Abstract
Background
The weightbearing axis of the limb goes from the pelvis to the ground and includes the hindfoot. However, the influence of hindfoot alignment on mechanical axis and overall limb alignment after TKA is unclear.
Questions/purposes
We therefore addressed the following questions: (1) Does hindfoot alignment change after TKA for knee osteoarthritis? (2) What factors influence hindfoot alignment after TKA? (3) Does deviation of the mechanical axis from the center of the knee vary when the hindfoot is considered (ground mechanical axis) as compared with when it is not (conventional mechanical axis) after TKA?
Patients and Methods
We prospectively reviewed the radiographs of 125 patients who underwent 165 TKAs. We evaluated the preoperative and postoperative hip-knee-ankle (HKA) angle, conventional mechanical axis deviation, ground mechanical axis (mechanical axis which included the hindfoot) deviation, and tibiocalcaneal angle.
Results
The preoperative hindfoot valgus alignment decreased after TKA. Preoperative hindfoot alignment was the only factor that influenced hindfoot alignment after TKA. The conventional mechanical axis showed less deviation from the center of the knee when compared with ground mechanical axis which showed lateral deviation after TKA. Despite limb alignment being restored to within 3° of neutral of the conventional mechanical axis after TKA, 29% of limbs had a postoperative ground mechanical axis deviation of 10 mm or greater.
Conclusions
Accurate restoration of limb alignment after TKA may be associated with persistent hindfoot valgus alignment with the ground mechanical axis passing lateral to the center of the knee. This could have implications on long-term survival of the implant owing to possible excessive loading laterally and needs further investigation.
Introduction
The mechanical axis frequently is used to assess the degree of deformity of the limb and runs from the center of the femoral head to the center of the ankle. However, the weightbearing axis of the limb goes from the floor to the pelvis and includes the hindfoot, in particular the subtalar joint. Guichet et al. [5] described the importance of the hindfoot in assessing the loading axis of the lower limb. Using the center of the ankle and the ground reaction point to plot two mechanical axis lines (which they termed the MADC line and MADG line, respectively), Guichet et al. [5] reported a difference between the mechanical axis deviation conventional (MADC) and mechanical axis deviation ground (MADG). Similarly, Lee et al. [6], in a study involving pediatric subjects, observed that ground mechanical axis may be a better measure of overall limb alignment than conventional mechanical axis.
Some authors have reported hindfoot malalignment in patients with deformed knees [1, 4, 8]. Desai et al. [4], in their analysis of 33 patients with genu varum deformities, reported associated hindfoot valgus deformities in 22 patients and varus hindfoot deformities in 11. Bouysset and Hugueny [1] and Souter [8] observed that rheumatoid varus arthritic knees have associated valgus hindfeet and rheumatoid valgus knees have varus hindfeet. Chandler and Moskal [2] observed larger varus knee deformities were associated with neutral or valgus hindfoot alignment. However, they concluded that although hindfoot alignment changes with change in knee alignment after TKA, the hindfoot alignment cannot be predicted on the basis of knee alignment. How hindfoot alignment influences overall limb alignment after TKA is unclear. Meding et al. [7], in their analysis of revisions performed in cruciate-retaining TKAs, found a high incidence of associated tibialis posterior tendon insufficiency and hindfoot valgus. This could have been attributable to the alteration in postoperative mechanical axis caused by the associated hindfoot deformity. We presume a substantial number of patients may have hindfoot valgus alignment, which may influence the overall weightbearing axis after TKA. However, whether hindfoot alignment influences the mechanical axis and overall limb alignment after TKA is unclear.
We therefore addressed the following questions: (1) Does hindfoot alignment change after TKA for knee osteoarthritis? (2) What factors influence hindfoot alignment after TKA? (3) Does deviation of the mechanical axis from the center of the knee vary when the hindfoot is taken into account (ground mechanical axis) as compared with when it is not (ie, with the conventional mechanical axis) after TKA?
