on mortality; and (4) compare the mortality of patients with distal femur fractures with that of a matched cohort of patients with hip fractures.
Patients and Methods
After protocol approval by the institutional review board, patients who had undergone lateral locked plating of a supracondylar femur fracture were identified from our institutional orthopaedic trauma database for the period from November 1999 to September 2009. Inclusion criteria were age of 60 years or older and mechanism of injury attributable to a fall from a standing height (low-energy injury). Patients with pathologic fractures (other than osteoporosis) were excluded. Operative records and charts were reviewed for patient characteristics (age, gender, smoking status, body mass index [BMI]) and fracture characteristics (laterality and soft tissue injury according to Gustilo et al. [25, 26]). Radiographs of the femur and knee were reviewed for fracture classification (AO/OTA [32]) and to establish the presence of a TKA. Time between admission and surgery was recorded. The Charlson Comorbidity Index (CCI) [11] and age-adjusted CCI [10] at the time of injury were calculated based on comorbidities obtained from patient clinical records and from administrative ICD-9 (International Classification of Diseases, Ninth Revision) codes as described by Deyo et al. [17]. The CCI and age-adjusted CCI have been validated as tools to predict 1-year mortality rates in longitudinal clinical studies. The CCI is calculated by adding the coefficients assigned to comorbidities present at enrollment. One point each is assigned to myocardial infarction, congestive heart failure, peripheral vascular disease, dementia, chronic pulmonary disease, connective tissue disease, peptic ulcer disease, mild liver disease, and diabetes. Two points are assigned to hemiplegia, moderate to severe renal disease, diabetes with organ damage, any tumor (within 5 years of enrollment), lymphoma, and leukemia. Three points are assigned to moderate to severe liver disease and 6 points to AIDS and metastatic solid tumor [11]. By adding age as an additional variable to predict mortality, the developers of the original CCI developed an age-adjusted CCI. It includes the same point system as the original CCI and adds 1 point for each decade after the age of 50 years, up to 6 points for patients 100 years or older [10].
Death and date of death were extracted for each patient from the Social Security Administration Death Master File (Social Security Death Index [SSDI]), a database available publicly through the www.rootsweb.ancestry.com Web site [43]. A combination of Social Security number, first name, middle initial, last name, and date of birth was used to maximize data accuracy [15, 20].
A total of 92 consecutive patients with distal femur fractures with an average age of 77.9 years (range, 60–100 years) were included. Seventy-two (78%) patients were women, and the minimum followup was 12 days (average, 2.8 years; range, 12 days–9.8 years). The average CCI was 1.8 (range, 0–9). The majority of fractures were closed (n = 87; 95%) and extraarticular (n = 70; 76%). More than half the fractures (n = 48; 52%) occurred around an existing TKA (Table 1).
Table 1.
Demographics and mortality rates for distal femur fractures
| Variable | Total (n = 92) | Nonperiprosthetic (n = 44) | Periprosthetic (n = 48) | p Value |
|---|---|---|---|---|
| Gender (female) | 72 (78%) | 35 (80%) | 37 (77%) | 0.78 |
| Smoker | 12 (13%) | 9 (21%) | 3 (6%) | 0.04 |
| Charlson Comorbidity Index* | 1.8 ± 1.9 (0–9) | 2.16 ± 2.1 (0–9) | 1.50 ± 1.6 (0–8) | 0.10 |
| Charlson Comorbidity Index (age adjusted)* | 5.1 ± 2.8 (2–13) | 5.5 ± 2.4 (2–13) | 4.8 ± 2.1 (2–12) | 0.14 |
| Age (years)* | 77.9 ± 10.2 (60–100) | 78.3 ± 10.0 (60–100) | 77.6 ± 10.5 (60–95) | 0.76 |
