Abstract
Background
The best location for biceps tenodesis is controversial as surgeons have begun to question whether tenodesis location affects the incidence of residual bicipital postoperative pain. An open distal tenodesis technique has been previously proposed to eliminate remaining symptoms at the bicipital groove.
Questions/purposes
We asked the following questions: (1) Does a higher tenodesis in the biceps groove result in postoperative pain? And (2) can the tenodesis location be successfully moved more distally (“suprapectoral tenodesis”) by an arthroscopic technique?
Methods
We retrospectively reviewed 17 patients undergoing arthroscopic biceps tenodesis and evaluated their tenodesis location, either within the upper half of the groove (five) or in the lower half of the groove or shaft (12). Patient outcomes were assessed with visual analog scale scores for pain, American Shoulder and Elbow Surgeons scores, and Constant-Murley scores. Minimum followup was 12 months (mean, 28 months; range, 12–69 months).
Results
Two patients had persistent pain at 12 months; both had a tenodesis in the upper half of the groove. The overall American Shoulder and Elbow Surgeons and Constant-Murley scores were improved at latest followup.
Conclusions
Arthroscopic suprapectoral biceps tenodesis represents a new technique for distal tenodesis. Our preliminary observations suggest a more distal tenodesis location may decrease the incidence of persistent postoperative pain at the bicipital groove, although additional research is needed to definitively state whether the proximal location is in fact more painful.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Surgery for painful disease of the long head of the biceps (LHB) may be addressed by tenotomy or tenodesis. Tenotomy of the biceps tendon provides pain relief and patient satisfaction has been shown with this procedure [24]. Although outcomes of tenotomy are reportedly similar to those for tenodesis [11], muscle belly retraction (the Popeye sign) is more common with tenotomy [4, 25], making it less preferable in patients concerned about the cosmetic appearance of the arm. Tenodesis of the biceps tendon is advocated in physiologically young and active patients, especially those with thin, muscular arms who may be concerned about cosmetic issues; it can be performed via either open [1, 3, 8, 23] or arthroscopic [5, 12, 13, 22] techniques (Table 1).
Table 1.
Published results of varying biceps tenodesis techniques
| Study | Number of patients | Surgical technique | Tenodesis location | Followup (months)* | Outcome |
|---|---|---|---|---|---|
| Crenshaw and Kilgore [8] | 89 (92 shoulders) | Open | Within greater tuberosity (64) | 12 | Good or excellent results in 90% |
| To lesser tuberosity (3) | |||||
| To coracoid (5) | |||||
| Boileau et al. [5] | 43 | Arthroscopic | Top of the groove | 12 | Average postoperative Constant-Murley score 79 Strength 90% of nonoperative arm |
| Elkousy et al. [10] | 11 | Arthroscopic | Intraarticular transtendon | 6 | 10/11 with relief of pain |
| 1 with persistent pain | |||||
| Mazzocca et al. [15] | 41 | Open | Subpectoral | 29 (12–49) | Mean Rowe score 86 |
| ASES score 81 | |||||
| SST score 9 | |||||
| Constant-Murley score 87 | |||||
| SANE score 84 |
* Values are expressed as mean or mean with range in parentheses; ASES = American Shoulder and Elbow Surgeons; SST = Simple Shoulder Test; SANE = Single Assessment Numeric Evaluation.
Tenodesis with an interference screw has been described by several authors [5, 13]. Biomechanical analysis has established interference screw fixation as stronger than soft tissue tenodesis [2, 18]. Since the original description of Gartsman and Hammerman [12] of an onlay technique with suture anchors in 2008, arthroscopic biceps tenodesis techniques have continued to evolve. However, the ideal tenodesis location remains a controversial subject. Concerns have been raised regarding persistent postoperative bicipital pain [3], leading some to question the cause of persistent pain after such a procedure. Intraarticular findings of biceps tenosynovitis streaking distally into the groove suggest an inflammatory component to the tendon within the bicipital groove, as suggested by DePalma and Callery [9]. Tenodesis within the upper portion of the groove may allow this inflammation to persist, representing a residual source of pain after tenodesis. Some authors have suggested a more distal tenodesis may eliminate pain generators from tendonitis within the groove [15–17, 19]. The technical challenges of arthroscopic biceps tenodesis distal to the bicipital groove have led to the development of the open subpectoral tenodesis technique. Although previous studies have suggested benefits from a more distal tenodesis location, the literature comparing these locations is sparse. However, revision rates after proximal arthroscopic tenodesis were higher (35.7%) than those after open distal tenodesis (2.7%) with mean 18 months’ followup [21].
