Abstract
Background: The relationship of exercise to weight loss, beyond minimal caloric expenditures possible in obese and deconditioned individuals, requires clarification.
Objective: We assessed whether changes in theory-based psychological variables associated with participation in an exercise treatment extended to psychologically based predictors of controlled eating and weight and waist-circumference reductions.
Methods: A group of 137 adults with severe obesity (mean body mass index, 42.2 kg/m2) volunteered for an exercise-support and nutrition-education treatment of 26 weeks' duration that was based on social cognitive theory. Exercise- and eating-related measures of mood, self-regulation, and self-efficacy were obtained at baseline and at treatment end, along with weight, waist circumference, and exercise volume. Analyses were also conducted separately for women participants only (n = 102).
Results: Treatment-induced changes in total mood disturbance, self-regulatory skill usage for exercise, and exercise self-efficacy were significantly related to changes in self-efficacy to control emotional eating, self-regulatory skill usage for controlled eating, and overall self-efficacy for controlled eating, respectively (p < 0.001). Changes in the eating-related measures significantly predicted changes in weight and waist circumference with adjusted R2 values from 0.15 to 0.21 and 0.28 to 0.30, respectively (p < 0.001). Post-hoc testing indicated a strong negative correlation between exercise completed and weight change (r = −0.62); however, only 12.4% of the observed weight change was accounted for through associated caloric expenditures.
Conclusion: Exercise may support weight loss primarily through psychological rather than physiological pathways. Although the models tested were viable, additional modifiable variables may further strengthen the prediction of weight and waist-circumference change and benefit weight-loss theory and treatment outcomes.
Introduction
Exercise is a strong predictor of weight loss and maintenance of weight loss.1 However, obese and deconditioned individuals are rarely able to complete enough physical exertion to induce meaningful weight loss through associated caloric expenditures.2 It has been suggested that improvements in psychological factors associated with participation in an exercise program may extend to improvements in psychological factors associated with controlled eating and subsequent weight loss.3 For example, exercise-induced improvements in mood4 may transfer to tempered emotional eating; self-regulatory skills developed to adhere to an exercise program may transfer to self-regulation for controlled eating5; and self-efficacy for maintaining exercise may transfer to a more generalized self-efficacy for weight management and, thus, controlled eating.3 A model proposed by Baker and Brownell,3 recently adapted and tested,6,7 suggests viability of these possibilities.
An understanding of the pathways by which exercise behaviors may affect weight loss beyond caloric expenditures is needed to shape both theoretical and treatment research. Thus, relations of changes in mood, self-efficacy, and self-regulation associated with an exercise program to changes in mood, self-efficacy, and self-regulation associated with controlled eating and weight loss were tested with severely obese adults.
Methods
Study Participants
Men and women responded to local newspaper solicitations for participation in research on weight loss. Requirements were being at least age 21 years, having a body mass index (BMI) of 35 kg/m2 to 50 kg/m2, and participating in no regular exercise (< 20 minutes per week) in the previous year. Pregnancy and the use of medication for weight loss or a psychological or psychiatric condition were reasons for exclusion. We obtained a written statement of adequate physical health to participate from a physician, approval from an institutional review board, and written consent from all study participants (N = 137; mean age = 43.6 years [Standard Deviation (SD} = 9.9]; mean BMI = 42.2 kg/m2 [SD = 6.6]; racial makeup: 53% white, 45% black, and 2% other races/ethnicities; socioeconomic level: mostly lower-middle to middle class).
Measures
Total mood disturbance (TMD) is an aggregate measure of mood derived from the six subscales of the Profile of Mood States Short Form.8 Respondents rate feelings during the preceding week for 30 items (5 items for each of its subscales: tension, depression, fatigue, confusion, anger, vigor) on a scale ranging from 0 (not at all) to 4 (extremely). The internal consistency ranged from 0.84 to 0.95, and test-retest reliability at 3 weeks averaged 0.69.8
Measurement of self-regulation skills usage for both exercise (SR-Ex) and appropriate eating (SR-Eat) was adapted from a validated scale that was based on treatment content.9 Responses to the 10 items for each scale ranged from 1 (never) to 5 (often). Internal consistencies were 0.79 and 0.81, and test-retest reliabilities during a span of 2 weeks were 0.78 and 0.74, respectively.
