Abstract
Background
Treatment of symptomatic spinoglenoid cysts has been controversial with options ranging from observation, to open excision, to arthroscopic decompression with or without labral repair. It has recently been suggested that isolated repair of SLAP lesions without cyst decompression can restore function in patients with spinoglenoid cysts and SLAP lesions.
Questions/purposes
We examined gains in external rotation strength after isolated SLAP repair versus SLAP repair and cyst decompression to ascertain if gains in external rotation strength are attributable to SLAP repair or cyst decompression.
Methods
We retrospectively reviewed external rotation strength of 12 patients: six with spinoglenoid cysts and Type II SLAP lesions who underwent arthroscopic SLAP repair and spinoglenoid cyst decompression and six with isolated SLAP lesions who underwent repair of the lesions. Preoperative and postoperative external rotation strength was evaluated using a digitally calibrated dynamometer on the operative and nonoperative sides. The minimum followup was 12 months (mean, 15.2 months; range, 12–27 months).
Results
All of the patients in both cohorts had preoperative external rotation weakness on physical examination and dynamometer testing. The average increase in external rotation strength in the group of patients with SLAP lesions and paralabral cysts was 40% of the contralateral side versus 10% for the cohort with isolated SLAP repairs.
Conclusions
Decompression of paralabral cysts and SLAP repair in patients with preoperative external rotation weakness resulted in greater strength improvement than in patients with isolated SLAP repairs without complications of suprascapular neuropathy. This suggests that gains in external rotation strength are likely mostly attributable to cyst decompression, questioning isolated SLAP repair in the treatment of patients who have primarily weakness with spinoglenoid cysts.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
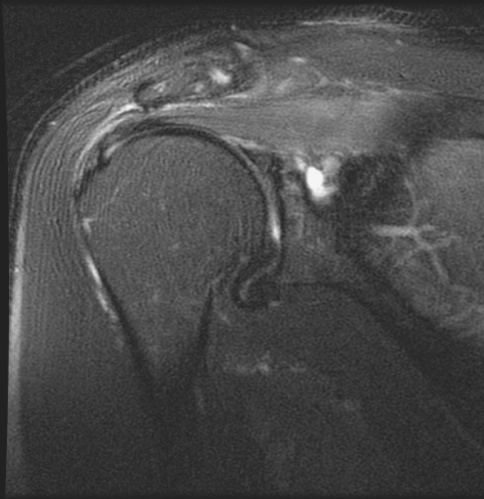
A paralabral ganglion cyst is uncommon but when they arise in the spinoglenoid notch, they may lead to nerve compression and substantial shoulder dysfunction [4]. Suprascapular nerve entrapment at the suprascapular notch was documented as early as 1959 by Koppell and Thompson [9]. In 1981, Ganzhorn et al. described entrapment at the spinoglenoid notch producing isolated weakness of the infraspinatus [6]. Recent investigations have increasingly recognized that the presence of a ganglion cyst adjacent to the superior labrum may cause suprascapular nerve compression at the spinoglenoid notch [2, 5, 13, 15] (Fig. 1).
Fig. 1.
A coronal T1-weighted MRI image demonstrates a cyst in the spinoglenoid notch.
Treatment options of symptomatic spinoglenoid cysts have varied from observation, to open excision, to arthroscopic decompression with or without labral repair [1–3, 5, 7, 10–14, 19]. Drainage under ultrasound, MRI, or CT guidance is effective in decompressing the cyst but does not address the underlying etiology of the cyst. Without labral repair, cyst formation often recurs [11, 13, 17, 18, 20]. Previous studies have established the pathophysiology and recommended a treatment algorithm for treatment of this condition [8, 13]. These studies recommend an initial trial of nonoperative management for patients with weakness and spinoglenoid notch cysts followed by arthroscopic cyst decompression and repair of SLAP (superior labral anterior posterior) lesions if the patients are still symptomatic, although the duration of nonoperative treatment was not specified. We treat patients with evidence of suprascapular nerve dysfunction and MRI documentation of both a spinoglenoid cyst and Type II (SLAP) lesion who have failed nonoperative management (consisting of antiinflammatory drugs, activity modification, and physical therapy) with arthroscopic decompression of the cyst and superior labral repair.
There has been recent controversy as a result of studies that suggest isolated SLAP repair in patients with both spinoglenoid cysts and SLAP lesions results in high patient satisfaction [16]. We question whether SLAP repair alone in patients with substantial weakness from isolated SLAP lesions would result in similar increases in strength compared to cyst decompression with SLAP repair.