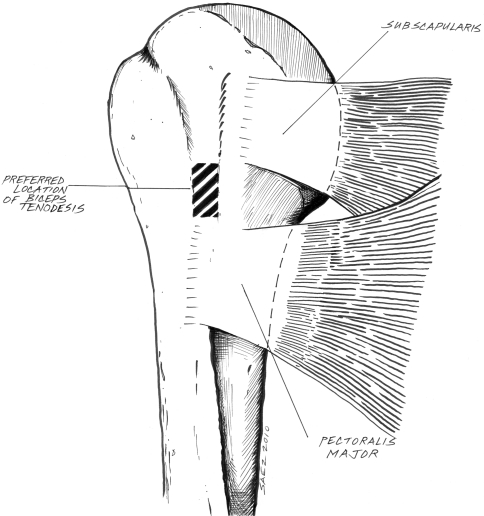
In recent years, we have developed a technique to arthroscopically tenodese the biceps tendon below the bicipital groove, accomplishing the same objective as the open procedure, while potentially improving cosmesis and minimizing morbidity. This technique arthroscopically achieves suprapectoral biceps tenodesis using a bioabsorbable interference screw (Fig. 1).
Fig. 1.
This line drawing demonstrates the preferred location for biceps tenodesis with the arthroscopic suprapectoral technique. This image is printed with the permission of Hector R. Saez, Jr.
We asked the following questions: (1) Does a higher tenodesis in the biceps groove result in postoperative pain? And (2) can the tenodesis location be successfully moved more distally (“suprapectoral tenodesis”) by an arthroscopic technique?
Patients and Methods
We retrospectively reviewed the surgical log of a single surgeon (ELF) to identify all patients who underwent arthroscopic shoulder LHB tenodeses using a bioabsorbable screw from 2000 to 2006 at Mount Sinai Medical Center. We identified 40 consecutive patients eligible during this time period. Seventeen patients completed minimum 12 months’ followup and were included in this study. Indications for biceps tenodesis included partial tear (eight patients), tenosynovitis (11 patients), or medial subluxation of the biceps tendon (none in this series). Additional procedures performed included arthroscopic subacromial decompression (15 primary, two revision), rotator cuff repair (nine), glenohumeral débridement (four), distal clavicle resection (four), capsular release (two), superior labral anterior-posterior repair for detachment of the entire superior labrum (one), and subscapularis tear (one). One patient underwent an isolated arthroscopic subacromial decompression and biceps tenodesis. Minimum followup for all patients was 12 months (mean, 28 months; range, 12–69 months; Group 1: mean, 26 months; range, 12–55 months; Group 2: mean, 32 months; range, 12–69 months). No patients were lost to followup, although one patient did not complete American Shoulder and Elbow Surgeons (ASES) and Constant-Murley scores at latest followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
The surgical technique has been previously described [14]. Surgery was performed by a single surgeon (ELF). All arthroscopic biceps procedures were performed in the beach chair position under regional (interscalene) anesthesia. The arm was positioned with the use of the SPIDER Limb positioner (Tenet Medical Engineering, Calgary, Alberta, Canada). The pump pressure was maintained at low pressure (30 mm Hg), and the fluid was mixed with 1:10,000 parts epinephrine.
Diagnostic glenohumeral arthroscopy was begun by establishing a standard posterior viewing portal. An anterior portal was created through the rotator interval. An inspection of the intraarticular glenohumeral joint was performed, including an assessment of the tendon of the LHB. The tendon was assessed at its origin and along the intertubercular groove by pulling the biceps tendon into the glenohumeral joint with a hooked probe. Once the decision to proceed with a tenodesis had been made, a spinal needle was used to pass two Number 0 polydiaxone monofilament absorbable sutures (PDS®; Ethicon, Cornelia, GA) through the tendon, just distal to the biceps insertion site. Both limbs of the sutures were retrieved from the anterior portal site to control the biceps tendon after tenotomy. The tendon was transected at its insertion site with an arthroscopic biter or electrocautery.
Subacromial decompression and bursectomy were then completed via a lateral portal to assist in visualization. Particular attention was given to the anterior and lateral gutters of the subacromial space. Rotator cuff integrity was evaluated and addressed as necessary after the biceps tenodesis. To aid in visualization of the bicipital groove, the arm was positioned at 60° of flexion, 30° of external rotation, and 30° of abduction. Viewing through the posterior portal, the arthroscope was turned to look down the bicipital groove. Débridement of additional bursa via the anterior portal was completed as necessary to obtain adequate visualization of the bicipital groove.
