Abstract
Ciclesonide is a novel inhaled corticosteroid used in the continuous treatment of mild-to-severe asthma. Its formulation and mechanism of action yield a low oral and systemic bioavailability, and high pulmonary deposition. In multiple clinical trials, ciclesonide is at least as effective as either fluticasone propionate or budesonide at symptom control, while in many cases having improved safety outcomes and tolerability. The improved safety and comparable efficacy profiles of ciclesonide demonstrated in current studies could potentially yield a treatment option that may lead to improved adherence and outcome.
Keywords: ciclesonide, asthma, inhaled corticosteroid
Introduction
Asthma poses a significant burden to society in terms of morbidity, mortality, quality of life, and healthcare costs.1–3 Among children, asthma rates in the United States are currently at record highs, with a nationwide prevalence of approximately 9% of children aged 1 to 17 years.3 Its burden on the economy is estimated at between US$4 to 6 billion annually, considering healthcare costs and lost work days for caregivers and patients alike.4 Inhaled corticosteroids (ICS) are recommended as first-line therapy for the treatment of asthma,5,6 and can improve both asthma symptomatology and the markers of airway inflammation.7–9 However, despite being demonstrated as an efficacious controller therapy, concerns remain regarding the potential for adverse side effects associated with chronic ICS treatment. Specifically, some ICS molecules have been demonstrated to cause reductions in growth velocity9–11 and bone mineral density,12,13 HPA-axis suppression,14,15 and oral candidiasis.16,17
Ciclesonide (Alvesco®; Sepracor, Inc., Nycomed, Inc.) is a novel, new corticosteroid developed for the treatment of mild to severe persistent asthma. It is delivered by metered-dose inhaler (MDI) once daily or twice daily (dosing depends on country). This review will focus on the safety and efficacy profile of ciclesonide, as well as to establish its mechanism of action.
Mechanism of action
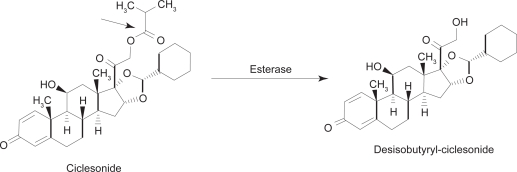
Ciclesonide ([R]-11β, 16α, 17, 21-tetrahydroxypregna-1,4-diene-3,20-dione cyclic 16,17-acetal with cyclohexanecarboxaldehyde 21-isobutyrate; CIC) is inhaled into the lungs via hydrofluoroalkane-MDI (HFA-MDI), where it is converted by local esterases to its active metabolite, desisobutyryl-ciclesonide (des-CIC, Figure 1). Relative to dexamethasone (100), CIC has a low glucocorticoid receptor binding affinity of 12, while des-CIC has a significantly higher binding affinity of 1212.18,19 Studies demonstrate no conversion of R-CIC or des-CIC to the S-epimer in vivo, which has different physicochemical properties, and a markedly lower receptor affinity.20 Pharmacokinetic profiles of des-CIC were similar in comparative healthy and asthma patients, likely indicating that bronchial narrowing and airway inflammation do not affect the distribution of CIC and its subsequent activation to des-CIC in the lungs.21 An additional study also demonstrated equivalent PK/PD profiles of CIC-HFA when administered with and without a spacer.22
Figure 1.
Molecular structure of ciclesonide and its activated metabolite, desisobutyryl-ciclesonide (des-CIC). Christie P. Ciclesonide: A novel inhaled corticosteroid for asthma. Drugs Today (Barc). 2004; 40(7):569–576.19 Copyright © 2004 Prous Science, S.A.U. All rights reserved.
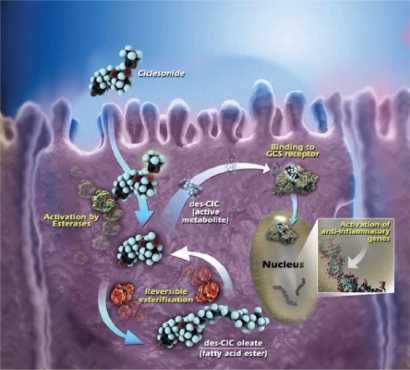
In vitro data indicate metabolism of des-CIC was different in precision-cut human lung and liver tissue slices.23 After 24 hours incubation with [14C]-CIC, 7.2 times more radioactivity was present in the lung tissue, as compared with the liver. Furthermore, in the lung tissue [14C]-CIC was converted to des-CIC and subsequently conjugated with fatty acid metabolites, a reversible process which increases lipophilicity of des-CIC and may result in prolonged drug retention and anti-inflammatory activity in the lung (Figure 2).23,24 Alternatively, [14C]-CIC was catabolically inactivated in liver tissue into at least 5 different polar compounds, with dihydroxylated des-CIC being the major metabolite.23 Additionally, other findings demonstrated that orally and intravenous-administered [14C]-CIC resulted in a negligible serum concentration of des-CIC and no accumulation in red blood cells, indicating a low absorption and almost complete first-pass metabolism (systemic bioavailability of des-CIC < 1%).25
Figure 2.
Intracellular activation of ciclesonide and reversible esterification of desisobutyryl-ciclesonide (des-CIC). Ciclesonide is activated by intracellular esterases to active metabolite, des-CIC, which has high affinity to the glucocorticosteroid (GCS) receptor. Desisobutyryl-ciclesonide can undergo reversible esterification to des-CIC oleate (fatty acid ester). Reprinted with permission from Nave R, Meyer W, Fuhst R, Zech K. Formation of fatty acid conjugates of ciclesonide active metabolite in the rat lung after 4-week inhalation of ciclesonide. Pulm Pharmacol Ther. 2005;18:390–396.62 Copyright © 2005 Elsevier.
