Abstract
Background
Primary metatarsalgia of the lesser metatarsals is common and caused by mechanical overload of the affected metatarsal heads. Increased metatarsal length generally is believed to be a factor in the development of primary metatarsalgia. However, there is no clear biomechanical evidence supporting this theory.
Questions/purposes
We asked whether metatarsal length correlated with plantar-loading parameters under the corresponding metatarsal heads.
Patients and Methods
We prospectively followed two groups of patients 46 (51 feet) with and 45 (51 feet) without metatarsalgia. Each foot was physically examined and underwent standardized full-weightbearing radiography and dynamic pedobarography to assess maximal peak pressure and maximal force under the first, second, and third metatarsal heads. We correlated the relative length of the first and third metatarsals with the corresponding two plantar-loading parameters. We compared maximal peak pressure and maximal force in patients with metatarsalgia with those of symptom-free patients.
Results
The relative length of the first and third metatarsals did not correlate (r < 0.13) with the maximal peak pressure or maximal force under the corresponding metatarsal heads. Maximal force under the first metatarsal head was decreased in the metatarsalgia group. There was no difference in maximal peak pressure between the metatarsalgia and nonmetatarsalgia groups.
Conclusions
Relative metatarsal length had no influence on plantar-loading parameters. Shortening of a symptomatic ray to decrease plantar-loading parameters cannot be supported from a biomechanical rationale.
Introduction
The ideal forefoot morphology is a concept developed by Maestro et al. [14] to facilitate planning of forefoot osteotomies. They defined a “harmonious morphotype,” which should assure physiologic function and weight distribution by studying radiographs of symptomatic and asymptomatic forefeet, and concluded increased metatarsal length predisposes to pain and calluses on the plantar side of the metatarsal heads. These symptoms are known as metatarsalgia and are commonly seen [7, 8]. Primary metatarsalgia is caused by mechanical overload of the affected metatarsal heads [7, 8]. Increased metatarsal length generally is believed to be a factor in the development of primary metatarsalgia [1, 7, 14, 15]. Nonoperative treatment consists of using molded insoles that include padding just proximal to the metatarsal heads.
For patients with insufficient pain relief, surgery frequently is recommended [1, 7, 8, 13, 15]. Some surgeons prefer metatarsal shortening osteotomies (eg, Weil’s osteotomy) to achieve a harmonious forefoot morphotype and to improve weight distribution under the metatarsal heads [1, 7]. Maestro et al. [14] recommended correction of only the symptomatic ray as far as the operation does not lead to an “inharmonious morphotype.” In these cases, they also recommended shortening of the adjacent asymptomatic rays.
Despite the fact that this theory has gained wide acceptance among numerous foot surgeons [1, 7, 14, 15], it is still unclear whether metatarsal length has an effect on biomechanical parameters. In an experimental cadaver study, dorsiflexion osteotomies decreased maximal peak pressure on the first metatarsal head [11] but additional shortening of 5 and 10 mm had no additional effect. In one study, the plantar loading parameters of 45 feet of patients treated by dorsal wedge osteotomy were compared with those of 29 symptom-free contralateral feet [6]. The patients with metatarsalgia had increased maximal peak pressure and increased plantar flexion of the metatarsal heads of the symptomatic rays. A substantial decrease of maximal peak pressure after the operation led to an improvement of the symptoms in the metatarsalgia group. Dreeben et al. found no correlation between the length of the metatarsals and plantar-loading parameters or symptoms [6]. According to these findings, we consider the concept of harmonious and inharmonious foot morphotypes determined by the relative metatarsal length as questionable. There is currently no evidence that increased metatarsal length influences biomechanical parameters and predisposes for primary metatarsalgia.
We therefore asked whether metatarsal length correlated with plantar-loading parameters under the corresponding metatarsal heads.
