Abstract
Background
Alcohol consumption is causally linked to nonadherence to antiretroviral treatment that in turn causes an increase in HIV/AIDS mortality. This article presents a method to calculate the percentage of HIV/AIDS deaths attributable to alcohol consumption and the associated uncertainty.
Methods
By combining information on risk relations from a number of published sources, we estimated alcohol-attributable fractions (AAFs) of HIV/AIDS in a stepwise procedure. First, we estimated the effect of alcohol consumption on adherence to antiretroviral treatment, and then we combined this estimate with the impact of nonadherence on death. The 95% uncertainty intervals were computed by estimating the variance of the AAFs using Taylor series expansions of one and multiple variables. AAFs were determined for each of the five Global Burden of Disease regions of Africa, based on country-specific treatment and alcohol consumption data from 2005.
Results
The effects of alcohol on HIV/AIDS in the African Global Burden of Disease regions range from 0.03% to 0.34% for men and from 0% to 0.17% for women, depending on region and age category. The detrimental effect of alcohol consumption was statistically significant in every region and age category except for the North Africa/Middle East region.
Conclusions
Although the method has its limitations, it was shown to be feasible and provided estimates of the impact of alcohol use on the mortality outcome of HIV/AIDS.
Background
Alcohol has been identified as a major risk factor for mortality and burden of disease in past comparative risk assessments within Global Burden of Disease studies [1,2]. In past iterations of comparative risk assessments, infectious diseases have not been included. However, evidence has been accumulating that alcohol has a causal impact on infectious disease categories [3,4].
Evidence indicates a strong association between alcohol and HIV/AIDS [5,6], but personality variables such as risk-taking or impulsive behavior cannot be excluded as potential alternative explanations [6]. There is sufficient evidence, however, that alcohol worsens the course of the disease, especially by impacting adherence to antiretroviral treatment. Globally, HIV/AIDS led to about 2 million deaths and 58.5 million lost disability-adjusted life years (DALYs) in 2004 [7]. Failing to estimate the alcohol-attributable HIV/AIDS burden could lead to substantial underestimation of the burden of disease and mortality attributable to alcohol.
Antiretroviral therapy has led to a change in the natural history of HIV [8-10]. Lima and colleagues have shown that nonadherence to antiretroviral therapy by as little as 5% has a significant effect on the mortality of HIV-infected people in a high-income country [11]. Studies from low- to middle-income countries have shown similarly elevated risks [12]. Therefore, adherence is a key to the success of antiretroviral therapy, and adherence levels of at least 90% to 95% are generally necessary to maximize treatment benefits [13,14]. Poor adherence to antiretroviral therapy is associated with an increased likelihood of hospitalization [15], as well as increased mortality [3,11,12,16].
Adherence is impacted by multiple variables such as injection drug use, forgetfulness, suspicions about treatment, complicated dosing regimens, number of pills required, decreased quality of life, and work and family responsibilities [17]. Alcohol use, and especially occasions of heavy drinking, has been shown to have a marked impact on adherence by interfering with one's capacity to plan for or remember dosing requirements. In addition, alcohol users might have decreased access to antiretroviral therapy or may use alcohol to reduce or avoid HIV-related negative mood states [18]. A recent meta-analysis [18] indicated that, compared to abstainers, drinkers have an odds ratio of 0.604 (95% confidence interval [CI]: 0.531, 0.687) of adhering at least 95% of the time to their treatment, meaning that those who used alcohol were about 0.60 times as likely to be classified as adherent to treatment as nonusers. Overall, the effect of alcohol use on antiretroviral treatment has been found to be causal [3,19].