| Body mass index (kg/m2)* | 29.6 ± 8.3 (17.9–54.8) | 27.7 ± 8.0 (18.6–54.8) | 31.4 ± 8.2 (17.9–53.1) | 0.03 |
| Side (right) | 53 (58%) | 26 (59%) | 27 (56%) | 0.78 |
| OTA/AO classification | < 0.001 | |||
| 33A | 70 (76%) | 22 (50%) | 48 (100%) | |
| 33C | 22 (24%) | 22 (50%) | 0 (0%) | |
| Fracture type | 0.18 | |||
| Closed | 87 (95%) | 40 (91%) | 47 (98%) | |
| Type I | 3 (3%) | 3 (7%) | 0 (0%) | |
| Type II | 2 (2%) | 1 (2%) | 1 (2%) | |
| Time from admission to surgery (days)* | 3.7 ± 5.4 (0–41) | 4.6 ± 7.1 (0–41) | 2.9 ± 3.0 (0–21) | 0.14 |
| Followup (months)* | 33.7 ± 33.4 (0.4–118) | 37.6 ± 36.3 (0.5–118) | 30.1 ± 30.4 (0.4–111) | 0.28 |
| Dead (total) | 35 (38%) | 13 (30%) | 22 (46%) | 0.08 |
| Dead at 30 days† | 5 (6%) | 1 (2%) | 4 (8%) | 0.22 |
| Dead at 6 months‡ | 15 (18%) | 5 (13%) | 10 (24%) | 0.15 |
| Dead at 1 year§ | 19 (25%) | 8 (23%) | 11 (27%) | 0.45 |
| Time from surgery to death (months)* | 21.4 ± 26.32 (0.4–86.7) | 21.0 ± 26.3 (0.5–86.7) | 21.7 ± 26.9 (0.4–81.7) | 0.94 |
* Values are expressed as mean ± SD, with range in parentheses; all other values are expressed as number of patients, with percentage in parentheses; †denominator n = 91 for total, n = 43 for nonperiprosthetic, and n = 48 for periprosthetic; ‡denominator n = 82 for total, n = 40 for nonperiprosthetic, and n = 42 for periprosthetic; §denominator n = 76 for total, n = 35 for nonperiprosthetic, and n = 41 for periprosthetic.
Overall mortality rates and 30-day, 6-month, and 1-year mortality rates were calculated for patients who had completed followup to that time. Cox regression was used to define the effect of the following variables on survivorship: age, gender, smoking status, CCI, age-adjusted CCI, BMI, classification of Gustilo et al., OTA classification, presence of TKA, and time from admission to surgery. Additionally, variables of the CCI were analyzed as an independent regression block. Survival rates for variables with significant hazard ratios (HRs) were plotted using Kaplan-Meier analysis.
The effect of surgical delay on mortality was assessed by comparing rates in patients who underwent surgery during the first 48 hours after admission, during 48 to 96 hours after admission, or 4 days after admission. Mortality rates were compared at 30 days, 6 months, and 1 year.
After assessing for predictors of survivorship, mortality of patients with distal femur fractures was compared with that of a 1:1 matched control group of patients with hip fractures (femoral neck or intertrochanteric fracture) that was extracted from our institutional database. As patients with periprosthetic distal femur fractures were identified as having a higher mortality risk, only patients with nonperiprosthetic fractures (n = 44) were selected for comparison with patients with hip fractures. A priori it was defined that control subjects had to be of the same gender, within 5 years of age, within 2 years of operation date, and have a CCI within 2 points of the patients with nonperiprosthetic distal femur fractures. The matched hip fracture control group was similar in terms of age, minimum followup, and CCI. Twenty-five (57%) fractures were extracapsular and all were closed. Hip fractures most frequently had been fixed using an intramedullary nail (n = 21; 48%). No differences were found between the two groups regarding demographic or personal variables. Furthermore, no difference was found in delay from admission to primary surgery. After exclusion of two patients who had been treated more than 10 days after admission in each group, the average delay to surgery was 2.5 and 3.1 days for patients with hip and distal femur fractures, respectively (p = 0.13). Patients with distal femur fractures had a greater BMI than patients with hip fractures (29.6 versus 23.9 kg/m2; p < 0.01) (Table 2).
Table 2.
