Abstract
Human cerebral malaria causes neurological and behavioral deficits which persist long after resolution of infection and clearance of parasites with antimalarial drugs. Previously, we demonstrated that during active infection, mice with cerebral malaria demonstrated negative behavioral outcomes. Here we used a chloroquine treatment model of cerebral malaria to determine whether these abnormal outcomes would be persistent in the mouse model. C57BL/6 mice were infected with Plasmodium berghei ANKA, and treated for ten days. After cessation of chloroquine, a comprehensive assessment of cognitive and motor function demonstrated persistence of abnormal behavioral outcomes, 10 days after successful eradication of parasites. Furthermore, these deficits were still evident forty days after cessation of chloroquine, indicating persistence long after successful treatment, a hallmark feature of human cerebral malaria. Thus, cognitive tests similar to those used in these mouse studies could facilitate the development of adjunctive therapies that can ameliorate adverse neurological outcomes in human cerebral malaria. Published by Elsevier Masson SAS on behalf of the Institut Pasteur.
Keywords: Plasmodium berghei ANKA, Object recognition, Spatial memory, Motor coordination, Brain pathology, Chloroquine treatment
1. Introduction
Cerebral malaria (CM) in humans is a severe neurological manifestation of Plasmodium falciparum infection [1,2], which results in neurological and behavioral deficits that span a wide range of behavioral domains and persist long after the infection has been successfully eradicated with antimalarial drugs [3–12]. It is estimated that 20–25% of children with successfully treated CM demonstrate residual neurological or cognitive deficits, including memory disturbances, speech and language difficulties, disorders of concentration and attention, seizures, visuo-spatial and motor deficits [3–12]. These deficits have been determined to persist after cessation of therapy, with follow-up periods extending to 9 years after infection [3–12].
Rodent models have been critical in elucidating the underlying mechanisms of CM and in the development of therapeutic agents that might salvage CNS function in patients with CM [13]. Susceptible mouse strains such as C57BL/6 infected with Plasmodium berghei ANKA (PbA) have been developed to investigate the pathogenesis of CM because they exhibit similar characteristics to human CM [13–23], including hemorrhage, axonal and neuronal damage [16,24–30], as well as behavioral and neurological impairments during active infection [12,19,22,31]. To date, however, there have been no studies of negative cognitive and behavioral outcomes after successful antimalarial therapy in experimental CM, despite the fact that persistent deficits occur in humans after resolution of malaria [3–12].
Using a chloroquine (CQ) treated CM model in C57BL/6 mice, we have demonstrated, for the first time, using a comprehensive test battery to determine whether the previously evident cognitive deficits during active infection are also observed after successful anti-parasitic treatment, the persistence of such cognitive defects in this rodent CM model. This model will be useful in the exploration of the mechanisms involved in long-term neuro-cognitive sequelae in CM, thereby facilitating the development of adjunctive therapy directed at the prevention of neuronal damage during treatment of CM.
2. Materials and methods
2.1. Animal infection and study design
Female C57BL/6 mice 4–6 weeks old were randomly assigned into 2 groups and either infected with P. berghei ANKA (PbA) or left uninfected for a comparative control group. Mice were injected intraperitoneally with either 1 × 105 red blood cells parasitized with PbA diluted in 200 μL of PBS (infected mice) or with uninfected blood diluted in PBS (control mice). This age group was chosen as older mice with PbA infection do not readily develop CM, indicating that age is important in this model [32]. Parasitemia, or the percentage of parasitized red blood cells, was assessed by microscopic examination of Giemsa-stained tail blood smears. Weight and activity levels were monitored. The infected mice were allowed to manifest the signs of CM, as described below, then treated with chloroquine (CQ) at a dose of 20 mg/kg for 10 days in order to prevent recrudescence of parasitism. Treatment was started when the infected mice reached 3 pre-determined criteria: (1) parasitemia of 7% or greater, (2) lower activity levels (as measured by the number of grid crosses and of rears defined below – in 1 min), and (3) a weight loss of 2% baseline body weight or greater. Previous unpublished observations indicate that neither parasite levels nor weight loss alone predicted the development of CM or negative behavioral sequelae, whereas the combination of all the above criteria resulted in stable and reproducible numbers of animals with evidence of CM, brain pathology and behavioral deficits. CQ therapy was initiated at 7 dpi in all control mice, the earliest day when infected mice first reached treatment criteria.
The experiments were replicated two times with the second cohort serving as its own internal replication. Both cohorts underwent behavioral testing 10 ± 2 days after cessation off CQ (henceforth referred to as the 10 day time point). The first cohort was tested at the 10-day time point, after which time the brains were harvested for pathology assessment. The second cohort, in which two groups of mice were infected on separate days, underwent behavioral testing at 10 days and at an additional time point, 40 days after the cessation of CQ, or one month after the administration of the first tests, in order to determine the persistence of any deficits demonstrated at the early time point.
Experiments were performed with the approval of The Institutional Animal Care and Use Committee of the Albert Einstein College of Medicine.
2.2. Open field
An open field test was performed whereby mice were placed in an opaque plastic arena (106 cm × 106 cm square) for 9 min, and activity was assessed with automated tracking software (Viewer: Biobserve, Bonn, Germany). General locomotor activity was assessed as well as total track length and exploration. Exploration, scored manually, was assessed as the number of rears, defined as lifting of the upper body and forepaws off the ground, whisking and sniffing. The open field was also used for habituation for the cognitive tests as visual cues were present during the tests.
2.3. Cognitive tests
The object placement and object recognition tests utilize the inherent tendency of rodents to preferentially explore novel objects and allow us to assess spatial and recognition memory, respectively. These assays are analogous to cognitive tests conducted in humans [33].