Patients and Methods
For this prospective study, we enrolled patients receiving primary computer-assisted TKAs performed for knee osteoarthritis from November 2007 to May 2008. During that time we operated on 128 patients (169 TKAs). We included every case of primary navigated TKA performed for primary osteoarthritis of the knee. We excluded patients with posttraumatic and rheumatoid arthritis of the knee, previous surgery, or fracture of the ankle or hindfoot, but included patients with abnormalities treated nonoperatively, such as planovalgus deformity of the foot. Based on the exclusion criteria, four TKAs were excluded from the study owing to rheumatoid arthritis, posttraumatic arthritis, and previous ankle and subtalar trauma or surgery, leaving 165 TKAs (40 simultaneous bilateral, 85 unilateral) performed in 125 patients (24 men, 101 women) for analysis. The mean age (± SD) of the patients at the time of surgery was 66.1 ± 9.5 years (range, 50–84 years). Twelve knees (7%) had valgus deformities and 153 knees had varus deformities preoperatively. One hundred twenty limbs (72%) had preoperative knee deformities less than 15° whereas 45 limbs (28%) had knee deformities of 15° or greater.
We assessed limb alignment, mechanical axis deviation (conventional and ground), and hindfoot alignment radiographically. For the two mechanical axis lines, instead of the term MADC (mechanical axis deviation conventional) line used by Guichet et al. [5], we have used conventional mechanical axis (CMA), and instead of MADG (mechanical axis deviation ground) line we have used the term ground mechanical axis (GMA). Subsequently we have termed the deviations measured using these two axes as CMAD instead of MADC and GMAD instead of MADG. Despite the difference in terminology, these denote the same things as described by Guichet et al. [5].
For plotting the ground mechanical axis and measuring the ground mechanical axis deviation, all standing full-length AP radiographs were taken using the wire technique described by Guichet et al. [5], in which a flexible metal wire is secured around the plantar surface of the heel to both malleoli (Fig. 1). To account for magnification during radiography, all full-length radiographs were taken using the scaled radiographic technique. A marker stand (OrthoRxTM; DePuy Orthopaedics Inc, Warsaw, IN, USA) consisting of three metal beads fixed to a radiolucent stand was placed at the midline of the bones of the affected knee. The inner distance between the two farthest metal beads was 90 mm. This known length was used to adjust for magnification for preoperative and postoperative radiographs. The hindfoot alignment was assessed with the help of a weightbearing modified Cobey’s view (Fig. 1). This radiograph was obtained with the patient standing on a radiolucent platform, with the radiographic beam angled from behind at an angle of 15° downward from the horizontal plane [3].
Fig. 1A–D.
(A) A preoperative hip to ankle full-length standing radiograph shows a left knee varus arthritic deformity of 16° (HKA angle = 164°). The conventional (straight line) and ground (dotted line) mechanical axes are overlapping with no difference in deviation. (B) A preoperative Cobey’s view of the ankle of the same patient shows hindfoot alignment of 6° valgus. (C) A postoperative hip to ankle full-length standing radiograph after TKA shows a fully corrected left knee alignment (HKA angle = 180°). The conventional mechanical axis (straight line) passes through the center of the knee whereas the ground mechanical axis (dotted line) passes approximately 9.5 mm lateral to the center of the knee. (D) A postoperative Cobey’s view of the ankle shows a hindfoot alignment of 4° valgus.
All TKAs were performed by one surgeon (AM) using the image-free Ci Navigation System (Brainlab, Munich, Germany). An anterior longitudinal incision and a medial parapatellar arthrotomy were used. All patients underwent TKA using a cemented, posterior cruciate-substituting design and all patients had resurfacing of the patella. During navigation, registration was performed in the standard fashion after insertion of two pins in the proximal tibia and distal femur to which arrays with three reflector spheres were affixed. The mechanical axis of the lower limb was obtained by navigation, using the center of femoral rotation, the malleoli, and the center of the intercondylar notch. Conventional cutting blocks were navigated into position to perform the appropriate bone cuts. The degree of soft tissue release was governed by the amount of soft tissue tightness assessed using a tensioning device and medial and lateral gap imbalance as quantified by the computer. Medial release for varus knees and lateral release for valgus knees were performed to achieve rectangular balanced gaps and a fully restored mechanical axis. All procedures were performed with the tourniquet inflated; the tourniquet was deflated after the cement had hardened.
