Abstract
Introduction: Patients with complex medical care needs often embark on multiple care transitions over an extended period of time. As these patients or their caregivers often become the chief source of communication for complex medical situations, each transition can create an opportunity for health care errors. Combining the efforts of the established departments of Chronic Care Coordination (CCC), Clinical Pharmacy Call Center (CPCC), and Continuing Care, Kaiser Permanente Colorado created programs to further safe care transitions.
Methods: Two key goals for safe care transitions were established: 1) reductions in medication errors and 2) increased follow-up with care plans. To achieve these goals, communication plans targeted at medication reconciliation, patient education, and coordination of outpatient recommendations were established. Expected outcomes included reductions in medication errors, decreased Emergency Department and hospital admissions, decreased readmissions, and increased outpatient follow-up and medication compliance.
Results: A review of medication-reconciliation records for intervention patients indicated that >90% of all discharge summaries contained at least one potential drug-related problem including duplicative drugs, omitted therapy, and medication contraindications. After skilled nursing facility discharge, patients who were transitioned by CPCC clinical pharmacists were: 1) 78% less likely to die; 2) 29% less likely to need an Emergency Department visit; and 3) 17% more likely to follow up with primary physicians and clinicians than were patients in the usual care group. Health care cost savings for patients seen by the CCC program demonstrated, conservatively, an annualized per patient savings of $5276. For 763 patients enrolled in 2003, this amounts to an estimated, annualized savings of $4,025,588.
Conclusions: Patients are becoming more informed and involved in their care, but they require ongoing education and coaching to become effective advocates for themselves. Identification of unintended medication discrepancies and potential drug-related problems and increased follow-up during care transitions can improve patient safety and quality of care while saving health care resources.
Introduction
In an increasingly taxed health care system, patients with complex medical care needs may often find themselves treated in a number of acute care settings, with the unspoken goal of transitioning to a lower acuity level at the earliest opportunity. Many of these patients will embark on multiple care transitions over an extended period of time either for several acute episodes or for the same episode of care. Within the health care delivery system, as patients pass between physicians, nurse practitioners, and pharmacists, the patient often becomes the chief source of communication for complex medical situations, meaning that each transition will create an opportunity for health care errors. These patients generally lack the perspicacity to determine which experiences or pieces of information transferred to them are the most salient to pass on to the next provider.1–4 Similarly, in a health care setting where even the best clinicians may be relying on faxed or copied information, communication may not merely get lost in the translation but may just get lost altogether.
… communication may not merely get lost in the translation but may just get lost altogether.
The substantive work of Eric Coleman and others5–12 has clarified the adverse outcomes often associated with the transition process. Such transitions can be from multiple care sites, such as from a hospital to a skilled nursing facility (SNF) or home, from an SNF to hospital or home. Although transition-communication errors can occur between health care settings, some of the most profound miscommunication may occur as the patient is transitioned to home and becomes wholly responsible for his or her own care. Coleman and others have identified four factors most notably associated with improved outcomes under these circumstances: 1) assistance with medication self-management, 2) a patient-centered record owned and maintained by the patient to facilitate cross-site information transfer, 3) timely follow-up with primary or specialty care, and 4) a list of red flags indicative of a worsening condition and instructions on how to respond to them. Similarly, they have identified two mechanisms for achieving these factors: 1) a personal health record and 2) a series of visits and telephone calls with a “transitional coach.” Incorporating the ideology of this work, Kaiser Permanente Colorado (KPCO) developed two synergistic programs at two key points of transition to lessen the opportunities for suboptimal care transition experiences: 1) from an SNF to home and 2) from hospital to home.
Combining the efforts of the established departments of Chronic Care Coordination (CCC), Clinical Pharmacy Call Center (CPCC), and Continuing Care, KPCO created programs for care transitions. Two key goals for improvement were established that built on the work of Coleman and others: 1) reductions in medication errors and 2) increased follow-up with care plans. To achieve these goals, it was necessary to formulate communication plans targeted at medication reconciliation, patient education, and coordination of outpatient recommendations. Expected outcomes included reductions in medication errors, decreased Emergency Department (ED) and hospital admissions, decreased readmissions, and increased outpatient follow-up and medication compliance.