Demographics and mortality rates for matched nonperiprosthetic distal femur and hip fractures
| Variable | Distal femur fracture (n = 44) | Hip fracture (n = 44) | p Value |
|---|---|---|---|
| Gender (female) | 35 (80%) | 35 (80%) | 1.00 |
| Smoker | 9 (21%) | 10 (23%) | 0.50 |
| Charlson Comorbidity Index* | 2.16 ± 2.1 (0–7) | 2.0 ± 1.6 (0–9) | 0.74 |
| Charlson Comorbidity Index (age adjusted)* | 5.5 ± 2.4 (2–13) | 5.3 ± 2.0 (2–10) | 0.70 |
| Age (years)* | 78.3 ± 10.0 (60–100) | 77.6 ± 9.8 (60–96) | 0.77 |
| Body mass index (kg/m2)* | 27.7 ± 7.0 (18.6–54.8) | 24.1 ± 5.4 (13.3–37.1) | 0.02 |
| Side (right) | 26 (59%) | 19 (43%) | 0.14 |
| OTA/AO classification | < 0.01 | ||
| 31A (intertrochanteric) | 0 (0%) | 25 (57%) | |
| 31B (femoral neck) | 0 (0%) | 19 (43%) | |
| 33A | 22 (50%) | 0 (0%) | |
| 33C | 22 (50%) | 0 (0%) | |
| Fracture type | 0.12 | ||
| Closed | 40 (91%) | 44 (100%) | |
| Type I | 3 (7%) | 0 (0%) | |
| Type II | 1 (2%) | 0 (0%) | |
| Time from admission to surgery (days)* | 4.6 ± 7.1 (0–41) | 4.3 ± 9.7 (0–63) | 0.89 |
| Procedure | < 0.01 | ||
| Lateral locking plate | 44 (100%) | 0 (0%) | |
| Intramedullary nail | 0 (0%) | 21 (48%) | |
| Hemiarthroplasty | 0 (0%) | 11 (25%) | |
| Cannulated screws | 0 (0%) | 6 (14%) | |
| Side plate and screws | 0 (0%) | 5 (11%) | |
| THA | 0 (0%) | 1 (2%) | |
| Followup (months)* | 37.6 ± 36.3 (0.5–118) | 35.0 ± 33.0 (1–124) | 0.72 |
| Dead (total) | 13 (30%) | 19 (43%) | 0.18 |
| Dead at 30 days† | 1 (2%) | 0 (0%) | 0.31 |
| Dead at 6 months‡ | 5 (13%) | 5 (14%) | 0.90 |
| Dead at 1 year§ | 8 (23%) | 8 (22%) | 0.95 |
| Time from surgery to death (months)* | 21.0 ± 26.3 (0.5–86.7) | 26.3 ± 26.0 (1.1–91.7) | 0.58 |
* Values are expressed as mean ± SD, with range in parentheses; all other values are expressed as number of patients, with percentage in parentheses; †denominator n = 43 for distal femur fractures; ‡denominator n = 40 for distal femur fractures and n = 37 for hip fractures; §denominator n = 35 for distal femur fractures and n = 36 for hip fractures.
Proportions and means were compared between groups using either the chi square or Fisher’s exact test and Student’s t test, respectively. Survival was evaluated using Kaplan-Meier analysis and compared using the log-rank (Mantel-Cox) test. Statistical significance was set at p < 0.05 and 95% confidence intervals (CIs). Statistical analysis was performed with SPSS® Version 16.0 for Windows® (SPSS Inc, Chicago, IL, USA).
Results
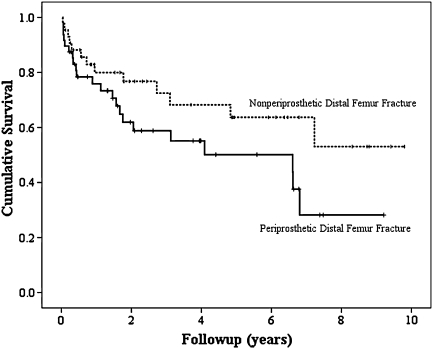
The overall mortality rate after distal femur fractures at a maximum followup of 9.8 years was 38%. Mortality rates at 30 days, 6 months, and 1 year after surgery were 6%, 18%, and 25%, respectively (Table 1). The five patients who died during the first 30 days had an average age of 85.3 years (range, 76–94 years) and an average CCI of 4 (range, 3–8). One 86-year-old patient with a history of prostate cancer and mitral valve repair (CCI, 3) died while in the hospital owing to pneumonia, respiratory failure, and sepsis. Four patients died after having been discharged from the hospital and their causes of death could not be established from the available medical records. Analysis of the distal femur fracture group showed the presence of a TKA and higher age-adjusted CCI led to shorter survival (HR = 3.21, p = 0.005; and HR = 1.32, p = 0.004, respectively). Overall mortality was 30% for nonperiprosthetic (native) fractures and 46% for periprosthetic fractures (p = 0.08) (Fig. 1). Thirty-day, 6-month, and 1-year mortality rates were 2%, 13%, and 23% for the native fracture group and 8%, 24%, and 27% for the periprosthetic fracture group (p = 0.22, 0.15, and 0.45, respectively) (Table 1).
Fig. 1.
Kaplan-Meier survival curves show survivorship of distal femur fractures in the presence and absence of a TKA. The vertical lines represent censored data.