In both the object placement and object recognition tests, animals received a sample trial (Trial 1) and a test trial (Trial 2). In the object recognition test, mice were placed in an open field and allowed to freely explore two identical objects for 3 min and then returned to the home cage (Trial 1). Object exploration was recorded manually. After a retention interval of either 45 or 120 min, mice were returned to the open field for trial 2 where one of the familiar objects was replaced by a novel object. The mice were again allowed to freely explore for 3 min and exploration of objects was recorded. The object placement test was conducted similarly except that trial 1 was extended to 5 min, and in trial 2, the original identical objects remained the same; however one of the objects was displaced to a conspicuously different position in the open field. Retention intervals in the object placement test were 30 min and 120 min. Both the objects and the arena were cleaned between each subject. In addition, the objects were counter-balanced so that the new and old objects were not always the same. For the 10-day assays, only the 45-min and 30-min retention intervals were used for the object recognition and the object placement tests respectively.
In both assays, normal mice are expected to preferentially explore the novel (or displaced) object. This is analyzed and illustrated as a preference score, defined as the percentage of time spent exploring the novel object (exploration of novel object/exploration of both objects × 100). A preference score of 50% indicates random exploration. Mice are also evaluated by their “success rate” or the proportion of animals with a novel object preference of 55% or better in each experimental group. The time spent exploring both objects is represented as total novel object exploration. The arena and objects were cleaned with 70% ethanol after each trial and after completion of the day's testing to avoid confounding effects of familiar odor. In addition, the objects were counterbalanced so that old and new objects were not always the same to remove the confounds of preferential exploration of particular objects. Examiners were blind to the conditions of the mice.
2.4. Motor function
The balance beam test provides a sensitive assessment of motor coordination [34]. The start side is highly illuminated and the goal side contains a darkened shelter and palatable food to encourage reliable crossing. Mice first received 3–4 pre-training trials on a plank 4 cm wide. They were then tested for motor coordination on 2 balance beams (65 cm long) of varying difficulty – a more difficult beam measuring 1.2 cm beam in diameter, and an easier 1.8 cm diameter beam. Motor coordination was assessed as both the number of slips and the latency to cross the beam. Grip strength was assessed by latency to fall when suspended by the forepaws from a wire.
2.5. Statistics
Preference scores, number of slips, latencies and other normally distributed data were statistically analyzed when comparing controls to infected mice at a single time point by a t-test (JMP: SAS, Cary. NC). Success rate in the cognitive tests was analyzed by Chi Square tests.
Comparisons over time were analyzed in a mixed (fixed and random) design as some subjects were not tested at both time points. This is similar in principle to a repeated measures analysis, as it compares within (random) and between (fixed) subjects variability but is not compromised by missing data points.
2.6. Histopathology and immunohistochemistry
The first cohort of mice was sacrificed 5 days after the completion of the 10-day behavioral assays. In addition, parallel experiments with untreated PbA infected mice and untreated control mice were performed for histological examination. These mice were sacrificed when the infected mice developed the above-described CQ treatment criteria for comparison. Mice were euthanized using CO2 gas, and their brains were harvested and fixed in 10% buffered formalin. Brain specimens were sectioned into 5-μm sagittal slices, embedded in paraffin, and stained with hematoxylin–eosin. At least two separate midline sagittal sections were examined for each animal (N = 5 PbA and 5 Control in the CQ treatment group and 6 PbA and 4 Control in the untreated group). Areas of the brain were examined in each section using a Nikon Microphot-FXA microscope system and a Nikon digital sight DS-5M camera (Nikon Corporation, Japan). A semi-quantitative method was used for analysis of hemorrhage based on a scale of 0–4: 0 = red blood cells (RBCs) are confined within the blood vessels; 1 = one vessel with minimal extravasation of RBCs in one field at 10× magnification; 2 = greater than 1 vessel with minimal extravasation in one field; 3 = 1 vessel with extensive extravasation in one field; 4 = greater than 1 vessel with extensive extravasation in one field. Areas of hemorrhage were then evaluated at 40× magnification to confirm vascular damage (Fig. 1). T-tests were used to compare the scores of the control to the infected mice. Two examiners blinded to the conditions of the specimens reviewed the slides.
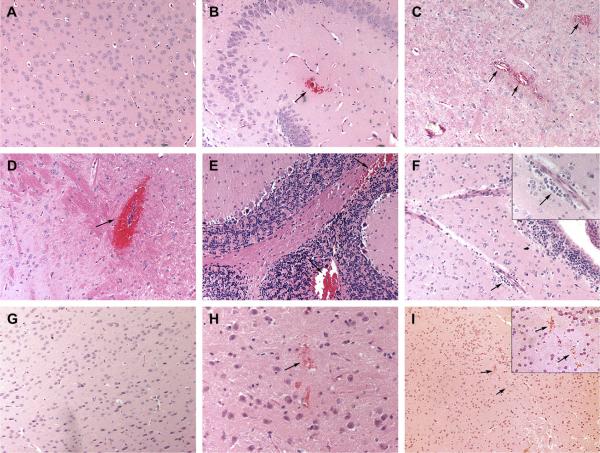
Fig. 1.
Pathology observed during CM. (A) Uninfected untreated control mice demonstrate no hemorrhage on histological examination of the brain; score = 0. (B–E) Untreated PbA infected mice demonstrated various degrees of hemorrhage (B) Arrow-one visible vessel in one field with extravasation of red blood cells (RBCs) in the hippocampus; score = 1. (C) Arrows-multiple vessels in the cortex with extravasation of RBCs; score = 2. (D) Arrow-single vessel in one field with more extensive vascular damage in the pons; score = 3. (E) Arrows-multiple vessels in cerebellum with extensive damage; score = 4. (F) Arrow and insert arrow-perivascular inflammation was also observed in different regions of the brain with CM. Hemorrhage largely resolved after anti-parasitic treatment (G) Chloroquine-treated control. (H, I) Arrows-RBC extravasation was virtually confined to scores of 1 or 2 in CQ treated PbA infected mice. Brains harvested 17 days after cessation of CQ therapy for mice in panels G–I.
Examination of a single midline section was also performed in each of the chloroquine-treated mice for evidence of microglial activation by immunostaining with a rabbit antibody to ionized calcium-binding adaptor molecule 1 (Iba1) (Wako Chemicals USA) [21]. Photographs were obtained of the cortex, cerebellum and hypothalamus (N = 5 controls, 5 PbA for cortex and hypothalamus, and 5 controls, 4 PbA for cerebellum) and Iba1 intensity was quantified as a percentage of the region of interest using ImageJ 1.42v (National Institutes of Health). T-tests were used for statistical analysis.
