Abstract
Background
Legg-Calvé-Perthes disease (LCPD) was described a century ago. In previous long-term reports of patients with LCPD, nonoperative treatment varied considerably. The likelihood of hip osteoarthritis (OA) developing in patients with LCPD and possible need for THA are not well defined.
Questions/purposes
The purpose of the study was to determine whether nonoperatively treated patients with LCPD (1) had an increased prevalence of THA compared with gender- and age-matched control subjects, (2) if patients with Stulberg Classes III/IV/V femoral heads had an increased risk of THA compared with those with Classes I/II femoral heads. Given the limitation in the study, we (3) evaluated whether patients with LCPD were at risk for having radiographic hip OA more commonly than control subjects and (4) whether hips with Classes III/IV/V femoral heads had an increased prevalence of OA compared with hips with Classes I/II femoral heads.
Patients and Methods
The study population consisted of 167 patients with LCPD treated with a Thomas splint. The control population consisted of gender- and age-matched control subjects who were participants in the Copenhagen City Heart Study: the Osteoarthritis Substudy. Radiographs at skeletal maturity were classified according to the classification system of Stulberg et al. Data from the Danish Hip Arthroplasty Register and the Registries of the National Board of Health were collected to obtain the number of patients with LCPD having THA. At a mean followup of 47 years later (range, 37–58 years), weightbearing pelvic radiographs were obtained. Radiographic OA was defined as a joint space width of 2.0 mm or less.
Results
Thirteen percent of patients with LCPD had THAs compared with none in the control group. Seven percent of the patients with LCPD had OA compared with 1% in the control group. The prevalence of THA and OA was increased in hips with Classes III/IV/V femoral heads compared with hips with Classes I/II femoral heads.
Conclusions
Patients with LCPD have an increased risk of having THA compared with a gender- and age-matched control group. Our data suggest that patients with LCPD have a greater risk of having radiographic OA develop than a gender- and age-matched control group. It seems that patients with Classes III/IV/V femoral heads have an increased risk of THA and OA compared with patients with Classes I/II femoral heads.
Level of Evidence
Level III, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Numerous studies [2, 5, 6, 10, 12, 14–16, 18, 20, 21] have focused on the need for THA and long-term risk for having hip OA develop in nonoperatively treated patients with LCPD. Earlier studies are retrospective without any control group. In addition, the treatments have been combinations of several treatments such as: bed rest [6, 12, 14–16, 18, 20], traction [5, 12, 15], abduction splints [15, 18], plaster [15], spica casting with [2, 5, 6, 10, 16, 18] and without [2, 5, 6] weightbearing, Thomas splint [20, 21], shoe elevation on the normal side [16, 20], crutches [10, 16, 20], wheelchair [10], or no treatment [2, 21]. In contrast, we evaluated one treatment method, namely, use of a Thomas splint.
One major problem for the patients with LCPD in the long-term is development of hip pain and OA that might result in the need for a THA. Earlier studies have shown an overall prevalence of OA between 5% and 100% [2, 5, 6, 10, 12, 14, 16, 20, 21], and a prevalence of THA ranging from 0% to 24% [2, 5, 6, 10, 12, 14–16, 18, 20, 21] (Table 1).
Table 1.