The patients were followed up at 2 weeks and 6 weeks postoperatively when a clinical examination was performed to determine ROM of the knee or any residual extensor lag or flexion deformity requiring further physiotherapy. Subsequently, the patients were followed up at 3 months, 6 months, 1 year, and every year thereafter. All radiographs, as described above for the study, were taken preoperatively and repeated at 6 weeks postoperatively. Thereafter, during followup, the patients were assessed using only AP and lateral radiographs of the knee. The full-length lower limb radiographs were analyzed by one orthopaedic surgeon (GMS) and the ankle radiographs were analyzed by another orthopaedic surgeon (AM) blinded to the amount of knee deformity.
All digital radiographic images were analyzed using the Image J image processing and analysis software (Version 1.41; US National Institutes of Health, Bethesda, MD, USA). The center of the femoral head was determined using Moses circles, the center of the knee was taken as the center of the tibial spines, and the midpoint of the tibial plafond was considered the center of the ankle. For radiographic evaluation, two types of limb axes were used: CMA and GMA. The CMA was drawn from the center of the femoral head to the center of the ankle. For the GMA, the ground reaction point was first marked on the wire below the heel as the midpoint of the flat part of the wire in contact with the ground (Fig. 1A). The axis then was drawn from the center of the femoral head to the ground reaction point. The following parameters were measured using preoperative and postoperative radiographs (Fig. 1): (1) HKA angle for limb alignment measured as the angle between the mechanical axis of the femur (from the center of the femoral head to the center of the knee) and the mechanical axis of the tibia (from the center of the knee to the center of the ankle); (2) CMA deviation (CMAD) as the perpendicular distance from the center of the knee to the CMA; (3) GMA deviation (GMAD) as the perpendicular distance from the center of the knee to the GMA; and (4) tibiocalcaneal angle (TCA) for hindfoot alignment measured as the angle between the middiaphyseal line of the distal tibia and the long axis of the calcaneus on a modified Cobey’s view.
Data from the study sample of 165 TKAs were tested for normal distribution using the Kolmogorov-Smirnov test which showed that the data did not have normal distribution. Therefore, the nonparametric Wilcoxon signed ranks test was used for statistical comparison between the preoperative and postoperative data. Preoperative and postoperative hindfoot alignment was compared for knee deformity groups based on preoperative HKA angle (ie, HKA angle < 195° or > 165°, HKA angle ≥ 195° or ≤ 165°, HKA angle ≤ 180°, and HKA angle > 180°). To determine the effect of hindfoot alignment on postoperative limb alignment after TKA, the mean CMAD and GMAD in various knee deformity groups were compared preoperatively and postoperatively. Postoperatively, the CMAD and GMAD were compared in limbs aligned to HKA angles within ± 1° of neutral and within ± 3° of neutral. Correlation was determined between preoperative knee and hindfoot alignment, postoperative knee and hindfoot alignment, preoperative and postoperative hindfoot alignment, and difference between pre- and postoperative HKA angle and TCA using Spearman’s correlation test. Statistical analysis was performed using SPSS® Version 14 statistical software (SPSS Inc, Chicago, IL, USA).
Results
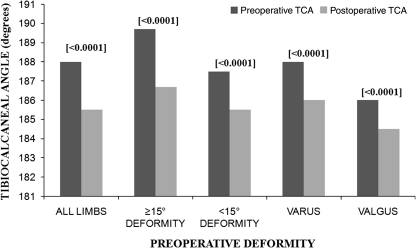
Preoperative hindfoot valgus alignment (TCA) decreased (p = < 0.001) after TKA. Regardless of the preoperative HKA subgroup (ie, HKA angle < 195° or > 165°, HKA angle ≥ 195° or ≤ 165°, HKA angle ≤ 180°, and HKA angle > 180°) the preoperative hindfoot valgus decreased after TKA (Fig. 2). Preoperatively, 96% of limbs had hindfoot valgus (> 180°) and six limbs (4%) had hindfoot varus (≤ 180°). Postoperatively, 87% of limbs had hindfoot valgus whereas 13% had hindfoot alignment in varus (Table 1).
Fig. 2.
A comparison of the median preoperative and postoperative TCAs based on knee deformity subgroups (HKA angle) is shown. p Values are shown in brackets.
Table 1.