Patients and Methods
Between January 1 and May 31, 2009, we prospectively followed all patients presenting to our outpatient clinic with weightbearing pain and/or plantar hyperkeratoses (calluses) under a lesser metatarsal head. All patients were examined by the same foot surgeon (CW). For this study we excluded patients with conditions such as fixed-foot deformities, forefoot malalignment (pes cavus, pes planus, hallux valgus, hammertoes/claw toes), previous foot surgery or major trauma, diabetes mellitus, rheumatic diseases, and nerve entrapment (eg, Morton’s neuroma). We also excluded patients who had a period of nonsurgical treatment (eg, molded insoles). With these exclusions we had 46 patients (51 feet) with symptoms longer than 4 weeks without remission under analgesic medication. All patients received standardized full-weightbearing radiographs in the AP and lateral views and underwent dynamic pedobarography. As control subjects, we enrolled all patients presenting to our outpatient clinic between January 1 and May 31, 2009 with achillodynia or plantar fasciitis. All patients were examined by the same foot surgeon (CW). For the control patients we excluded those with any additional forefoot and midfoot complaints and those with conditions such as fixed-foot deformities, forefoot malalignment (pes cavus, pes planus, hallux valgus, hammertoes/claw toes), previous foot surgery or major trauma, diabetes mellitus, rheumatic diseases, and nerve entrapment (eg, Morton’s neuroma); we also excluded patients who wore molded insoles for a period of time. We included only patients who experienced complete pain relief within 8 weeks after analgesic medication, stretching exercises, and cold application. With these exclusions, we had 45 patients in the control group. All patients received standardized full-weightbearing radiographs in the AP and lateral views and underwent dynamic pedobarography. The mean age of the 46 patients with metatarsalgia was 53.6 years; there were 31 women and 15 men and 31 right and 20 left feet. In the symptom-free control group, we included 45 patients (51 feet) with a mean age of 52.2 years; there were 29 women and 16 men and 24 right and 27 left feet. Study protocols were approved by the local ethics committee.
We performed weightbearing AP radiographs using a template to ensure standardized placement of the foot with respect to the cassette and the xray beam. A radiopaque scale was placed beneath the xrayed foot as a reference marker. The radiographs were converted into JPEG files using a flatbed scanner (CanoScan Lide 20; Canon Inc, Tokyo, Japan). After electronic calibration, one investigator (CW) determined the length of the second metatarsal using a MATLAB® graphic tool (MATLAB® Version 2007/B; The MathWorks Inc, Natick, MA, USA). He determined the second metatarsal axis and drew a perpendicular reference line through the tip of the second metatarsal head according to the method of Maestro et al. [14] (Fig. 1). He measured the distance from this reference line to the tips of the first and third metatarsals and calculated the relative length in relation to the second metatarsal.
Fig. 1.

Electronic metatarsal length measurement is shown.
Dynamic pedobarography was performed using the EMED-SF® pressure platform (Novel GmbH, Munich, Germany) with a spatial resolution of four sensors per cm2. Measurements at 50-Hz sample frequency were used to obtain barefoot plantar pressures. Each subject was tested using the two-step method in which platform contact was made on the second step after initiation of gait [4, 5]. The reliability of this method was reported previously and led to preferential use in research and clinical settings [3]. The subjects walked at self-selected speeds. Before data acquisition, each subject was given the opportunity to practice walking across the pressure-sensitive platform. Thereafter, five repeated trials were recorded and the median was calculated for further analysis. By automated masking, the plantar pressure map of the foot was divided into 12 anatomic regions that corresponded to the heel, the midfoot, each of the five metatarsal heads, and all five toes (Fig. 2). In this study, maximal peak pressure and maximal force under the first, second, and third metatarsal heads were determined. During stance phase, the plantar pressure was measured continuously by all sensors of the pressure platform. The most increased pressure measurement in one defined region represented the maximal peak pressure. According to previous studies, maximal peak pressure directly correlates with the risk for developing mechanical-induced forefoot complaints [2, 16]. Maximal force was the most increased force in one defined anatomic region (F = p/A). According to a previous study, maximal force is the most import biomechanical parameter of the foot’s function [10].