3. Results
3.1. Parasitemia, weight loss and locomotor activity
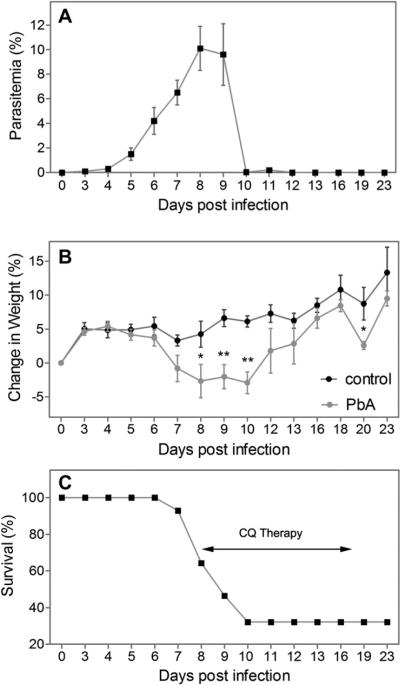
The percent parasitemia in the infected mice was 10.1 ± 1.8% infected red blood cells at the start of chloroquine (CQ) treatment and returned to 0% by 3 days after CQ treatment (Fig. 2A). CQ was started when individual animals reached the previously determined treatment criteria. Infected mice had a significant decrease in locomotor activity at 9 days post-infection (dpi) as demonstrated by the number of grids crossed in 1 min (PbA 29±3.5 vs. control 55.4±2.4, p<0.001) and the number of rears (PbA 10.9 ± 1.7 vs. control 24.8 ± 1.8, p < 0.001). Infected mice also showed fluctuations in weight (illustrated as the percent change from original weight) during the course of active infection, with significant decreases (2% or greater) of original body weight occurring between 8 and 10 dpi (Fig. 2B). A mortality of 67.9% was observed which occurred between 7 and 10 dpi (Fig. 2C). This mortality increased to 71.4% at 29 days post-CQ treatment, prior to retesting at 40 days.
Fig. 2.
Parasitemia, weight change and survival of PbA infected mice in this study. (A) By 8 days post-infection (dpi), parasitemia was greater than 7% in all infected mice. (B) Infected animals demonstrated a gradual decrease in weight after infection with significant decrease occurring between 8 and 10 days. Weights of infected animals increased to original levels after CQ treatment, though there was a transient loss of weight in both groups at day 20, which resolved by the time of testing. (C) Survival curve of PbA infected mice with mortality occurring between 7 and 10 days. *p < 0.05, **p < 0.001. Arrow-ten-day course of CQ treatment in accordance with the previously selected treatment criteria was initiated at 8.5 ± 1.5 dpi in PbA mice. CQ was started at 7 dpi in control mice.
All surviving infected mice recovered their weight by the time of testing (Fig. 2B), though there was a transient decrease in weight at day 20, and none of the mice demonstrated differences in activity or exploration after the resolution of infection as assessed in the open field. General locomotor activity, measured by track length (PbA 3224 ± 128.1 cm vs. control 3431 ± 155.0 cm), and exploration, measured by the number of rears (PbA 72.7 ± 6.0 vs. control 85.6 ± 6.0) were not significantly different between control and infected mice after the resolution of infection (Fig. S1A–C).
3.2. Mice with CM have cognitive deficits after resolution of infection
Infected mice demonstrated evidence of cognitive deficits in both spatial memory and recognition memory when tested 10 days after the cessation of CQ treatment despite the total resolution of malarial infection.
Infected mice demonstrated significantly lower preference scores in the object placement test of spatial memory after a 30 min retention interval when tested 10 days after the cessation of CQ (Fig. 3A; p < 0.05). Furthermore, a significantly higher proportion of the infected mice showed spatial memory deficits (Fig. 3C) based on the criteria for random exploration (p < 0.05).
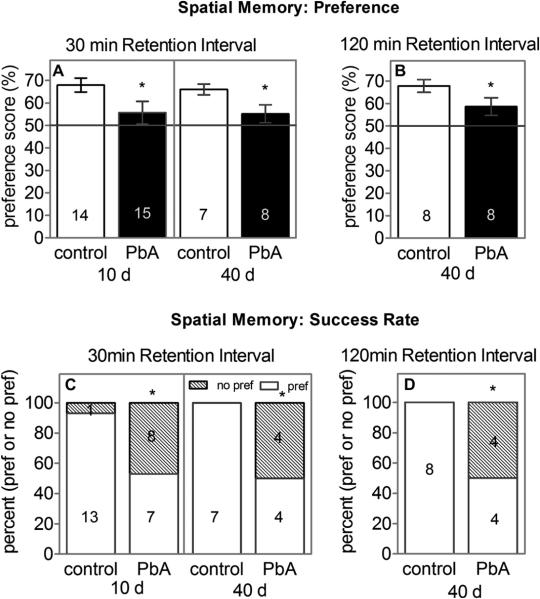
Fig. 3.
Spatial memory deficits are evident in infected mice both 10 and 40 days after cessation of treatment with antimalarial drugs. (A) Infected mice (PbA) had significantly lower preference scores in the object placement test of spatial memory when assessed after a 30 min retention interval or (B) after a 120 min retention interval. (C) A significantly higher percentage of the infected mice performed at random levels (preference score of 55% or lower = no pref, preference score higher than 55% = pref) after the 30 min retention interval at both time points and (D) at 120 min retention interval. *p < 0.05.