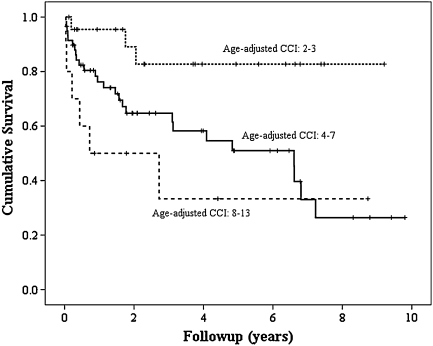
Overall mortality was predicted by the age-adjusted CCI (p = 0.01). Mortality rates were 13%, 44%, and 60% for patients with an age-adjusted CCI of 2 or 3, 4 to 7, and 8 to 13, respectively (p = 0.01). Thirty-day, 6-month, and 1-year mortality rates also were predicted by age-adjusted CCI (Fig. 2). Cox regression analysis also revealed congestive heart failure (HR = 4.52; 95% CI, 1.96–10.42; p < 0.001), dementia (HR = 4.52; 95% CI, 1.77–11.63; p = 0.002), moderate to severe renal disease (HR = 4.67; 95% CI, 1.91–11.36; p = 0.001), and history of a malignant tumor (HR = 2.9; 95% CI, 1.17–7.19; p = 0.022) led to shorter survival times. Regression analysis did not show an effect of either age or CCI individually on survival. Furthermore gender, smoking habit, BMI, and fracture classification did not independently affect mortality.
Fig. 2.
Kaplan-Meier survival curves show survivorship of distal femur fractures according to age-adjusted CCI. The vertical lines represent censored data.
Delay to surgery also was not identified as an independent predictor for mortality. However, according to univariate analysis, some mortality rates varied according to delay to surgery. No differences were found for 30-day mortality according to surgical delay (p > 0.32). Six-month mortality was related to surgical delay when patients who had surgery within the first 48 hours and those who underwent surgery more than 4 days after admission were compared [5% versus 35% (p = 0.02)]. One-year mortality was similarly related to delay when patients who had surgery within 48 hours were compared with those who had a delay in surgery greater than 4 days [6% versus 47% (p = 0.005)]. There was no difference in mean age, age adjusted CCI, or percent of patients with periprosthetic fractures in the groups of patients with delays to surgery.
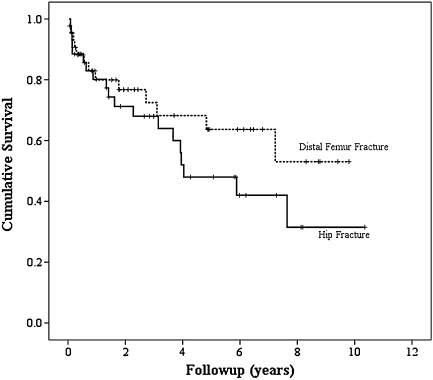
Mortality rates were similar when proximal and distal femur fractures were compared. The overall mortality rate at a maximum followup of 9.8 years for patients with distal femur fractures was 30%, compared with 43% for patients with hip fractures at a maximum followup of 10.3 years (p = 0.18). The mortality rates at 30 days, 6 months, and 1 year after surgery were 2%, 13%, and 23% for patients with distal femur fractures and 0%, 14%, and 22% for patients with hip fractures (p = 0.31, 0.90, and 0.95, respectively) (Table 2). Kaplan-Meier analysis showed similar overall survival plots during the three first postoperative years for distal femur and hip fractures (Fig. 3). No difference was found according to the log-rank test (p = 0.83).
Fig. 3.
Kaplan-Meier survival curves show survivorship of nonperiprosthetic distal femur and hip fractures. The vertical lines represent censored data.
Discussion
We assessed mortality in elderly patients with distal femur fractures, determined the existence of variables that influence survivorship, evaluated the importance of surgical delay on mortality, and compared the mortality of patients with distal femur fractures with that of a matched cohort of patients with hip fractures.
Our study had several limitations. Our data for mortality were obtained using the SSDI, instead of the National Death Registry (NDR) [43]. The NDR has been considered the gold standard for data on mortality as supported by an earlier study that showed the SSDI to be accurate in 83% of cases compared with 87% to 98% for the NDR [15]. A recent study by Fillenbaum et al. [20] however showed, by combining Social Security Number with date and month of birth, a match between NDR and SSDI was obtained in 94.7% of cases. We assume, by using these data points, in addition to first and last name and middle initial for every patient included in our study, a satisfactory level of accuracy was achieved. The SSDI also has the advantage of being publicly available and free of charge. Additionally, our stringent matching protocol allowed us to have similar patient characteristics for patients with distal femur fractures and with hip fractures. As patients with hip fractures were matched to the characteristics of the consecutive nonperiprosthetic distal femur fracture cohort, it may be suggested an artificial patient composition was created that is not comparable to the average patient with a hip fracture. However, we believe it was important to reduce the number of possible confounders (age, gender, comorbidities) to be able to accurately compare the effect of fracture type on mortality. Furthermore, by identifying periprosthetic fractures as a risk factor for increased mortality using multiple regression analysis, we were able to further improve group comparability.
