Abstract
The use of labeled US microbubbles opens the possibility of in vivo molecular profiling of tumor angiogenesis as a diagnostic tool.
Summary
In the study of Deshpande et al (1), ultrasonographic (US) microbubbles targeted with one of several antibodies—anti-integrin, anti-endoglin, or anti–vascular endothelial growth factor receptor 2—were injected into mice with implanted breast, ovarian, or pancreatic tumors. Changes in the relative uptake of each targeted microbubble were observed as the tumors grew, reflecting changes in the angiogenic mechanisms the tumor invoked at different stages of growth. This opens the possibility of in vivo molecular profiling of tumor angiogenesis as a diagnostic tool.
The Setting
Angiogenic inhibitor therapy for cancer is more than 10 years old, and, while there have been impressive responses in individual patients, there is concern that the improvements in overall survival across many tumors are modest even while they are obtained at great expense (2). There is growing recognition that angiogenic inhibitor therapy alone is probably not sufficient but must be combined with more traditional chemotherapies and/or combinations of angiogenic inhibitors. Therapeutic benefits can be obtained only at the cost of many different, and sometimes additive, side effects and high costs. Yet, while a growing menu of angiogenic inhibitors is emerging, it is unclear what agents should be administered to whom and in what order.
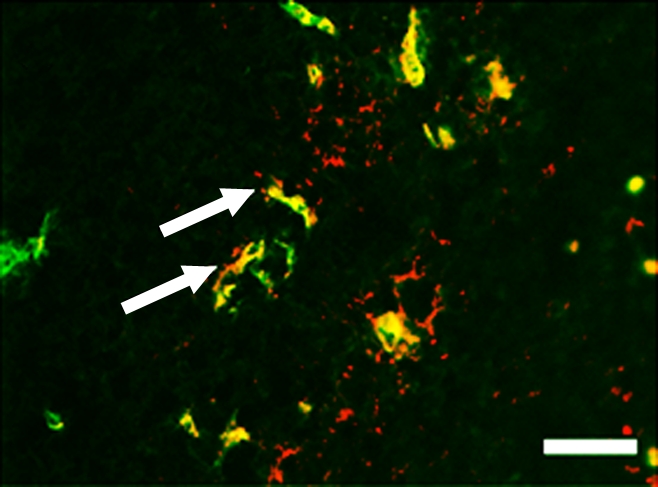
Current imaging techniques for angiogenesis, such as dynamic computed tomography, magnetic resonance imaging, and conventional color or power Doppler are nonspecific with regard to molecular angiogenic pathways. Imaging methods that could help select patients for more individualized angiogenic inhibitor therapy on the basis of tumor vessel molecular expression patterns are greatly desired. Inoue et al (3) demonstrated in a mouse model of islet cell tumors of the pancreas that different expression patterns in the angiogenic pathway occur at different steps of tumor development. In this issue of Radiology, Deshpande et al (1) have used a family of targeted microbubbles, each homing to a different marker of angiogenesis, to document the changes that occur in tumor vasculature with growth. Having this set of tools to investigate the natural history of tumor angiogenesis in vivo is a very exciting development.
The Science
The concept of tumor angiogenesis, as described in the 1970s by the late Judah Folkman (4), is deceptively simple. Tumors need a blood supply to provide oxygen and nutrients for growth and a means for dumping toxic waste. The logic behind angiogenic inhibitor therapy is unassailable: Deprive tumors of their vessels and they will die. The problem is that angiogenesis is not one process but many that interact and “cross talk.” Tumors simply adapt to angiogenic inhibitor therapy to achieve the same goal.
The science is made even more difficult by the necessity of performing studies in a “natural state.” The time-honored method of inducing a human tumor xenograft in a mouse requires a bolus of a million cells or more to be administered into a muscle or subcutaneously, hardly the normal course of events in the development of most tumors. While such xenografts are technically in vivo, they do not replicate the host-tumor interface. In the case of angiogenesis, the sudden development of a tumor in the flank of a mouse leads to intense peripheral enhancement of the tumor, which is partly an immunologic response to the sudden injection of foreign tumor cells. Thus, it is difficult to mirror tumor angiogenesis in animal models. The real process of angiogenesis must be studied in spontaneously forming tumors.