Fig. 2.
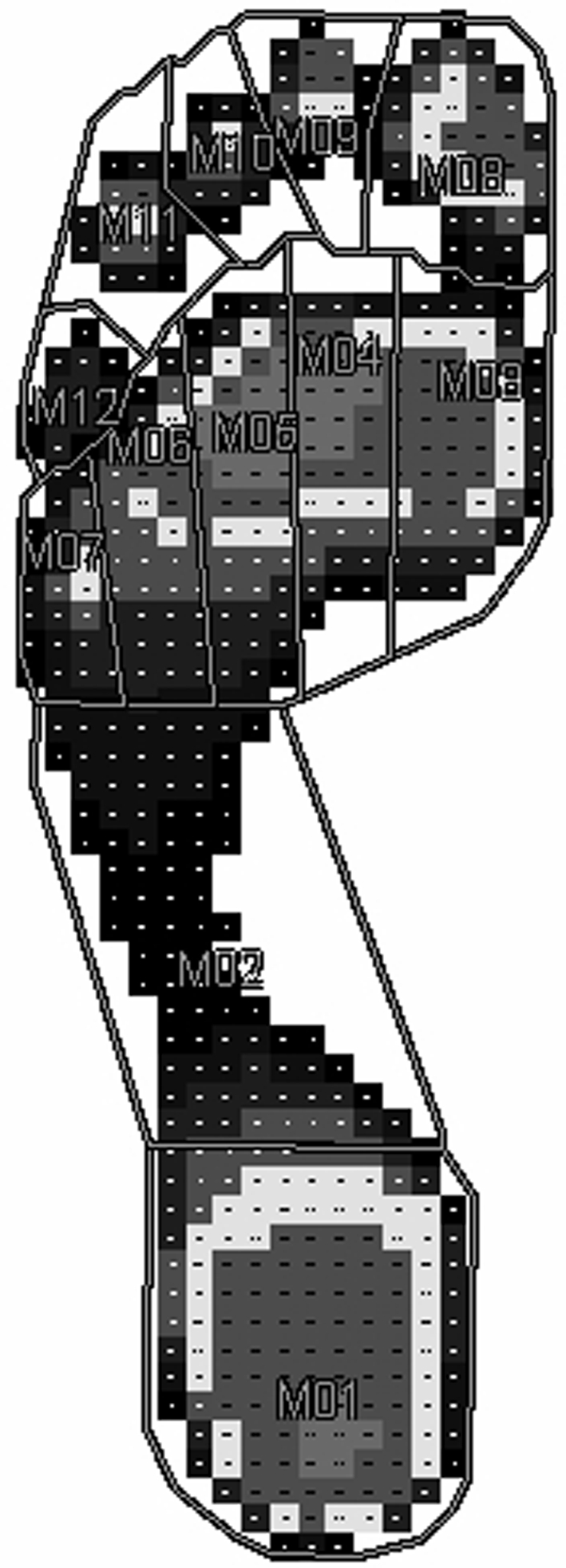
For dynamic pedobarography, the plantar pressure map was divided into 12 anatomic regions.
To ensure that our data were representative for a larger study population we compared our force/time curves with those from a previously published study that included 42 patients [9]. Plantar-loading parameters of our patients showed no differences compared with the population of that study.
To assess the correlation between metatarsal length and plantar-loading parameters, we pooled the data for patients with metatarsalgia and symptom-free control subjects. The Spearman’s rank correlation coefficient (R) was calculated for the relative metatarsal length with maximal peak pressure and maximal force under the corresponding metatarsal head. Comparisons of plantar-loading parameters between the metatarsalgia and control groups were performed using the Wilcoxon rank-sum test. Comparisons of gender and age between groups were performed using the Wilcoxon rank-sum test and the chi square test. All calculations were performed using MATLAB® software.