Previous studies of patients with LCPD who were treated conservatively
| Study | Followup (years) | Prevalence of THA | Definition of radiographic OA | Prevalence of OA |
|---|---|---|---|---|
| Gower and Johnston [2] | 36 | 3/36 hips (8%) | Not specified | 23/30 (77%) |
| Ippolito et al. [5] | 27 | 1/11 (9%) | Sclerosis, JSW narrowing, osteophytes | 10/10 (100%) |
| Ippolito et al. [6] | 25 | 0/61 (0%) | Sclerosis, JSW narrowing, osteophytes, cysts | Stulberg Class I: 0/8 (0%) Stulberg Class II: 0/17 (0%) Stulberg Class III: 9/25 (37%) Stulberg Class IV: 7/10 (70%) Stulberg Class V: 1/1 (100%) |
| Kelly et al. [10] | 22 | 2/80 (3%) | Not specified | 4/80 (5%) |
| Lecuire [12] | 50 | 12/51 hips (24%) | Not specified | 7/32 hips (22%) |
| Perpich et al. [14] | 29 | 3/38 (8%) | JSW less than 2 mm compared with other hip | 3/41 hips (7%) |
| Rush [15] | 26 | 0/35 (0%) | Not specified | Not specified |
| Stulberg et al. [16] | 40 | 0/171 (0%) | Sclerosis, JSW narrowing, osteophytes, cysts | Stulberg Class I: 0/20 (0%) Stulberg Class II: 2/30 (7%) Stulberg Class III: 10/28 (36%) Stulberg Class IV: 28/42 (67%) Stulberg Class V: 26/32 (81%) |
| Templeton and Green [18] | 32 | 0/37 (0%) | Not specified | Not specified |
| Yrjönen [20] | 35 | 0/19 (0%) | Not specified | 12/19 hips (63%) |
| Yrjönen et al. [21] | 35 | 5/106 (5%) | Sclerosis, JSW narrowing, osteophytes, cysts | 51/106 (48%) |
Because of the wide variation reported in the literature, we determined whether nonoperatively treated patients with LCPD: (1) had an increased prevalence of THA compared with gender- and age-matched control subjects, and (2) if patients with Stulberg Classes III/IV/V femoral heads had an increased risk of THA compared with patients with Classes I/II femoral heads. Given the limitations of the study, we (3) evaluated whether patients with LCPD were at risk for having radiographic hip OA develop more commonly than control subjects, and (4) whether hips with Classes III/IV/V femoral heads had an increased prevalence of OA compared with hips with Classes I/II femoral heads.
Patients and Methods
This retrospective case-control study consists of a cohort of 167 patients (191 hips) with LCPD referred to The Community of Disabled in Kolding, Denmark from 1941 to 1962. One hundred forty-three patients had unilateral and 24 patients had bilateral involvement. All patients were treated by a Thomas splint regardless of gender, age at onset of the disease, and severity of disease. The Thomas splint is regarded as a noncontainment treatment and reportedly reduces load on the hip [11]. The splint was used from the time of diagnosis until the reconstitution stage of the disease appeared on the radiographs, a mean of 25 ± 9 months (range, 9–38 months). The splint was worn all day except when swimming and bathing. None of the patients had surgery during their childhood or were referred to other hospitals. The patient’s gender, age at onset, and duration of treatment with a Thomas splint were obtained from the medical records. Onset of disease was defined as the onset of limping or complaints of pain in the hip, thigh, or knee.
At skeletal maturity, supine AP and frog-leg lateral radiographs of the pelvis were taken. We defined skeletal maturity as the point when closure of the triradiate cartilage and the femoral head physis had occurred. One of the authors not involved in the treatment of the patients (LF) classified the radiographs according to the classification system of Stulberg et al. as reported by Herring et al.: Classes I and II hips have a spherical femoral head, a Class III hip has an ovoid head, and Classes IV and V hips have a flattened femoral head [3]. The advantages of the classification included the simplicity of application and reliability with interobserver and intraobserver agreement reflected by weighted kappa values of 0.79 and 0.88, respectively [3]. We combined Classes I and II as hips in these classes were considered not to be disposed to having OA develop and Classes III, IV, and V as these hips were considered to have an increased risk of having OA develop in adulthood, as reported in two studies [4, 16].
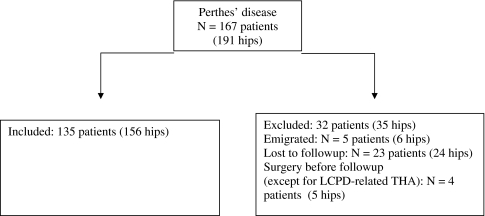
Except for patients who were deceased, who had emigrated, or were lost to followup owing to lack of a civil registration number, all patients were invited to a followup in 2005–2006, and 111 accepted. For the 111 patients with LCPD, weightbearing standardized AP pelvic radiographs were obtained with a tube to film distance of 100 cm. Joint space width (JSW) was measured on AP pelvis radiographs (Fig. 1) by using a 0.1-mm graded magnifying glass (Haff, Pfronten, Germany). Hip OA was defined as a JSW of 2.0 mm or less regardless of the presence of osteophytes, subchondral sclerosis, or subchondral cysts [8]. One observer (LF) performed all measurements.
Fig. 1.