The demonstrated mean lung deposition of CIC is 52%.26 The internal diameter of the smallest airways in adults are typically ∼2 μm, thus, it can be inferred that smaller ICS particles lead to greater pulmonary deposition and more even distribution throughout the lungs (Table 1). Accordingly, the HFA-MDI formulation of CIC contains a majority of ICS particles which range between 1.1 and 2.1 μm.27,28 This particle size is likely related to the high observed pulmonary deposition of CIC.28 Furthermore, uptake of CIC, budesonide (BUD), and fluticasone propionate (FP) in human alveolar type II epithelial cells (A549) was measured, and at all incubation timepoints, intracellular concentration of CIC was higher than that of BUD and FP.29 This indicates a more rapid uptake of CIC molecules into target tissue, and at a higher concentration. Additionally, separate in vitro data indicate intracellular concentration of des-CIC in A549 cells to be maintained for >20 hours.29
Table 1.
Characteristics of ciclesonide
| Method of delivery | HFA-MDI |
|---|---|
| Particle size27 | 1.1–2.1 μm |
| Pulmonary Deposition26 | 52% |
| Oral deposition26 | 38% |
| Systemic bioavailability30 | CIC = 18% Des-CIC = 50% |
| Serum protein binding (des-CIC)62 | ∼99%, <1% unbound fraction |
| Target tissue retention (des-CIC)25 | >24 hours |
| Mean terminal half-life (t1/2; des-CIC)27 | 3.5 hours |
| Elimination half-life (t1/2; CIC)27 | 0.71 hours |
Abbreviations: CIC, ciclesonide; des-CIC, desisobutyryl-ciclesonide; HFA-MDI, hydrofluoroalkane metered dose inhaler.
Efficacy
Placebo-controlled
The therapeutic action of ciclesonide is achieved after the inhaled parent compound (CIC) is cleaved by esterases in the lungs to its active metabolite (des-CIC), a corticosteroid with high receptor affinity and anti-inflammatory activity.18,19,30 In a randomized, double-blind trial, early (EAR) and late (LAR) phase allergen-induced asthmatic reactions were significantly inhibited (p < 0.05) by treatment with CIC, versus placebo (as evaluated by decrease in FEV1 following allergen challenge).31 These anti-imflammatory properties were also exhibited in vitro, as CIC attenuated EAR/LAR, infiltration of inflammatory cells into bronchoalveolar lumen, and airway hyperresponsiveness in sensitized Brown Norway rats.32 These effects were observed in a dose-dependent manner.
These anti-inflammatory properties have been noted in patients with mild, persistent asthma, treated with CIC 160 μg (all doses noted in this review are ex-actuator) once-daily over a period of 4 weeks.33 Measurements were made before and after treatment in this double-blind study for adenosine monophosphate (AMP) bronchial challenge, and exhaled nitric oxide (eNO). Mean AMP challenge PC20 following ciclesonide treatment was significantly increased (p < 0.001) compared to placebo, and decreases in eNO (ppb) and induced sputum eosinophil cell counts were also noted.33 Additionally, Bateman et al34 demonstrated the effectiveness of CIC 320 μg and 640 μg in reducing oral corticosteroid use in adults with severe, persistent asthma, versus placebo.
Three double-blind studies demonstrated that treatment with CIC improves symptom control in patients who were previously treated with another ICS. O’Connor, et al35 demonstrated significant improvement in FEV1 in moderate-to-severe asthmatics treated with either CIC 800 μg or 1600 μg daily, compared to placebo (12-week treatment, pretreatment with 800–2000 μg/day BDP). A similarly designed study by Langdon et al36 noted improvements in baseline FEV1 and morning PEF in subjects treated with CIC over a period of 12 weeks, but at more clinically-relevant doses (CIC 80 μg, 320 μg daily, versus placebo). Subjects were also previously treated with lower, constant doses of BDP or its equivalent (400–800 μg daily) for at least 4 weeks prior to randomization. Asthma control in previously treated subjects was maintained by CIC 160 μg or 640 μg once daily in another study by Chapman.37
In a large, double-blind, 12-week study (n = 1031), Gelfand38 studied the effect of multiple strength doses of CIC (40 μg, 80 μg, or 160 μg) on children aged 4 to 11 with mild to severe persistent asthma. Following run-in, subjects were randomized to one of three once-daily CIC treatments, or placebo. All CIC doses were associated with significant increases in FEV1 compared to placebo at study endpoint (CIC 40 μg, 11.91; CIC 80 μg, 13.58; CIC 160 μg, 14.17). Reductions in rescue medication use within study treatment cohorts were also reported.
Comparative studies
Once-daily dosing of CIC (which is approved in some, but not all countries) is a significant distinction between it and other common ICS for treatment of asthma, such as BUD and FP. Currently, there have not been any comparative efficacy trials between CIC and mometasone furoate, another commonly used ICS which is approved for once-daily dosing; future studies should directly compare efficacy of these two agents. CIC has demonstrated efficacy with a single daily dose,33–42 as well as when administered either in the morning or evening.39 The effectiveness of a single daily dose could lead to improved compliance and symptom control in patients using CIC as asthma control therapy.
