Abstract
Background
The importance of the radial head to elbow function and stability is increasingly apparent. Although preservation of the native radial head is preferred, severely comminuted fractures may necessitate resection or arthroplasty. Silastic radial head arthroplasty has been condemned on the basis of several sporadic reports of silicone synovitis. However, problems of “overstuffing,” cartilage wear, and motion loss are becoming apparent with metal prostheses, indicating this also is not an ideal solution. Thus, the choices remain controversial.
Questions/purposes
We asked whether intact or reconstructed primary elbow stabilizers permit use of silastic radial head implants without fragmentation, failure, and silicone synovitis.
Methods
We retrospectively reviewed 23 patients with unreconstructable radial head fractures who were treated with silastic radial head arthroplasty and concomitant repair and/or reconstruction of the medial ulnar collateral ligament and/or lateral ulnar collateral ligament. Analysis included range of motion, pain, stability, and radiographic assessments; Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire; and Mayo Elbow Performance Score (MEPS). The minimum followup was 16 months (average, 69.6 months; range, 16-165 months).
Results
At last followup, the mean elbow flexion was 145°, extension 11°, supination 80°, and pronation 83°. The mean MEPS score was 88.9. The mean DASH score was 11.8. There were eight reoperations, none resulting from failure of the radial head implants.
Conclusions
These results demonstrate silastic radial heads can be used with low complication rates and without evidence of synovitis when concomitant elbow ligament repair or reconstruction is performed.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The radial head is an important secondary valgus restraint [16, 25] and can bear up to 60% of the load transmitted from the forearm [9]. The goals of treating radial head fractures are to restore stability, preserve motion, and maintain length of the radius. If preservation of the head is not possible, prosthetic replacement has been advocated to preserve the radiocapitellar articulation. Currently, several models of radial head prosthesis are in use, including monopolar, bipolar, cemented, or press-fit implants. Regardless of design, recent literature has favored metal prostheses [1, 24, 30, 36, 37] despite evidence of altered joint contact pressures in radiocapitellar articulations involving metallic implants [18]. “Overstuffing” as a result of an excessively large prosthesis has received considerable attention [4, 40] and problems of persistent pain and radiographic evidence of arthritis (Fig. 1A–B) are becoming apparent, suggesting, like other metal-on-cartilage interfaces, metal hemiarthroplasty may not be an ideal solution (Fig. 2).
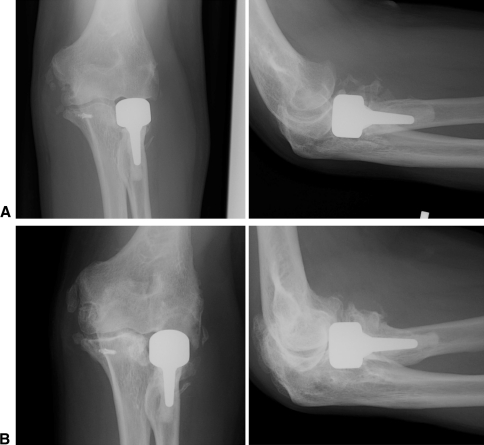
Fig. 1A–B.
AP and lateral views of a metallic radial head prosthesis (A) 4 months after implantation and (B) 3 years after implantation demonstrating degeneration of the capitellum.
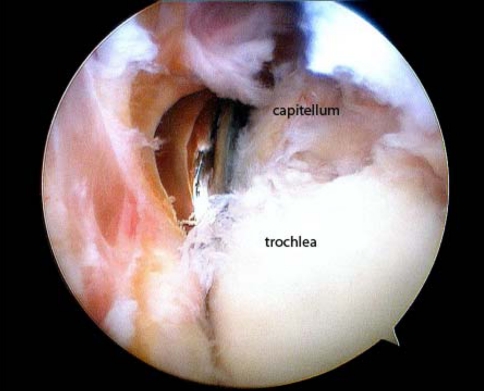
Fig. 2.
Intraoperative arthroscopy image showing the articular wear of the capitellum from a metallic radial head prosthesis. Radiographs demonstrate the prosthesis is in good position. Criteria for “overstuffing” are indefinite, but the prosthesis does not appear grossly oversized.
Meanwhile, the use of silastic radial head implants is widely condemned. Once commonly used in the 1970s and 1980s, this type of prosthesis is currently maligned based on reports of mechanical failure of the implant, inflammatory arthritis, and reactive synovitis [5, 20, 27, 38, 39]. Our review of the literature, however, suggests this poor reputation has been earned on the basis of limited data with questionable surgical indications and technique.