Using needle localization, an additional working portal, the anterolateral portal, was established directly over the biceps groove. Once the portal was established, the biceps could be probed in its groove. Using a beaver blade, the biceps sheath was incised longitudinally, carefully and cleanly exposing the tendon. The tendon was pulled into the subdeltoid space, and its previously placed traction sutures were shuttled out through the anterolateral portal. The tendon was then pulled out of the portal and exteriorized.
Distal to the traction stitch, a Number 2 FiberWire® (Arthrex, Inc, Naples, FL) Krackow stitch was placed in the biceps tendon, removing 2 cm of biceps tendon proximal to the suture, allowing for the portion of the biceps that would be pulled down the bone tunnel to set the correct tension. The tendon diameter was then measured to determine the reamer size (Arthrex). The FiberWire® ends were then shuttled out through the anterior portal to pull the biceps medially and improve visualization of the bicipital groove.
To optimize tenodesis, a bony bed was prepared. Early in the series, this was often in the upper biceps groove. Later, the technique was modified to place the tunnel distal to the bicipital groove. The superior edge of the pectoralis major tendon insertion could often be visualized; however, this was not critical as it was not violated with this technique. A 2.4-mm drill guide wire was placed through the anterolateral portal, perpendicular to the humeral shaft. Reaming was completed over a guide wire through the near cortex only with a cannulated reamer matching the tendon diameter.
The FiberWires® and tendon were then shuttled out of the anterolateral portal. Depending on the quality of bone, a Bio-Tenodesis™ screw (Arthrex) of the same diameter, or one size smaller, was loaded onto the Bio-Tenodesis™ screw driver. The two ends of the previously placed suture were fed into the tip of the Bio-Tenodesis™ screw driver and pulled through to the handle of the driver. The sutures were tensioned such that the tip of the screw abutted the biceps tendon.
The tendon-screwdriver complex was then advanced through the anterolateral portal and into the prepared socket. The screw was advanced until it was flush with the anterior humeral cortex. Concomitant shoulder pathology was addressed after the tenodesis because any fluid extravasation from other procedures would make visualization for the tenodesis more difficult.
Postoperative restrictions to movement were dictated by the presence of a concomitant rotator cuff repair. If the rotator cuff was not addressed, shoulder active and passive motion was allowed. Active flexion without resistance, active extension, and passive ROM of the elbow were allowed immediately. Active biceps flexion against resistance was restricted for 6 weeks. Postoperative radiographs were obtained to assess the tenodesis location (Fig. 2).
Fig. 2.
This radiographic view demonstrates the typical postoperative appearance with a suprapectoral tenodesis.
Patients were routinely seen at 2 weeks, 6 weeks, 6 months, and 1 year postoperatively. As the patients in this study underwent a variety of other procedures, patients may have had more or less frequent visits. A series of shoulder radiographs (AP, Grashey, scapular Y, and axillary views) were obtained not before 6 weeks from surgery. Postoperatively, patients were examined and ASES scores [20], Constant-Murley scores [6, 7], and visual analog scale scores for pain were obtained. Clinical postoperative assessment included evaluation of the appearance of the extremity to assess for any biceps deformity or change in the shape of the arm. Full clinical assessments, including pre- and postoperative ASES and Constant-Murley scores, were available in 16 of 17 patients. Postoperative complications, including tenodesis failure and persistent bicipital pain, were recorded for both the 6-month time point and the examination at most recent followup. We retrospectively evaluated operative notes, arthroscopic pictures, and postoperative radiographs to determine the location of the biceps tenodesis. Location was stratified retrospectively into two groups: Group 1 with tenodesis in the upper half of the bicipital groove (classic technique) and Group 2 with tenodesis in the lower half of the groove or below (suprapectoral technique). The two groups were created retrospectively as the technique evolved toward a more distal tenodesis site. When patients presented with persistent pain after proximal tenodesis, the tenodesis location was moved distally.
Results
Five of 17 tenodeses were within the upper half of the bicipital groove and two of these five patients had persistent tenderness at their tenodesis site 1 year after surgery. One patient had relief of pain after a lidocaine injection into the bicipital groove. Both patients had resolution of their pain with simple débridement of the biceps groove. Of the 12 patients who underwent a suprapectoral tenodesis, 10 were placed such that no portion of the tendon remained in the groove and two patients had a tenodesis with some portion of the tendon remaining in the distal portion of the groove. In the suprapectoral group, two were symptomatic at their tenodesis site at 6 months’ followup. Both patients were managed nonoperatively and were asymptomatic at their 12 months’ office visit. The suprapectoral tenodesis group was entirely asymptomatic with regard to tenderness at the tenodesis site at final followup. These results suggest tenodesis higher in the groove may result in a higher rate of postoperative pain.