CIC comparative efficacy trials are summarized in Table 2. Ukena43 demonstrated CIC 320 μg once daily to be superior to BUD 200 μg twice-daily in increasing FEV1 from baseline (416 mL in CIC versus 321 mL in BUD; p = 0.019, 95% CI). While improvements were seen in FVC for both cohorts, a significantly larger difference was seen in CIC-treated subjects. Additionally, significant improvement versus baseline in morning PEF was seen after Day 2 in the CIC cohort (p = 0.039 versus baseline) and Day 7 in the BUD cohort (p = 0.047 versus baseline), indicating a more rapid onset of action for CIC.
Table 2.
Ciclesonide comparative efficacy trials
| Author/citation | Dosing | Subject characteristics | Treatment duration | Outcome |
|---|---|---|---|---|
| Knox40, 2007 | CIC 160 μg qd; FP 250 μg bid | 17–75 y; controlled asthma w/pretreatmenta | 2-week baseline w/current ICS, 12 week treatment | CIC and FP had similar FEV1 maintenance and symptom-free days |
| Lee41, 2004 | CIC 160 μg qd; FP 110 μg bid; placebo | mild to moderate asthmatics | separate 4 week treatment arms, separated by 2-week washout w/ salmeterol + montelukast | No difference between groups in methacholine PC20 hyperresponsiveness |
| Buhl42, 2006 | CIC 160 μg qd; FP 88 μg bid | 12–74 y; mild to moderate asthma (GINA) | 1- to 2-week baseline w/rescue med only; 12-week treatment | CIC and FP similarly improved lung function, symptom scores, and rescue med use. During last 4 weeks, CIC had higher percentage of symptom-free days |
| Niphadkar44, 2005 | CIC 160 μg qd; BUD 200 μg bid | adults w/ FEV1 ≤ 70%, pretreated | 12 weeks, 2-week run-in w/BUD 200 μg bid | CIC as effective as BUD at symptom control |
| Boulet45, 2006 | CIC 320 μg qd; BUD 200 μg bid | pretreated, FEV1 inc. ≥ 7% and 65%–90% pred. after run-in | 2-week baseline w/ BUD 1600 μg qd, 12-week treatment | CIC qd as effective as BUD bid |
| Hansel46, 2006 | CIC 80 μg qd; CIC 320 μg qd; BUD 200 μg bid | FEV1 50%–90% pred. | 12 weeks | CIC and BUD improved FEV1, FVC, and PEF similarly |
| von Berg47, 2007 | CIC 160 μg qd; BUD 400 μg qd | children w/moderate to severe asthma (GINA 1995) | 2- to 4-week run-in w/rescue med only, 12 week treatment | CIC and BUD similarly improved FEV1, morning PEF, rescue med use, and QoL scores |
| Vermeulen48, 2007 | CIC 320 μg qd; BUD 800 μg qd | Children 12–17 y w/severe asthma (GINA 1995) | 2-week baseline w/BUD 400 μg qd, 12-week treatment | CIC and BUD comparably improved FEV1, FVC, PEF, symptom-free days, and rescue med use |
| Boulet49, 2007 | CIC 320 μg qd; FP 200 μg bid | 12–75 y; FEV1 ≥ 80% w/pretreatment, or FEV1 60–80 and pred | 1- to 4-week run-in, 12-week treatment | CIC and FP similarly increased FEV1 and resulted in comparable numbers of symptom-free days |
| Bateman50, 2008 | CIC 320 μg bid; FP 330 μg bid | 12–75 y; moderate to severe controlled asthma w/pretreatment | 2-week baseline w/current ICS, 24-week treatment | CIC and FP maintained FEV1, and improved morning/evening PEF, rescue med use, and QoL scores |
| Pedersen51, 2006 | CIC 80 μg bid; FP 88 μg bid | symptomatic children 6–15 y; FEV1 50%–90% pred | 2- to 4-week baseline w/rescue med only; 12-week treatment | CIC and FP similarly improved FEV1, morning/evening PEF, rescue med usage, and reported symptoms |
Pretreatment defined as subjects having daily ICS treatment prior to randomization. All doses noted are ex-actuator.
Abbreviations: BUD, budesonide; CIC, ciclesonide; FP, fluticasone propionate; ICS, inhaled corticosteroids.
However, these findings appear to be an outlier, as the majority of trials have found CIC at least as effective as BUD (Turbuhaler®/DPI) in controlling asthma, in varying subject populations and disease severities.44–48 FEV1 improvement was noted in these studies with both BUD and CIC, and no significant between-group differences were noted. Pediatric Asthma Quality of Life Questionnaire (PAQLQ) and Pediatric Asthma Caregiver’s Quality of Life Questionnaire (PACQLQ) scores were similarly improved over a 12-week study comparing CIC 160 μg once daily to BUD 400 μg once daily.47 Some modest benefit was seen for CIC, with Boulet45 finding a greater percentage of symptom-free days for CIC (43%) than BUD (34%; p = 0.0288), but overall, both ICS seem to be comparably efficacious. Similarly, comparative studies between CIC and FP show clear non-inferiority of CIC.40–42,49–51 No difference in comparative efficacy was observed when comparing CIC to both FP-DPI49 and FP-MDI.40–42,50,51 FP and CIC were equally effective at maintaining asthma control in subjects who were on continuous ICS therapy prior to randomization.40,50
Safety and tolerability
Oral candidiasis
Considering CIC is relatively inactive, and is converted to active des-CIC in the lungs versus some conversion in the oral cavity, this profile would suggest a lower oropharyngeal deposition and frequency of side effects (ie, candidiasis). Indeed, comparative studies indicate low deposition and activated des-CIC within the oropharynx. Two similarly designed studies compared CIC to FP52 and BUD53, using mouthwash solutions containing 50% ethanol at 5 time points (immediate, 15, 30, 45, and 60 minutes after inhalation) to compare deposition. The sum of CIC and des-CIC molar AUCs0–60 min was 53% (95% CI: 40%–69%) of FP deposition52 and 47% of the BUD deposition.53 Furthermore, oral deposition of des-CIC was less than 10% that of FP and BUD.