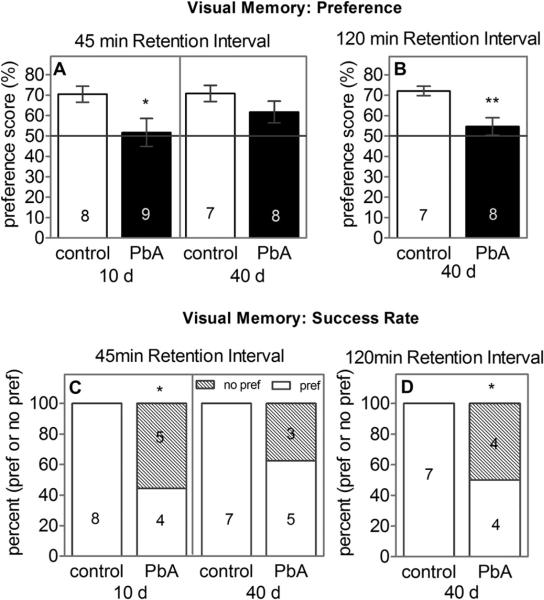
Infected mice also had evidence of cognitive deficits in a test of recognition memory after a 45 min retention interval when tested 10 days after the cessation of CQ, as indicated by the lower preference scores in the object recognition test (Fig. 4A; p < 0.05). Furthermore, a significantly higher proportion of the infected mice showed recognition memory deficits (Fig. 4C; p < 0.05).
Fig. 4.
Recognition memory deficits are evident in infected mice. (A) Infected mice had significantly lower preference scores in the object recognition test after a 45 min retention interval, 10 days after the cessation of CQ and (B) after a 120 min retention interval 40 days after cessation of CQ. (C) A significantly higher percentage of the infected mice also performed at random levels after a 30 min retention interval 10 days post-CQ treatment and (D) after a 120 min retention interval 40 days post-CQ. There were no deficits after a 45 min retention 40 days post-CQ treatment (A and C). *p < 0.05, **p < 0.01. One control mouse was excluded from testing at 40 days since there was no exploration of either object after a 30 min retention.
3.3. Cognitive deficits are persistent
The cognitive deficits evident early after CQ treatment persisted when the mice were tested one month later. Spatial memory deficits were evident using a 30 min retention interval, when infected mice were tested 40 days after the cessation of CQ (Fig. 3A; p < 0.05). A significantly higher proportion of mice still exhibited random exploration (Fig. 3C; p < 0.05) in the object placement test. Testing after a 120 min retention interval also revealed significant deficits in CM mice, with lower preference scores (Fig. 3B; p < 0.05) and a higher rate of random exploration (Fig. 3D; p < 0.05).
Though CM mice did not exhibit significant deficits after a 45 min retention interval in the object recognition 40 days after the cessation of CQ (Fig. 4A, C), further testing using a 120 min retention revealed significantly lower preference scores in CM mice (Fig. 4B; p < 0.01) and a higher proportion of the infected mice performed at random exploration levels (Fig. 4D; p < 0.05) compared to controls.
Infected and control mice had similar durations of total novel object exploration (Fig. S1D–F) when tested either 10 days (PbA 13.6 ± 2.5 s vs. control 14 ± 3.5 s) or 40 days (PbA 23.6 ± 2.0 s vs. control 27.2 ± 5.0 s) after the cessation of CQ, using a 45-min retention interval. Similar results were also obtained after 120 min retention (PbA 29.7 ± 4.9 s vs. control 36.5 ± 6.4 s). Furthermore, infected mice were able to perform the object placement task when tested after a short (10 min) retention interval, indicating that the cognitive defects were not purely due to non-specific behavioral impairment.
3.4. Mice with CM have motor coordination deficits after resolution of infection
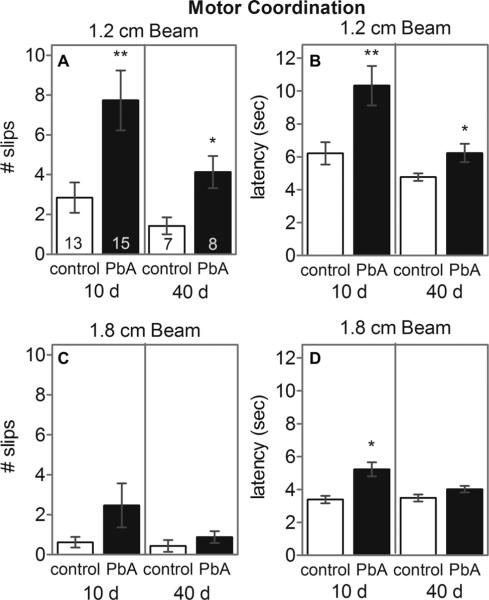
Impairment of motor coordination on the balance beam was present in infected mice 10 days after the cessation of CQ, evidenced by the number of slips (Fig. 5A; p < 0.01) and latency to cross the 1.2 cm diameter beam (Fig. 5B; p < 0.01). Moreover, the infected mice took a significantly longer time than controls to cross the 1.8 cm diameter beam (Fig. 5D; p < 0.05).
Fig. 5.
Infected mice performed poorly in balance beam test of motor coordination when compared to controls. (A) The infected mice had a greater number of slips and longer latency (B) on the 1.2 cm beam at both 10 and 40 days time point. On the 1.8 cm beam, infected mice had no significant difference in slips (C), but exhibited significantly longer latency (D) 10 days post-CQ treatment. There were no significant deficits on the larger beam 40 days post-CQ treatment (C and D). *p < 0.05, **p < 0.01. A control mouse was excluded from testing at 40 days as there was no exploration of either objects using 45 min or a 120 min retention intervals.
The early motor coordination deficits were still evident 40 days after the cessation of CQ on the 1.2 cm beam as infected mice had significantly more slips (Fig. 5A; p < 0.05) and a longer latency to cross (Fig. 5B; p < 0.05) the beam. However, no significant difference in slips or latency existed on 1.8 cm beam between infected and control animals 40 days after the cessation of CQ (Fig. 5C,D).
Though over time, there was a trend toward improvement on the 1.2 cm beam, there were no significant effects of time on balance beam performance (1.2 cm: F (1, 36) = 3.71; p = 0.062. 1.8 cm: F (1, 8) = 1.1; p = 0.3). However, there was a significant effect of infection condition on performance on the 1.2 cm beam as CM mice continued to perform worse than controls (F (1, 38) = 8.72; p < 0.01). This effect was lost on the 1.8 cm beam (p = NS). Interestingly, there were no interactions between time and infection condition with respect to performance on either beam, suggesting that learning capacity in infected mice may be intact (1.2 cm: F (1, 38) = 0.58; 1.8 cm: F (1, 5) = 0.69; p = NS).