The purpose of our study was to determine gains in external rotation strength after cyst decompression and SLAP repair versus isolated SLAP repair in a subgroup of patients without spinoglenoid notch cysts.
Patients and Methods
We retrospectively identified from the hospital records 17 patients with SLAP lesions who underwent SLAP repair and nine patients with spinoglenoid cysts and SLAP lesions who underwent SLAP repair and cyst decompression from January 2000 to March 2005. We excluded patients with weakness or pain of the contralateral arm and patients with MRI or operative findings demonstrating acromioclavicular pathology and full-thickness or partial-thickness rotator cuff tears. Eleven of the 17 patients with SLAP lesions and three of the nine patients with cysts and SLAP lesions had inadequate followup strength testing, leaving 12 patients for study. Six of these patients (three men and three women) had MRI evidence of a paralabral cyst in the spinoglenoid notch (Fig. 1), which was then further confirmed by arthroscopy. The average age of this group was 42 years (range, 33–61 years). All of the patients with a paralabral cyst and SLAP lesion had a Type II SLAP tear. One patient additionally had a subacromial decompression. These six patients had a minimum of 12 months followup (mean, 15.2 months; range, 12–27 months). Six other patients (five men and one woman) had an isolated SLAP tear. The average age of these patients was 44.3 years (range, 31–56 years). Four of the six patients with isolated SLAP lesions also underwent concomitant arthroscopic subacromial decompression. The minimum followup for these six patients was 12 months (mean, 30 months; range, 12–48 months) after surgical repair. No patients were recalled specifically for this study; all data were obtained from medical records. Institutional Review Board approval was obtained for this study.
Preoperatively, all patients were symptomatic, demonstrating pain and weakness. Other than the SLAP lesion and the cyst in those patients with spinoglenoid notch cysts, no other pathology, including bursitis or a spur, was consistent with the patients’ signs and symptoms. After an unsuccessful trial of nonoperative treatment, including physical therapy, activity modification, and rest, patients were indicated for operative intervention. Average duration of preoperative subjective weakness for the patients with SLAP lesions and paralabral cysts was 114.6 days (range, 20–373 days). Of the patients with paralabral cysts and SLAP lesions, 50% of the patients’ affected side was their dominant side. Isolated SLAP lesions occurred in the dominant shoulder in 67% (four of six) of cases. Preoperatively, all patients underwent MRI and a thorough physical examination, including quantitative external rotation strength testing of bilateral shoulders. As part of our standard prospective data collection for all shoulder patients, external rotation strength testing was completed using a digitally calibrated dynamometer with the arm held at the side of the body and with the elbow at 90°. The patient was then asked to externally rotate the shoulder against the calibrated dynamometer and the greatest force that the patient was able to attain was recorded in pounds. This testing was performed once preoperatively. The senior author (ELF) does not routinely obtain electromyography/nerve conduction velocity (EMG/NCV) studies in patients who present with clinical signs and symptoms consistent with SLAP tear and external rotation weakness who have an MRI documenting the presence of a SLAP lesion along with a spinoglenoid notch cyst. One patient presented with an EMG/NCV study that was consistent with suprascapular nerve injury to the branch to the infraspinatus.
Postoperative external rotation strength was similarly quantified and then compared with both preoperative external rotation strength and contralateral shoulder external rotation strength.
Patients with SLAP lesions and paralabral cysts underwent arthroscopic cyst decompression and labral repair. All procedures were performed by the senior author. Surgery was performed under regional interscalene block with patients in the modified beach chair position. A posterior viewing portal and an anterior working portal were created. The glenohumeral joint, rotator cuff, and labrum were examined and the structures probed. Synovitis, cartilage damage, and/or partial tears of the rotator cuff were noted. Starting anterior to the biceps tendon, the labrum was examined and probed for stability circumferentially. All patients had a Type II SLAP tear. In the six patients who had a preoperative MRI demonstrating a ganglion cyst, the posterosuperior aspect of the labrum was elevated and the area examined. A blunt instrument was introduced medially through the SLAP tear to decompress the cyst. Entering the cyst released a viscous, gelatinous material consistent with a ganglion cyst. In preparation for the SLAP repair, the superior glenoid and deep surface of the labrum were freshened. A curette and motorized shaver were used to create a bony bed with punctate bleeding. The labral edges were trimmed, as needed, to a stable rim. An accessory anterosuperior portal was created and anchors were placed, each one loaded with a Number 2 permanent suture. Two types of anchors were used; 75% of the tears were repaired with bioabsorbable 1–3 TAG anchors (Smith and Nephew, Memphis, TN) and 25% were repaired with bioabsorbable BioFASTak (Arthrex, Naples, FL) anchors. Sutures were passed through the capsulolabral tissue through a Spectrum suture shuttle. Knots were tied down with alternating half-hitches (Fig. 2).