Incidence of candidiasis from continuous ICS treatment is a concern, and a common reason for poor adherence, and in some cases, not beginning an asthma patient on an ICS treatment regimen.16 For example, in one of the aforementioned efficacy studies, 9 cases of candidiasis were noted (over a 12-week treatment period) among subjects receiving FP 200 μg twice-daily, compared to no reported cases in subjects treated with CIC 320 once-daily.49 Likewise, Gelfand38 found the incidence of oral candidiasis and pharyngitis over a 12-week treatment period with CIC 40 μg, 80 μg, and 160 μg to be not significantly different from placebo. This finding is consistent with that of Pearlman,54 who found incidences of oropharyngeal side effects similar to placebo in patients treated with CIC 80 μg, 160 μg, or 320 μg over the same duration.
HPA-axis function
Concerns of ICS acting as endogenous glucocorticoids, thereby suppressing the HPA-axis, have resulted in reluctance of some physicians to prescribe such a treatment continuously. CIC has high protein binding and high systemic clearance, a profile that would seem to minimize interference with normal HPA-axis function. In one double-blind, randomized, crossover trial, Agertoft55 studied children aged 6 to 12 years who were given placebo, CIC 40 μg, 80 μg, or 160 μg once daily during four 2-week treatment periods, followed by 2-week washouts. Analysis of 12 hours urinary cortisol at the end of each treatment period yielded no significant between-group differences or dose-response effects. This is of interest because these subjects were given clinically relevant doses of CIC for their age and disease severity.
Vermeulen et al48 found that over 12 weeks of treatment in children, CIC 320 μg once-daily was not associated with a significant decrease in 24 urinary free cortisol (Δ = +1.05; nmol/mmol), while BUD 800 μg once daily was (Δ = −2.63). This between-group difference was significant (p = 0.003). Adult patients (n = 60, ≥18 years) in a separate study were randomized to receive CIC 320 μg or 640 μg twice daily, FP 440 μg or 880 μg twice daily (CFC-MDI), or placebo. Neither CIC nor FP treatment was associated with a significant change in mean serum cortisol AUC0–24 h at these clinically relevant doses.56 Alternatively, a study by Lipworth et al using the same comparative doses of FP and CIC, found evidence of adrenal suppression by FP, using cosyntropin-stimulated peak serum cortisol levels to analyze HPA-axis function.57
Noteworthy is that this pattern of adrenal safety continued even when CIC was administered in doses higher than would normally be used in clinical practice. Derom et al58 concluded that doses as high as CIC 640 μg twice daily had no significant effect on mean urinary cortisol levels (AUC0–24 h), while FP 440 μg and 880 μg twice daily suppressed them by 29% (95% CI, 15–41), compared with placebo. Decreases in PC20 hyperresponsiveness were similar in all cohorts.58 In the previously mentioned study by Szefler,56 serum and urinary cortisol suppression was associated with high-dose FP 2000 μg daily, but not with CIC 1600 μg daily.56 Again, airway outcomes (PC20 hyperresponsiveness, exhaled nitric oxide) were improved with both treatments.
Growth effects
The effects of continuous CIC treatment on childhood growth velocity have been studied. Knemometry, though not a predictor of long-term growth velocity or final adult height, is an extremely sensitive measure of short-term changes in lower-leg growth. This method was utilized by Agertoft55 to determine if 2-week treatment with CIC 40 μg, 80 μg, and 160 μg once daily resulted in any short-term changes in growth velocity. Lower leg growth rates for CIC were not significantly different from placebo, and no dose-response effects were noted (placebo: 0.412 mm/week; CIC 40: 0.425 mm/week; CIC 80: 0.397 mm/week; CIC 160: 0.370 mm/week).
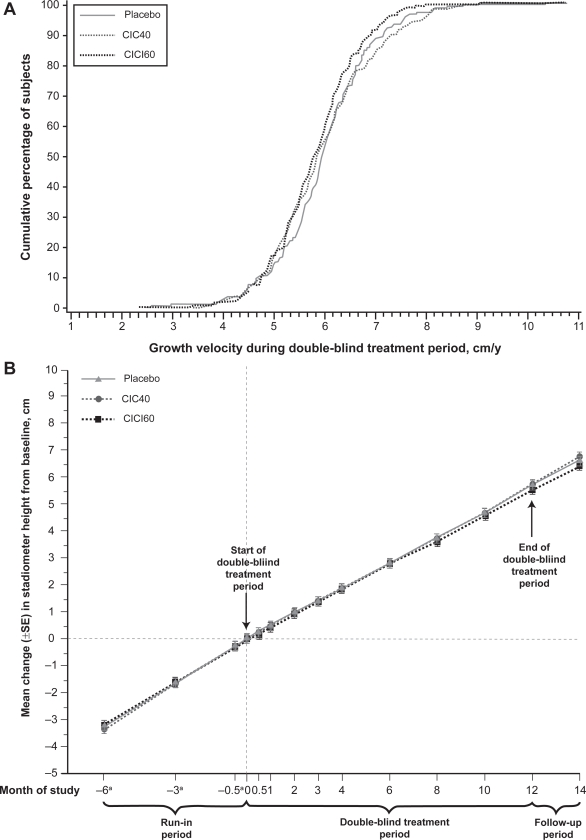
To date, the only long-term assessment of growth velocity in children treated with CIC was completed by Skoner et al59 where height was assessed by stadiometry. Children (n = 661) aged 5 to 8½ years were randomized to receive placebo, CIC 40 μg, or CIC 160 μg once daily, for a treatment period of 1 year. Mean differences in yearly height from placebo (5.75 cm/year) were nonsignificant (−0.02 cm/year for CIC 40 and −0.15 cm/year for CIC 160), illustrating the noninferiority of CIC for growth velocity, when compared to placebo (Figure 3).59 Ideally, a study similar to that of Agertoft and Pedersen,60 which determined children treated with BUD eventually reached normal adult height despite some initial reduction in growth velocity, should be performed with CIC.