Preoperative and postoperative values of various parameters in limbs based on preoperative knee deformity (HKA angle) groups
| Group | Number | Time | HKA angle (°) | CMAD (mm) | GMAD (mm) | TCA (°) |
|---|---|---|---|---|---|---|
| All limbs | 165 | Preoperative | 170 (152–201) | +34.3 (−91 to +98) | +31 (−102 to +98) | 188 (160–203) |
| Postoperative | 180 (170–185) | 0 (−17 to +28) | −6 (−24 to +20) | 185.5 (173–200) | ||
| < 195° or > 165° (< 15° varus or valgus) | 121 | Preoperative | 171.5 (165.5–194) | +28 (−43 to +52.3) | +25 (−50 to +50) | 187.5 (160–203) |
| Postoperative | 180 (176.5–185) | −6.8 (−17 to +28) | −23 (−24 to +20) | 185.5 (173–200) | ||
| ≥ 195° or ≤ 165° (≥ 15° varus or valgus) | 44 | Preoperative | 164 (152–201) | +53.3 (−91 to +98) | +49.5 (−102 to +98) | 189.7 (175–200) |
| Postoperative | 180 (177–183) | 0 (−8.7 to +12) | −5 (−15.3 to +10.6) | 186.7 (178–199) | ||
| ≤ 180° (varus) | 153 | Preoperative | 169.5 (152–180) | +35.6 (−12 to +98) | +32 (−20 to +98) | 188 (175–203) |
| Postoperative | 180 (176.5–185) | −6.8 (−17 to +28) | −22.4 (−24 to 20) | 186 (173–200) | ||
| > 180° (valgus) | 12 | Preoperative | 187.5 (180.5–201) | −59.7 (0 to −91) | −73.3 (−10.6 to −102) | 186 (160–199) |
| Postoperative | 180.7 (180–183) | 0 (+6 to −11) | −6.9 (+5 to −16.3) | 184.5 (173–198) |
Values expressed as median (range); negative values for CMAD and GMAD indicate lateral deviation of mechanical axis at knee, positive values indicate medial deviation; HKA angle = hip-knee-ankle angle, CMAD = conventional mechanical axis deviation; GMAD = ground mechanical axis deviation; TCA = tibiocalcaneal angle.
Only preoperative hindfoot alignment influenced hindfoot alignment after TKA. The preoperative TCA correlated with (rho = 0.58; p < 0.001) the postoperative TCA. We observed no correlation between preoperative HKA angle and postoperative TCA, postoperative HKA angle and postoperative TCA, and difference between pre- and postoperative HKA angle and postoperative TCA.
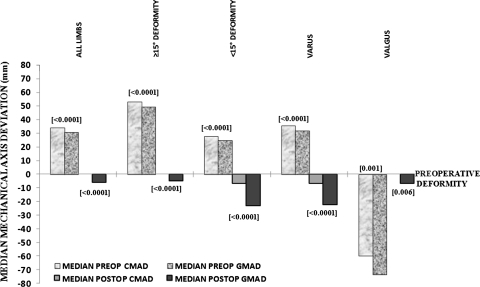
The CMA showed less deviation from the center of the knee than the GMA, which was laterally deviated after TKA. This difference in deviation between the two axes was significant in all limbs regardless of preoperative HKA subgroup (Fig. 3). Postoperatively, in 47% of limbs, the difference between CMAD and GMAD was less than 5 mm; in 48%, it was between 5 and 10 mm; and in 5%, it was 10 mm or greater. Similarly, in knees with postoperative HKA angles within ± 1° of neutral (82 of 165 limbs) and in knees with postoperative HKA angles within ± 3° of neutral (159 of 165 limbs), the CMA was much closer (p < 0.001) to the center of the knee compared with the GMA, which showed lateral deviation. Distribution of limbs based on postoperative GMAD in knees with postoperative alignment within 1° and 3° from neutral showed the GMA deviated by 10 mm or greater from the center of the knee in 13% and 29% of the limbs, respectively (Fig. 4). Therefore, postoperatively, the GMA continued to fall laterally despite the CMA having been restored to within ± 1° or ± 3° of neutral, owing to hindfoot valgus.
Fig. 3.
A comparison of the median preoperative and postoperative CMAD and GMAD based on knee deformity subgroups (HKA angle) is shown. p Values are shown in brackets. Preop = preoperative; Postop = postoperative.