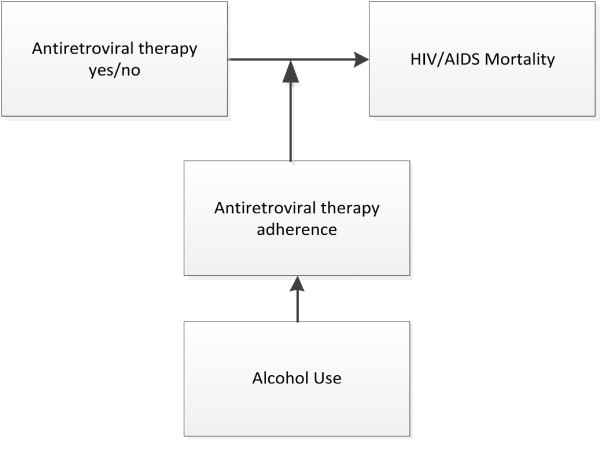
Despite the demonstrated role of alcohol use on antiretroviral medication adherence, research on and modeling of the effect of alcohol use on the HIV/AIDS burden of mortality and disease remain limited [20]. This article suggests a method to quantify the fraction of HIV/AIDS deaths attributable to alcohol consumption from nonadherence to antiretroviral therapy. We estimate the alcohol-attributable fraction (AAF) for HIV/AIDS-related mortality by combining the effect of alcohol consumption on antiretroviral adherence and the effect of adherence on mortality. Therefore, this method only considers increased mortality due to alcohol consumption that is linked to a resulting worsened adherence to antiretroviral treatment. It does not take into consideration any effect that alcohol might have on the outcome of HIV/AIDS in the absence of treatment. These causal assumptions are summarized in Figure 1.
Figure 1.
Causal assumptions of our method of calculating mortality due to nonadherence to antiretroviral therapy because of alcohol use.
Methods
We conducted an analysis using data from the five Global Burden of Disease (GBD) regions of Africa. These regions were chosen for their high variation in both prevalence of HIV/AIDS and adult per capita estimates of alcohol consumption. These regions are defined as follows:
• North Africa/Middle East: Algeria, Bahrain, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Occupied Palestinian Territory, Oman, Qatar, Saudi Arabia, Syria, Tunisia, Turkey, United Arab Emirates, Western Sahara, Yemen
• Sub-Saharan Africa, Central: Angola, Central African Republic, Congo, the Democratic Republic of the Congo, Equatorial Guinea, Gabon
• Sub-Saharan Africa, East: Burundi, Comoros, Djibouti, Eritrea, Ethiopia, Kenya, Madagascar, Malawi, Mayotte, Mozambique, Rwanda, Somalia, Sudan, Tanzania, Uganda, Zambia
• Sub-Saharan Africa, South: Botswana, Lesotho, Namibia, South Africa, Swaziland, Zimbabwe
• Sub-Saharan Africa, West: Benin, Burkina Faso, Cameroon, Cape Verde, Chad, Côte d'Ivoire, Gambia, Ghana, Guinea, Guinea-Bissau, Liberia, Mali, Mauritania, Niger, Nigeria, Saint Helena, Sao Tome and Principe, Senegal, Sierra Leone, Togo
Data sources
Country data on the proportion of people who are in need of antiretroviral therapy and receive such treatment were obtained for 2005 from the 2006 Report on the Global AIDS Epidemic [21]. Regional data were then calculated as a population-weighted average. Table 1 outlines the resulting regional proportion of people receiving antiretroviral treatment compared to all those who are in need of such treatment for the five African GBD regions.
Table 1.
Proportion of people in need of antiretroviral therapy receiving antiretroviral therapy.
| Region | Proportion | ||
|---|---|---|---|
| lower bound | point estimate | upper bound | |
| North Africa/Middle East | 15.01% | 17.36% | 19.71% |
| Sub-Saharan Africa, Central | 3.00% | 4.25% | 5.50% |
| Sub-Saharan Africa, East | 12.07% | 14.24% | 16.41% |
| Sub-Saharan Africa, South | 19.11% | 21.67% | 24.22% |
| Sub-Saharan Africa, West | 11.36% | 13.47% | 15.59% |
In order to establish the prevalence of nonadherence, we adopted an estimate of 40.1% for the rate of nonadherence to antiretroviral treatment (95% CI: 36.9%, 43.3%), provided by Lima and colleagues [18,22]. This estimate was between two other estimates of 47.6% and 31.8% for adherence rates of <80% and <90%, respectively [12,16]. Please note that even though the relative risk for people adhering to antiretroviral treatment compared to people who are nonadherent is larger than the relative risk for not being in treatment compared to being in treatment, this does not mean that being in antiretroviral treatment and partially adhering is associated with worse outcomes than not being in treatment at all. On the contrary, the risk relations between the different groups based on the assumptions of Table 2 are as follows:
Table 2.