Figure 3.
Subjects in all cohorts (CIC40, CIC160, placebo) achieved virtually the same growth velocity during one year of continuous CIC treatment. Reprinted with permission from Skoner DP, Maspero J, Banerji D, and the Ciclesonide Pediatric Growth Study Group. Assessment of the Long-term Safety of Inhaled Ciclesonide on Growth in Children with Asthma. Pediatrics. 2008 Jan;121(1):e1–14.59 Copyright © 2008 American Academy of Pediatrics.
Conclusion
From the evidence currently available, CIC appears to be a novel, safe, and efficacious ICS for use in the continuous treatment of asthma. The low oral bioavailability can likely be attributed to the low affinity of CIC to glucocorticoid receptors, as compared to its active metabolite, des-CIC, which is activated in the lungs. des-CIC is highly lipid conjugated in the lungs, allowing for greater retention in target tissues, and clinically, once-daily dosing (in at least some patients). While these pharmacokinetic properties result in an efficacious ICS, they directly contribute to the noticeably enhanced safety profile of CIC, especially in comparison with other ICS molecules, such as BUD and FP. High protein binding and the aforementioned receptor affinity of CIC result in low systemic bioavailability, and potentially explain the low occurrence of adverse events such as candidiasis, adrenal suppression, and growth velocity disturbance. Comparative studies indicate the effectiveness of CIC to be similar to that of FP and BUD, but with an improved safety profile, indicating the potential of this alternative treatment option in patients concerned about the risks of continuous ICS treatment. Minimizing risk of treatment while maintaining efficacy is a top clinical priority to improve treatment adherence and gain optimal outcome of therapy.
Footnotes
Disclosures
Speakers’ Bureau: AstraZeneca, Sanofi-Aventis, GlaxoSmithKline, Merck, Inc., Schering Plough Laboratories, Inc., Novartis Pharmaceuticals Corp. Grant/Research Support: AstraZeneca, Sanofi-Aventis, GlaxoSmithKline, Novartis Pharmaceuticals Corp., Merck, Inc., Greer Laboratories, Inc., Alcon Laboratories, Inc., Schering-Plough. Consultant: Merck, Inc., Nycomed, Schering-Plough.
References
- 1.Fuhlbrigge AL, Adams RJ, Guillbert TW, et al. The burden of asthma in the United States. Am J Repir Crit Care Med. 2002;166:1044–1049. doi: 10.1164/rccm.2107057. [DOI] [PubMed] [Google Scholar]
- 2.Kivity S, Shochat Z, Bressler R, Wiener M, Lerman Y. The characteristics of bronchial asthma among a young adult population. Chest. 1995;108:24–27. doi: 10.1378/chest.108.1.24. [DOI] [PubMed] [Google Scholar]
- 3.Akinbami L. Hyattsville, MD: National Center for Health Statistics; 2006. The state of childhood asthma, United States 1980–2005. Advance data from vital and health statistics: no 381. [Google Scholar]
- 4.Mannino DM, Homa DM, Akinbami LJ, et al. Surveillance for asthma – United States 1980–1999. MMWR Surveill Summ. 2002 Mar 29;51(1):1–13. [PubMed] [Google Scholar]
- 5.National Asthma Education and Prevention Program . Bethesda, MD: National Institutes of Health, National Heart, Lung and Blood Institute; Aug, 2007. NAEPP Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma – Full Report 2007. [Google Scholar]
- 6.Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2007. Available from: http://www.ginasthma.org.