From a statistical perspective, our sample was underpowered to determine similarity in mortality rates among distal femur and hip fractures. According to post hoc analysis, a sample size of 92 fractures would have been required in each group to achieve a power of 80% for the comparison of mortality using the log-rank (Mantel-Cox) test [42]. Although comparing the overall distal femur group with a control group with hip fractures seemed statistically adequate, the large proportion of periprosthetic fractures in the distal femur group would have compromised clinical comparability. Results for 30-day, 6-month, and 1-year mortality were similar, however, strongly supporting the similarity in survival of these two patient populations.
Regarding the external validity of our results, we believe our patient groups are representative of the population seen in the clinical setting. All patients underwent operative treatment, as nonoperative treatment only seldom is required for the most infirm patients, which would represent clinical outliers [9, 49]. Although various treatment alternatives were performed in the hip fracture group, we included only fractures of the distal femur managed with lateral locked plating. Even though similar results have been reported for this treatment modality and retrograde nailing, locked plating is the standard treatment at our institution as it allows fixation in very distal fractures, allows use of the plate for fracture reduction, and in our experience, leads to more reliable fracture alignment [27, 31, 38, 40].
During the first 30 days after surgery, five patients with distal femur fractures died, accounting for 14% of the 35 patients who died during the overall followup. Of these, one patient died of pneumonia, respiratory failure, and sepsis. Although the causes of death could not be determined for the remaining patients, it is likely events associated with the surgical procedure and acute physiologic stress were the most probable causes during the early postoperative phase. According to Deakin et al. [16], bronchopneumonia is responsible for 39% of in-hospital deaths in patients with isolated limb and pelvic fractures, followed by malignancy in 11%, ischemic heart disease in 11%, and sepsis in 7%. Little is known about the causes of death at later times during the postoperative course of patients with fractures. Of the 35 patients who died during the overall followup, 29% (n = 10) died during the second to sixth months and 26% (n = 9) died during the second half of the first postoperative year. We assume causes of death most likely were related to the patients’ baseline comorbidities and postoperative complications, which may be exacerbated by prolonged immobility and decreased ambulatory capacity. Roche et al. [39] reported chest infection and heart failure were the most frequent postoperative complications in elderly patients with hip fractures. Both of these conditions correlated with increased mortality at 1 year after surgery.
When adjusting for gender, age, comorbidities, and surgical delay, our results show patients with periprosthetic distal femur fractures have a shorter survival compared with those with nonperiprosthetic fractures. Extrapolating these results to those of the comparison between nonperiprosthetic distal femur fractures and hip fractures, it could be inferred periprosthetic distal femur fractures likely carry a higher mortality risk than hip fractures. Bhattacharyya et al. [4] found similar mortality rates between patients with hip fractures and those with periprosthetic fractures of the femur about THA stems. Although this in contrast to our results, of their periprosthetic fracture cohort of 106 patients, only 32 were classified as having Vancouver Type C fractures, which, in some instances, could have been distal femur fractures. Therefore it may be possible periprosthetic distal femur fractures carry a higher mortality risk than periprosthetic fractures of the femoral shaft about THA stems.
Although age and comorbidity were not identified as isolated predictors for mortality after distal femur fractures, the combination of these variables, in the form of the age-adjusted CCI, was a predictor. This finding suggests age and comorbidity by themselves do not increase the risk of mortality but rather act in combination, thereby requiring elevated age and comorbidity to act synergistically. Three distinct groups of age-adjusted CCI could be established (Fig. 2). Clinically significant differences in mortality rates between groups could be established. We believe this is relevant when discussing the prognosis for a patient with a distal femur fracture based on the patient’s age and his or her comorbidities. Of special prognostic value are patients with heart failure, dementia, advanced renal disease, and a history of a malignant tumor. Although it may be difficult to alter the natural history of dementia and malignancy, a special focus on optimizing cardiac and renal function may be required.