Parameters used in calculating the AAF for people who die of AIDS due to nonadherence to antiretroviral therapy.
| Parameter | Symbol | Value | 95% Confidence Interval | Source |
|---|---|---|---|---|
| Proportion of people on antiretroviral therapy who are not adhering to medication regimen | Pna | 40.1% | (36.9% to 43.3%) | Lima and colleagues [22] |
| Risk ratio of nonadherence to antiretroviral therapy, comparing current drinkers to abstainers | RRdrink | 1.82 | (1.63 to 2.04) | Hendershot and colleagues[18] |
| Mortality risk ratio for nonadherence to antiretroviral therapy compared to those who adhere to antiretroviral therapy | RRna | 3.13 | (1.95 to 5.05) | Lima and colleagues[11] |
| Mortality hazard ratio for people not on antiretroviral therapy treatment compared to those who are | HRnontreat | 2.63 | (1.92 to 3.57) | Murphy and colleagues[23] |
1 = risk of people in antiretroviral treatment adhering on an arbitrary scale
3.13 = risk of people in antiretroviral treatment not adhering to treatment
1.85 = risk of people in antiretroviral treatment overall (assuming 0.401 nonadherent)
4.88 = risk of people not in treatment
Multiple sources were used to characterize the relationship between alcohol consumption and nonadherence to antiretroviral therapy and the effect of nonadherence on HIV/AIDS-related mortality. To characterize the effect of alcohol consumption on antiretroviral adherence, we used the odds ratio of 0.60 (95% CI: 0.53, 0.69) from the meta-analysis performed by Hendershot and colleagues [18,22] for adherence by global drinkers (defined as alcohol consumption within the past month) compared to abstainers. Since there have been no meta-analyses of nonadherence on mortality, we used a hazard ratio of 3.13 (95% CI: 1.95, 5.05) for deaths of people not adhering to treatment (defined as less than 95% of the time) compared to people adhering to treatment, as reported by Lima and colleagues [11]. This estimate is similar to but slightly lower than the hazard ratios of 3.2 and 3.9 for adherence rates of <80% and <90%, respectively, as described in other studies [12,16]. For the rate ratio of HIV/AIDS-related deaths of people on antiretroviral treatment compared to people not on treatment, we used a rate ratio reported by Murphy and colleagues [23] that gives a point estimate of 0.38 (95% CI: 0.28, 0.52). These values were combined to obtain the AAF for HIV/AIDS for a given population. The following sections will first present the derivation of the AAF for HIV/AIDS mortality from nonadherence to antiretroviral therapy and then describe the derivation of the 95% uncertainty intervals associated with these AAFs. Estimations of uncertainty for the calculated AAFs are of critical importance for the estimated burden of disease attributable to alcohol and for policy recommendations aimed at reducing this burden. Table 2 outlines the measures of association used to compute the AAFs for the five African GBD regions and the prevalence of nonadherence to antiretroviral therapy for those who are currently receiving antiretroviral therapy.
Derivation of AAFs for HIV/AIDS
Continuous modeling of the effects of alcohol use on adherence [24,25] was impossible given the data available to us, and thus we limited our analysis to two broad categories: drinkers versus nondrinkers, and antiretroviral therapy adherence (at least 95% of the time) versus nonadherence.
The attributable fraction (AF) is defined as:
where P represents prevalence of exposure and RR represents the relative risk for exposure compared to no exposure. Depending on the design of the original epidemiological study, the RR information could be derived from hazard ratios, risk ratios, or odds ratios.
However, for the AAF of mortality due to not adhering to antiretroviral therapy for people with HIV/AIDS, the lack of research and limited information available on the effects of alcohol on HIV/AIDS forced us to calculate the AAFs for HIV/AIDS-related mortality in several steps (for the definition and calculation of AAF in general, see [26,27]).
First, we calculated the adherence attributable fraction (AdAF) using a definition of nonadherence as adherence to antiretroviral therapy less than 95% of the time. The AdAF represents the fraction of HIV/AIDS-related deaths attributable to nonadherence to antiretroviral therapy, and is calculated as follows:
where Padher is the proportion of people adhering to treatment more than 95% of the time, Pna is the proportion of people adhering to treatment less than 95% of the time, and RRna is the relative risk of mortality for those who are not adhering compared to those who are.