- 7.Pedersen S, Hansen OR. Budesonide treatment of moderate and severe asthma in children: a dose-response study. J Allergy Clin Immunol. 1995;95(1pt 1):29–33. doi: 10.1016/s0091-6749(95)70149-4. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro G, Mendelson L, Kraemer M, Cruz-Rivera M, Walton-Bowen K, Smith JA. Efficacy and safety of budesonide inhalation suspension in young children with inhaled steroid-dependent, persistent asthma. J Allergy Clin Immunol. 1998;102:789–796. doi: 10.1016/s0091-6749(98)70019-3. [DOI] [PubMed] [Google Scholar]
- 9.Skoner DP. Balancing safety and efficacy in pediatric asthma management. Pediatrics. 2002;109(2 suppl):381–392. [PubMed] [Google Scholar]
- 10.Becker AB, Kuznetsova O, Vermeulen J, et al. Pediatric Montelukast Linear Growth Study Group Linear growth in prepubertal asthmatic children treated with montelukast, beclomethasone, or placebo: a 56-week randomized double-blind study. Ann Allergy Asthma Immunol. 2006;96(6):800–807. doi: 10.1016/s1081-1206(10)61342-7. [DOI] [PubMed] [Google Scholar]
- 11.Simons FE. A comparison of beclomethasone, salmeterol, and placebo in children with asthma. Canadian Beclomethasone Dipropionate-Salmeterol Xinafoate Study Group. N Engl J Med. 1997;337(23):1659–1665. doi: 10.1056/NEJM199712043372304. [DOI] [PubMed] [Google Scholar]
- 12.Hanania NA, Chapman KR, Sturtridge WC, et al. Dose-related decrease in bone density among asthmatic patients treated with inhaled corticosteroids. J Allergy Clin Immunol. 1995;96(5Pt 1):571–579. doi: 10.1016/s0091-6749(95)70254-7. [DOI] [PubMed] [Google Scholar]
- 13.Israel E, Banerjee TR, Fitzmaurice GM, Kotlov TV, LaHive K, LeBoff MS. Effects of inhaled glucocorticoids on bone density in premenopausal women. N Engl J Med. 2001;345(13):941–947. doi: 10.1056/NEJMoa002304. [DOI] [PubMed] [Google Scholar]
- 14.Zollner EW. Hypothalamic-pituitary-adrenal axis suppression in asthmatic children on inhaled corticosteroids (Part 2) – the risk as determined by gold standard adrenal function tests: a systematic review. Pediatr Allergy Immunol. 2007;18(6):469–474. doi: 10.1111/j.1399-3038.2007.00539.x. [DOI] [PubMed] [Google Scholar]
- 15.Chrousos GP, Ghaly L, Shedden A, Iezzoni DG, Harris AG. Effects of mometasone furoate dry powder inhaler and beclomethasone dipropionate hydrofluoroalkane and chlorofluorocarbon on the hypothalamic-pituitary-adrenal axis in asthmatic subjects. Chest. 2005;128(1):70–77. doi: 10.1378/chest.128.1.70. [DOI] [PubMed] [Google Scholar]
- 16.Rachelefsky GS, Liao Y, Faruqi R. Impact of inhaled corticosteroid-induced oropharyngeal adverse events: results from a meta-analysis. Ann Allergy Asthma Immunol. 2007;98(3):225–238. doi: 10.1016/S1081-1206(10)60711-9. [DOI] [PubMed] [Google Scholar]
- 17.Fukushima C, Matsuse H, Saeki S, et al. Salivary IgA and oral candidiasis in asthmatic patients treated with inhaled corticosteroid. J Asthma. 2005;42(7):601–604. doi: 10.1080/02770900500216259. [DOI] [PubMed] [Google Scholar]
- 18.Stoeck M, Riedel R, Hochhaus G, et al. In vitro and in vivo anti-inflammatory activity of the new glucocorticoid ciclesonide. J Pharmacol Exp Ther. 2004;309:249–258. doi: 10.1124/jpet.103.059592. [DOI] [PubMed] [Google Scholar]
- 19.Christie P. Ciclesonide: A novel inhaled corticosteroid for asthma. Drugs Today (Barc) 2004;40(7):569–576. doi: 10.1358/dot.2004.40.7.850475. [DOI] [PubMed] [Google Scholar]
- 20.Nave R, Drollman A, Meyer W, Zech K. In vivo epimeric stability of ciclesonide. Am J Respir Crit Care Med. 2003;167 Abstract A1485. [Google Scholar]
- 21.Nave R, Gunawardena KA, Zech K, Bethke TD. Pharmacokinetic disposition of inhaled ciclesonide and its metabolite desisobutyryl-ciclesonide in healthy subjects and patients with asthma are similar. Int J Clin Pharm Ther. 2006;44(1):1–7. doi: 10.5414/cpp44001. [DOI] [PubMed] [Google Scholar]
- 22.Drollmann A, Nave R, Steinijans VW, Baumgartner E, Bethke TD. Equivalent pharmacokinetics of the active metabolite of ciclesonide with and without use of the AeroChamber Plus spacer for inhalation. Clin Pharmacokinet. 2006;45:729–736. doi: 10.2165/00003088-200645070-00007. [DOI] [PubMed] [Google Scholar]
- 23.Nave R, Fisher R, Zech K. In vitro metabolism of ciclesonide in human lung and liver precision-cut tissue slices. Biopharm Drug Dispos. 2006;27:197–207. doi: 10.1002/bdd.500. [DOI] [PubMed] [Google Scholar]
- 24.Nave R, Fischer R, McCracken N. In vitro metabolism of beclomethasone dipropionate, budesonide, ciclesonide, and fluticasone propionate in human lung precision-cut tissue slices. Respir Res. 2007;8:65. doi: 10.1186/1465-9921-8-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nave R, Bethke TD, van Marle SP, Zech K. Pharmacokinetics of [14C]-Ciclesonide after oral administration to healthy subjects. Clin Pharmacokinet. 2004;43(7):479–486. doi: 10.2165/00003088-200443070-00004. [DOI] [PubMed] [Google Scholar]