Measurement of minimal JSW was performed perpendicular to the femoral head surface by determining the femoral head center using a best-fit circle and drawing lines from the center to the acetabular weightbearing surface. The JSW from the femoral head surface to the acetabulum was measured at three sites chosen where the smallest distance visual was present and not on predefined locations, as the caput and acetabulum in some patients were incongruent. The JSW used for statistical analysis was the smallest of the measurements.
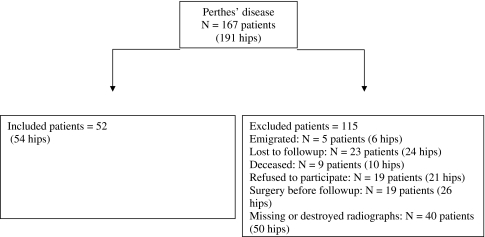
We examined the data for 156 of the 191 hips to determine the risk for having a THA. Thirty-two patients (35 hips) were excluded: five (six hips) owing to emigration, 23 (24 hips) were lost to followup, and four (five hips) had surgery in the pelvis or leg, not related to LCPD, before followup (Fig. 2). We were able to include deceased patients and patients who did not want to participate at followup in this part of the study, because data from the national Danish Hip Arthroplasty Register and the Registries of the National Board of Health were collected. Patients participating were asked whether they had a THA. In this part of the study, unilateral disease was present in 114 hips (73%) and bilateral disease in 42 hips (27%). There were 109 male patients (125 hips, 80%) and 26 female patients (31 hips, 20%) included in the study. Age at onset of disease was 6 ± 2 years and the Thomas splint was used for 25 ± 9 months. Of the 156 hips included, 57 (37%) were classified as having Classes I/II femoral heads, 26 (17%) had Classes III/IV/V femoral heads, and 73 (46%) were not classified owing to destroyed or missing radiographs. The classified hips did not differ regarding the patients’ gender, age at onset, and duration of the Thomas splint compared with hips that were not classified (Table 2).
Fig. 2.
A flowchart shows the patients eligible for evaluation of THA.
Table 2.
Demographic data of hips with and without a Stulberg classification in the THA study
| Parameter | Stulberg Classes I/II (n = 57 hips) | Stulberg Classes III/IV/V (n = 26 hips) | Without Stulberg classification (n = 73 hips) | p Value for difference between patients classified and not classified |
|---|---|---|---|---|
| Ratio male:female | 4:1 | 3:1 | 4:1 | 0.42 |
| Age at onset/years | 6 ± 2 | 6 ± 3 | 6 ± 2 | 0.21 |
| Duration of Thomas splint/months | 25 ± 6 | 25 ± 9 | 25 ± 12 | 0.89 |
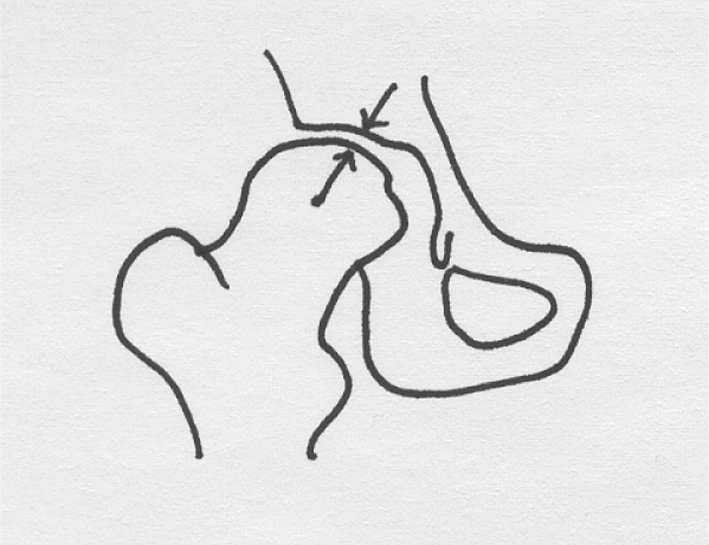
To assess the prevalence of radiographic hip OA, 52 (54 hips) of the 167 patients (191 hips) were included. One hundred fifteen patients (137 hips) were excluded owing to emigration (five patients, six hips), lost to followup (23 patients, 24 hips), deceased (nine patients, 10 hips), refused to participate (19 patients, 21 hips), surgery in the pelvis or lower limb before followup (19 patients, 26 hips), or missing or destroyed radiographs (40 patients, 50 hips) (Fig. 3). For this part of the study unilateral disease was present in 50 hips (93%) and bilateral disease in four (7%). There were 44 male patients (46 hips, 85%) and eight female patients (eight hips, 15%). Age at onset was 6 ± 2 years. The Thomas splint was used for 25 ± 7 months. Of 54 hips, 42 (78%) had Classes I/II femoral heads (Table 3). We observed no differences between hips with Classes I/II femoral heads and those with Classes III/IV/V femoral heads regarding gender, age at onset, and duration of time the Thomas splint was used (Table 3). Age at followup was 52 ± 4 years for males and 54 ± 5 years for females. Time from onset of disease until followup was 47 ± 5 years.