In the normally functioning elbow, the anterior band of the medial ulnar collateral ligament (MUCL) provides the primary stabilization against valgus force [6, 12, 16, 23, 32]. Transection of the anterior bundle alone is sufficient to create demonstrable instability on the application of a valgus force and abnormally high radiocapitellar pressures [28]. The interosseous membrane (IOM) functions as another primary stabilizer of the elbow by providing longitudinal restraint to proximal migration of the radius during axial loading [21]. Radial head fracture or fracture/dislocation is attended by a high incidence of ligament damage and repair of the collateral ligaments is critical to re-establishing normal joint biomechanics during surgical treatment of these injuries [14, 16]. In an in vitro model, Pollock et al. recently demonstrated repair of the lateral ulnar collateral ligament (LUCL) and MUCL restored elbow stability to varus and valgus stress, even in the presence of a displaced Type II coronoid fracture, suggesting evaluation and repair of the collateral ligaments is essential in cases of persistent instability [29]. When both the MUCL and IOM are intact, the radial head functions as a secondary stabilizer. However, if the MUCL or IOM is ruptured, the radial head becomes the primary stabilizer and is subjected to supraphysiological loads. In throwing athletes, such increased loading is associated with premature arthrosis even with only an isolated ligament rupture, a situation that becomes further confounded by additional trauma and instability [3]. We speculate that the reported failures of silicone prostheses were caused by supraphysiologically high loads borne by the prostheses as a consequence of rupture and functional incompetence of the primary restraints.
Our purpose was to demonstrate these implants can be used without reported complications to restore function as assessed by standardized, validated outcome instruments (Disabilities of the Arm, Shoulder, and Hand [DASH] and Mayo Elbow Performance Score [MEPS]) if combined with ligamentous reconstruction and/or repair at the time of initial treatment.
Patients and Methods
We retrospectively reviewed 26 patients who received silastic radial head implants (Dow Corning Corporation Silastic Swanson Radial Head Implant, Midland, MI) combined with treatment of the ligamentous injury between 1995 and 2007. One patient died 7 months after surgery, and two others were lost to followup. This left 23 patients with an average age of 48 years (range, 19–75 years). The arthroplasties were performed in 13 women and 10 men. There were two Workers’ Compensation cases. Thirteen arthroplasties were performed on the patient’s dominant arm. The minimum followup was 16 months (average, 69.6 months; range, 16–165 months; Table 1). We have prior approval from our Institutional Review Board.
Table 1.
Summary of patient demographics and treatment
| Patient number | Age (years) | Gender | Dominant arm | Workers’ compensation | Length of followup (months) | Diagnosis | Procedure |
|---|---|---|---|---|---|---|---|
| 1 | 66 | F | Y | N | 59 | RH fracture, MUCL rupture, LUCL rupture, coronoid fx | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid |
| 2 | 75 | F | N | N | 19 | RH fracture, MUCL rupture, LUCL rupture | RH arthroplasty, MUCL repair, LUCL repair |
| 3 | 40 | M | N | N | 16.5 | RH fracture, MUCL rupture, LUCL rupture, coronoid fx | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid |
| 4 | 74 | F | N | N | 17.5 | RH fracture, MUCL rupture, LUCL rupture, coronoid fx | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid |
| 5 | 29 | F | Y | N | 118 | Type IV Monteggia fracture dislocation | RH arthroplasty, ORIF proximal ulna |
| 6 | 64 | F | Y | N | 45.5 | RH fracture, LUCL rupture | RH arthroplasty, LUCL repair |
| 7 | 24 | M | Y | N | 112.5 | RH fracture, LUCL rupture, MUCL rupture | RH arthroplasty, MCUL reconstruction, LUCL repair, brachialis repair |
| 8 | 44 | M | Y | N | 17.5 | RH fracture, MUCL rupture, LUCL rupture, coronoid fx | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid |
| 9 | 19 | M | N | N | 109 | RH fracture, MUCL rupture, ipsilateral scaphoid fracture, and trapeziometacarpal subluxation | RH arthroplasty, MUCL repair; ORIF scaphoid, thumb CMC volar ligament reconstruction |
| 10 | 63 | F | N | N | 77 | RH fracture, LUCL rupture, coronoid fracture | RH arthroplasty, ORIF coronoid fx, LUCL reconstruction |
| 11 | 72 | F | Y | N | 66 | RH fracture, LUCL rupture | RH arthroplasty, LUCL repair |
| 12 | 87 | F | Y | N | 20 | RH fracture, LUCL rupture, MUCL rupture, coronoid fracture | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid |
| 13 | 66 | F | Y | N | 28 | RH fracture, LUCL rupture, MUCL rupture, coronoid fracture | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid |
| 14 | 42 | M | N | N | 165 | RH fracture, MUCL rupture | RH arthroplasty, MUCL reconstruction |