The Exercise Self-Efficacy Scale10 (ExSE) measured perceived ability to overcome barriers to exercise. Responses range from 1 (not at all confident) to 7 (very confident). Internal consistencies ranged from 0.76 to 0.82, and test-retest reliability during a span of 2 weeks was 0.90.11
The Weight Efficacy Lifestyle Questionnaire12 measured self-efficacy for controlled eating. It is made up of 5 subscales (4 items for each of its subscales: negative emotions, availability, social pressure, physical discomfort, positive activities). Item responses range from 0 (not confident) to 9 (very confident). For this research, both the total score (WEL-Tot) and the negative emotions subscale (WEL-NegEm) were used. Internal consistencies ranged from 0.70 to 0.90 and 0.87 to 0.88, respectively.12
The Godin Leisure-Time Exercise Questionnaire13 measured exercise through study participants' entry of weekly frequencies of strenuous, moderate, and light exercise for more than 15 minutes per session. Responses are multiplied by 9, 5, and 3 standard metabolic equivalents (METs), respectively, and then summed. For adults, test-retest reliability during a span of 2 weeks was 0.74.13 Construct validity was indicated by significant correlations with accelerometer and maximum oxygen consumption measurements.14,15
A recently calibrated digital scale was used to measure weight (kg). A tape measure was used to measure waist circumference at the umbilicus. Change scores were the difference from baseline to week 26.
Procedure
Participants were provided access to YMCA wellness centers and were enrolled in a treatment program that was based on tenets of social cognitive theory. The exercise support portion of the treatment consisted of 6 one-on-one meetings of 45 to 60 minutes each, during a span of 26 weeks.6 Instruction in an array of self-regulatory methods (eg, long- and short-term goal setting, cognitive restructuring, relapse prevention) was a primary focus. Exercise plans were based on each participant's tolerance; however, the volume suggested for health promotion (150 minutes per week)16 was described, and it was suggested that any volume of exercise may have benefit.
The nutrition portion of the treatment consisted of six 1-hour group sessions over the initial 14 weeks.17 Components included 1) using the US Food Guide Pyramid, 2) developing a plan for snacking, and 3) using self-regulatory skills for controlled eating. Overall, attendance in treatment sessions was 72%.
Data Analyses
First, score changes in TMD, SR-Ex, ExSE, WEL-NegEm, SR-Eat, WEL-Tot, weight, waist circumference, and recalled exercise per week during the 26-week treatment were calculated. As in previous research,18,19 changes throughout treatment, rather than scores at a particular temporal point, were used to account for the dynamic nature of weight-loss treatment processes. Both actual score changes and changes controlling for baseline scores were used for analyses.
Next, linear bivariate relationships between changes in the following exercise-related and eating-related variables were calculated: 1) TMD and WEL-NegEm, 2) SR-Ex and SR-Eat, and 3) ExSE and WEL-Tot. Finally, the variance in changes in weight and waist circumference accounted for by changes in the three eating-related variables was derived using multiple regression analysis with simultaneous entry of the predictors.
Because treatments that include exercise (and hence may increase muscle density) may temper reduction in weight,20 changes in both weight and waist circumference were incorporated as outcome measures. Because WEL-NegEm was a subscale of WEL-Tot and thus had some redundancy in item responses, multiple regression analyses were also completed using only changes in WEL-Tot and SR-Eat as predictors.
For a multiple regression equation with three predictors, to detect an effect size of f 2 = 0.15 at the statistical power of 0.90, a minimum of 98 study subjects was required. Because emotional eating may affect women differently than men,21 analyses were conducted with the entire sample (N = 137) and then with women only (n = 102). An intention-to-treat design was used with multiple imputation.22 Significance levels were set at α = 0.05 (two-tailed), with the Bonferroni adjustment applied where appropriate.
Results
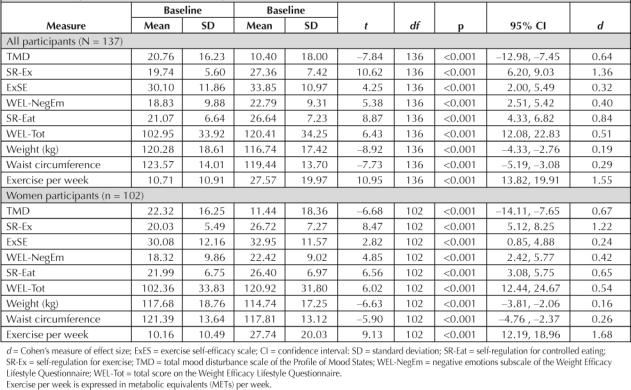
For both the entire sample and women-only subsample, independent t-tests indicated statistically significant improvements over a span of 26 weeks in all study variables (Table 1). In all subsequent analyses, results were similar whether actual change scores or changes controlling for baseline values were incorporated. Thus, only results from actual score changes are reported. For both the entire sample and women-only subsample, significant bivariate relationships were found between changes in
Table 1.
Changes in study variables during a span of 26 weeks
TMD and WEL-NegEm (β = −0.30, SE = 0.05, p < 0.001, and β = −0.31, SE = 0.05, p = 0.002, respectively)
SR-Ex and SR-Eat (β = 0.65, SE = 0.06, p < 0.001, and β = 0.61, SE = 0.07, p < 0.001, respectively)
ExSE and WEL-Tot (β = 0.51, SE = 0.23, p < 0.001, and β = 0.53, SE = 0.26, p < 0.001, respectively).