Second, we calculated the nonadherence due to alcohol attributable fraction (NAAAF) - the proportion of nonadherence due to alcohol consumption - as follows:
where Pdrink is the proportion of drinkers among the antiretroviral-treated HIV-infected population, Pabs is the proportion of abstainers, and RRdrink is the relative risk of nonadherence for drinkers compared to nondrinkers. Table 3 outlines the prevalence of current drinkers by age and sex for the five African GBD regions.
Table 3.
Prevalence of current drinkers by region.
| Current Drinkers | ||||||
|---|---|---|---|---|---|---|
| Region | Men (age in years) | Women (age in years) | ||||
| 15 - 34 | 35 - 54 | 55+ | 15 - 34 | 35 - 54 | 55+ | |
| North Africa/Middle East | 7.2% | 12.0% | 5.5% | 3.5% | 1.1% | 0.4% |
| Sub-Saharan Africa, Central | 51.0% | 51.9% | 20.5% | 32.4% | 28.5% | 11.9% |
| Sub-Saharan Africa, East | 24.6% | 38.8% | 37.2% | 16.1% | 24.9% | 21.4% |
| Sub-Saharan Africa, South | 38.0% | 38.0% | 29.5% | 12.6% | 15.7% | 9.8% |
| Sub-Saharan Africa, West | 36.2% | 50.9% | 40.5% | 20.8% | 31.2% | 27.1% |
Finally, we needed to know the proportion of deaths of people under treatment compared to the total number of deaths in the population due to HIV infection. Because the exact numbers are not known, we estimated this proportion using the hazard ratio for deaths in people without treatment compared to people with treatment. This proportion of deaths of people undergoing treatment (PDT) was calculated as follows:
where Ptreat is the proportion of HIV-infected people receiving treatment, Pnontreat is the proportion of HIV-infected people not receiving treatment, and HRnontreat is the hazard ratio of people without treatment. It should be noted that hazard ratio and relative risk are synonymous in this case. These three proportions can be combined to calculate the AAF for HIV/AIDS mortality for a given population.
Estimation of the variance of AAFs
It is possible to derive a mathematical expression of the variance of the AAFs when the variances of each parameter making up the final expression are known. Calculating the variance of the AAF of HIV/AIDS-related mortality requires the combination of several steps. Because these steps involve Taylor series expansions, they yield only an approximation of the real variance. We calculated the variance of the AAFs by calculating the variance of the simplest combinations first, which were then used in more complex functions. The derivations of the variance of two distributions and the derivation of the variances using Taylor series expansions can be found in 'additional file 1 appendix 1'.
In the literature, the uncertainty intervals for AFs due to risk factors based on meta-analyses are usually computed using a Monte Carlo-type method (for alcohol, see [3]). The Monte Carlo method uses repeated random samples of an AF to estimate its variance [28].
The AAF samples are obtained by randomly generating each parameter using the information we have on its distribution. The main advantage of this method is its broad range of applications. The method can be applied to virtually any field and any function and is especially useful in cases in which an algebraic solution to a problem is impossible to derive. Our AAF, however, is a relatively simple function of several independent variables that makes the use of Monte Carlo samples unnecessary. Indeed, an algebraic solution, when possible to obtain, should always be preferred to a simulation, as the results are more precise and require fewer resources. In fact, the results obtained with this method are generated instantaneously on any computer and do not require the use of servers or the handling of large datasets, as is usually the case with a Monte Carlo analysis. In addition, a decomposition of sources of variation and their relative contribution to overall variance can be obtained more readily. Even though it is possible to derive only an approximation of the variance of the original function using second order Taylor series expansions, the assumption that the spread of the function around its mean value is relatively small guarantees an accurate result. The variations around the point estimate of each AF function depend only on the variance of the parameters used; therefore, knowledge of these parameters is important. It should be noted that for large variances of each parameter, the error in the variance of the final function will increase as the assumption of small variations is not satisfied. This is not specific to the analytic expression derived here, but would also affect a Monte Carlo method for which a convergence would not be ensured unless a very large number of data points are collected [29]. Finally, the use of a second order approximation has the advantage of yielding very simple expressions that combine only the derivative of the function and the variance of its parameters; this means that they can be computed nearly instantaneously in R using only a few command lines. It should be noted that in many fields, such as electrical engineering, quantum mechanics, and protein engineering, Taylor series of order two or fewer are used daily and yield excellent results.