- 26.Drollman A, Hasselquist BE, Boudreau RJ, et al. Ciclesonide shows high lung deposition in 2D and 3D-imaging. Am J Respr Crit Care Med. 2002;165 Abstract A40. [Google Scholar]
- 27.Rohtagi S, Arya V, Zech K, et al. Population pharmacokinetics and pharmacodynamics of ciclesonide. J Clin Pharmacol. 2003;43:365–378. doi: 10.1177/0091270002250998. [DOI] [PubMed] [Google Scholar]
- 28.Leach C, Bethke T, Boudreau R. 2-D and 3-D imaging show ciclesonide has high lung deposition and peripheral distribution: a nonrandomized study in healthy volunteers. J Aerosol Med. 2006;19:117–126. doi: 10.1089/jam.2006.19.117. [DOI] [PubMed] [Google Scholar]
- 29.Nave R, Sato H, Nonaka T, Mochiduki T, Takahama S, Kondo S. Uptake, retention and metabolism of ciclesonide in human alveolar epithelial cells. Eur Respir J. 2005;26(suppl 49):255s. [Google Scholar]
- 30.Reynolds RA, Scott LJ. Ciclesonide. Drugs. 2004;64(5):511–519. doi: 10.2165/00003495-200464050-00005. [DOI] [PubMed] [Google Scholar]
- 31.Dahl R, Nielsen LP, Christensen MB, Engelstätter R. Ciclesonide – an inhaled corticosteroid prodrug – inhibits allergen induced early and late phase reactions. Eur Respir J. 1998;12(suppl 28):26s. Abstract P0475. [Google Scholar]
- 32.Nonaka T, Sugiyama H, Taneda M, et al. Effect of a novel inhaled glucocorticoid, ciclesonide, on an allergen-induced asthmatic response in rats and its prolonged anti-inflammatory activity in vitro. Eur Respir J. 2002;20(suppl 38) Abstract P652. [Google Scholar]
- 33.Wilson AM, Duong M, Pratt B, Dolovich M, O’Byrne PM. Anti-inflammatory effects of once daily low dose inhaled ciclesonide in mild to moderate asthmatic patients. Allergy. 2006;61:537–542. doi: 10.1111/j.1398-9995.2006.01061.x. [DOI] [PubMed] [Google Scholar]
- 34.Bateman E, Karpel J, Casale T, Wenzel S, Banerji D. Ciclesonide reduces the need for oral steroid use in adult patients with severe, persistent asthma. Chest. 2006;129:1176–1187. doi: 10.1378/chest.129.5.1176. [DOI] [PubMed] [Google Scholar]
- 35.O’Connor BJ, Kilfeather S, Cheung D, et al. Treatment of moderate to severe asthma with ciclesonide: a long-term investigation over 52 weeks. Eur Respir J. 2002;20(suppl 38) Abstract 2579. [Google Scholar]
- 36.Langdon CG, Adler M, Mehra S, Alexander M, Drollman A. Once-daily ciclesonide is safe and effective in patients with persistent asthma. Respir Med. 2005;99:1275–1285. doi: 10.1016/j.rmed.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 37.Chapman KR, Patel P, D’Urzo AD, et al. Maintenance of asthma control by once-daily ciclesonide in adults with persistent asthma. Allergy. 2005;60:330–337. doi: 10.1111/j.1398-9995.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- 38.Gelfand EW, Georgitis JW, Noonan M, Ruff ME. Once-daily ciclesonide in children: efficacy and safety in asthma. J Pediatr. 2006;148:377–383. doi: 10.1016/j.jpeds.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 39.Postma DS, Sevette C, Martinat Y, Schlösser N, Aumann J, Kafé H. Treatment of asthma by the inhaled corticosteroid ciclesonide given either in the morning or evening. Eur Respir J. 2001;17:1083–1088. doi: 10.1183/09031936.01.00099701. [DOI] [PubMed] [Google Scholar]
- 40.Knox A, Langan J, Martinot JB, Gruss C, Häfner D. Comparison of a step-down dose of once-daily ciclesonide with a continued dose of twice-daily fluticasone propionate in maintaining control of asthma. Curr Med Res Opin. 2007;23(10):2387–2394. doi: 10.1185/030079907X226203. [DOI] [PubMed] [Google Scholar]
- 41.Lee DK, Haggart K, Currie GP, Bates CE, Lipworth BJ. Effects of hydroflouroalkane formulations of ciclesonide 400 μg once daily vs fluticasone 250 μg twice daily on methacholine hyper-responsiveness in mild-to-moderate persistent asthma. Br J Clin Pharm. 2004;58(1):26–33. doi: 10.1111/j.1365-2125.2004.02108.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buhl R, Vinkler I, Magyar P, et al. Comparable efficacy of ciclesonide once daily versus fluticasone propionate twice daily in asthma. Pulm Pharmacol Ther. 2006;19(6):404–412. doi: 10.1016/j.pupt.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 43.Ukena D, Biberger C, Steinijans V, et al. Ciclesonide is more effective than budesonide in the treatment of persistent asthma. Pulm Pharmacol Ther. 2007;20(5):562–570. doi: 10.1016/j.pupt.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 44.Niphadkar P, Jagannath K, Joshi JM, et al. Comparison of the efficacy of ciclesonide 160 μg QD and budesonide 200 μg BID in adults with persistent asthma: A phase III, randomized, double-dummy, open-label study. Clin Ther. 2005;27(11):1752–1763. doi: 10.1016/j.clinthera.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 45.Boulet LP, Drollman A, Magyar P, et al. Comparative efficacy of once-daily ciclesonide and budesonide in the treatment of persistent asthma. Respir Med. 2006;100:785–794. doi: 10.1016/j.rmed.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 46.Hansel TT, Benezet O, Kafé H, et al. A multinational, 12-week, randomized study comparing the efficacy and tolerability of ciclesonide and budesonide in patients with asthma. Clin Ther. 2006;28(6):906–920. doi: 10.1016/j.clinthera.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 47.von Berg A, Engelstätter R, Minic P, et al. Comparison of the efficacy and safety of ciclesonide 160 μg once daily vs budesonide 400 μg once daily in children with asthma. Pediatr Allergy Immunol. 2007;18:391–400. doi: 10.1111/j.1399-3038.2007.00538.x. [DOI] [PubMed] [Google Scholar]