Our multiple regression analysis did not show time to surgery as an independent predictor for mortality. However, univariate analysis showed patients undergoing surgery more than 4 days after admission had a sevenfold greater 6-month and an almost eightfold greater 1-year mortality risk compared with those of patients undergoing surgery during the first 48 hours after admission. The mean age of the patients was similar across groups, and fractures treated more than 4 days after admission were periprosthetic in 36% of cases compared with 52% of fractures treated within 48 hours. The latter may suggest the effect of surgical delay may offset that of a lower proportion of periprosthetic fractures. However, age-adjusted CCI was 4.9 in patients undergoing surgery during the first 48 hours of admission, 5.0 in those treated 48 to 96 hours after admission, and 5.6 in those treated 4 days after admission. Although not significant, these differences may suggest the effect of delay to surgery on mortality may be related to the increase in age-adjusted CCI. With age-adjusted CCI identified as an independent risk factor for mortality, surgical delay may be regarded as a surrogate variable for patient health status, and a consequence of it, rather than as a cause for decreased survival. Surgical delay after hip fractures has been studied extensively but continues to be a source of debate. Gdalevich et al. [22] and Elliott et al. [19] found surgical delay reduced the probability of 1-year survival. However, an effect of preexisting disease severity on mortality also was found. As mentioned previously, these findings suggest delay of surgery may be a confounding factor related to the dependent (mortality) and the independent variables (comorbidity), rather than a causative factor of mortality. This idea is further supported by studies showing, after adjusting for patient age, gender, and comorbidities, surgical delay greater than 1 day does not lead to an increase of mortality [21, 24, 30, 47]. However, other studies have shown, even after adjusting for comorbidities, surgical delay greater than 48 hours led to an increase in 30-day and 1-year mortality rates [7, 34, 37, 41, 50]. Despite the conflicting evidence, we support early surgical intervention in healthy patients and those with minor physiologic abnormalities and attempt to delay surgery only in patients requiring physiologic stabilization or additional preoperative workup [46].
As distal femur fractures have their highest incidence in elderly patients, treatment often is challenged by the presence of medical comorbidities. According to Nieves et al. [36], 11% of women with a distal femur fracture have osteoporosis, 21% of patients have diabetes, more than 32% have cardiovascular disease, and a substantial proportion of patients takes at least one prescription drug. As a consequence, medical complications are not uncommon, and mortality rates have been reported to be similar to those of patients with hip fractures [8, 12]. Butt et al. [9] reported a 30-day mortality rate of 7% in 42 elderly patients treated for distal femur fractures (10% after operative treatment and 5% after nonoperative treatment). Dunlop and Brenkel [18] reported mortality rates of 17% at 6 months and 30% at 1 year after intramedullary nailing of 31 displaced distal femur fractures. Although they concluded their results paralleled those published in the literature for hip fractures, no study had to date directly compared the mortality rates for these two fractures. Our results showed almost identical mortality rates at 30 days, 6 months, and 1 year after surgery. The similarity in mortality rates between distal and proximal femur fractures reported in the literature and found in our study suggests metaphyseal fractures of the femur have a similar impact on patient survival. Whether this is true for other metaphyseal fractures of the lower extremity needs to be evaluated in future studies. Although fractures of the proximal and distal tibia may be regarded as posing a lower physiologic burden on the patient than fractures of the hip or distal femur, the effect of functional limitations leading to decreased ambulation may be sufficient to impact patient mortality.
An interesting finding was the presence of a greater BMI in patients with distal femur fractures. Among several factors, decreased body mass has been determined to increase the risk for hip fractures. This has in part been attributed to the fact that decreased adipose tissue surrounding the trochanteric area leads to increased energy dissipation in the soft tissues during a fall. In patients with increased adipose tissue, as our results suggest, the proximal femur therefore may be protected from injury, transposing fracture energy to the distal femur.
Fractures of the distal femur carry a mortality risk comparable to that of hip fractures. Patients with periprosthetic fractures and those with dementia, heart failure, advanced renal disease, and metastasis have shorter survival, which may be predicted with the age-adjusted CCI. Although data for surgical delay are inconclusive, results suggest a delay greater than 4 days after admission increases the risk of 6-month and 1-year mortality. A multidisciplinary approach to address patient comorbidities and allow for timely surgery therefore may be indicated in this patient population, as advocated for patients with hip fractures. Additional studies are required to evaluate whether other metaphyseal and intraarticular fractures of the lower extremity have a similar effect on mortality.
Acknowledgments
We thank Angel Brandt for invaluable help in obtaining study approval and supporting data management.
Footnotes
One or more of the authors have received funding from an educational and research grant from Smith and Nephew (Memphis, TN) (PNS, WMR, AW, MJG), AO North America (Paoli, PA) (PNS, WMR, AW, MJG), Synthes, Inc (Paoli, PA) (PNS, WMR, AW, MJG), and Foundation of Orthopaedic Trauma (PNS, WMR, AW, MJG).