Fig. 3.
A flowchart shows the patients eligible for evaluation of hip OA.
Table 3.
Demographic data for hips with Stulberg Classes I/II and Classes III/IV/V femoral heads in the OA study
| Parameter | Stulberg Classes I/II (n = 42 hips) | Stulberg Classes III/IV/V (n = 12 hips) | p Value |
|---|---|---|---|
| Ratio male:female | 7:1 | 3:1 | 0.40 |
| Age at onset/years | 6 ± 2 | 6 ± 2 | 0.75 |
| Duration of Thomas splint/months | 25 ± 7 | 24 ± 6 | 0.77 |
The prevalence of THA and radiographic OA was evaluated in a gender- and age-matched control group who were participants of The Copenhagen City Heart Study; Osteoarthritis Substudy [7]. The ratio of patients with LCPD to control subjects was 1:2. Radiographs for the control group were obtained with the patients standing and standardized with a tube to film distance of 120 cm. The difference between tube to film distances in the study and control groups was taken into consideration when measuring JSW.
Normality tests, by probit plots, showed all data were normally distributed. Thus, data are presented as means ± standard deviation. The relationships between hip OA and THA in patients with LCPD and a gender- and age-matched control group were evaluated by exact logistic regression analysis. Odds ratio (OR) exact test was performed to assess interrelationship between class and THA and radiographic hip OA. The T-test was used to evaluate differences between demographic data. All statistical analyses were performed with the STATA® Version 10.0 statistical software (StataCorp LP, College Station, TX, USA).
Results
The risk of THA was increased from none of 312 hips (0%) in the gender- and age-matched control group compared with 20 of 156 hips (13%) in the patients with LCPD (p < 0.001; OR = 49.0; CI = 8.2 – infinity) (Table 4). None of the patients who emigrated had a THA performed in Denmark. Whether they had a THA performed outside Denmark is unknown.
Table 4.
Number of hips having THA in patients with LCPD and for gender- and age-matched control group
| Parameter | THA | No THA |
|---|---|---|
| LCPD group | ||
| Stulberg Classes I/II (n = 57) | 5 (9%) | 52 (91%) |
| Stulberg Classes III/IV/V (n = 26) | 7 (27%) | 19 (73%) |
| Unknown Stulberg class (n = 73) | 8 (11%) | 65 (89%) |
| Gender- and age-matched control group (n = 312) | 0 (0%) | 312 (100%) |
The risk of THA was increased from five of 57 hips (9%) with Classes I/II femoral heads to seven of 26 hips (27%) with Classes III/IV/V femoral heads (p = 0.04; OR = 3.8; CI = 1.1–12.9) (Table 4).
The risk of radiographic OA was increased from one of 108 hips (1%) in the gender- and age-matched control group to four of 54 hips (7%) in the patients with LCPD (p = 0.04; OR = 8.5; confidence interval [CI] = 1.8–428.8) (Table 5).
Table 5.
Number of hips with or without hip OA in the LCPD group and the gender- and age-matched control group
| Group | Number of hips with OA | Number of hips without OA |
|---|---|---|
| LCPD group | ||
| Stulberg Classes I/II (n = 42) | 1 (2%) | 41 (98%) |
| Stulberg Classes III/IV/V (n = 12) | 3 (25%) | 9 (75%) |
| Control group (n = 108) | 1 (1%) | 107 (99%) |
OA was present when the joint space width was 2.0 mm or less regardless of other features of OA; OA = osteoarthritis; LCPD = Legg-Calvé-Perthes disease.