3.5. Brain inflammation and parenchymal hemorrhage largely resolve in CM mice with CQ treatment
We previously demonstrated that during acute malarial infection, mice with CM sustain substantial hemorrhage in several regions of the brain [21]. Hematoxylin and eosin (H&E) staining of the sagittal section of acutely infected mice (N = 6) corroborated our previous demonstration of significant hemorrhage compared to untreated controls (N = 4) (Fig. 1A–E), with the more striking scores occurring in the cerebellum (PbA 1.94 ± 0.54 vs. Con 0.08 ± 0.08; p < 0.05), the midbrain (PbA 1.17 ± 0.33 vs. Con 0; p < 0.05), and the medulla (PbA 1.08 ± 0.38 vs. Con 0; p < 0.05). Interestingly, the central respiratory center, the brainstem, including the pons, demonstrated the most significant changes (PbA 1.14 ± 0.23 vs. Con 0.025 ± 0.025; p < 0.001). In addition, though individually the hemorrhage scores in the cortex, hippocampus, and fornix were not different from controls, when combined there was a ten-fold increase in the hemorrhage score in some of the regions most commonly associated with cognitive function (PbA 0.58 ± 0.2 vs. Con 0.05 ± 0.03; p < 0.05). There was also an increase in perivascular and periventricular inflammation adjacent to those regions (Fig. 1F). These lesions were largely resolved after CQ treatment, as there were no significant differences in the hemorrhage scores between control and PbA infected mice (Fig. 1G–I). Most of the animals showed at least one brain region with minimal extravasation of RBCs at 10× magnification, likely as a result of post-mortem processing, with the frontal cortex (PbA 1 ± 0.63 vs. Control 0.4 ± 0.24; p = NS; N = 5) and the cerebellum (PbA 1 ± 0.71, Control 0; p = NS; N = 4 PbA and 5 control) exhibiting the highest hemorrhage scores.
Similarly, the inflammation observed during acute infection [21] was also resolved after CQ as Iba1 immunoreactivity (quantified as the percent region of interest) in CM mice did not demonstrate any significant degree of monocytic infiltration in the cerebral vasculature or of microglial activation compared to control mice in the frontal cortex (PbA 0.82 ± 0.18% vs. Control 0.48 ± 0.12%; p = NS; N = 5), cerebellum (PbA 1.05 ± 0.25% vs. Control 0.68 ± 0.07%; p = NS; N = 4 PbA, 5 control) or the hypothalamus (PbA 1.14 ± 0.27% vs. Control 0.58 ± 0.11%; p = NS; N = 5), indicating that the persistent cognitive and motor impairments in CM were not due to residual vascular damage or to inflammation in the brain.
4. Discussion
Even with successful anti-parasitic treatment, greater than 20% of the children who survive an episode of cerebral malaria (CM) develop persistent neurological and cognitive deficits [3,5,8,10,31,35–38]. Cognitive impairment after successful therapy for malaria is becoming increasingly evident, and the global economic and scholastic health consequences of long-term residual deficits in CM patients cannot be underestimated, considering the vast number of people affected in endemic regions. Despite extensive studies on the pathogenesis of CM, significant gaps exist in our understanding of the precise etiology of the cerebral dysfunction seen in CM because the pathological processes are difficult to document in humans. The murine model of C57BL/6, infection with P. berghei ANKA (PbA) used in this study enables us to assess a disease process in which several aspects are analogous to human infection.
Previously, our laboratory group has demonstrated that susceptible mice sustain significant memory deficits during acute infection with PbA [21], and demonstrate many of the histopathologic features of human CM such as hemorrhage, neuronal and axonal damage [21,24,30]. With this study we present a treatment model of PbA infection that mimics the problem of persistency in neurological sequelae after parasitological cure that is observed in human CM when infected with P. falciparum. In our model, both cognitive and motor deficits were evident in infected mice early after the eradication of parasites and persisted on retesting one month after cure of infection and after resolution of cerebral pathology. Significant deficits were observed in the object recognition and object placement tests of spatial and recognition memory 10 days after the completion of successful antimalarial therapy with CQ. These deficits persisted when the animals were evaluated more than a month after the resolution of their infection.
In addition, CM mice also demonstrated significant motor coordination deficits when evaluated on the balance beam both early and after a prolonged period post-resolution of malaria, consistent with the pronounced pathology in the cerebellum observed during acute disease. Motor deficits on the balance beam were not accompanied by deficits in grip strength or general locomotor activity suggesting some specificity for motor coordination rather than peripheral muscle dysfunction or general sickness behavior. Although there seemed to be a tendency toward improvement in motor coordination on the 1.2 cm balance beam with time, this was not significant. In addition, there were no interactions between time and infection status with regard to motor coordination suggesting that motor learning capacity in infected mice may be at least partially intact.
Although cognitive deficits were persistent 40 days after cessation of CQ, infected mice approached the performance levels of controls and demonstrated no significant deficits in the object recognition test after a 45 min retention. This may be a reflection of experimental variables such as the loss of sicker and presumably more impaired animals, or possible variability in improvement of symptoms and the rate of such improvements. The nature of the improved performance also suggests that these deficits over time might be more subtle as brain pathology resolves, or that the mice might have learned to compensate for their deficits, as more sensitive tests, for example the extension of the retention interval to 120 min, were still able to detect significant impairment in infected mice.
It is important to separate the specific cognitive deficits from non-specific behavioral deficits induced by previous illness, general sickness due to malarial infection, CQ therapy or peripheral pathology. A recent article by Reis et al. [39] found that CM-resistant mice infected with PbA did not incur cognitive deficits after chloroquine treatment, indicating that the neuro-cognitive impairment observed during CM are specific, and not just due to general severe malarial disease. In this regard, in the present study, the lack of impairment in total novel exploration, locomotor activity and exploration, and normal cognitive performance using very short retention intervals (3 min) in the object placement test in CM mice (data not shown) indicate that the cognitive deficits observed were not likely to be due to confounding factors such as perceptual deficits, development of neophobia, peripheral organ or muscle dysfunction due to general systemic illness, or effects of CQ treatment.