Results
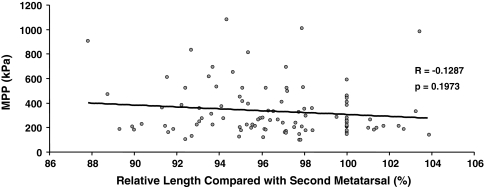
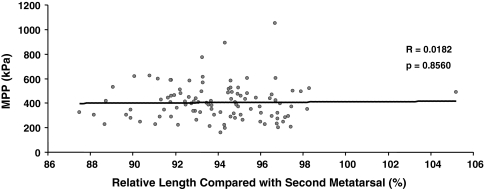
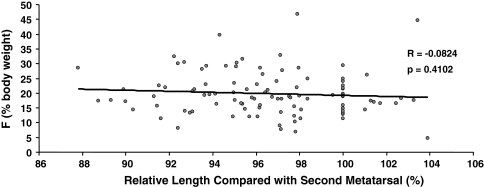
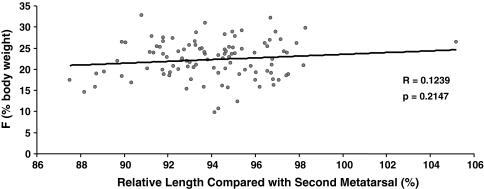
Relative length of the first and third metatarsals (compared with the second metatarsal) did not correlate with maximal peak pressure (first metatarsal: Fig. 3; third metatarsal: Fig. 4) and maximal force (first metatarsal: Fig. 5; third metatarsal: Fig. 6). The corresponding Spearman’s rank correlations coefficients (R) ranged from 0.0182 to 0.1708.
Fig. 3.
A graph shows correlation of maximal peak pressure (MPP) and relative length of the first metatarsal (compared with the second metatarsal). There was no correlation (R = −0.1287; p = 0.1973) between maximal peak pressure and relative length of the first metatarsal.
Fig. 4.
A graph shows correlation of maximal peak pressure (MPP) and relative length of the third metatarsal (compared with the second metatarsal). There was no correlation (R = 0.0182; p = 0.8560) between maximal peak pressure and relative length of the third metatarsal.
Fig. 5.
A graph shows correlation of maximal force (F) and relative length of the first metatarsal (compared with the second metatarsal). There was no correlation (R = −0.0824; p = 0.4102) between maximal force and relative length of the first metatarsal.
Fig. 6.
A graph shows correlation of maximal force (F) and relative length of the third metatarsal (compared with the second metatarsal). There was no correlation (R = 0.1239; p = 0.2147) between maximal force and relative length of the third metatarsal.
Maximal force under the first metatarsal head (F1) was decreased (p = 0.0076) in the metatarsalgia group (Table 1). There was no difference in maximal peak pressure between the metatarsalgia and control groups.
Table 1.
Dynamic pedobarographic data
| Group | L2 (mm) | MPP1 (kPa) | MPP2 (kPa) | MPP3 (kPa) | F1 (% body weight) | F2 (% body weight) | F3 (% body weight) |
|---|---|---|---|---|---|---|---|
| Patients with metatarsalgia (n = 46) | 80.34 (± 6.85) | 314.87 (± 214.71) | 505.49 (± 220.34) | 406.40 (± 119.96) | 18.38 (± 7.91) | 22.27 (± 4.66) | 22.85 (± 4.47) |
| Healthy control subjects (n = 45) | 82.45 (± 5.56) | 353.57 (± 201.05) | 448.83 (± 206.44) | 404.08 (± 168.47) | 21.36 (± 6.51) | 21.05 (± 5.03) | 21.70 (± 4.49) |
| p Value | 0.0906 | 0.1004 | 0.2071 | 0.5359 | 0.0076 | 0.2348 | 0.3680 |
Data are presented as mean (±SD); L2 = absolute length of the second metatarsal; MPP1, 2, 3 = maximal peak pressure under metatarsal heads 1 to 3; F1, 2, 3 = maximal force under metatarsal heads 1 to 3.