It was determined that for families experiencing sentinel health care events and transitioning to often-uncertain home care settings, telephone initiatives would likely be the most successful at optimizing participation in transition programs and minimizing travel to clinics. Additionally, given the multiple foci and complexity of communications that would occur, use of the electronic medical record (EMR—ie, HealthConnect) was instituted as the primary form of transfer and communication of information. Fortunately, in KPCO, HealthConnect is available at core hospitals and in all pharmacies and outpatient facilities. In toto, these fundamental practices have allowed for the establishment of two successful transition care processes.
Department Descriptions.
Chronic Care Coordination
The KPCO CCC Department includes 13.5 full-time equivalents (FTEs) of registered nurses and 1.8 FTE of licensed clinical social workers. Members of this department have had significant training in chronic disease management, goal-setting, and motivation communication. In addition, these staff members have a comprehensive understanding of resources available both through Kaiser Permanente and in the community. Each outpatient clinic has at least one chronic care coordinator on staff. More than 90% of the care provided by this team is by telephone. Patients generally are referred to this team through the in-baskets or pools available in HealthConnect. Most communications are sent directly to the individual clinic “hospital follow-up pool.” This obviates the need for clinicians to be familiar with the individual names of nurses, as all pools have the same name, with the individual clinic name placed at the end so that providers need know only the name of the patient's home clinic. These in-baskets are monitored five days a week, with cross-coverage from other team members when necessary.
Clinical Pharmacy Call Center
The KPCO CPCC Department consists of 20.0 FTEs of clinical pharmacists and 6.0 FTEs of pharmacy technicians. The CPCC provides service to the entire Colorado Region; thus, its clinical pharmacists provide medication-management services to multiple patient populations. Members of the CPCC team have substantial training in polypharmacy detection and management, along with extensive experience in managing the care of patients with multiple comorbid conditions. The CPCC's clinical pharmacists provide telephone care using established protocols for communication, comprehensive documentation, and interactions with patients and their caregivers. In addition to SNF transitions, the CPCC manages medication transitions for members new to Kaiser Permanente and reaches out to patients eligible for Medicare Part D for medication therapy management.
Continuing Care
The KPCO Continuing Care Department consists of 9.0 physician FTEs and 9.0 nurse practitioner FTEs. These practitioners monitor more than 100 SNF, long-term care (LTC) facilities, and assisted-living facilities (ALFs) in the Colorado region. There are approximately 300 patients per month discharged from the SNFs and more than 1100 patients monitored in LTC facilities and ALFs by Continuing Care providers. Using a process developed in collaboration with the CPCC and CCC departments, practitioners enter a discharge summary, in a format designed with input from pharmacy and primary care, in the EMR on the day of discharge and forward it to the CPCC.
Methods
I. Transition Program Descriptions
From Skilled Nursing Facility to Home
Kaiser Permanente (KP) nurse practitioners and physicians from the Continuing Care Department conduct onsite rounds at eight contracted SNFs that care for KP patients. These nurse practitioners and physicians generate thorough discharge summaries and use discharge communication forms that are communicated via HealthConnect to the CPCC. The CPCC pharmacists receive these notes and contact the individual patient or his or her caregiver within the following 24 to 48 hours. Before contacting the patient, the pharmacist reviews the patient's discharge medication orders, prior outpatient medications, and medications that the patient received from the SNF to take home. After reconciling all medications, including addressing any duplication, discontinuations, new initiations, and potential drug–drug or drug–disease interactions, the pharmacist calls the patient's home. During the conversation with the patient or caregiver, the pharmacist recommends that all of the patient's medications, including prescription and over-the-counter medications and dietary supplements, be brought to the phone to allow the pharmacist to record each medication and supplement. During this extended conversation, to ensure that the patient or caregiver understands, the pharmacist reviews and clarifies for each medication the appropriate dose, route of administration, and time to take.
… the pharmacist recommends that all of the patient's medications, including prescription and over-the-counter medications and dietary supplements, be brought to the phone to allow the pharmacist to record each medication and supplement.