Variance of AdAF and NAAAF
Using the variances of Pna and RRna described in the previous section, we derived a mathematical expression for the variance of AdAF and NAAAF using Taylor series expansions. The complete derivations can be found in 'additional file 1, appendix1', and the final expression of the variance of these terms is as follows:
For AdAF:
where
And for NAAAF:
where
Variance of PDT
The variance of the proportion of deaths of HIV-infected people under treatment (PDT) cannot be derived using the above methods. Since the variance of PDT is a function of two variables, we used a Taylor series expansion performed in two dimensions. These derivations are shown in additional file 1, appedx1, and the final expression of the variance is as follows:
where DPtreat and DHRnontreat are the partial derivatives of the PDT function with respect to Ptreat and HRnontreat and can be expressed as follows:
In this manner, the variances of all three components of the final AAF function are determined. Using the variances for AdAF, NAAAF, and PDT, the variance of the AAF can be determined by the variance of (AdAF·NAAAF) PDT (see 'additional file 1, appendix 1').
Computation of variances for hazard ratios and relative risks
Little information on the relative risks and hazard ratios mentioned above is available in the literature. Accordingly, previously published raw data had to be transformed to be useful for our analysis. The following paragraphs describe how these data from various sources yielded values for the relative risks and hazard ratios.
Computation of variance for the hazard ratio for people under treatment
The hazard ratio for people under treatment was taken from Murphy and colleagues [23]. Because relative risks are found using a linear regression on a logarithmic scale, the variance of the parameter on a linear scale has to be estimated. The variance of the logarithm of a variable can be estimated using a second order Taylor series expansion. Thus, we can describe a hazard ratio for which only the variance of its natural logarithm is known as follows:
Computation of variance for the relative risk of death for nonadherence
The relative risk of death for people not adhering to treatment is only known as its logarithmic counterpart. Since the value taken from Lima and colleagues [11] represented the relative risk of people adhering to their treatment, the relative risk used in our formula requires the inverse of this parameter. The variance of the relative risk for nonadherence, RRna, can be derived from the variance of the logarithm of the relative risk of mortality for nonadherence using the following method:
where RRa is the relative risk of mortality for people who adhere to antiretroviral therapy.
Computation of variance for relative risk of nonadherence due to alcohol
The odds ratio for adherence related to alcohol use provided by Hendershot and colleagues [18] can be transformed into a relative risk function following two simple steps:
• Take the inverse of the odds ratio to obtain the odds ratio of nonadherence for drinkers compared to nondrinkers.
• Compute the relative risk for nonadherence for drinkers versus nondrinkers.
The propagation of variance needs to be estimated for each of these steps. The variance of the first step can be approximated in the same manner as the hazard ratio. The relative risk for nonadherence of drinkers compared to nondrinkers is then calculated as follows:
where OR is the odds ratio of nonadherence for drinkers compared to nondrinkers, and P is the proportion of nonadherence among drinkers. Lacking the necessary information about this proportion, we took the proportion of nonadherence of the entire population as a conservative estimate of this value.
The variance of this relative risk can be computed using the Taylor series approximation with two variables as derived for the variance of PDT. In this case, the variance is given by:
with
and
The above relations define the relative risks, hazard ratio, and their respective variances, and allow us to compute the AAF of HIV/AIDS deaths.
Results
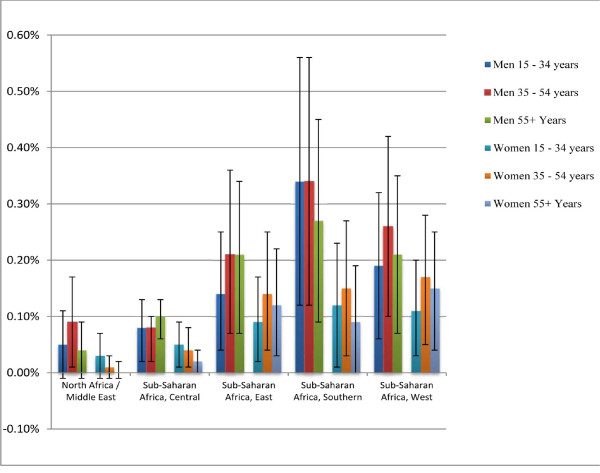
Figure 2 shows the AAFs and their 95% uncertainty intervals for the five African GBD regions, separated by sex and age. Although the effect is small, an inspection of the uncertainty intervals shows that alcohol has a negative effect on the outcome of an HIV infection. Of the five African GBD regions, only the North Africa/Middle East region had strata where the 95% uncertainty intervals crossed 0, with only the men in that region aged 35 to 54 years exhibiting a significant positive AAF.