Discussion
Primary metatarsalgia of the lesser metatarsals is common and presumed caused by mechanical overload of the affected metatarsal heads [7, 8]. A commonly noted theory suggests increased metatarsal length is a factor in the development of metatarsalgia [1, 7, 14, 15]. However, there is no biomechanical evidence to support this theory. We therefore asked whether metatarsal length correlated with plantar-loading parameters under the corresponding metatarsal heads.
This study has some limitations. First, despite our efforts to include only patients with primary, mechanically mediated metatarsalgia in the study, a coincidence of an inflammatory/rheumatic etiology (secondary metatarsalgia) cannot be ruled out in every subject. There are no standardized diagnostic criteria for primary and secondary metatarsalgia in the literature [7, 8, 15]. As a consequence the differentiation of etiologies is arbitrary and depends on the clinical experience of the examiner. We tried to overcome the problem by excluding all patients with diabetes mellitus, rheumatic diseases, and nerve entrapment (eg, Morton’s neuroma). Second, we pooled the biomechanical data of symptomatic and asymptomatic rays of patients with metatarsalgia. We included subjects with isolated metatarsalgia (eg, only the second or third ray) and those with multiple regions (eg, second, third, and fourth rays were symptomatic). Including only patients with isolated metatarsalgia would have resulted in a more homogeneous study population. In our opinion this limitation would not influence our main finding in the first part of the study. We mathematically assessed the relation of two biomechanical parameters and objectively determined metatarsal length and maximal peak pressure/maximal force according to standardized protocols. We studied a large population obtained by pooling symptomatic patients with metatarsalgia and asymptomatic control subjects. We found no correlation between metatarsal length and maximal peak pressure/maximal force in this study population. We consider this finding as an objective biomechanical statement independent from subjective factors like pain under one or multiple metatarsal heads. However, in the second part of the study, we assessed potential differences in plantar-loading parameters of patients with metatarsalgia and symptom-free control subjects. Those group comparisons may be compromised by the second limitation. In this study we found decreased maximal force under the first metatarsal head in patients with metatarsalgia. It is possible that additional differences in plantar-loading parameters were not detected owing to our heterogeneous study population. In our opinion, additional studies including only patients with isolated metatarsalgia are needed to confirm our findings. Third, owing to reasons of reproducibility we defined the anatomic regions of the pressure map by automated masking. As a result the masks of all metatarsals are not limited to the metatarsal heads but extend to the whole length of the metatarsals. There might be concerns that this influences our measurements. In this study, we assessed only maximal peak pressure and maximal force of the first, second, and third metatarsals. Both parameters occur during the push-off phase when only the toes and the metatarsal heads are loaded while the remaining midfoot and hindfoot are detached from the ground. In this phase only loaded sensors of the pressure platform provide pressure data. As a consequence maximal peak pressure measured in one metatarsal mask corresponds to the anatomic region of the loaded metatarsal head. Thus we believe our findings are not limited by the presence of the extended metatarsal pressure masks.