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Arneson TJ, Melton LJ, 3rd, Lewallen DG, O’Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965–1984. Clin Orthop Relat Res. 1988;234:188–194. [PubMed] [Google Scholar]
- 2.Baker DM. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1997;79:470. [PubMed] [Google Scholar]
- 3.Beringer TR. Mortality and morbidity after hip fractures. BMJ. 1994;308:343. doi: 10.1136/bmj.308.6924.343b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhattacharyya T, Chang D, Meigs JB, Estok DM, 2nd, Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007;89:2658–2662. doi: 10.2106/JBJS.F.01538. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharyya T, Iorio R, Healy WL. Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am. 2002;84:562–572. doi: 10.2106/00004623-200204000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Bolhofner BR, Carmen B, Clifford P. The results of open reduction and Internal fixation of distal femur fractures using a biologic (indirect) reduction technique. J Orthop Trauma. 1996;10:372–377. doi: 10.1097/00005131-199608000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006;332:947–951. doi: 10.1136/bmj.38790.468519.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boyd AD, Jr, Wilber JH. Patterns and complications of femur fractures below the hip in patients over 65 years of age. J Orthop Trauma. 1992;6:167–174. doi: 10.1097/00005131-199206000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Butt MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in elderly patients: operative versus non-operative treatment. J Bone Joint Surg Br. 1996;78:110–114. [PubMed] [Google Scholar]
- 10.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 11.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 12.Christodoulou A, Terzidis I, Ploumis A, Metsovitis S, Koukoulidis A, Toptsis C. Supracondylar femoral fractures in elderly patients treated with the dynamic condylar screw and the retrograde intramedullary nail: a comparative study of the two methods. Arch Orthop Trauma Surg. 2005;125:73–79. doi: 10.1007/s00402-004-0771-5. [DOI] [PubMed] [Google Scholar]
- 13.Clayer MT, Bauze RJ. Morbidity and mortality following fractures of the femoral neck and trochanteric region: analysis of risk factors. J Trauma. 1989;29:1673–1678. doi: 10.1097/00005373-198912000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res. 2004;425:64–71. doi: 10.1097/01.blo.0000132406.37763.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cowper DC, Kubal JD, Maynard C, Hynes DM. A primer and comparative review of major US mortality databases. Ann Epidemiol. 2002;12:462–468. doi: 10.1016/S1047-2797(01)00285-X. [DOI] [PubMed] [Google Scholar]
- 16.Deakin DE, Boulton C, Moran CG. Mortality and causes of death among patients with isolated limb and pelvic fractures. Injury. 2007;38:312–317. doi: 10.1016/j.injury.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 18.Dunlop DG, Brenkel IJ. The supracondylar intramedullary nail in elderly patients with distal femoral fractures. Injury. 1999;30:475–484. doi: 10.1016/S0020-1383(99)00136-9. [DOI] [PubMed] [Google Scholar]
- 19.Elliott J, Beringer T, Kee F, Marsh D, Willis C, Stevenson M. Predicting survival after treatment for fracture of the proximal femur and the effect of delays to surgery. J Clin Epidemiol. 2003;56:788–795. doi: 10.1016/S0895-4356(03)00129-X. [DOI] [PubMed] [Google Scholar]
- 20.Fillenbaum GG, Burchett BM, Blazer DG. Identifying a national death index match. Am J Epidemiol. 2009;170:515–518. doi: 10.1093/aje/kwp155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Franzo A, Francescutti C, Simon G. Risk factors correlated with post-operative mortality for hip fracture surgery in the elderly: a population-based approach. Eur J Epidemiol. 2005;20:985–991. doi: 10.1007/s10654-005-4280-9. [DOI] [PubMed] [Google Scholar]
- 22.Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004;124:334–340. doi: 10.1007/s00402-004-0662-9. [DOI] [PubMed] [Google Scholar]
- 23.Giles JB, DeLee JC, Heckman JD, Keever JE. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am. 1982;64:864–870. [PubMed] [Google Scholar]
- 24.Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112:702–709. doi: 10.1016/S0002-9343(02)01119-1. [DOI] [PubMed] [Google Scholar]
- 25.Gustilo RB, Gruninger RP, Davis T. Classification of type III (severe) open fractures relative to treatment and results. Orthopedics. 1987;10:1781–1788. [PubMed] [Google Scholar]