Fig. 2A–B.

(A) An arthroscopic image shows a Type II superior labral anterior posterior (SLAP) tear. (B) An arthroscopic image showing repair of a SLAP lesion with bioabsorbable anchors.
The instruments were then withdrawn from the glenohumeral joint and the joint was irrigated. The camera was then redirected into the subacromial space. Four patients who had SLAP tears without cysts had attritional changes or prominence of the acromion. These patients had previously on examination demonstrated signs of impingement. If it was believed that the acromion morphology could lead to abrasion of the rotator cuff, arthroscopic subacromial decompression was performed. One patient who had both a SLAP repair and cyst decompression also underwent arthroscopic subacromial decompression.
Postoperatively, all patients were placed in an arm sling for 4 weeks. During this time, no ROM of the shoulder was performed. At 4 weeks, the slings were discontinued, and ROM and strengthening exercises were begun under the supervision of a physical therapist.
Patients were typically evaluated at 2 weeks, 6 weeks, 3 months, and then yearly. The medical records were reviewed and the following data recorded: patient age, gender, preoperative diagnosis, duration of symptoms, hand dominance, and detailed physical examination findings, including external rotation strength preoperatively and postoperatively.
We determined external rotation strength ratios of affected versus unaffected sides for both cohorts of patients both preoperatively and postoperatively. Student’s t-test was used to compare the preoperative external rotation strength ratio and postoperative external rotation strength ratio of both cohorts. In addition, the increase in strength ratio of the patients who underwent SLAP repair and cyst decompression versus the patients who underwent isolated SLAP repair was compared using the Student’s t-test.
Results
Patients who underwent concomitant SLAP repair and cyst decompression demonstrated an increase in external rotation strength ratio of 40% versus patients who underwent isolated SLAP repair who demonstrated an increase of 10%. Although the patients did not all subjectively state that they had weakness of the affected extremity, objective testing demonstrated weakness as compared with the contralateral shoulder for all patients. Preoperatively both cohorts demonstrated decreased shoulder external rotation strength as compared with the other side. The group with isolated SLAP lesions had a preoperative external rotation strength ratio of 75% of the contralateral side, whereas the patients with SLAP lesions and cysts had a preoperative external rotation strength ratio of 45% as compared with the other side (Table 1). Postoperatively patients who underwent cyst decompression along with SLAP repair had an increase in external rotation strength ratio of 40%, from 45% to 85%, whereas patients with isolated SLAP repairs had an increase in ratio of 10%, from 75% to 85% (Table 2). There were no postoperative complications of suprascapular neuropathy.
Table 1.
External rotation (ER) ratios preoperatively and postoperatively
| Parameters | SLAP | SLAP/cyst | p Value |
|---|---|---|---|
| Preoperative ER ratio | 75% | 45% | 0.04 |
| Postoperative ER ratio | 85% | 85% | 0.51 |
SLAP = superior labral anterior posterior.
Table 2.
Improvement in external strength ratios
| Cohorts | Preoperative ER ratio | Postoperative ER ratio | p Value |
|---|---|---|---|
| SLAP | 75% | 85% | 0.1 |
| SLAP/cyst | 45% | 85% | 0.002 |
ER = external rotation; SLAP = superior labral anterior posterior.
Incidentally noted was a general trend toward increased gain in external rotation strength postoperatively in patients with a shorter preoperative duration of weakness. Patients who were treated surgically with a relatively short duration of weakness were indicated for surgical intervention as a result of a longer history of pain that had failed nonoperative management. We noted patients with duration of weakness less than 1 month demonstrated the greatest return of strength postoperatively with a 61% average increase in strength in two patients. Three patients with symptoms from 1 to 3 months demonstrated a 30% average increase in strength. One patient who demonstrated weakness for 1 year before surgery had a 32% increase in external rotation strength.
Discussion
Sporadic case reports describing paralabral cysts were published in the 1980s. With the advent of MRI, paralabral cysts are now more easily diagnosed and have been recognized as a cause of shoulder pain and dysfunction, although uncommonly. Paralabral cysts in the spinoglenoid notch are frequently associated with labral tears. Formation of the cyst in the spinoglenoid notch can result in suprascapular nerve impairment, secondary to a mass effect, with resulting infraspinatus weakness. The treatment of symptomatic spinoglenoid cysts has varied from observation, to open excision, to arthroscopic decompression with or without labral repair [1–3, 5, 7, 12, 13]. Recently authors have suggested that these patients can be treated with an isolated SLAP repair because a large percentage of these cysts resolve postoperatively and patients typically have high satisfaction rates after repair alone [16, 21]. Because there is controversy regarding the optimal way to manage these patients surgically, we questioned whether an isolated SLAP repair would result in an increase in external rotation strength in patients with spinoglenoid cysts and SLAP lesions whose primary symptom is weakness.