| 15 | 38 | M | N | N | 155 | RH fracture, MUCL rupture | RH arthroplasty, MUCL reconstruction |
| 16 | 35 | M | Y | N | 57 | Failed conservative treatment: RH nonunion and elbow contracture | Capsulectomy and contracture release, RH arthroplasty |
| 17 | 45 | F | Y | N | 53 | Failed conservative treatment: RH fracture and MUCL rupture | RH arthroplasty, MUCL reconstruction |
| 18 | 21 | F | N | N | 18 | Revision surgery: elbow contracture, HO, status post-MUCL reconstruction | Arthroscopic HO excision and contracture release, RH arthroplasty |
| 19 | 30 | F | Y | Y | 85 | Failed ORIF RH and MUCL reconstruction | Excision of HO and contracture release, neurolysis, RH arthroplasty |
| 20 | 53 | M | Y | N | 58.5 | Synositis, status post-ORIF radial head and proximal ulna | Excision of HO and contracture release, RH arthroplasty |
| 21 | 46 | M | N | N | 101.5 | Type IV Monteggia fracture dislocation | Revision ORIF ulna, RH arthroplasty |
| 22 | 36 | M | N | Y | 152 | Failed RH metallic prosthesis and instability (MCL attenuation) | Revision RH arthroplasty, MUCL reconstruction |
| 23 | 45 | F | Y | N | 50.5 | Failed RH metallic arthroplasty with severe elbow contracture | Revision RH arthroplasty, HO excision, and contracture release |
F = female; M = male; Y = yes; N = no; fx = fracture; HO = heterotrophic ossification; LUCL = lateral ulnar collateral ligament; MUCL = medial ulnar collateral ligament; ORIF = open reduction internal fixation; RH = radial head; ROH = removal of hardware.
The indications for radial head arthroplasty included fracture–dislocation of the elbow with an unsalvageable Type III or IV radial head fracture. Fifteen patients presented for initial management of the injury after sustaining acute trauma to the elbow. In these cases, the elbow was stressed intraoperatively to assess ligamentous integrity. Instability was treated by primary repair of the LUCL and/or reconstruction of the MUCL with a palmaris longus tendon graft. Of these 15 patients presenting acutely, six patients sustained fracture–dislocations of the elbow, seven presented with terrible triad injuries, and two had Monteggia-variant fracture–dislocations. One patient in the fracture–dislocation group underwent an ipsilateral open reduction and internal fixation of the scaphoid and reconstruction of a thumb carpometacarpal joint volar ligament reconstruction (Patient 17).
Two of the 23 patients presented for delayed treatment of their injured elbows after failing initial nonoperative management. One had a radial head nonunion, whereas the other had a neglected radial head fracture with MUCL rupture.
Six other patients presented after a failed index procedure. They underwent revision surgery with contracture release and silastic radial head arthroplasty. Three of these six had initially sustained terrible triad injuries, and one had sustained a Monteggia fracture–dislocation. The remaining two patients underwent revision for joint contracture after placement of a metallic radial head implant or after metallic radial head breakage.
The silastic implant was never used in cases of Essex-Lopresti injuries because no reliable means of repairing or reconstructing the interosseous membrane is known. Metallic radial heads were used instead.
All surgery was performed by the senior author (MRH). After induction of anesthesia and prepping of the extremity, valgus stability of the elbow is assessed first. If there is valgus instability, a medial approach to the elbow is carried out first, and the MUCL is reconstructed with a tendon autograft using the Jobe [17] or the docking technique [35]. After skin closure of the medial side, a lateral midaxial incision is used. The radial head is exposed anterior to the LUCL, and the arthroplasty is carried out. The LUCL is either spared if intact or repaired if torn. A coronoid fracture is repaired from either the medial or the lateral approach.
Postoperatively, the patients are splinted for 3 to 5 days and are started on both supervised and self-administered overhead ROM exercises while avoiding valgus stress. Strengthening begins at 10 weeks.
The patients were followed up on a weekly basis for the first 4 weeks and then every 2 to 4 weeks for the next 3 months. Sixteen patients were able to return for a physical examination conducted by the senior author (MRH), the fellow (YM), or a senior resident (JB) in the office. The physical examination included ROM measurements to the nearest 5° using a goniometer and stability assessment of the elbow with varus and valgus stresses under fluoroscopy. DASH [13] and MEPS [26] were assessed as well. Seven patients were unable to come in for physical examination; pain assessment, DASH, and MEPS scores were obtained through a phone interview conducted by the fellow (YM) or the senior resident (JB). ROM measurements for these patients were taken from a chart review based on their most recent office visit at an average of 57 months after their procedure (range, 20–109 months).