- 26.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Haidukewych G, Sems SA, Huebner D, Horwitz D, Levy B. Results of polyaxial locked-plate fixation of periarticular fractures of the knee. J Bone Joint Surg Am. 2007;89:614–620. doi: 10.2106/JBJS.F.00510. [DOI] [PubMed] [Google Scholar]
- 28.Henry SL. Supracondylar femur fractures treated percutaneously. Clin Orthop Relat Res. 2000;375:51–59. doi: 10.1097/00003086-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18:509–520. doi: 10.1097/00005131-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Majumdar SR, Beaupre LA, Johnston DW, Dick DA, Cinats JG, Jiang HX. Lack of association between mortality and timing of surgical fixation in elderly patients with hip fracture: results of a retrospective population-based cohort study. Med Care. 2006;44:552–559. doi: 10.1097/01.mlr.0000215812.13720.2e. [DOI] [PubMed] [Google Scholar]
- 31.Markmiller M, Konrad G, Sudkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res. 2004;426:252–257. doi: 10.1097/01.blo.0000141935.86481.ba. [DOI] [PubMed] [Google Scholar]
- 32.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 33.Martinet O, Cordey J, Harder Y, Maier A, Buhler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury. 2000;31(suppl 3):C62–C63. doi: 10.1016/S0020-1383(00)80034-0. [DOI] [PubMed] [Google Scholar]
- 34.McGuire KJ, Bernstein J, Polsky D, Silber JH. The 2004 Marshall Urist Award: Delays until surgery after hip fracture increases mortality. Clin Orthop Relat Res. 2004;428:294–301. doi: 10.1097/01.blo.0000146743.28925.1c. [DOI] [PubMed] [Google Scholar]
- 35.Melton LJ, 3rd, Crowson CS, O’Fallon WM. Fracture incidence in Olmsted County, Minnesota: comparison of urban with rural rates and changes in urban rates over time. Osteoporos Int. 1999;9:29–37. doi: 10.1007/s001980050113. [DOI] [PubMed] [Google Scholar]
- 36.Nieves JW, Bilezikian JP, Lane JM, Einhorn TA, Wang Y, Steinbuch M, Cosman F. Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int. 2010;21:399–408. doi: 10.1007/s00198-009-0962-6. [DOI] [PubMed] [Google Scholar]
- 37.Novack V, Jotkowitz A, Etzion O, Porath A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19:170–176. doi: 10.1093/intqhc/mzm003. [DOI] [PubMed] [Google Scholar]
- 38.Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma. 2006;20:190–196. doi: 10.1097/00005131-200603000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schutz M, Muller M, Krettek C, Hontzsch D, Regazzoni P, Ganz R, Haas N. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001;32(suppl 3):SC48–SC54. [DOI] [PubMed]
- 41.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–154. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 42.Shih J. Shih/SIZE. 2009. Johns Hopkins School of Public Health. Available at: http://cct.jhsph.edu/javamarc/Shih/powerpropv2.htm. Accessed December 2, 2009.
- 43.Social Security Death Index. 2009. Social Security Administration. Available at: http://ssdi.rootsweb.ancestry.com. Accessed October 10, 2009.
- 44.Streubel PN, Gardner MJ, Morshed S, Collinge CA, Gallagher B, Ricci WM. Are extreme distal periprosthetic supracondylar fractures of the femur too distal to fix using a lateral locked plate? J Bone Joint Surg Br. 2010;92:527–534. doi: 10.1302/0301-620X.92B3.22996. [DOI] [PubMed] [Google Scholar]
- 45.Streubel PN, Gardner MJ, Ricci WM. Intracapsular femoral neck fractures in elderly patients. Minerva Ortop Traumatol. 2009;60:541–554. [Google Scholar]
- 46.Streubel PN, Ricci WM, Gardner MJ. Fragility fractures: preoperative, perioperative, and postoperative management. Curr Orthop Pract. 2009;20:482–489. doi: 10.1097/BCO.0b013e3181b3a384. [DOI] [Google Scholar]
- 47.Sund R, Liski A. Quality effects of operative delay on mortality in hip fracture treatment. Qual Saf Health Care. 2005;14:371–377. doi: 10.1136/qshc.2004.012831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomson AB, Driver R, Kregor PJ, Obremskey WT. Long-term functional outcomes after intra-articular distal femur fractures: ORIF versus retrograde intramedullary nailing. Orthopedics. 2008;31:748–750. doi: 10.3928/01477447-20080801-33. [DOI] [PubMed] [Google Scholar]
- 49.Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005) J Orthop Trauma. 2006;20:366–371. doi: 10.1097/00005131-200605000-00013. [DOI] [PubMed] [Google Scholar]
- 50.Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77:1551–1556. doi: 10.2106/00004623-199510000-00010. [DOI] [PubMed] [Google Scholar]