We recognize limitations to our study. First is the lack of a third cohort of patients who had spinoglenoid cysts along with SLAP lesions and underwent isolated SLAP repairs. Because this was a retrospective study and the senior author performs cyst decompressions and SLAP repairs in all patients with cysts and SLAP lesions who have failed nonoperative management, we did not have this third cohort of patients to examine. Although the addition of this cohort would have been helpful in more directly addressing the impact of cyst decompression versus SLAP repair on external rotation strength in patients with cysts and SLAP lesions, our study suggests a minimal increase in external rotation strength is obtained with SLAP repair alone versus the increase that is seen with concomitant cyst decompression. Second, our population was heterogeneous in terms of surgical procedures performed with five of the 12 patients undergoing a subacromial decompression as well. This may affect outcomes regarding pain but is unlikely to affect our primary outcome of objective measurement of external rotation strength. Third, we have a relatively small sample size. This is the result of the low incidence of spinoglenoid cysts and SLAP lesions but also limited as a result of the structure of our study in which one surgeon performed all cases. The small sample of patients with SLAP lesions is the result of the desire to have full strength testing data at 1 year for all patients. In addition, we had multiple postoperative examiners and they were not blinded in regard to whether the patients had cyst decompression and SLAP repair versus SLAP repair alone. The use of the dynamometer provided an objective measurement of strength, which is less likely to be affected by the lack of blinding. The method of strength testing itself has limitations because patient effort and pain can be a confounding factor. Furthermore, the patients underwent only one trial of strength testing. In a prospective study it would be of benefit to do multiple trials.
Many patients who present with spinoglenoid cysts and SLAP tears have both a component of pain and weakness. There is controversy regarding whether these patients can be surgically treated with an isolated SLAP repair with good results. Advocates of isolated SLAP repair in patients with spinoglenoid cysts and SLAP lesions have used outcome measures primarily based on pain or subjective improvement in strength [16, 21]. We question whether return of strength can reliably be achieved with SLAP repair in isolation. When performing concomitant SLAP repair and cyst decompression, we demonstrate a marked increase in external rotation strength that is not seen in patients with SLAP lesions who undergo only a SLAP repair, suggesting patients with considerable weakness would benefit from SLAP repair along with cyst decompression with a very low risk of complications.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Mount Sinai School of Medicine, New York, NY, USA.
Contributor Information
James Gladstone, Email: James.gladstone@mountsinai.org.
Evan L. Flatow, Email: evan.flatow@msnyuhealth.org.
References
- 1.Catalano JB, Fenlin JM., Jr Ganglion cysts about the shoulder girdle in the absence of suprascapular nerve involvement. J Shoulder Elbow Surg. 1994;3:34–41. doi: 10.1016/S1058-2746(09)80006-2. [DOI] [PubMed] [Google Scholar]
- 2.Chen A, Ong B, Rose D. Arthroscopic management of spinoglenoid cysts associated with SLAP lesions and suprascapular neuropathy. Arthroscopy. 2003;19:E17–E23. doi: 10.1016/s0749-8063(03)00381-5. [DOI] [PubMed] [Google Scholar]
- 3.Chochole MH, Senker W, Meznik C, Breitenseher MJ. Glenoid-labral cyst entrapping the suprascapular nerve: dissolution after arthroscopic débridement of an extended SLAP lesion. Arthroscopy. 1997;13:753–755. doi: 10.1016/S0749-8063(97)90013-X. [DOI] [PubMed] [Google Scholar]
- 4.Drez D., Jr Suprascapular neuropathy in the differential diagnosis of rotator cuff injuries. Am J Sports Med. 1976;4:43–45. doi: 10.1177/036354657600400201. [DOI] [PubMed] [Google Scholar]