Figure 2.
Proportions of deaths caused by nonadherence to antiretroviral therapy due to alcohol consumption with their 95% uncertainty intervals for the five African GBD regions, by sex and age.
Overall, in Africa, men have higher AAFs than women, with AAFs generally highest in people under 55 years of age; however, not all of these differences are statistically significant. The highest AAFs are in sub-Saharan Africa, East, where the AAF was 0.34 (95% CI: 0.12, 0.56) for men aged 15 to 34 years, and 0.27 (95% CI: 0.09, 0.45) for men aged 35 to 54 years. In women, the highest AAFs are observed in the sub-Saharan Africa regions; however, unlike the men, the AAFs are very similar for the East, South, and West regions.
Discussion
This method allows a systematic computation of partial AAFs for HIV/AIDS in any given population, including the 95% uncertainty intervals. Despite the limited information available, the results show a clear negative impact of alcohol on adherence to an antiretroviral treatment regime and consequently on the outcome of the disease, especially in the sub-Saharan regions of Africa. Although the AAFs are relatively low, HIV/AIDS was responsible for 58.5 million DALYs in 2004 [7], indicating that the burden of alcohol-attributable nonadherence to HIV/AIDS treatment is substantial.
The very broad categories used to describe alcohol consumption and adherence to antiretroviral therapy do not allow us to distinguish between moderate and heavy drinking or different percentages of nonadherence, and future research will be necessary to estimate a more accurate AAF for HIV/AIDS mortality. Ideally, AAFs would be estimated by using a continuous distribution of alcohol consumption and the risk relations for adherence to antiretroviral treatment associated with each level of consumption, as well as by specific patterns of drinking, such as heavy occasional drinking [30]. Modeling alcohol consumption with these two dimensions continuously and triangulating data obtained from surveys with adult per capita consumption information [31,32] are especially important for countries with high variation in patterns of drinking among drinkers.
These results may not be relevant for all parts of Africa. Many Africans completely abstain from alcohol, while many of those who drink tend to do so heavily, resulting in comparatively small variations in drinking patterns among drinkers http://apps.who.int/globalatlas/default.asp. Since we expect alcohol consumed as part of heavy drinking patterns to interfere more with antiretroviral treatment than moderate patterns of drinking [18,33], our estimates of AAFs based on the dichotomous variable of alcohol consumption (yes/no) constitute conservative estimates of the alcohol-attributable HIV/AIDS disease burden.
It is important to note that both the proportion of drinkers as well the proportion of people on antiretroviral therapy influence the AAF. Indeed, even though the proportion of drinkers in the sub-Saharan Africa, South region, is lower than in the sub-Saharan Africa, West region, the proportion of people in treatment is larger in the South region, which yields a larger overall AAF for this region. It is very likely that alcohol also has an effect on the progress of the disease in people without treatment that we did not estimate, but today's research does not allow us to deduce causality or quantify such an effect [6]. Improving this situation by conducting research to ascertain and quantify the effect of alcohol use on the disease progression of HIV/AIDS-related morbidity and mortality without antiretroviral treatment should be a priority.
Conclusions
Although the presented method could be improved by better definition and quantification of exposure, it provides an evidence-based conservative estimate of the impact of alcohol use on HIV/AIDS mortality and highlights the importance of further research in this field. It also points to the need to integrate alcohol prevention measures [34] into the protocol for antiretroviral treatment.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
GG, KS, and JR conceptualized the overall article, contributed to the methodology, identified sources for risk relations and exposure, and contributed to the writing. GG was responsible for the derivations. All authors have approved the final version.
Supplementary Material
Appendix 1 outlines the derivation of the AAF variance for HIV. The derivations of the variance of the multiplication of two independent random variables and the derivations of the variances of AdAF, NAAAF, and PDT, using Taylor Series expansions for one or multiple variables, are described.