Several theories exist about the etiology of long-term cognitive impairment with CM. It is postulated that these cognitive deficits occur as a result of a complicated host inflammatory response in conjunction with vascular impairment [40], causing abnormalities in neuronal cells, which adversely affect cognitive function [41–43]. This was consistent with our observations in the acute CM murine model [26,44]. However, more recent analysis suggests that the development of long-term deficits with CM is more complex [45] and may involve a host of metabolic and physiological processes in several brain regions that remain long after malaria parasites have been cleared. This idea is more in line with our demonstration that after the resolution of inflammation and hemorrhage with parasitological cure, mice still remained with persistent cognitive and motor deficits.
Both experimental and human models of CM have already demonstrated evidence for neuronal damage during active infection [21–28,30]. In this regard neuronal apoptosis has been demonstrated in mice with CM [46,47], and irreversible glial cell injury and dysfunction in the brainstem has been described in cases of severe human CM [25]. These data not only lend support to our observed increase in hemorrhagic damage in the brainstem during infection which may be implicated in downstream neuronal damage, but also point toward damage to the central respiratory center, both vascular and neuronal, as a possible explanation for the increased mortality associated with CM in this model. Our data demonstrate that geographical distribution of vascular damage during CM is clearly important as persistent cognitive and motor deficits as well as mortality correlate with the areas of damage in acute infection. However, as demonstrated in this study, vascular damage or inflammation alone cannot result in the long-term neuro-cognitive effects of cerebral malaria. There is a dearth of information on neural factors that may affect cognitive and sensorimotor function after malarial treatment. The persistence of negative functional outcomes despite the resolution of hemorrhage and inflammation underscores the need for further evaluation of preventable neuronal damage as a possible etiologic factor of long-term neuro-cognitive sequelae in CM.
Though this study does not expressly resolve the etiology of long-term negative neurological outcomes with CM, it does recapitulate the process observed in human CM. This report, to our knowledge, is the first of this kind. This important model can not only serve as a rationale for existing analogous tests in human CM, but it can aid in the exploration of the mechanism involved in neuro-cognitive sequelae in CM; thereby allowing us to devise adjunctive therapy directed at the prevention of neuronal damage during treatment of CM.
Supplementary Material
Acknowledgments
The authors acknowledge Mr. Dazhi Zhao for his considerable assistance with the maintenance, infection and treatment of the mice.
This work was supported by the NIH Training Grant in Mechanisms of Cardiovascular Diseases (T32 HL-07675) to MSD; Dominick P. Purpura Department of Neuroscience and Department of Psychiatry and Behavioral Sciences (neuroscience fellowship support to MSD), Albert Einstein College of Medicine; Burroughs-Wellcome Fund's Career Awards for Medical Scientists to MSD; Einstein-Montefiore Institute for Clinical and Translational Research Career Development Award to MSD; AI076248 to HBT; AI39454 to LMW; NS041282 to DCS.
Abbreviations
- PbA
Plasmodium berghei ANKA
- CQ
chloroquine
- CM
Cerebral malaria
- RBC
red blood cell
- cm
centimeter
- dpi
days post-infection
Footnotes
Conflict of interest statement The authors report no commercial or other association that might pose a conflict of interest.
Appendix. Supplementary material Supplementary data related to this article can be found online at doi:10.1016/j.micinf.2010.08.006.
References
- [1].Garg RK. Cerebral malaria. J. Assoc. Physicians India. 2000;48:1004e1013. [PubMed] [Google Scholar]
- [2].Mackintosh CL, Beeson JG, Marsh K. Clinical features and pathogenesis of severe malaria. Trends Parasitol. 2004;20:597–603. doi: 10.1016/j.pt.2004.09.006. [DOI] [PubMed] [Google Scholar]
- [3].Boivin MJ, Bangirana P, Byarugaba J, Opoka RO, Idro R, Jurek AM, John CC. Cognitive impairment after cerebral malaria in children: a prospective study. Pediatrics. 2007;119:E360–E366. doi: 10.1542/peds.2006-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Idro R, Ndiritu M, Ogutu B, Mithwani S, Maitland K, Berkley J, Crawley J, Fegan G, Bauni E, Peshu N, Marsh K, Neville B, Newton C. Burden, features, and outcome of neurological involvement in acute falciparum malaria in Kenyan children. J. Am. Med. Assoc. 2007;297:2232–2240. doi: 10.1001/jama.297.20.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Carter JA, Ross AJ, Neville BG, Obiero E, Katana K, Mung'ala-Odera V, Lees JA, Newton CR. Developmental impairments following severe falciparum malaria in children. Trop. Med. Int. Health. 2005;10:3–10. doi: 10.1111/j.1365-3156.2004.01345.x. [DOI] [PubMed] [Google Scholar]
- [6].Crawley J, Smith S, Muthinji P, Marsh K, Kirkham F. Electroencephalographic and clinical features of cerebral malaria. Arch. Dis. Child. 2001;84:247–253. doi: 10.1136/adc.84.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Falchook GS, Malone CM, Upton S, Shandera WX. Postmalaria neurological syndrome after treatment of Plasmodium falciparum malaria in the United States. Clin. Infect. Dis. 2003;37:e22–24. doi: 10.1086/375269. [DOI] [PubMed] [Google Scholar]