What becomes clear from the data of Deshpande et al (1) and others is that the process of angiogenesis is multiparametric and dynamic: Different signatures of expression emerge at different points in the development of the tumor. The results of this study suggest that it may be possible to track such changes by using targeted US microbubbles. This is unquestionably a step forward in diagnostic sophistication.
The Practice
Clinical use: Is clinical translation feasible? Before labeled microbubbles are introduced into the clinic, they must be shown to be safe and effective. For reimbursement, labeled microbubbles must not only impact patient care but also alter management in a cost-neutral or cost-negative manner. This will require extensive clinical testing in phase II trials.
Impediments to the use of nontargeted microbubbles include concern over the black box warning issued by the U.S. Food and Drug Administration (FDA) after several deaths were reported. However, many believe this risk has been overstated (5). Given the limited market, will development of such agents be sufficiently profitable to interest companies? Finally, there are few practitioners trained in the practice and quantitation of microbubble imaging. For these reasons, the clinical translation of targeted microbubbles will be challenging.
However, assuming that one can prove that the endothelial expression profile is relevant to the response rate to a particular angiogenic inhibitor therapy, one can envision a multistep procedure in which the patient’s tumor is tested in vivo for a variety of targets. Much the way an allergist lays down a panel of allergens during a patch test to determine sensitivities, the modern US imager could sequentially administer a panel of labeled microbubbles. When the patient returns after treatment, this same panel could be repeated to look for changes in endothelial expression as a function of the response, regression, and maturation of the tumor.
Clinical development and approval of labeled microbubbles will require a different paradigm for the FDA and related regulatory organizations around the world.
Future opportunities and challenges: Deshpande et al (1) present their experience with three labeled microbubbles. Imagine a future where there were not three, but hundreds, of labeled microbubbles available. Imagine further the presence of a “sono-pharmacy” in which “shake and bake” kits were available to combine microbubbles with virtually any human antibody. This could have enormous impact in developing personalized therapy.
Clinical development and approval of labeled microbubbles will require a different paradigm for the FDA and related regulatory organizations around the world. Is it possible to approve a platform with labeling kit without specifying exactly what that label is? If so, it may be practical to develop such a library of imaging agents. However, if the standard paradigm of “one molecule–one approval” prevails, then the financial barriers will at best delay, and at worst prevent, the actualization of a panel of labeled microbubbles.
There will certainly be challenges. It will require reduction to practice that is efficient, safe, and effective, a far-from-trivial goal. It will require improvements in animal modeling and quantitative validation. It will require substantial public and private investments. It will require marked reengineering of the chemistry of synthesizing and labeling microbubbles. It will require all these and other tasks still unforeseen. Easy? No. Possible? Maybe. Worthwhile? Definitely.
Disclosures of Potential Conflicts of Interest: P.L.C. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: has research agreements—but no financial arrangements—with Siemens, Philips, and GE. Other relationships: none to disclose.
Footnotes
See also the article by Deshpande et al.
References
- 1.Deshpande N, Ren Y, Foygel K, Rosenberg J, Willmann JK. Tumor angiogenic marker expression levels during tumor growth: longitudinal assessment with molecularly targeted microbubbles and US imaging. Radiology 2011;258(3):804–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roodink I, Leenders WP. Targeted therapies of cancer: angiogenesis inhibition seems not enough. Cancer Lett 2010;299(1):1–10 [DOI] [PubMed] [Google Scholar]
- 3.Inoue M, Hager JH, Ferrara N, Gerber HP, Hanahan D. VEGF-A has a critical, nonredundant role in angiogenic switching and pancreatic beta cell carcinogenesis. Cancer Cell 2002;1(2):193–202 [DOI] [PubMed] [Google Scholar]
- 4.Folkman J. Proceedings: Tumor angiogenesis factor. Cancer Res 1974;34(8):2109–2113 [PubMed] [Google Scholar]
- 5.Main ML, Goldman JH, Grayburn PA. Thinking outside the “box”: the ultrasound contrast controversy. J Am Coll Cardiol 2007;50(25):2434–2437 [DOI] [PubMed] [Google Scholar]