The main finding of this study is the absence of any correlation between metatarsal length and plantar-loading parameters in patients with metatarsalgia and symptom-free control subjects. This finding contradicts the common theory that increased length of a lesser metatarsal leads to increased weightbearing load under the metatarsal head and predisposes for primary metatarsalgia [1, 7, 14, 15]. Maestro et al. [14] conducted a forefoot morphotype study including 154 feet (50 hallux valgus and 30 hallux rigidus deformities, 84 feet of control subjects) and defined four different forefoot morphotypes depending on the position of the lateral sesamoid and the length of the lesser metatarsals. A “harmonious forefoot morphotype” was found in 31% of the study population. “Inharmonious forefoot morphotypes” were characterized by an increased length of the first or the lesser metatarsals. Based on their clinical experience, they stated relative metatarsal length disorders are a major factor of metatarsalgia [14]. This theory has gained acceptance [1, 7, 14, 15] even though there are no studies directly confirming a correlation between a metatarsal malalignment and increased incidence of degenerative forefoot diseases [8]. One study focused on radiographic and pedobarographic findings in patients with primary metatarsalgia [6]. Thirty-seven patients (45 feet) with a diagnosis of primary metatarsalgia were followed preoperatively and postoperatively, and 29 contralateral symptom-free feet were used as healthy controls. The authors found no correlation between morphologic features of the forefoot and the occurrence of metatarsalgia [6]. Preoperatively, no correlations were observed between the length of the symptomatic ray and the metatarsal height, plantar pressure, and symptoms. We also found no correlation between metatarsal length and plantar-loading parameters. Our data suggest prophylactic shortenings of asymptomatic rays to achieve an harmonious forefoot morphotype cannot be supported from a biomechanical rationale. However, are there any objective predisposing parameters for primary metatarsalgia? A possible factor may be increased plantar flexion of the metatarsal head. A clinical and biomechanical study showed patients with metatarsalgia had increased plantar-flexed heads of the symptomatic metatarsal (+1.6 mm/20%) compared with those of healthy control subjects [6]. Patients with no pain relief after the operation (dorsal wedge osteotomy) showed insufficient dorsiflexion of the symptomatic metatarsal head. This finding was partly supported by clinical and experimental hallux valgus studies [11, 17]. Dorsal wedge osteotomies of the first metatarsal led to decreased pain and plantar pressure under the first metatarsal head. In our study, there was no attempt to evaluate plantar flexion of the metatarsal heads. Additional studies are needed to provide biomechanical evidence for a correlation between increased plantar flexion of metatarsal heads and increased plantar pressure/force.
Our second finding is that maximal force under the first metatarsal head was decreased in the metatarsalgia group compared with the symptom-free control group. This finding is supported by several studies showing decreased plantar-loading parameters under the first ray but increased parameters under the symptomatic ray [6, 12, 17] of patients with metatarsalgia. As a consequence, some authors consider metatarsalgia primarily a mechanical problem [1, 12, 15]. These authors discussed a pathologic load-transfer mechanism from the first ray to the symptomatic rays of the lesser toes [1, 12, 15]. According to this theory, we would have expected increased plantar-loading parameters under the second and third metatarsal heads in the metatarsalgia group. This was not the case in our study. In our opinion, a load-transfer mechanism from the symptomatic second or third ray to the fourth and fifth rays could be responsible for this controversial finding. Patients with metatarsalgia could have shown slight supination in the forefoot to unload the symptomatic rays. Further kinematographic studies and assessment of plantar-pressure parameters of the fourth and fifth metatarsal heads are necessary to support this theory.
We found relative metatarsal length has no influence on maximal peak pressure and maximal force. We believe there is no objective biomechanical evidence supporting the theory that increased metatarsal length increases plantar-loading parameters under the metatarsal head and predisposes patients to the development of primary metatarsalgia.
Acknowledgments
We thank H.A.C. Jacob PhD, for important advice during biomechanical testing and for reviewing the manuscript. We also thank M.D. Zumstein MD, for his organisational support in conducting the study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Kantonsspital Aarau.