Two of us (YM and MRH, the treating surgeon) evaluated all radiographs. All patients had radiographs at last followup. We assessed degenerative changes (osteophytes, joint space narrowing), prosthesis alignment, deformation, fracture or fragmentation, or multiple cysts indicative of synovitis by using the criteria defined by Forster et al. [7].
Results
The mean extension and flexion obtained in our patients was 11° to 145° (range, 0°–30° of extension and 130°–150° of flexion; Table 2). Mean supination and pronation were 80° and 83°, respectively (range, 45°–90° of supination and 50°–90° of pronation). The mean DASH score was 11.8 (SD, 14.5; range, 0–56) and a mean MEPS score of 88.9 (SD, 14.8; range, 45–100). Four patients had either a DASH score greater than 25 (n = 2) or a MEPS score less than 75 (n = 3) with two of these patients having sustained subsequent ipsilateral elbow trauma and three having been a revision or delayed procedure.
Table 2.
Results of treatment
| Patient number | Procedure | ROM extension–flexion (degrees) | ROM pronation–supination (degrees) | Forster radiographic score | DASH Score | MEPS | Reoperations |
|---|---|---|---|---|---|---|---|
| 1 | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid | 20–135 | 85–85 | 9 | 15 | 85 | Unrelated PIN palsy treated with tendon transfers |
| 2 | RH arthroplasty, MUCL repair, LUCL repair | 5–130 | 90–50 | 2 | 0.93 | 100 | Return to OR—arthroscopic radical capsulectomy; second return for I&D status postinfection |
| 3 | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid | 5–145 | 85–85 | 4 | 15 | 85 | Return to OR—contracture release |
| 4 | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid | 5–140 | 75–85 | 2 | 5 | 85 | |
| 5 | RH arthroplasty, ORIF proximal ulna | 0–145 | 70/80 | 3 | 7.5 | 85 | Return to OR—ROH of ulnar plate |
| 6 | RH arthroplasty, LUCL repair | 10–135 | 80–80 | 7 | 2.5 | 100 | |
| 7 | RH arthroplasty, MCUL reconstruction, LUCL repair, brachialis repair | 10–145 | 80–80 | 6 | 7.5 | 100 | |
| 8 | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid | 0–145 | 85–85 | 6 | 0.83 | 100 | |
| 9 | RH arthroplasty, MUCL repair; ORIF scaphoid, thumb CMC volar ligament reconstruction | 0–145 | 85–85 | 5 | 7.5 | 100 | |
| 10 | RH arthroplasty, ORIF coronoid fx, LUCL reconstruction | 20–150 | 85–85 | 5 | 42.5 | 80 | Return to OR—contracture release; second return for ORIF left distal humerus |
| 11 | RH arthroplasty, LUCL repair | 5–145 | 80–90 | 4 | 3.25 | 100 | |
| 12 | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid | 35–135 | 85–85 | 6 | 15 | 85 | |
| 13 | RH arthroplasty, MUCL reconstruction, LUCL repair, ORIF coronoid | 25–130 | 70–80 | 7 | 20.7 | 80 | |
| 14 | RH arthroplasty, MUCL reconstruction | 10–145 | 85–85 | 6 | 0 | 100 | Return to OR—contracture release |
| 15 | RH arthroplasty, MUCL reconstruction | 20–145 | 85–85 | 4 | 0.833 | 100 | Manipulation under anesthesia |
| 16 | Capsulectomy and contracture release, RH arthroplasty | 0–145 | 85–85 | 3 | 0.75 | 100 | |
| 17 | RH arthroplasty, MUCL reconstruction | 0–145 | 85–85 | 3 | 2.5 | 100 | |
| 18 | Arthroscopic HO excision and contracture release, RH arthroplasty | 35–150 | 85–85 | 7 | 56 | 45 | |
| 19 | Excision of HO and contracture release, neurolysis, RH arthroplasty | 0–145 | 85–85 | 8 | 12 | 85 | |
| 20 | Excision of HO and contracture release, RH arthroplasty | 30–145 | 45–85 | 7 | 2.5 | 100 | |
| 21 | Revision ORIF ulna, RH arthroplasty | 5–145 | 70–85 | 6 | 2.5 | 100 | |
| 22 | Revision RH arthroplasty, MUCL reconstruction | 10–145 | 85–85 | 9 | 18 | 65 | |
| 23 | Revision RH arthroplasty, HO excision and contracture release | 5–140 | 85–85 | 8 | 33 | 65 | Developed ulnar neuropathy after an MVA—treated with ulnar nerve transposition and contracture release |
DASH = Disabilities of the Arm, Shoulder, and Hand; HO = heterotrophic ossification; LUCL = lateral ulnar collateral ligament; MEPS = Mayo Elbow Performance score; MUCL = medial ulnar collateral ligament MVA = motor vehicle accident; OR = operating room; ORIF = open reduction internal fixation; PIN = posterior interosseous nerve; RH = radial head; I&D = irrigation and débridement; ROH = removal of hardware.