- 48.Vermeulen JH, Gyurkovits K, Rauer H, Engelstätter R. Randomized comparison of the efficacy and safety of ciclesonide and budesonide in adolescents with severe asthma. Respir Med. 2007;101(10):2182–2191. doi: 10.1016/j.rmed.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 49.Boulet LP, Bateman ED, Voves R, Müller T, Wolf S, Engelstätter R. A randomized study comparing ciclesonide and fluticasone propionate in patients with moderate persistent asthma. Respir Med. 2007;101(8):1677–1686. doi: 10.1016/j.rmed.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 50.Bateman ED, Linnhof AE, Homik L, Freudensprung U, Smau L, Engelstätter R. Comparison of twice-daily inhaled ciclesonide and fluticasone propionate in patients with moderate-to-severe persistent asthma. Pulm Pharmacol Ther. 2008;21(2):264–275. doi: 10.1016/j.pupt.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 51.Pedersen S, Garcia Garcia ML, Manjra AI, Theron I, Engelstätter R. A comparative study of inhaled ciclesonide 160 μg/day and fluticasone propionate 176 μg/day in children with asthma. Pediatr Pulmonol. 2006;41(10):954–961. doi: 10.1002/ppul.20474. [DOI] [PubMed] [Google Scholar]
- 52.Richter K, Kanniess F, Biberger C, Nave R, Magnussen H. Comparison of the oropharyngeal deposition of inhaled ciclesonide and fluticasone propionate in patients with asthma. J Clin Pharmacol. 2005;45:146–152. doi: 10.1177/0091270004271094. [DOI] [PubMed] [Google Scholar]
- 53.Nave R, Zech K, Bethke TD. Lower oropharyngeal deposition of inhaled ciclesonide via hydroflouroalkane metered-dose inhaler compared with budesonide via chlorofluorocarbon metered-dose inhaler in healthy subjects. Eur J Clin Pharmacol. 2005;61:203–208. doi: 10.1007/s00228-005-0910-0. [DOI] [PubMed] [Google Scholar]
- 54.Pearlman DS, Berger WE, Kerwin E, LaForce C, Kundu S, Banerji D. Once-daily ciclesonide improves lung function and is well tolerated by patients with mild-to-moderate persistent asthma. J Allergy Clin Immunol. 2005;116:1206–1212. doi: 10.1016/j.jaci.2005.08.037. [DOI] [PubMed] [Google Scholar]
- 55.Agertoft L, Pedersen S. Short-term lower-leg growth rate and urine cortisol excretion in children treated with ciclesonide. J Allergy Clin Immunol. 2005;115:940–945. doi: 10.1016/j.jaci.2005.01.066. [DOI] [PubMed] [Google Scholar]
- 56.Szefler S, Rohatagi S, Williams J, Lloyd M, Kundu S, Banerji D. Ciclesonide, a novel inhaled steroid, does not affect hypthalamic-pituitary-adrenal axis function in patients with moderate-to-severe persistent asthma. Chest. 2005;128:1104–1114. doi: 10.1378/chest.128.3.1104. [DOI] [PubMed] [Google Scholar]
- 57.Lipworth BJ, Kaliner MA, LaForce CF, Baker JW, Kaiser HB, Amin D, et al. Effect of ciclesonide and fluticasone on hypothalamic-pituitary-adrenal axis function in adults with mild-to-moderate persistent asthma. Ann Allergy Asthma Immunol. 2005;94:465–472. doi: 10.1016/S1081-1206(10)61117-9. [DOI] [PubMed] [Google Scholar]
- 58.Derom E, Van De Velde V, Marissens S, Engelstätter R, Vincken W, Pauwels R. Effects of inhaled ciclesonide and fluticasone propionate on cortisol secretion and airway responsiveness to adenosine 5’monophosphate in asthmatic patients. Pulm Pharmacol Ther. 2005;18(5):328–336. doi: 10.1016/j.pupt.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 59.Skoner DP, Maspero J, Banerji D, the Ciclesonide Pediatric Growth Study Group Assessment of the long-term safety of inhaled ciclesonide on growth in children with asthma. Pediatrics. 2008;121(1):e1–14. doi: 10.1542/peds.2006-2206. [DOI] [PubMed] [Google Scholar]
- 60.Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med. 2000;343(15):1064–1069. doi: 10.1056/NEJM200010123431502. [DOI] [PubMed] [Google Scholar]
- 61.Rohatagi S, Luo Y, Shen L, Guo Z, Schemm C, Huang Y, et al. Protein binding and its potential for eliciting minimal systemic side effects with a novel inhaled corticosteroid, ciclesonide. Am J Ther. 2005;12(3):201–209. [PubMed] [Google Scholar]
- 62.Nave R, Meyer W, Fuhst R, Zech K. Formation of fatty acid conjugates of ciclesonide active metabolite in the rat lung after 4-week inhalation of ciclesonide. Pulm Pharmacol Ther. 2005;18:390–396. doi: 10.1016/j.pupt.2005.02.012. [DOI] [PubMed] [Google Scholar]