After the clinical pharmacist finishes medication review and patient outreach, a copy of the CPCC chart note is forwarded via HealthConnect to the follow-up in-basket at the patient's clinic for the next phase of transition care. Within 24 to 48 hours of receiving the note, the CCC contacts the member. During this conversation, the care coordinator completes a review of systems, conducts a home safety evaluation, provides patient education, and assists in the coordination of outpatient follow-up recommendations. Included in this follow-up is a review to determine whether all referrals and orders, including any home health care, have been completed and any durable medical equipment has been delivered. The goals of this interaction have been compiled into one standard HealthConnect text that is used by every chronic care coordinator to provide uniformity and continuity of care. This formatted note, known as a Smart-Text has been created for each follow-up contact provided by the chronic care coordinators. These notes are already set up with every question that needs to be asked, reminders for the nurses and drop down menus for certain questions that have limited responses. These texts can be used to ensure that key health care, follow-up questions are asked—such as last HgA1C or shortness of breath—which then can be modified for quality improvement work.
From Hospital to Home
KP hospitalists at the two core KPCO facilities have partnered with the CCC Department to identify key elements to be included in hospital discharge information. Included in these elements are not only comprehensive discharge plans but also salient and often-overlooked information such as where the patient was discharged to, with whom the patient was discharged, a telephone number where the patient may be reached in the next 48 hours, and the name of the hospital from which the patient was discharged. These hospital discharge notes are sent on the day of discharge to the individual clinic hospital follow-up pool. As soon as possible after the discharge note is received, the CCC contacts the patient or the authorized caregiver to review the same HealthConnect text (similar to standard text used for SNF discharges but with an added area for medication reconciliation, because these patients are not sent directly to the CPCC for medication reconciliation). The CCC then completes the review of systems, the home safety check, and an assessment of care-coordination needs. If the medication reconciliation is identified as overly complex, then the chronic care coordinator will consult with a CPCC clinical pharmacist for assistance in medication reconciliation. After the phone assessment is completed, the note, including a scheduled follow-up appointment for the majority of patients, is sent directly to the primary care physician.
II. Study Evaluation of Program
Medication Reconciliation
Although there have been a limited number of studies examining the effect of a medication-reconciliation process on the incidence of medication errors and of use of medical services after discharge from an acute-care facility, we found no reports on the effect of such a process in a managed-care setting. Thus, the CPCC collaborated with the KPCO Clinical Pharmacy Research Department to design an analysis to assess the effectiveness of the CPCC medication-reconciliation program in decreasing mortality rates, the number of ED visits, and the number of follow-up clinic visits after discharge from an SNF, compared with usual care. The analysis was a quasi-experimental controlled study. All male and female KPCO patients over the age of 18 years who were discharged from one of three KPCO-contracted SNFs between October 2003 and March 2004 were eligible for inclusion in our study. All phases of the study were reviewed and approved by the KPCO Institutional Review Board.
Patients with discharge summaries received by the CPCC within 48 hours of SNF discharge to primary care had medication reconciliation performed (CPCC group), whereas those whose discharge summaries were not received within 48 hours were sent to primary care to be given usual transition care services (Usual Care group). The primary objective of this study was to assess whether there were differences between the groups in the time to death during the 60 days after discharge; secondary objectives included an assessment of the relationship between each group and the rate of ambulatory visits and the risk of an ED visit during the 60 days after SNF discharge. Risk ratios, with 95% confidence intervals, were calculated between the groups, and adjustments were made for age, sex, chronic disease score (a risk-adjustment score indicating health status at the time of SNF admission), discharging SNF, and hospital-to-SNF primary discharge diagnosis.
Chronic Care Coordination Cost Analyses
In order to document the continuing benefits of the CCC program as a whole, the Institute for Health Research (formerly the Clinical Research Unit) funded a retrospective, data-only evaluation of patients who had already been discharged from the program. A 12-month pre-post analysis of utilization and resulting costs was performed for KPCO members who were enrolled in the program from January 2001 through September 2002 and who were not enrolled in other disease management programs. Utilization and associated costs were measured and compared 12 months prior to a patient's enrollment in the CCC program and 12 months after enrollment. Costs were determined for outpatient visits, inpatient admissions, hospital outpatient and ED visits, professional services (durable medical equipment, ambulance, physician consults, non-KP provided radiology, oxygen therapy, etc), and home health visits.