All elbows were stable at the last followup visit throughout their arc of motion with no evidence of dislocation, posterolateral or posteromedial rotatory instability, or varus or valgus instability on physical examination or fluoroscopic evaluation. No patient reported radiocapitellar area pain. Final radiographic evaluation revealed a concentric reduction of all elbows (Fig. 3A–B). One prosthesis fractured at the neck (Patient 5). This patient had a MEPS score of 85, DASH score of 7.5, and a full ROM of the elbow despite the prosthesis fracture. The average Forster radiographic score was 5.5.
Fig. 3A–B.
Example of AP and lateral views of a silastic arthroplasty (A) 18 months postoperatively showing a concentric reduction and good preservation of the radiocapitellar joint and (B) 165 months postoperatively from a different patient, again showing concentric reduction and good preservation of the radiocapitellar joint. Some “cold flow” deformation of the prosthesis is seen in late followup, but no fragmentation was seen.
Eight patients were returned to the operating room. Five of the eight patients developed contractures necessitating either manipulation under anesthesia (n = 1) or arthroscopic contracture release (n = 4). Biopsies were sent on three patients for histologic analysis. No histologic signs of synovitis were noted. No patients demonstrated clinical or radiographic features of silicone synovitis, as reported by Morrey et al. [27]. Two of those requiring releases again returned to the operating room, one of which acquired a secondary superficial oxacillin-resistant Staphylococcus aureus infection, requiring irrigation and débridement before healing uneventfully, and one patient required operative fixation of a distal humerus fracture sustained 9 months after the index procedure. One patient whose initial injury was a Monteggia’s fracture had symptomatic hardware removed from her proximal ulna. One patient who had revision surgery from a metallic head and severe contracture developed an ulnar neuropathy after a second injury to his elbow from a motor vehicle accident. He was treated with ulnar nerve transposition. Another patient who was initially treated for a terrible triad injury developed a delayed posterior interosseous nerve palsy years later unrelated to the elbow injury and was treated with tendon transfers. None of the patients undergoing contracture release required downsizing of the radial head implants.
Discussion
Radial head prosthetic arthroplasty is indicated by comminuted fractures [33] but there is no consensus on optimal prosthetic design. Silastic prostheses are easily inserted and have favorable hardness and elastic modulus but are condemned on the basis of reports of prosthesis failure and silicone synovitis. We question whether those failures are attributable to the prosthesis and material or the indications and technique and have studied the outcomes of silastic prostheses combined with restoration of the primary elbow ligament stabilizers.
We acknowledge limitations of our study. First, our review of 23 patients cannot definitively answer the question of radial head prosthesis design owing to selection bias inherent in retrospective reviews, limited followup, and limited outcome measures (particularly the radiographic analysis). It is useful, however, in sharing data that can be used to compare the outcomes of more recent designs, particularly in light of increasing concerns of arthrosis, stiffness, and “overstuffing.” Second, our inclusion criteria were broad. It is possible different diagnoses and procedures would fare differently with the use of a silastic head. However, given the study size, we grouped them together. Third, physical examination and review of radiographs at final followup were performed by the treating surgeon as well and not by an independent blinded individual.
Our report of intermediate and long-term results suggests ligament reconstruction may minimize or avoid complications of prosthesis fragmentation and silicone synovitis. Despite reports of restoration of full motion, minimal symptoms, and return to preinjury level of function [19] (Table 3), silastic radial head arthroplasty has been condemned because of isolated case reports of silicone synovitis [20, 27, 38, 39, 42]. Close examination of these data, however, suggest that instability of the elbow resulting from disruption of the primary ligamentous constraints is a common denominator of all the reported failures. In the report of Morrey report, 17 patients underwent silastic arthroplasty for revision of failed treatment for fracture–dislocations of the elbow, including an Essex-Lopresti lesion. Treatment did not include ligament reconstruction [27]. Similarly, in the report of Mayhall et al., five symptomatic implants were all done for revision surgery, again without ligament repair or reconstruction [20]. Synovitis is also reported in a rheumatoid patient with instability resulting from attrition of the MCL by rheumatoid disease [42]. This failure to address instability is common throughout all the reports of silicone synovitis on which condemnation of the prosthesis is based. This leads us to ask if failures are attributable to the silicone prosthesis or the indications and manner in which it has been used.
Table 3.