Fig. 4.
Distribution of limbs based on postoperative GMAD in knees with postoperative alignment within 1° and 3° from neutral is shown.
Discussion
For patients with rheumatoid arthritis, varus deformities of the knee may result in valgus alignment of the hindfoot and valgus knees may result in varus alignment of the hindfoot [8]. However, it is unknown what the alignment of the hindfoot is when the knee is deformed in patients with osteoarthritis and whether this hindfoot alignment changes after TKA. Hindfoot alignment is a part of the weightbearing axis or the GMA of the lower limb. How this hindfoot alignment influences limb alignment after TKA has not been studied. Our rationale was that a substantial number of patients may have hindfoot valgus alignment, which may influence the overall weightbearing axis despite having accurately restored the CMA of the limb after TKA. We sought answers to the following questions: (1) Does hindfoot alignment change after TKA for knee osteoarthritis? (2) What factors influence hindfoot alignment after TKA? (3) Does deviation of the mechanical axis from the center of the knee vary when the hindfoot is taken into account (ground mechanical axis) as compared with when it is not (ie, with the conventional mechanical axis) after TKA?
Our study has some limitations. First, this is a radiographic study in which improper radiographic technique may be a source of error. We tried to minimize this source of error by using the scaled radiographic technique to account for any error attributable to image magnification. The wire technique used to mark the ground reaction point and to draw the GMA fixes a point in the soft tissue and not the center point of the calcaneus. However, taking the center point of calcaneus to plot the GMA is difficult in a full-length lower limb radiograph in which the calcaneus is not clearly observed. Therefore, the wire technique may be less prone to error. Second, this radiographic study gives a static picture of the behavior of the hindfoot in patients who undergo TKA. Although not an aim of this study, including a dynamic study such as gait analysis would have added additional information regarding the change in alignment of the hindfoot after TKA in these patients. However, facilities for such dynamic analysis are not readily available, and are difficult to perform in large numbers of patients due to logistic constraints. Third, the hindfoot malalignment seen in patients with knee osteoarthritis in our study should be assessed and differentiated based on the etiopathogenesis (flexible compensatory malalignment secondary to knee deformities and primary flexible or rigid hindfoot deformities). This may help in predicting any change that may occur in hindfoot malalignment after TKA. Flexible hindfoot deformities may be more likely to improve after TKA whereas rigid hindfoot deformities may not improve and may require orthotic or surgical correction. This was not an aim of the current study and needs further evaluation.
From our study, it appears that varus deformity at the knee is associated with valgus hindfoot. Hindfoot valgus alignment decreased after TKA when compared with preoperative alignment. Despite this decrease in hindfoot valgus, 87% of the hindfeet continued to have valgus alignment after TKA. Chandler and Moskal [2], in a similar prospective analysis of hindfoot alignment after 86 TKAs, reported larger varus knee deformities (based on femorotibial anatomic axis) were associated with neutral or valgus hindfoot alignment. They also reported, on average, the hindfoot alignment changes postoperatively by ½ of the total degrees. In contrast to our study, their study had fewer patients, with knees that had lesser degrees of deformity, and the deformity was measured using the femorotibial anatomic axis.
The only factor that positively correlated with postoperative hindfoot alignment was the preoperative hindfoot alignment. Chandler and Moskal [2] similarly reported a relationship between alignment of the foot before and after TKA. In their study, the mean change in hindfoot alignment was 50% after TKA and the larger preoperative deformities had the most postoperative change. We observed a change of approximately 31% in hindfoot alignment after TKA compared with preoperative alignment. This difference in results may be attributable to the relatively larger number of knees with a greater degree of deformity in our study.