All statistical analyses were performed using SAS version 9.1 (SAS Institute Inc, Cary, NC). A p-value ≤ 0.05 was considered significant. Differences in total health care costs for the 12-month period prior to CCC enrollment and the 12-month period following CCC enrollment were compared using a generalized linear model with a gamma distribution and log link function. The total cost model was adjusted for age, gender, and the number of days a patient could use medical services (this was typically 365 days but some patients died or disenrolled from KPCO during the 12-month post-enrollment period).
Results
Clinical Care Analysis
A total of 521 patients (113 and 408 in the CPCC and Usual Care groups, respectively) were included in the analysis. At baseline, the groups had equivalent characteristics.
A review of medication-reconciliation records for intervention patients indicated that >90% of all discharge summaries contained at least one potential drug-related problem including duplicative drugs, omitted therapy, and medication contraindications. After SNF discharge, patients who were transitioned by CPCC clinical pharmacists were: 1) 78% less likely to die; 2) 29% less likely to need an ED visit: and 3) 17% more likely to follow-up with primary care clinicians than were patients in the Usual Care group (Figure 1).
Figure 1.
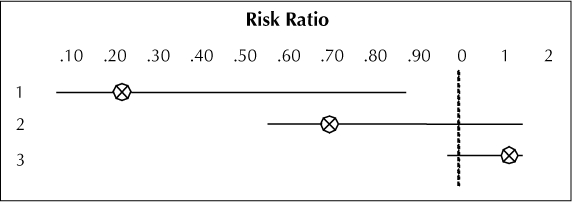
Skilled nursing facility discharge outcomes.
1 = hazard ratio for 60-day mortality, 0.22 (95% confidence interval [CI], 0.06–0.88), 78% less likely to die;
2 = odds ratio for an Emergency Department visit, 0.71 (95% CI, 0.36–1.39), 29% less likely to need an Emergency Department visit;
3 = incidence risk ratio for follow-up primary care visits, 1.17 (95% CI, 0.99–1.37), 17% more likely to follow-up with primary care clinician.
Chronic Care Coordination Cost Analyses
There was a mean pre-post decrease in total costs per patient of $9974 over the 12-month post-enrollment period for CCC patients who were not enrolled in another disease management program (30% of the total CCC patient sample were enrolled in at least one other disease management program). Patients significantly increased their pharmacy utilization and costs after their CCC enrollment but this was offset by significant decreases in post-enrollment inpatient (the primary cost driver) and professional service costs.
CCC patients enrolled in 2001, 2002, and 2003 had significantly lower post-enrollment total costs for each of those years suggesting that any time-dependent effect was minimal. The primary cost driver again was a significant decrease in post-enrollment inpatient costs.
When total costs were examined for the six-month period starting 12 months before their enrollment compared to a six-month period that began six months after their CCC enrollment, the total, annualized cost savings per patient was $5276. Looking at costs further out from (before and after) a patient's enrollment in the program was an attempt to remove some of the effects of regression to the mean that could occur due to a patient having high costs just prior to their entry into the CCC program (a sentinal event that prompted program enrollment) and then those costs dropping following program enrollment. Regression to the mean is the increased probablility of extreme values moving toward their mean value rather than to become even more extreme.
This generation will outlive any of its predecessors but will do so with a multitude of chronic conditions.
Discussion
Our results indicate that identification of unintended medication discrepancies and potential drug-related problems through the medication-reconciliation process can improve patient safety and quality of care. An additional value of the CPCC program, compared with usual care, may have been an enrichment of the discharged patient's awareness of his or her medication regimen, discharge orders, and potential medication adverse effects. The clinical pharmacist's speaking directly with patients or their care-givers in the home may have helped patients and caregivers retain more information because the environment was less stressful and thus more conducive to concentration on the counseling provided.
A pre-post analysis of the utilization and costs prior to and after enrollment in the CCC program showed a costs savings of $5276 when adjusting for the possible effects of regression to the mean. Although not all of the savings can reliably be attributed to the program because of design limitations, the saving occurred despite some increases in costs associated with increased patient compliance with health care recommendations.