The risk of radiographic OA was increased from one of 42 hips (2%) with Classes I/II femoral heads compared with three of 12 hips with Classes III/ IV/V femoral heads (p = 0.03; OR = 13.7; CI = 1.9–97.1) (Table 5).
Discussion
The long-term problems for patients with LCPD are the risk for having hip pain and OA develop and the subsequent need for a THA. In previous reports [2, 5, 6, 10, 12, 14–16, 18, 20, 21], treatment of the patients and definition of OA varied considerably (Table 1), and the prevalence of THA and OA in a gender- and age-matched population have not been taken into account. The current case-control study determined whether nonoperatively treated patients with LCPD (1) had an increased prevalence of THA compared with gender- and age-matched control subjects, and (2) if patients with Stulberg Classes III/IV/V femoral heads had an increased risk of THA compared with patients with Classes I/II femoral heads. Given the limitations of the study, we evaluated (3) whether patients with LCPD have radiographic hip OA develop more commonly than control subjects, and (4) whether hips with Classes III/IV/V femoral heads had an increased prevalence of OA compared with hips with Classes I/II femoral heads.
There are limitations to our study. First, the study is based on AP radiographic findings, and the clinical status of the patients was not evaluated. We used only AP radiographic findings as a lateral view was not obtained for the control subjects. Second, our study comprises a small number of patients. Owing to different inclusion criteria, 156 of 191 hips (82%) were included in the THA study (Fig. 2) and 54 of 191 hips (28%) were included in the OA study (Fig. 3). Third, owing to inadequate or destroyed radiographs, it was possible to classify only 83 of the 156 (53%) hips in the THA study. Third, OA was defined as JSW narrowing regardless of the presence of osteophytes, sclerosis, and cysts. One study showed a substantial association between a reduced JSW and self-reported hip pain [9]. We used a reduced JSW of 2.0 mm or less as a specific definition of radiographic OA as it has been associated with self-reported hip pain and has an acceptable intrarater reliability (intraclass correlation coefficients, 0.87–0.91) [9]. This is in contrast to Dieppe et al. [1], who found no correlation between pain, stiffness and physical function, and radiographic severity evaluated by the Kellgren and Lawrence radiographic score. This might be explained by differences in clinical and radiographic evaluations of the patients. Sun et al. [17] found that interrater reliability of JSW narrowing showed a high reliability compared with other radiographic features of OA (Kappa, 0.70–0.79). In contrast, the interrater reliability of the Kellgren and Lawrence score has a lower kappa value (0.50). Fourth, although we expended much effort trying to find the patients and obtain radiographs, some patients had emigrated, some were deceased, and others did not want to participate or were lost to followup owing to lack of a civil registration number; other patients were located but did not keep followup appointments. The current study is comprised of patients with a followup of nearly 50 years. We were able to trace 144 patients (167 of 191 hips, 87%) registered in our archives who were diagnosed with LCPD from 1941 to 1962, and in contrast to other studies [2, 5, 6, 10, 12, 14–16, 18, 20, 21], all children had the same weight-relieving noncontainment treatment in their childhood regardless of gender, age at onset, degree of femoral head involvement, and unilateral or bilateral involvement. We were able to include 156 of 191 (82%) hips in the THA study, as the patients could be found in the Danish Hip Arthroplasty Register and The Register of the National Board of Health. In the OA study, 54 of 191 hips (28%) were included; therefore, the risk of misinterpretation of the results in this part of the study should be taken into account.
We do not believe any patients were missed at followup in this part of the study owing to insufficient or incorrect registration. The Danish Hip Arthroplasty Register has existed since 1995 and has a 94.1% complete rate for registration for primary THA [13]. In The Register of the National Board of Health, every operation performed in Denmark has been recorded under a unique personal civil registration number since 1977 [19]. The civil registration number is used in every contact with the public system in Denmark and follows each individual his/her entire life and after death. Fifth, it was possible to classify only 83 of the 156 (53%) hips in the THA study. However, we have no reason to believe that hips with and without a classification were biased as no difference was found regarding gender, age at onset, and duration of use of the Thomas splint. For assessment of radiographic OA, 137 of 191 hips (72%) were excluded. However, except for patients excluded owing to surgery before followup (19 patients, 26 hips), we have no reason to believe that the excluded and included patients differed. Of the surgically treated hips, 20 had LCPD-related THA. Finally, no preoperative radiographs were available for 17 hips, and in three hips with preoperative radiographs, the JSW observed on AP radiographs of the pelvis was greater than 2.0 mm, and according to our definition, without OA. In the OA study, 42 of 54 hips (78%) were classified as having Classes I/II femoral heads, which is a high percentage compared with the study of Herring et al. [4]. This difference might be attributable to patients in our study who were excluded owing to THA; these patients were more likely to have Classes III/IV/V femoral heads, as shown in the Results section.