Overall ASES scores (49 preoperative to 78 postoperative) and Constant-Murley scores (58 preoperative to 81 postoperative) improved at last followup. All patients healed at the tenodesis site without clinical evidence of biceps rupture or screw failure. No patient developed a deformity of the biceps muscle or had a change in the shape of the arm. No patient had any radiographic evidence of fracture at the tenodesis site. There were no substantial complications, such as humeral fracture, infection, or nerve injury, associated with this technique.
Discussion
Arthroscopic biceps tenodesis can be technically challenging without careful planning, proper arm positioning, and adequate visualization of the proximal anterior humerus. We present our modification of the technique presented by Lo and Burkhart [14] for achieving a biceps tenodesis; this modification targets a tenodesis site distal to the biceps groove. We asked the following questions: (1) Does a higher tenodesis in the biceps groove result in postoperative pain? And (2) can the tenodesis location be successfully moved more distally (“suprapectoral tenodesis”) by an arthroscopic technique?
This study suggests improved results with a new technique but does have several limitations. First, our sample size is small and prospective study of a larger population is needed to determine whether tenodesis location statistically affects postoperative pain and function. Second, the minimum patient followup is short at 12 months, although improvement beyond 12 months would not be expected for biceps tenodesis. Third, we assessed biceps integrity clinically, not objectively with ultrasound or MRI, as these studies are not included in routine postoperative evaluations and were not available for this retrospective study. Finally, patient outcomes may be affected by concomitant procedures performed, such as rotator cuff repair and subacromial decompression, though biceps tenodesis is almost never performed in isolation. Although it would be ideal to review isolated tenodesis cases, as this is so rarely performed alone, it would be difficult to compile a pure series.
Concerns over persistent bicipital pain associated with arthroscopically placed Bio-Tenodesis™ screws has led some surgeons to advocate for open tenodesis at or under the insertion of the pectoralis major [15–17, 19]. Sanders et al. [21] presented their results comparing proximal and distal tenodesis sites. Their retrospective review of 188 patients demonstrated a higher revision rate for proximal arthroscopic tenodesis (35.7%) than for distal open tenodesis (2.7%). The authors also noted proximal techniques that included a release of the biceps sheath had a lower revision rate than those in which the sheath was not released (2.4% versus 13.4%, respectively). Tenodesis location remains controversial. We were motivated to present our findings of a new distal arthroscopic fixation technique after two patients required additional treatment for persistent pain after proximal arthroscopic tenodesis. Although anterior shoulder pain has many etiologies, the two patients with persistent pain at 1 year localized their discomfort to the bicipital groove. One patient had complete relief of symptoms with a lidocaine injection into the groove. Both had relief of pain after débridement of the groove, supporting this location as the source of their symptoms.
We present a novel modification of the standard arthroscopic biceps tenodesis: a suprapectoral tenodesis below the bicipital groove. Our results demonstrated improved ASES and Constant-Murley scores. Our results comparing the proximal and distal tenodesis sites are comparable to that in the literature [21]. Notably, none of the patients undergoing tenodesis at the distal location had persistent pain or required additional treatment or a revision procedure. This is comparable to results with open subpectoral tenodesis. Most recently, Nho et al. [17] reported persistent pain after open subpectoral tenodesis in only 0.57% of 353 patients at 3 years. Those authors acknowledge their low rate of residual pain may be attributed to their distal tenodesis location.
Our data suggest suprapectoral tenodesis may allow predictable pain relief, with decreased incidence of persistent tenderness around the tenodesis site, and as this study demonstrates, it can be achieved with an arthroscopic technique.