- [8].Holding PA, Stevenson J, Peshu N, Marsh K. Cognitive sequelae of severe malaria with impaired consciousness. Trans. R. Soc. Trop. Med. Hyg. 1999;93:529–534. doi: 10.1016/s0035-9203(99)90368-1. [DOI] [PubMed] [Google Scholar]
- [9].John CC, Bangirana P, Byarugaba J, Opoka RO, Idro R, Jurek AM, Wu BL, Boivin MJ. Cerebral malaria in children is associated with long-term cognitive impairment. Pediatrics. 2008;122:E92–E99. doi: 10.1542/peds.2007-3709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kihara M, Carter JA, Newton CR. The effect of Plasmodium falciparum on cognition: a systematic review. Trop. Med. Int. Health. 2006;11:386–397. doi: 10.1111/j.1365-3156.2006.01579.x. [DOI] [PubMed] [Google Scholar]
- [11].Richardson ED, Varney NR, Roberts RJ, Springer JA, Wood PS. Long-term cognitive sequelae of cerebral malaria in Vietnam veterans. Appl. Neuropsychol. 1997;4:238–243. doi: 10.1207/s15324826an0404_5. [DOI] [PubMed] [Google Scholar]
- [12].Senanayake N, de Silva HJ. Delayed cerebellar ataxia complicating falciparum malaria: a clinical study of 74 patients. J. Neurol. 1994;241:456–459. doi: 10.1007/BF00900965. [DOI] [PubMed] [Google Scholar]
- [13].Hunt NH, Grau GE. Cytokines: accelerators and brakes in the pathogenesis of cerebral malaria. Trends Immunol. 2003;24:491–499. doi: 10.1016/s1471-4906(03)00229-1. [DOI] [PubMed] [Google Scholar]
- [14].Schetters T, Curfs J, van Zon A, Hermsen C, Eling W. Cerebral lesions in mice infected with Plasmodium berghei are the result of an immunopathological reaction. Trans. R. Soc. Trop. Med. Hyg. 1989;83:103–104. doi: 10.1016/0035-9203(89)90615-9. [DOI] [PubMed] [Google Scholar]
- [15].Rest JR. Cerebral malaria in inbred mice. I. A new model and its pathology. Trans. R. Soc. Trop. Med. Hyg. 1982;76:410–415. doi: 10.1016/0035-9203(82)90203-6. [DOI] [PubMed] [Google Scholar]
- [16].Medana IM, Hunt NH, Chan-Ling T. Early activation of microglia in the pathogenesis of fatal murine cerebral malaria. Glia. 1997;19:91–103. doi: 10.1002/(sici)1098-1136(199702)19:2<91::aid-glia1>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- [17].Martins YC, Smith MJ, Pelajo-Machado M, Werneck GL, Lenzi HL, Daniel-Ribeiro CT, Carvalho LJ. Characterization of cerebral malaria in the outbred Swiss Webster mouse infected by Plasmodium berghei ANKA. Int. J. Exp. Pathol. 2009;90:119–130. doi: 10.1111/j.1365-2613.2008.00622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bagot S, Idrissa Boubou M, Campino S, Behrschmidt C, Gorgette O, Guenet JL, Penha-Goncalves C, Mazier D, Pied S, Cazenave PA. Susceptibility to experimental cerebral malaria induced by Plasmodium berghei ANKA in inbred mouse strains recently derived from wild stock. Infect. Immun. 2002;70:2049–2056. doi: 10.1128/IAI.70.4.2049-2056.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Lou J, Lucas R, Grau GE. Pathogenesis of cerebral malaria: recent experimental data and possible applications for humans. Clin. Microbiol. Rev. 2001;14:810–820. doi: 10.1128/CMR.14.4.810-820.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].de Souza JB, Riley EM. Cerebral malaria: the contribution of studies in animal models to our understanding of immunopathogenesis. Microbes Infect. 2002;4:291–300. doi: 10.1016/s1286-4579(02)01541-1. [DOI] [PubMed] [Google Scholar]
- [21].Desruisseaux MS, Gulinello M, Smith DN, Lee SC, Tsuji M, Weiss LM, Spray DC, Tanowitz HB. Cognitive dysfunction in mice infected with Plasmodium berghei strain ANKA. J. Infect. Dis. 2008;197:1621–1627. doi: 10.1086/587908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Lackner P, Beer R, Heussler V, Goebel G, Rudzki D, Helbok R, Tannich E, Schmutzhard E. Behavioural and histopathological alterations in mice with cerebral malaria. Neuropathol. Appl. Neurobiol. 2006;32:177–188. doi: 10.1111/j.1365-2990.2006.00706.x. [DOI] [PubMed] [Google Scholar]
- [23].Stoltenburgdidinger G, Neifer S, Bienzle U, Eling WMC, Kremsner PG. Selective damage of hippocampal neurons in murine cerebral malaria prevented by pentoxifylline. J. Neurol. Sci. 1993;114:20–24. doi: 10.1016/0022-510x(93)90043-x. [DOI] [PubMed] [Google Scholar]
- [24].Medana IM, Day NP, Hien TT, Mai NTH, Bethell D, Phu NH, Farrar J, Esiri MM, White NJ, Turner GD. Axonal injury in cerebral malaria. Am. J. Pathol. 2002;160:655–666. doi: 10.1016/S0002-9440(10)64885-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Medana IM, Mai NTH, Day NPJ, Hien TT, Bethell D, Phu NH, Farrar J, White NJ, Turner GDH. Cellular stress and injury responses in the brains of adult Vietnamese patients with fatal Plasmodium falciparum malaria. Neuropathol. Appl. Neurobiol. 2001;27:421–433. doi: 10.1046/j.0305-1846.2001.00360.x. [DOI] [PubMed] [Google Scholar]
- [26].Kennan RP, Machado FS, Lee SC, Desruisseaux MS, Wittner M, Tsuji M, Tanowitz HB. Reduced cerebral blood flow and N-acetyl aspartate in a murine model of cerebral malaria. Parasitol. Res. 2005;96:302–307. doi: 10.1007/s00436-005-1349-z. [DOI] [PubMed] [Google Scholar]