Summary of studies
| Author | Number of patients | Procedure | Average followup time | Results | Prosthetic failure | Silicone synovitis | Revision |
|---|---|---|---|---|---|---|---|
| Morrey et al. [27] | 17 | Silastic radial head | 6.7 years | 12/17 (71%) satisfactory; 5/17 (29%) unsatisfactory | 8/17 (47%) | Not specified | 29% |
| Mackay et al. [19] | 18 | Silastic radial head | 26 months | 7/18 (39%) excellent; 10/18 (56%) good; 1/18 (5%) poor | 2/18 (11%) | Not specified | 1/18 (5%) |
| Mayhall et al. [20] | 11 patients (12 prostheses) | Silastic radial head | Not specified; Case reports | Not specified | 5/12(42%) | Not specified | 3/12 (25%) |
| Herbertsson et al. [11] | 61 | Radial head excision | 18 years | 28 patients were symptoms free, 27 occasional pain and 6 with daily pain | N/A | N/A | N/A |
| Harrington et al. [10] | 20 | Metallic radial head arthroplasty | 12.1 years | 12 excellent; 4 good; 2 fair; 2 poor | N/A | ||
| Grewal et al. [8] | 26 | Metallic radial head arthroplasty | 24.5 months | Mean SF-36 score = 41.8; mean DASH = 24.4; mean MEPS = 83.4 with 50% excellent and 17% good | 0 | N/A | 0 |
| Popovic et al. [31] | 51 | Bipolar metallic arthroplasty | 8.4 years | MEPS: 14 excellent, 25 good, 9 fair, 3 poor. 37 with progressive osteolysis | None | N/A | None |
| Ring and King [34] | 27 | Metallic radial head arthroplasty | 40 months | MEPS: 13 excellent, 9 good, 3 fair, and 2 poor; Avg DASH = 17; Avg ASES instrument = 84 | 1 overstuffing | N/A | None |
| Hausman et al. | 23 patients | Silastic radial head replacement with concomitant medial ligament repair or reconstruction | 69.6 months | Avg DASH score 11.8; Avg MEPS 88.9: (12 excellent, 8 good, 2 fair, 1 poor) | 1/23 (4%) | Not observed | No revisions |
Avg = Average; DASH = Disabilities of the Arm, Shoulder, and Hand; MEPS = Mayo Elbow Performance Score; ASES = American Shoulder and Elbow Surgeons; N/A = not available.
Morrey and An demonstrated the importance of the MCL as the primary valgus restraint with the radial head being the secondary valgus stabilizer [24]. We believe the low elastic modulus and softness of the silastic make it unable to withstand the higher radiocapitellar loads that occur when the ligaments are not functional and that these increased forces lead to prosthesis fragmentation and failure. However, our data suggest this complication may be preventable by reconstructing the primary restraint (MCL) at the time of arthroplasty, thus dramatically reducing the radiocapitellar load on the prosthesis [24]. This is pertinent information given the uncertainty about the optimal treatment for nonreconstructable radial head fractures. Simple excision is associated with proximal migration of the radius, wrist pain, grip weakness, and ulnohumeral arthrosis [2, 11, 15, 22]. Absence of the radial head also increases elbow instability [2].
Metal prosthetic arthroplasty, although currently favored, is not supported with long-term data to validate their use and reports of early radiocapitellar arthrosis are cause for concern [8, 10, 31, 34, 41].
A perfect replacement for the complex geometry and function of the radial head may not presently exist, and a retrospective review of 23 patients cannot definitively answer the question of radial head prosthesis. However, this is the largest series of silastic arthroplasties yet reported and the only one in which ligament dysfunction and elbow instability were concomitantly treated. Our data will be a useful context in which to evaluate functional outcomes and complication rates for metal prostheses, especially as further information about concerns of arthrosis, stiffness, and “overstuffing” with metal prostheses becomes available. The data also suggest the silastic radial head prosthesis may be used in a stable elbow or one rendered stable by ligament repair or reconstruction without complications of prosthesis fragmentation or silicone synovitis to yield good radiographic and functional results by standardized outcome instruments such as the DASH and MEPS.