Acknowledgments
We thank Andrew Hsiao, MD, Andrew Neviaser, MD, and Bradford Parsons, MD, for their assistance with this study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ball C, Galatz LM, Yamaguchi K. Tenodesis or tenotomy of the biceps tendon: why and when to do it. Tech Shoulder Elbow Surg. 2001;2:140–152. doi: 10.1097/00132589-200109000-00002. [DOI] [Google Scholar]
- 2.Barber FA, Byrd JW, Wolf EM, Burkhart SS. How would you treat the partially torn biceps tendon? Arthroscopy. 2001;17:636–639. doi: 10.1053/jars.2001.24852. [DOI] [PubMed] [Google Scholar]
- 3.Becker DA, Cofield RH. Tenodesis of the long head of the biceps brachii for chronic bicipital tendinitis: long-term results. J Bone Joint Surg Am. 1989;71:376–381. [PubMed] [Google Scholar]
- 4.Boileau P, Baque F, Valerio L, Ahrens P, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Krishnan SG, Coste JS, Walch G. Arthroscopic biceps tenodesis: a new technique using bioabsorbable interference screw fixation. Tech Shoulder Elbow Surg. 2001;2:153–165. doi: 10.1097/00132589-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Constant CR. An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg Br. 1997;79:695–696. [PubMed] [Google Scholar]
- 7.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 8.Crenshaw AH, Kilgore WE. Surgical treatment of bicipital tenosynovitis. J Bone Joint Surg Am. 1966;48:1496–1502. [PubMed] [Google Scholar]
- 9.DePalma AF, Callery GE. Bicipital tenosynovitis. Clin Orthop Relat Res. 1954;3:69–85. [PubMed] [Google Scholar]
- 10.Elkousy HA, Fluhme DJ, O’Connor DP, Rodosky MW. Arthroscopic biceps tenodesis using the percutaneous, intra-articular trans-tendon technique: preliminary results. Orthopedics. 2005;28:1316–1319. doi: 10.3928/0147-7447-20051101-08. [DOI] [PubMed] [Google Scholar]
- 11.Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sports Med. 2009;37:828–833. doi: 10.1177/0363546508322179. [DOI] [PubMed] [Google Scholar]
- 12.Gartsman GM, Hammerman SM. Arthroscopic biceps tenodesis: operative technique. Arthroscopy. 2000;16:550–552. doi: 10.1053/jars.2000.4386. [DOI] [PubMed] [Google Scholar]
- 13.Klepps S, Hazrati Y, Flatow E. Arthroscopic biceps tenodesis. Arthroscopy. 2002;18:1040–1045. doi: 10.1053/jars.2002.36467. [DOI] [PubMed] [Google Scholar]
- 14.Lo IK, Burkhart SS. Arthroscopic biceps tenodesis using a bioabsorbable interference screw. Arthroscopy. 2004;20:85–95. doi: 10.1016/j.arthro.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 15.Mazzocca AD, Cote MP, Arciero CL, Romeo AA, Arciero RA. Clinical outcomes after subpectoral biceps tenodesis with an interference screw. Am J Sports Med. 2008;36:1922–1929. doi: 10.1177/0363546508318192. [DOI] [PubMed] [Google Scholar]
- 16.Mazzocca AD, Rios CG, Romeo AA, Arciero RA. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;21:896. doi: 10.1016/j.arthro.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Nho SJ, Reiff SN, Verma NN, Slabaugh MA, Mazzocca AD, Romeo AA. Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19:764–768. doi: 10.1016/j.jse.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 18.Ozalay M, Akpinar S, Karaeminogullari O, Balcik C, Tasci A, Tandogan RN, Gecit R. Mechanical strength of four different biceps tenodesis techniques. Arthroscopy. 2005;21:992–998. doi: 10.1016/j.arthro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Provencher MT, LeClere LE, Romeo AA. Subpectoral biceps tenodesis. Sports Med Arthrosc. 2008;16:170–176. doi: 10.1097/JSA.0b013e3181824edf. [DOI] [PubMed] [Google Scholar]
- 20.Richards RR, An K, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA, Zuckerman JD. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 21.Sanders B, Lavery K, Pennington S, Warner JJP. Biceps tendon tenodesis: success with proximal versus distal fixation (SS-16) Arthroscopy. 2008;24:e9–e9. doi: 10.1016/j.arthro.2008.04.017. [DOI] [Google Scholar]
- 22.Sekiya LC, Elkousy HA, Rodosky MW. Arthroscopic biceps tenodesis using the percutaneous intra-articular transtendon technique. Arthroscopy. 2003;19:1137–1141. doi: 10.1016/j.arthro.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 23.Sethi N, Wright R, Yamaguchi K. Disorders of the long head of the biceps tendon. J Shoulder Elbow Surg. 1999;8:644–654. doi: 10.1016/S1058-2746(99)90105-2. [DOI] [PubMed] [Google Scholar]
- 24.Szabo I, Boileau P, Walch G. The proximal biceps as a pain generator and results of tenotomy. Sports Med Arthrosc. 2008;16:180–186. doi: 10.1097/JSA.0b013e3181824f1e. [DOI] [PubMed] [Google Scholar]
- 25.Walch G, Edwards TB, Boulahia A, Nove-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]