Contributor Information
Gerrit Gmel, Email: gerrit.gmel@gmail.com.
Kevin D Shield, Email: kevin.shield@utoronto.ca.
Jürgen Rehm, Email: jtrehm@aol.com.
Acknowledgements
Financial support for this study was provided to the last author listed above by the National Institute for Alcohol Abuse and Alcoholism (NIAAA) with contract # HHSN267200700041C to conduct the study titled "Alcohol- and Drug-attributable Burden of Disease and Injury in the US." In addition, the last author received a salary and infrastructure support from the Ontario Ministry of Health and Long-Term Care. We would like to thank Gerhard Gmel, Paul Shuper, and Ben Taylor for helpful comments on earlier versions of this manuscript.
References
- World Health Organization. Global Health Risks. Mortality and burden of disease attributable to selected major risks. Geneva, Switzerland; 2009. [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol use disorders. Lancet. 2009;373:2223–22233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rehm J, Baliunas D, Borges GLG, Graham K, Irving HM, Kehoe T, Parry CD, Patra J, Popova L, Poznyak V, Roerecke M, Room R, Samokhvalov AV, Taylor B. The relation between different dimensions of alcohol consumption and burden of disease - An overview. Addiction. 2010;105:817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry CDH, Rehm JR, Poznyak V, Room R. Alcohol and infectious diseases: are there causal linkages? Addiction. 2009;104:331–332. doi: 10.1111/j.1360-0443.2008.02500.x. [DOI] [PubMed] [Google Scholar]
- Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health. 2010;55:159–166. doi: 10.1007/s00038-009-0095-x. [DOI] [PubMed] [Google Scholar]
- Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS - a systematic review. Alcohol Alcohol. 2010;45:159–166. doi: 10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The global burden of disease: 2004 update. Geneva, Switzerland; 2008. [Google Scholar]
- Havlir DV, Richman DD. Viral dynamics of HIV: implications for drug development and therapeutic strategies. Annals of internal medicine. 1996;124:984–994. doi: 10.7326/0003-4819-124-11-199606010-00006. [DOI] [PubMed] [Google Scholar]
- Palella FJ Jr, Deloria-Knoll M, Chmiel JS. Survival benefit of initiating antiretroviral therapy in HIV-infected persons in different CD4+ cell strata. Annals of internal medicine. 2003;138:620–626. doi: 10.7326/0003-4819-138-8-200304150-00007. [DOI] [PubMed] [Google Scholar]
- Jensen-Fangel S, Pedersen L, Pedersen C. Low mortality in HIV-infected patients starting highly active antiretroviral therapy: a comparison with the general population. AIDS. 2004;18:89–97. doi: 10.1097/00002030-200401020-00011. [DOI] [PubMed] [Google Scholar]
- Lima VD, Harrigan R, Bangsberg DR, Hogg RS, Gross R, Yip B, Montaner JS. The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. Journal of Acquired Immune Deficiency Syndromes. 2009;50:529–536. doi: 10.1097/QAI.0b013e31819675e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nachega JB, Hislop M, Dowdy DW, Lo M, Omer SB, Regensberg L, Chaisson RE, Maartens G. Adherence to Highly Active Antiretroviral Therapy assessed by pharmacy claims predicts survival in HIV-infected South African adults. J Acquir Immune Defic Syndr. 2006;43:78–84. doi: 10.1097/01.qai.0000225015.43266.46. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR, Deeks SG. Is average adherence to HIV antiretroviral therapy enough? Journal of general internal medicine. 2002;17:812–813. doi: 10.1046/j.1525-1497.2002.20812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of internal medicine. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Fielden SJ, Rusch MLA, Yip B, Wood E, Shannon K, Levy AR, Muntaner JSG, Hogg RS. Nonadherence increases the risk of hospitalization among HIV-infected antiretroviral naive patients started on HAART. Journal of the International Association of Physicians in AIDS Care: JIAPAC. 2008;7:238–244. doi: 10.1177/1545109708323132. [DOI] [PubMed] [Google Scholar]
- Garcia de Olalla P, Knobel H, Carmona A, Guelar A, Lopez-Colomes JL, Cayla JA. Impact of Adherence and Highly Active Antiretroviral Therapy on Survival in HIV-Infected Patients. Journal of Acquired Immune Deficiency Syndromes. 2002;30:105–110. doi: 10.1097/00126334-200205010-00014. [DOI] [PubMed] [Google Scholar]
- Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, Wilson K, Buchan I, Gill CJ, Cooper C. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Medicine. 2006;11:438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol Use and Antiretroviral Adherence: Review and Meta-Analysis. Journal of Acquired Immune Deficiency Syndromes. 2009;52:180–202. doi: 10.1097/QAI.0b013e3181b18b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. Lippincott, Williams, & Wilkins; 2008. [Google Scholar]
- Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. Lancet. 2010;376:398–400. doi: 10.1016/S0140-6736(10)60884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. 2006 Report on the global AIDS epidemic. Geneva, Switzerland; 2006. [Google Scholar]
- Lima VD, Harrigan R, Murray M, Moore DM, Wood E, Hogg RS, Montaner JSG. Differential impact of adherence on long-term treatment response among naïve HIV-infected individuals. AIDS. 2008;22:2371–2380. doi: 10.1097/QAD.0b013e328315cdd3. [DOI] [PubMed] [Google Scholar]
- Murphy EL, Collier AC, Kalish LA, Assmann SF, Para MF, Flanigan TP, Kumar PN, Mintz L, Wallach FR, Nemo GJ. Highly Active Antiretroviral Therapy Decreases Mortality and Morbidity in Patients with Advanced HIV Disease. Annals of internal medicine. 2001;135:17–26. doi: 10.7326/0003-4819-135-1-200107030-00005. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. On the comparable quantification of health risks: lessons from the Global Burden of Disease Study. Epidemiology. 1999;10:594–605. doi: 10.1097/00001648-199909000-00029. [DOI] [PubMed] [Google Scholar]
- Ezzati M, Lopez AD, Rodgers A, Murray CJL. Comparative Quantification of Health Risks. Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Geneva: World Health Organization; 2004. [Google Scholar]
- Walter SD. The estimation and interpretation of attributable risk in health research. Biometrics. 1976;32:829–849. doi: 10.2307/2529268. [DOI] [PubMed] [Google Scholar]
- Walter SD. Prevention of multifactorial disease. Am J Epidemiol. 1980;112:409–416. doi: 10.1093/oxfordjournals.aje.a113007. [DOI] [PubMed] [Google Scholar]
- Kalos MH, Whitlock PA. Monte Carlo Methods. Weinheim, Germany: WILEY-VCH; 2008. [Google Scholar]
- Gmel Gj, Shield K, Frick H, Kehoe T, Gmel Gs, Rehm J. Estimating uncertainty for alcohol-attributable fractions for infectious and chronic diseases. BMC Medical Research Methodology. 2010. in press . [DOI] [PMC free article] [PubMed]
- Gmel G, Kuntsche E, Rehm J. Risky single occasion drinking: bingeing is not bingeing. Addiction. 2010. in press . [DOI] [PubMed]
- Rehm J, Klotsche J, Patra J. Comparative quantification of alcohol exposure as risk factor for global burden of disease. Int J Methods Psychiatr Res. 2007;16:66–76. doi: 10.1002/mpr.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Kehoe T, Gmel G, Stinson F, Grant B, Gmel G. Statistical modelling of volume of alcohol exposure for epidemiological studies of population health: the example of the US. Popul Health Metr. 2010;8:3. doi: 10.1186/1478-7954-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcellin F, Boyer S, Potopopescu C, Dia A, Ongolo-Zogo P, Koulla-Shiro S, Abega SC, Abe C, Moatti JP, Spire B, Carrieri MP. Determinants of unplanned antiretroviral treatment interruptions among people living with HIV in Yaoundé, Cameroon. Tropical medicine & international health. 2008;13:1470–1478. doi: 10.1111/j.1365-3156.2008.02170.x. [DOI] [PubMed] [Google Scholar]
- Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, Grube J, Gruenewald P, Hill L, Holder H, Homel R, Livingston M, Österberg E, Rehm J, Room R, Rossow I. Alcohol: No ordinary commodity. Research and public policy. 2. Oxford and London: Oxford University Press; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1 outlines the derivation of the AAF variance for HIV. The derivations of the variance of the multiplication of two independent random variables and the derivations of the variances of AdAF, NAAAF, and PDT, using Taylor Series expansions for one or multiple variables, are described.