- [27].Ma NL, Madigan MC, ChanLing T, Hunt NH. Compromised blood-nerve barrier, astrogliosis, and myelin disruption in optic nerves during fatal murine cerebral malaria. Glia. 1997;19:135–151. doi: 10.1002/(sici)1098-1136(199702)19:2<135::aid-glia5>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- [28].Lewallen S, Bronzan RN, Beare NA, Harding SP, Molyneux ME, Taylor TE. Using malarial retinopathy to improve the classification of children with cerebral malaria. Trans. R. Soc. Trop. Med. Hyg. 2008;102:1089–1094. doi: 10.1016/j.trstmh.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Beare NAV, Riva CE, Taylor TE, Molyneux ME, Kayira K, White VA, Lewallen S, Harding SP. Changes in optic nerve head blood flow in children with cerebral malaria and acute papilloedema. J. Neurol. Neurosurg. Psychiatry. 2006;77:1288–1290. doi: 10.1136/jnnp.2005.083956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].White VA, Lewallen S, Beare NAV, Molyneux ME, Taylor TE. Retinal pathology of pediatric cerebral malaria in Malawi. Plos One. 2009;4 doi: 10.1371/journal.pone.0004317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Boivin MJ. Effects of early cerebral malaria on cognitive ability in Senegalese children. J. Dev. Behav. Pediatr. 2002;23:353–364. doi: 10.1097/00004703-200210000-00010. [DOI] [PubMed] [Google Scholar]
- [32].Hearn J, Rayment N, Landon DN, Katz DR, de Souza JB. Immunopathology of cerebral malaria: morphological evidence of parasite sequestration in murine brain microvasculature. Infect. Immun. 2000;68:5364–5376. doi: 10.1128/iai.68.9.5364-5376.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Caterini F, Della Sala S, Spinnler H, Stangalino C, Turnbull OH. Object recognition and object orientation in Alzheimer's disease. Neuropsychology. 2002;16:146–155. [PubMed] [Google Scholar]
- [34].Stanley JL, Lincoln RJ, Brown TA, McDonald LM, Dawson GR, Reynolds DS. The mouse beam walking assay offers improved sensitivity over the mouse rotarod in determining motor coordination deficits induced by benzodiazepines. J. Psychopharmacol. 2005;19:221–227. doi: 10.1177/0269881105051524. [DOI] [PubMed] [Google Scholar]
- [35].Carter JA, Mung'ala-Odera V, Neville BG, Murira G, Mturi N, Musumba C, Newton CR. Persistent neurocognitive impairments associated with severe falciparum malaria in Kenyan children. J. Neurol. Neurosurg. Psychiatry. 2005;76:476–481. doi: 10.1136/jnnp.2004.043893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Carter JA, Lees JA, Gona JK, Murira G, Rimba K, Neville BG, Newton CR. Severe falciparum malaria and acquired childhood language disorder. Dev. Med. Child. Neurol. 2006;48:51–57. doi: 10.1017/S0012162206000107. [DOI] [PubMed] [Google Scholar]
- [37].Fernando D, De Silva D, Wickremasinghe R. Short-term impact of an acute attack of malaria on the cognitive performance of schoolchildren living in a malaria-endemic area of Sri Lanka. Trans. R. Soc. Trop. Med. Hyg. 2003;97:633–639. doi: 10.1016/s0035-9203(03)80093-7. [DOI] [PubMed] [Google Scholar]
- [38].Meremikwu MM, Asindi AA, Ezedinachi E. The pattern of neurological sequelae of childhood cerebral malaria among survivors in Calabar, Nigeria. Cent. Afr. J. Med. 1997;43:231–234. [PubMed] [Google Scholar]
- [39].Reis PA, Comim CM, Hernani F, Silva B, Barichello T, Portella AC, Gomes FC, Sab IM, Frutuoso VS, Oliveira MF, Bozza PT, Bozza FA, Dal-Pizzol F, Zimmerman GA, Quevedo J, Castro-Faria-Neto HC. Cognitive dysfunction is sustained after rescue therapy in experimental cerebral malaria, and is reduced by additive antioxidant therapy. PLoS Pathog. 2010;6:e1000963. doi: 10.1371/journal.ppat.1000963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Grote CL, PierreLouis SJC, Durward WF. Deficits in delayed memory following cerebral malaria: a case study. Cortex. 1997;33:385–388. doi: 10.1016/s0010-9452(08)70014-5. [DOI] [PubMed] [Google Scholar]
- [41].Sparkman NL, Buchanan JB, Heyen JRR, Chen J, Beverly JL, Johnson RW. Interleukin-6 facilitates lipopolysaccharide-induced disruption in working memory and expression of other proinflammatory cytokines in hippocampal neuronal cell layers. J. Neurosci. 2006;26:10709–10716. doi: 10.1523/JNEUROSCI.3376-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Bessis A, Bechade C, Bernard D, Roumier A. Microglial control of neuronal death and synaptic properties. Glia. 2007;55:233–238. doi: 10.1002/glia.20459. [DOI] [PubMed] [Google Scholar]
- [43].Griffin R, Nally R, Nolan Y, McCartney Y, Linden J, Lynch MA. The age-related attenuation in long-term potentiation is associated with microglial activation. J. Neurochem. 2006;99:1263–1272. doi: 10.1111/j.1471-4159.2006.04165.x. [DOI] [PubMed] [Google Scholar]
- [44].Machado FS, Nagajyothi M.S. Desruisseaux, Kennan RP, Hetherington HP, Wittner M, Weiss LM, Lee SC, Scherer PE, Tsuji M, Tanowitz HB. Endothelin in a murine model of cerebral malaria. Exp. Biol. Med. 2006;231:1176–1181. [PubMed] [Google Scholar]
- [45].Kihara M, Carter JA, Holding PA, Vargha-Khadem F, Scott RC, Idro R, Fegan GW, de Haan M, Neville BGR, Newton C. Impaired everyday memory associated with encephalopathy of severe malaria: the role of seizures and hippocampal damage. Malar. J. 2009;8 doi: 10.1186/1475-2875-8-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Lackner P, Burger C, Pfaller K, Heussler V, Helbok R, Morandell M, Broessner G, Tannich E, Schmutzhard E, Beer R. Apoptosis in experimental cerebral malaria: spatial profile of cleaved caspase-3 and ultrastructural alterations in different disease stages. Neuropathol. Appl. Neurobiol. 2007;33:560–571. doi: 10.1111/j.1365-2990.2007.00833.x. [DOI] [PubMed] [Google Scholar]
- [47].Wiese L, Kurtzhals JAL, Penkowa M. Neuronal apoptosis, metallothionein expression and proinflammatory responses during cerebral malaria in mice. Exp. Neurol. 2006;200:216–226. doi: 10.1016/j.expneurol.2006.02.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.