Acknowledgment
We thank Jason Baynes, MD, for his help in preparation of the manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bain GI, Ashwood N, Baird R, Unni R. Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization (surgical technique) J Bone Joint Surg Am. 2005;87:136–147. doi: 10.2106/JBJS.D.02710. [DOI] [PubMed] [Google Scholar]
- 2.Beingessner DM, Dunning CE, Gordon KD, Johnson JA, King GJ. The effect of radial head excision and arthroplasty on elbow kinematics and stability. J Bone Joint Surg Am. 2004;86:1730–1739. doi: 10.2106/00004623-200408000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Birkbeck DP, Failla JM, Hoshaw SJ, Fyhrie DP, Schaffler M. The interosseous membrane affects load distribution in the forearm. J Hand Surg [Am] 1997;22:975–980. doi: 10.1016/S0363-5023(97)80035-4. [DOI] [PubMed] [Google Scholar]
- 4.Birkedal JP, Deal DN, Ruch DS. Loss of flexion after radial head replacement. J Shoulder Elbow Surg. 2004;13:208–213. doi: 10.1016/j.jse.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Bohl WR, Brightman E. Fracture of a silastic radial-head prosthesis: diagnosis and localization of fragments by xerography A case report. J Bone Joint Surg Am. 1981;63:1482–1483. [PubMed] [Google Scholar]
- 6.Floris S, Olsen BS, Dalstra O, Sojbjerg JO, Sneppen O. The medial collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elbow Surg. 1998;7:345–351. doi: 10.1016/S1058-2746(98)90021-0. [DOI] [PubMed] [Google Scholar]
- 7.Forster MC, Clark DI, Lunn PG. Elbow osteoarthritis: prognostic indicators in ulnohumeral debridement—the Outerbridge-Kashiwagi procedure. J Shoulder Elbow Surg. 2001;10:557–560. doi: 10.1067/mse.2001.118416. [DOI] [PubMed] [Google Scholar]
- 8.Grewal R, MacDermid JC, Faber KJ, Drosdowech DS, King GJ. Comminuted radial head fractures treated with a modular metallic radial head arthroplasty. Study of outcomes. J Bone Joint Surg Am. 2006;88:2192–2200. doi: 10.2106/JBJS.E.00962. [DOI] [PubMed] [Google Scholar]
- 9.Halls AA, Travill A. Transmission of pressures across the elbow joint. Anatomical Record. 1964;150:243–247. doi: 10.1002/ar.1091500305. [DOI] [PubMed] [Google Scholar]
- 10.Harrington IJ, Sekyi-Otu A, Barrington TW, Evans DC, Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma. 2001;50:46–52. doi: 10.1097/00005373-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Nyqvist F, Karlsson MK. Fractures of the radial head and neck treated with radial head excision. J Bone Joint Surg Am. 2004;86:1925–1930. doi: 10.2106/00004623-200409000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Hotchkiss RN, Weiland AJ. Valgus stability of the elbow. J Orthop Res. 1987;5:372–377. doi: 10.1002/jor.1100050309. [DOI] [PubMed] [Google Scholar]
- 13.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 14.Itamura J, Roidis N, Mirzayan R, Vaishnav S, Learch T, Shean C. Radial head fractures: MRI evaluation of associated injuries. J Shoulder Elbow Surg. 2005;14:421–424. doi: 10.1016/j.jse.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Jensen SL, Olsen BS, Søjbjerg JO. Elbow joint kinematics after excision of the radial head. J Shoulder Elbow Surg. 1999;8:238–241. doi: 10.1016/S1058-2746(99)90135-0. [DOI] [PubMed] [Google Scholar]
- 16.Jensen SL, Olsen BS, Tyrdal S, Søjbjerg JO, Sneppen O. Elbow joint laxity after experimental radial head excision and lateral collateral ligament rupture: efficacy of prosthetic replacement and ligament repair. J Shoulder Elbow Surg. 2005;14:78–84. doi: 10.1016/j.jse.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68:1158–1163. [PubMed] [Google Scholar]
- 18.Liew VS, Cooper IC, Ferreira LM, Johnson JA, King GJ. The effect of metallic radial head arthroplasty on radiocapitellar joint contact area. Clin Biomech (Bristol, Avon) 2003;18:115–118. doi: 10.1016/S0268-0033(02)00172-9. [DOI] [PubMed] [Google Scholar]
- 19.Mackay I, Fitzgerald B, Miller JH. Silastic replacement of the head of the radius in trauma. J Bone Joint Surg Br. 1979;61:494–497. doi: 10.1302/0301-620X.61B4.500763. [DOI] [PubMed] [Google Scholar]
- 20.Mayhall WST, Tiley FT, Paluska DJ. Fracture of silastic radial-head prosthesis. J Bone Joint Surg Am. 1981;63:459–461. [PubMed] [Google Scholar]
- 21.McGinley JC, Kozin SH. Interosseous membrane anatomy and functional mechanics. Clin Orthop Relat Res. 2001;383:108–122. doi: 10.1097/00003086-200102000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Morrey BF. Radial head fracture. In: Morrey BF, editor. The Elbow and Its Disorders. 3. Philadelphia, PA: WB Saunders; 2000. pp. 341–364. [Google Scholar]