- 5.Fehrman D, Orwin J, Jennings R. Suprascapular nerve entrapment by ganglion cysts: a report of six cases with arthroscopic findings and review of the literature. Arthroscopy. 1995;11:727–734. doi: 10.1016/0749-8063(95)90118-3. [DOI] [PubMed] [Google Scholar]
- 6.Ganzhorn RW, Hocker JT, Horowitz M, Switzer HE. Suprascapular-nerve entrapment. J Bone Joint Surg Am. 1981;63:492–494. [PubMed] [Google Scholar]
- 7.Iannotti JP, Ramsey ML. Arthroscopic decompression of a ganglion cyst causing suprascapular nerve compression. Arthroscopy. 1996;12:739–745. doi: 10.1016/S0749-8063(96)90180-2. [DOI] [PubMed] [Google Scholar]
- 8.Kessler MA, Stoffel K, Oswald A, Stutz G, Gaechter A. The SLAP lesion as a reason for glenolabral cysts: a report of five cases and review of the literature. Arch Orthop Trauma Surg. 2007;127:287–292. doi: 10.1007/s00402-006-0154-1. [DOI] [PubMed] [Google Scholar]
- 9.Koppell HP, Thompson WAL. Peripheral Entrapment Neuropathies. Baltimore, MD: Williams & Wilkins; 1963. [Google Scholar]
- 10.Leitschuh PH, Bone CM, Bouska WM. Magnetic resonance imaging diagnosis, sonographically directed percutaneous aspiration, and arthroscopic treatment of a painful shoulder ganglion cyst associated with a SLAP lesion. Arthroscopy. 1999;15:85–87. doi: 10.1053/ar.1999.v15.015008. [DOI] [PubMed] [Google Scholar]
- 11.Lichtenberg S, Magosch P, Habermayer P. Compression of the suprascapular nerve by a ganglion cyst of the spinoglenoid notch: the arthroscopic solution. Knee Surg Sports Traumatol Arthrosc. 2004;12:72–79. doi: 10.1007/s00167-003-0443-y. [DOI] [PubMed] [Google Scholar]
- 12.Moore TP, Fritts HM, Quick DC, Buss DD. Suprascapular nerve entrapment caused by supraglenoid cyst compression. J Shoulder Elbow Surg. 1997;6:455–462. doi: 10.1016/S1058-2746(97)70053-3. [DOI] [PubMed] [Google Scholar]
- 13.Piatt B, Hawkins R, Fritz R, Ho C, Wolf E, Schickendantz M. Clinical evaluation and treatment of spinoglenoid notch ganglion cysts. J Shoulder Elbow Surg. 2002;11:600–604. doi: 10.1067/mse.2002.127094. [DOI] [PubMed] [Google Scholar]
- 14.Rachbauer F, Sterzinger W, Frischhut B. Suprascapular nerve entrapment at the spinoglenoid notch caused by a ganglion cyst. J Shoulder Elbow Surg. 1996;5:150–152. doi: 10.1016/S1058-2746(96)80011-5. [DOI] [PubMed] [Google Scholar]
- 15.Romeo AA, Rotenberg DD, Bach BR., Jr Suprascapular neuropathy. J Am Acad Orthop Surg. 1999;7:358–367. doi: 10.5435/00124635-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Schroder CP, Skare O, Stiris M, Gjengedal E, Uppheim G, Brox JI. Treatment of labral tears with associated spinoglenoid cysts without cyst decompression. J Bone Joint Surg Am. 2008;90:523–530. doi: 10.2106/JBJS.F.01534. [DOI] [PubMed] [Google Scholar]
- 17.Tirman PF, Feller JF, Janzen DL, Peterfy CG, Bergman AG. Association of glenoid labral cysts with labral tears and glenohumeral instability: radiologic findings and clinical significance. Radiology. 1994;190:653–658. doi: 10.1148/radiology.190.3.8115605. [DOI] [PubMed] [Google Scholar]
- 18.Tung GA, Entzian D, Stern JB, Green A. MR imaging and MR arthrography of paraglenoid labral cysts. AJR Am J Roentgenol. 2000;174:1707–2715. doi: 10.2214/ajr.174.6.1741707. [DOI] [PubMed] [Google Scholar]
- 19.Wang DH, Koehler SM. Isolated infraspinatus atrophy in a collegiate volleyball player. Clin J Sport Med. 1996;6:255–258. doi: 10.1097/00042752-199610000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Westerheide K, Karzel R. Ganglion cysts of the shoulder: technique of arthroscopic decompression and fixation of associated type II superior labral anterior to posterior lesions. Orthop Clin N Am. 2003;34:521–528. doi: 10.1016/S0030-5898(03)00102-0. [DOI] [PubMed] [Google Scholar]
- 21.Youm T, Matthews PV, El Attrache NS. Treatment of patients with spinoglenoid cysts associated with superior labral tears without cyst aspiration, débridement, or excision. Arthroscopy. 2006;22:548–552. doi: 10.1016/j.arthro.2005.12.060. [DOI] [PubMed] [Google Scholar]