The prevalence of THA was 13% in patients in the current study compared with 0% to 24% reported in previous studies [2, 5, 12, 14, 20]. The studies have mean followups ranging from 28 to 50 years, which might explain the difference (Table 1). For 83 of 156 hips (53%) with a Stulberg et al. [16] classification, the risk of having THA was increased threefold for hips with Classes III/IV/V femoral heads compared with hips with Classes I/II femoral heads, which is in accordance with the increased risk of radiographic OA resulting from the disease [6, 16].
The overall prevalence of OA for patients in the current study was 7%. This is lower compared with some other studies [2, 5, 6, 12, 15, 16, 20, 21], and might be attributable to the difference in the definition of OA (Table 1). Perpich et al. [14] defined OA as JSW narrowing less than 2.0 mm compared with the other hip. The prevalence of OA in their patients was 8% which is in concordance with our results.
Given the limitations, our data suggest that patients with Classes III/IV/V femoral heads were more likely to have radiographic OA develop than patients with Classes I/II femoral heads. The prevalence of OA in patients in the current study was 2% for those with Classes I/II femoral heads and 25% for those with Classes III/IV/V femoral heads. In contrast, Stulberg et al. [16] reported that 3% of patients with Classes I/II femoral heads and 63% of patients with Classes III/IV/V femoral heads had radiographic signs of OA develop 40 years after onset of disease (Table 1). In the study by Ippolito et al. [6], the prevalence of OA after 25 years was 0% for patients with Classes I/II femoral heads and 47% for those with Classes III/IV/V femoral heads (Table 1). In both studies, OA was defined as either narrowing of the JSW, presence of osteophytes, subchondral sclerosis, or subchondral cysts, which might explain the differences between those studies [6, 16] and our study. Patients with LCPD have an increased risk of having THA compared with a gender- and age-matched control group. Our data suggest that patients with LCPD have a greater risk of having radiographic OA develop than a gender- and age-matched control group. It seems that patients with Classes III/IV/V femoral heads have an increased risk of THA and OA compared with patients with Classes I/II femoral heads.
Acknowledgments
We thank Stig Sonne-Holm MD, PhD, and Steffen Jacobsen MD, PhD, from the Department of Orthopaedic Surgery, Copenhagen University Hospital, Hvidovre Hospital, Copenhagen, for permission to study radiographs of patients from The Copenhagen City Heart Study; Osteoarthritis Substudy. Lars Korsholm PhD, Institute of Public Health, was helpful with the statistical work.
Footnotes
One of the authors (LF) has received funding from the Research Board of Kolding Hospitals, Denmark. The funding did not play a role in the investigation.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Kolding Hospital, Denmark and Odense University Hospital, Denmark.