- 23.Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83:1201–1211. doi: 10.2106/00004623-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985;201:84–90. [PubMed] [Google Scholar]
- 25.Morrey BF, An KN. Stability of the elbow: osseous constraints. J Shoulder Elbow Surg. 2005;14(Suppl S):174S–178S. doi: 10.1016/j.jse.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 26.Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow. In: Morrey BF, editor. The Elbow and Its Disorders. 2. Philadelphia, PA: WB Saunders; 1993. pp. 86–89. [Google Scholar]
- 27.Morrey BF, Askew L, Chao EY. Silastic prosthetic replacement for the radial head. J Bone Joint Surg Am. 1981;63:454–458. [PubMed] [Google Scholar]
- 28.Pichora JE, Fraser GS, Ferreira LF, Brownhill JR, Johnson JA, King GJ. The effect of medial collateral ligament repair tension on elbow joint kinematics and stability. J Hand Surg Am. 2007;32:1210–1217. doi: 10.1016/j.jhsa.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 29.Pollock JW, Pichora J, Brownhill J, Ferreira L, McDonald CP, Johnson J, King GJ. The influence of type II coronoid fractures, collateral ligament injuries, and surgical repair on the kinematics and stability of the elbow: an in vitro biomechanical study. J Shoulder Elbow Surg. 2009;18:408–417. doi: 10.1016/j.jse.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 30.Popovic N, Gillet P, Rodriguez A, Lemaire R. Fracture of the radial head with associated elbow dislocation: results of treatment using a floating radial head prosthesis. J Orthop Trauma. 2000;14:171–177. doi: 10.1097/00005131-200003000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Popovic N, Lemaire R, Georis P, Gillet P. Midterm results with a bipolar radial head prosthesis: radiographic evidence of loosening at the bone-cement interface. J Bone Joint Surg Am. 2007;89:2469–2476. doi: 10.2106/JBJS.F.00723. [DOI] [PubMed] [Google Scholar]
- 32.Regan WD, Korineck SL, Morrey BF, An AK. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. 1991;271:170–179. [PubMed] [Google Scholar]
- 33.Ring D. Displaced, unstable fractures of the radial head: fixation vs replacement—what is the evidence? Injury. 2008;39:1329–1337. doi: 10.1016/j.injury.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 34.Ring D, King G. Radial head arthroplasty with a modular metal spacer to treat acute traumatic elbow instability Surgical technique. J Bone Joint Surg Am. 2008;90:63–73. doi: 10.2106/JBJS.G.01248. [DOI] [PubMed] [Google Scholar]
- 35.Rohrbough JT, Altchek DW, Hyman J, Williams RJ, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541–548. doi: 10.1177/03635465020300041401. [DOI] [PubMed] [Google Scholar]
- 36.Shore BJ, Mozzon JB, MacDermid JC, Faber KJ, King GJ. Chronic posttraumatic elbow disorders treated with metallic radial head arthroplasty. J Bone Joint Surg Am. 2008;90:271–280. doi: 10.2106/JBJS.F.01535. [DOI] [PubMed] [Google Scholar]
- 37.Smets S, Govaers K, Jansen N, Riet R, Schaap M, Glabbeek F. The floating radial head prosthesis for comminuted radial head fractures: a multicentric study. Acta Orthop Belg. 2000;66:353–358. [PubMed] [Google Scholar]
- 38.Trepman E, Ewald FC. Early failure of silicone radial head implants in the rheumatoid elbow. A complication of silicone radial head implant arthroplasty. J Arthroplasty. 1991;6:59–65. doi: 10.1016/S0883-5403(06)80158-0. [DOI] [PubMed] [Google Scholar]
- 39.Vanderwilde RS, Morrey BF, Melberg MW, Vinh TN. Inflammatory arthritis after failure of silicone rubber replacement of the radial head. J Bone Joint Surg Br. 1994;76:78–81. [PubMed] [Google Scholar]
- 40.Glabbeek F, Riet RP, Baumfeld JA, Neale PG, O’Driscoll SW, Morrey BF, An KN. Detrimental effects of overstuffing or understuffing with a radial head replacement in the medial collateral-ligament deficient elbow. J Bone Joint Surg Am. 2004;86:2629–2635. doi: 10.2106/00004623-200412000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Riet RP, Glabbeek F, Verborgt O, Gielen J. Capitellar erosion caused by a metal radial head prosthesis. A case report. J Bone Joint Surg Am. 2004;86:1061–1064. doi: 10.2106/00004623-200405000-00028. [DOI] [PubMed] [Google Scholar]
- 42.Worsing RA, Engber WD, Lange TA. Reactive synovitis from particulate silastic. J Bone Joint Surg Am. 1982;64:581–585. [PubMed] [Google Scholar]