Preoperatively, we observed a difference between the CMAD and GMAD and this trend continued even after TKA, when we observed that the GMAD was greater than the CMAD. This could be attributable to the fact that, although the deformity was fully corrected at the knee and the CMA was restored to within 3° of neutral in 97% of the limbs, hindfoot valgus persisted in the majority of the limbs. In knees that had postoperative alignment (HKA angle) within ± 1° of neutral and within ± 3° of neutral, the postoperative GMAD was 10 mm or greater in 13% and 29% of limbs, respectively. Therefore, the GMA continued to show lateral deviation postoperatively. We found no published studies analyzing the effect of hindfoot alignment on postoperative limb alignment after TKA. However, Meding et al. [7], in their analysis of revisions performed in cruciate-retaining TKA, found a high incidence of associated tibialis posterior tendon insufficiency and hindfoot valgus. This could have been attributable to the alteration in mechanical axis caused by the associated hindfoot deformity. Therefore, the effect of lateral deviation of the GMA in the presence of hindfoot valgus after TKA needs to be evaluated further. This raises the question regarding whether varus arthritic knees with hindfoot valgus undergoing TKA should be undercorrected and valgus knees with hindfoot valgus overcorrected so that the GMA ultimately passes through the center of the knee to prevent eccentric loading of the implant and perhaps to confer a more normal gait. If hindfoot deformity is flexible, correction of knee arthritis with TKA may cause a decrease in the hindfoot deformity. However, a change in hindfoot deformity after TKA may not occur if the deformity is rigid. This may result in the rigid hindfoot deformity causing severe lateral deviation of the GMA after TKA. Therefore, the surgeon may wish to consider corrective surgery for a rigid hindfoot deformity before performing TKA. This would need to be discussed with the patient who likely presented to the surgeon primarily for knee pain.
We found that varus osteoarthritic knees were associated with hindfoot valgus. Although hindfoot valgus alignment decreased after TKA when compared with before surgery, 87% of the hindfeet continued to have valgus alignment. Postoperatively, the mean CMAD was less than the mean GMAD, with the GMA falling laterally despite the CMA having been restored to within ± 1° or ± 3° of neutral, attributable to hindfoot valgus. Complete restoration of limb alignment in arthritic knees after TKA may be associated with persistent hindfoot valgus alignment, with the GMA passing lateral to the center of the knee. Our data suggest the hindfoot should be evaluated carefully in patients who undergo TKA and measures may be warranted to align the GMA as close to the limb mechanical axis as possible.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Breach Candy Hospital.
References
- 1.Bouysset M, Hugueny P. The rheumatoid foot: pathomechanics, clinical and radiological features. Therapeutic conditions. In: Bouysset M, Tourne Y, Tillmann K, editors. Foot and Ankle in Rheumatoid Arthritis. Paris, France: Springer Verlag; 2006. pp. 9–48. [Google Scholar]
- 2.Chandler JT, Moskal JT. Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: a prospective analysis. J Arthroplasty. 2004;19:211–216. doi: 10.1016/j.arth.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Cobey JC, Sella E. Standardizing methods of measurement of foot shape by including the effects of subtalar rotation. Foot Ankle. 1981;2:30–36. doi: 10.1177/107110078100200106. [DOI] [PubMed] [Google Scholar]
- 4.Desai SS, Shetty GM, Song HR, Lee SH, Kim TY, Hur CY. Effect of foot deformity on conventional mechanical axis deviation and ground mechanical axis deviation during single leg stance and two leg stance in genu varum. Knee. 2007;14:452–457. doi: 10.1016/j.knee.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Guichet JM, Javed A, Russell J, Saleh M. Effect of the foot on the mechanical alignment of the lower limbs. Clin Orthop Relat Res. 2003;415:193–201. doi: 10.1097/01.blo.0000092973.12414.ec. [DOI] [PubMed] [Google Scholar]
- 6.Lee ST, Song HR, Mahajan R, Makwana V, Suh SW, Lee SH. Development of genu varum in achondroplasia: relation to fibular overgrowth. J Bone Joint Surg Br. 2007;89:57–61. doi: 10.1302/0301-620X.89B1.18223. [DOI] [PubMed] [Google Scholar]
- 7.Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME, Malinzak RA. The planovalgus foot: a harbinger of failure of posterior cruciate-retaining total knee replacement. J Bone Joint Surg Am. 2005;87(suppl 2):59–62. doi: 10.2106/JBJS.E.00484. [DOI] [PubMed] [Google Scholar]
- 8.Souter WA. Surgical strategy in surgery of the lower limb in rheumatoid arthritis. In: Bouysset M, Tourne Y, Tillmann K, editors. Foot and Ankle in Rheumatoid Arthritis. Paris, France: Springer Verlag; 2006. pp. 229–236. [Google Scholar]