With the aging of the large baby boomer generation, a crisis in health care is at hand. This generation will outlive any of its predecessors but will do so with a multitude of chronic conditions. A conservative estimate of the annualized savings would be to use the $5276 per patient savings. For 763 patients (the number of patients enrolled in 2003) this equals an annualized savings of $4,025,588. Although systemwide, physicians and nurse practitioners have been educated in evidence-based guidelines for treating these complex chronic conditions and improving outcomes and quality of life, the urgent questions that health care professionals face center on: with what resources and at what cost will such care be provided? There is no single, simple answer to these questions, but the necessary multifaceted approach will have to address both cost containment and quality of care. Opportunities to tackle these components occur at key transitions in care such as those identified here. For improving outcomes among patients with chronic conditions, this transition care project establishes pathways to target.
The use of an EMR provides the means to generate consistent, effective, thorough, and timely communication. The introduction of nearly seamless handoffs, as de-fined within these programs, would not have been possible without this contiguous form of communication. Additionally, providing the right information to the right person at the right time is an absolute necessity for an efficient process. Ideal communication avoids frustrating redundancy for the patient and clinician without losing critical content. This is established through the electronic transfer of information, making paper charts and phone calls between clinicians nearly obsolete.
Patient care will only continue to become more complicated as improved medications and strategies for care become prevalent. Although patients are becoming more informed and involved in their care, they will require ongoing education and coaching to become effective advocates for themselves. This will require a trusting partnership with their health care team as well as a multidisciplinary approach to case management. This transition care project is only the beginning of the handoffs and collaboration possible between multiple specialty programs and a patient's primary care physician. With continued investigation and improvement, more streamlining and enhancement of the population approach to managing care for patients with complex conditions will address the health care crisis of an ever-enlarging patient population.
Acknowledgments
Katharine O'Moore-Klopf of KOK Edit provided editorial assistance.
References
- Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003 Apr;51(4):549–55. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- Parry C, Kramer HM, Coleman EA. A qualitative exploration of a patient-centered coaching intervention to improve care transitions in chronically ill older adults. Home Health Care Serv Q. 2006;25(3–4):39–53. doi: 10.1300/J027v25n03_03. [DOI] [PubMed] [Google Scholar]
- Siegler EL, Murtaugh CM, Rosati RJ et al. Improving the transition to home healthcare by rethinking the purpose and structure of the CMS 485: first steps. Health Care Serv Q. 2006;25(3–4):27–38. doi: 10.1300/J027v25n03_02. [DOI] [PubMed] [Google Scholar]
- Halasyamani L, Kripalani S, Coleman E et al. Transition of care for hospitalized elderly patients—development of a discharge checklist for hospitalists. J Hosp Med. 2006 Nov;1(6):354–60. doi: 10.1002/jhm.129. [DOI] [PubMed] [Google Scholar]
- Coleman EA, Smith JD, Frank JC. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004 Nov;52(100):1817–25. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822–8. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- AACP Continuity of Care Guidelines: best practices for managing transitions between levels of care [monograph on the Internet] Pittsburgh (PA): American Association of Community Psychiatrists; 2001 Aug. [cited 2007 Jun 25]. Available from: www.comm.psych.pitt.edu/finds/cog.doc. [Google Scholar]
- Anderson G, Knickman JR. Changing the chronic care system to meet people's needs. Health Aff (Millwood) 2001 Nov–Dec;20(6):146–60. doi: 10.1377/hlthaff.20.6.146. [DOI] [PubMed] [Google Scholar]
- Alkema GE, Shannon GR, Wilber KH. Using interagency collaboration to serve older adults with chronic care needs: the Care Advocate Program. Fam Community Health. 2003 Jul–Sep;26(3):221–9. doi: 10.1097/00003727-200307000-00007. [DOI] [PubMed] [Google Scholar]
- Sunderhaus CG. ABC of postacute care. Case Manager. 2004 Nov–Dec;15(6):67–9. doi: 10.1016/j.casemgr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Poole DL, Chainakul JN, Pearson M, Graham L. Medication reconciliation: a necessity in promoting a safe hospital discharge. J Healthc Qual. 2006 May–Jun;28(3):12–29. doi: 10.1111/j.1945-1474.2006.tb00607.x. [DOI] [PubMed] [Google Scholar]
- Aufseeser-Weiss MR, Ondeck DA. Medication use risk management: hospital meets home care. Home Health Care Management and Practice. 2000 Feb;12(2):5–10. [Google Scholar]