References
- 1.Dieppe P, Judge A, Williams S, Ikwueke I, Guenther KP, Floeren M, Huber J, Ingvarsson T, Learmonth I, Lohmander LS, Nilsdotter A, Puhl W, Rowley D, Thieler R, Dreinhoefer K, EUROHIP Study Group Variations in the pre-operative status of patients coming to primary hip replacement for osteoarthritis in European orthopaedic centres. BMC Musculoskelet Disord. 2009;10:19. doi: 10.1186/1471-2474-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gower WE, Johnston RC. Legg-Perthes disease: long-term follow-up of thirty-six patients. J Bone Joint Surg Am. 1971;53:759–768. [PubMed] [Google Scholar]
- 3.Herring JA, Kim HT, Browne R. Legg-Calvé-Perthes disease. Part I: Classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004;86:2103–2120. [PubMed] [Google Scholar]
- 4.Herring JA, Kim HT, Browne R. Legg-Calvé-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86:2121–2134. [PubMed] [Google Scholar]
- 5.Ippolito E, Tudisco C, Farsetti P. Long-term prognosis of Legg-Calvé-Perthes disease developing during adolescence. J Pediatr Orthop. 1985;5:652–656. doi: 10.1097/01241398-198511000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Ippolito E, Tudisco C, Farsetti P. The long-term prognosis of unilateral Perthes’ disease. J Bone Joint Surg Br. 1987;69:243–250. doi: 10.1302/0301-620X.69B2.3818755. [DOI] [PubMed] [Google Scholar]
- 7.Jacobsen S. Adult hip dysplasia and osteoarthritis: studies in radiology and clinical epidemiology. Acta Orthop Suppl. 2006;77:1–37. doi: 10.1080/17453670610045614. [DOI] [PubMed] [Google Scholar]
- 8.Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B. Radiographic case definitions and prevalence of osteoarthrosis of the hip: a survey of 4151 subjects in the Osteoarthritis Substudy of the Copenhagen City Heart Study. Acta Orthop Scand. 2004;75:713–720. doi: 10.1080/00016470410004085. [DOI] [PubMed] [Google Scholar]
- 9.Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. The relationship of hip joint space to self reported hip pain: a survey of 4.151 subjects of the Copenhagen City Heart Study: the Osteoarthritis Substudy. Osteoarthritis Cartilage. 2004;12:692–697. doi: 10.1016/j.joca.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 10.Kelly FB, Jr, Canale ST, Jones RR. Legg-Calvé-Perthes disease: long-term evaluation of non-containment treatment. J Bone Joint Surg Am. 1980;62:400–407. [PubMed] [Google Scholar]
- 11.Kohn D, Wirth CJ, John H. The function of the Thomas splint: an experimental study. Arch Orthop Trauma Surg. 1991;111:26–28. doi: 10.1007/BF00390188. [DOI] [PubMed] [Google Scholar]
- 12.Lecuire F. The long-term outcome of primary osteochondritis of the hip (Legg-Calvé-Perthes disease) J Bone Joint Surg Br. 2002;84:636–640. doi: 10.1302/0301-620X.84B5.12124. [DOI] [PubMed] [Google Scholar]
- 13.Pedersen AB, Johnsen S, Overgaard S, Søballe K, Sørensen HT, Lucht U. Registration in the Danish Hip Arthroplasty Registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications. Acta Orthop Scand. 2004;75:434–441. doi: 10.1080/00016470410001213-1. [DOI] [PubMed] [Google Scholar]
- 14.Perpich M, McBeath A, Kruse D. Long-term follow-up of Perthes disease treated with spica casts. J Pediatr Orthop. 1983;3:160–165. doi: 10.1097/01241398-198305000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Rush J. Perthes’ disease: a long-term follow-up of cases treated by prolonged recumbency. Aust N Z J Surg. 1973;43:261–265. doi: 10.1111/j.1445-2197.1973.tb05698.x. [DOI] [PubMed] [Google Scholar]
- 16.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 17.Sun Y, Günther KP, Brenner H. Reliability of radiographic grading of osteoarthritis of the hip and knee. Scand J Rheumatol. 1997;26:155–165. doi: 10.3109/03009749709065675. [DOI] [PubMed] [Google Scholar]
- 18.Templeton J, Green AD. Perthes’ disease: a long-term follow-up. Ulster Med J. 1983;52:125–130. [PMC free article] [PubMed] [Google Scholar]
- 19.The Register of the National Board of Health. Available at: http://www.sst.dk/Indberetning%20og%20statistik/Landspatientregisteret.aspx. Accessed August 17, 2009.
- 20.Yrjönen T. Prognosis in Perthes’ disease after noncontainment treatment: 106 hips followed for 28–47 years. Acta Orthop Scand. 1992;63:523–526. doi: 10.3109/17453679209154728. [DOI] [PubMed] [Google Scholar]
- 21.Yrjönen T, Poussa M, Hoikka V, Österman K. Poor prognosis in atypical Perthes’ disease: radiographic analysis of 19 hips after 35 years. Acta Orthop Scand. 1992;63:399–402. doi: 10.3109/17453679209154753. [DOI] [PubMed] [Google Scholar]