References
- 1.Barouk LS. [Weil’s metatarsal osteotomy in the treatment of metatarsalgia] [in German. Orthopade. 1996;25:338–344. doi: 10.1007/s001320050034. [DOI] [PubMed] [Google Scholar]
- 2.Boulton AJ, Hardisty CA, Betts RP, Franks CI, Worth RC, Ward JD, Duckworth T. Dynamic foot pressure and other studies as diagnostic and management aids in diabetic neuropathy. Diabetes Care. 1983;6:26–33. doi: 10.2337/diacare.6.1.26. [DOI] [PubMed] [Google Scholar]
- 3.Bryant A, Singer K, Tinley P. Comparison of the reliability of plantar pressure measurements using the two-step and midgait methods of data collection. Foot Ankle Int. 1999;20:646–650. doi: 10.1177/107110079902001006. [DOI] [PubMed] [Google Scholar]
- 4.Bus SA. Foot Deformity in Diabetic Neuropathy: A Radiological and Biomechanical Analysis [dissertation] Amsterdam, The Netherlands: University of Amsterdam; 2004. [Google Scholar]
- 5.Debrunner HU, Jacob HAC. [Biomechanics of the Foot] [in German] 2. Stuttgart, Germany: Enke; 1998. [Google Scholar]
- 6.Dreeben SM, Noble PC, Hammerman S, Bishop JO, Tullos HS. Metatarsal osteotomy for primary metatarsalgia: radiographic and pedobarographic study. Foot Ankle. 1989;9:214–218. doi: 10.1177/107110078900900502. [DOI] [PubMed] [Google Scholar]
- 7.Espinosa N, Maceira E, Myerson MS. Current concept review: metatarsalgia. Foot Ankle Int. 2008;29:871–879. doi: 10.3113/FAI.2008.0871. [DOI] [PubMed] [Google Scholar]
- 8.Fuhrmann RA, Roth A, Venbrocks RA. [Metatarsalgia: differential diagnosis and therapeutic algorithm] [in German]. Orthopade. 2005;34:767–768, 769–772, 774–775. [DOI] [PubMed]
- 9.Hayafune N, Hayafune Y, Jacob HAC. Pressure and force distribution characteristics under the normal foot during the push-off phase in gait. The Foot. 1999;9:88–92. doi: 10.1054/foot.1999.0518. [DOI] [Google Scholar]
- 10.Jacob HA. Forces acting in the forefoot during normal gait: an estimate. Clin Biomech (Bristol, Avon). 2001;16:783–792. doi: 10.1016/S0268-0033(01)00070-5. [DOI] [PubMed] [Google Scholar]
- 11.Jung HG, Zaret DI, Parks BG, Schon LC. Effect of first metatarsal shortening and dorsiflexion osteotomies on forefoot plantar pressure in a cadaver model. Foot Ankle Int. 2005;26:748–753. doi: 10.1177/107110070502600913. [DOI] [PubMed] [Google Scholar]
- 12.Kang JH, Chen MD, Chen SC, Hsi WL. Correlations between subjective treatment responses and plantar pressure parameters of metatarsal pad treatment in metatarsalgia patients: a prospective study. BMC Musculoskelet Disord. 2006;7:95. doi: 10.1186/1471-2474-7-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy JG, Deland JT. Resolution of metatarsalgia following oblique osteotomy. Clin Orthop Relat Res. 2006;453:309–313. doi: 10.1097/01.blo.0000229354.96996.3e. [DOI] [PubMed] [Google Scholar]
- 14.Maestro M, Besse JL, Ragusa M, Berthonnaud E. Forefoot morphotype study and planning method for forefoot osteotomy. Foot Ankle Clin. 2003;8:695–710. doi: 10.1016/S1083-7515(03)00148-7. [DOI] [PubMed] [Google Scholar]
- 15.O’Kane C, Kilmartin TE. The surgical management of central metatarsalgia. Foot Ankle Int. 2002;23:415–419. doi: 10.1177/107110070202300508. [DOI] [PubMed] [Google Scholar]
- 16.Veves A, Murray HJ, Young MJ, Boulton AJ. The risk of foot ulceration in diabetic patients with high foot pressure: a prospective study. Diabetologia. 1992;35:660–663. doi: 10.1007/BF00400259. [DOI] [PubMed] [Google Scholar]
- 17.Wanivenhaus A, Brettschneider W. Influence of metatarsal head displacement on metatarsal pressure distribution after hallux valgus surgery. Foot Ankle. 1993;14:85–89. doi: 10.1177/107110079301400206. [DOI] [PubMed] [Google Scholar]