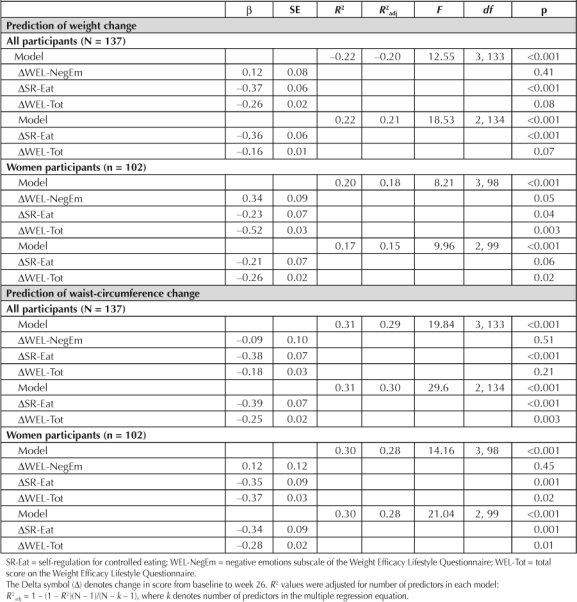
For both the entire sample and the women-only subsample, changes in WEL-NegEm, SR-Eat, and WEL-Tot accounted for a significant portion of the variance in weight and waist-circumference changes (Table 2). In each of the four multiple regression equations having three predictors, changes in SR-Eat explained a significant unique portion of the variance. In the women-only subsample, change in WEL-Tot was also a significant unique predictor. For both the entire sample and the women-only subsample, changes in SR-Eat and WEL-Tot accounted for a significant portion of the variance in waist-circumference changes in each of the multiple regression equations having two predictors (Table 2). In the two-predictor equations, both predictors explained at least a marginally significant (p < 0.07) unique portion of the variance.
Table 2.
Results of multiple regression analyses for prediction of changes in weight and waist circumference
Post-Hoc Test
When change in exercise volume per week for both the entire sample and the women-only subsample was converted to caloric expenditure on the basis of previous research,18,23 only 12.4% and 13.1%, respectively, of weight change was explained, although the correlations between changes in exercise and weight were strong (r values = −0.62 and −0.55, respectively; p < 0.001).
Discussion
Carryover from improvements in mood, self-regulation, and self-efficacy, (associated with an exercise treatment using cognitive-behavioral methods) to improvements in corresponding variables associated with controlled eating was previously suggested,3,19 but empirical verification was largely missing. The present findings suggested that exercise's association with weight loss was better explained through such psychological, rather than physiological (ie, caloric expenditure), pathways. This has considerable implications for weight-loss theory development and clinical applications, suggesting that attention should be given to the mood-enhancing properties and to improvements in self-regulation and self-efficacy that are possible through behaviorally based exercise treatments.
Replications should incorporate more controlled settings, direct measurement of eating behaviors and caloric consumption, and, possibly, inclusion of additional variables to extend the present prediction models. Continued testing within field settings with a variety of sample types (eg, persons who have undergone bariatric surgery, morbidly obese persons), however, may have more immediate benefits for practical application of findings.24 The directionality of the identified relationships also requires further investigation. Hopefully, behavioral interventions directed at eating behaviors can be paired with appropriately supported exercise to reliably improve lagging weight-loss treatment outcomes25 over the long term.
… exercise's association with weight loss was better explained through psychological, rather than physiological (ie, caloric expenditure), pathways.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Acknowledgments
The research reported herein was supported by a grant from Blue Cross Blue Shield of Georgia.
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
References
- Miller WC, Koceja DM, Hamilton EJ. A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Int J Obes Relat Metab Disord. 1997 Oct;21(10):941–7. doi: 10.1038/sj.ijo.0800499. [DOI] [PubMed] [Google Scholar]
- Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, American College of Sports Medicine American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009 Feb;41(2):459–71. doi: 10.1249/MSS.0b013e3181949333. Erratum in: Med Sci Sports Exerc 2009 Jul;41(7):1532. [DOI] [PubMed] [Google Scholar]
- Baker CW, Brownell KD. Physical activity and maintenance of weight loss: physiological and psychological mechanisms. In: Bouchard C, editor. Physical activity and obesity. Champaign, IL: Human Kinetics; 2000. pp. 311–28. editor. p. [Google Scholar]
- Landers DM, Arent SM. Physical activity and mental health. In: Tennenbaum G, Eklund RC, editors. Handbook of sport psychology. 3rd ed. New York, NY: Wiley; 2007. pp. 469–91. p. [Google Scholar]
- Hagger MS, Wood C, Stiff C, Chatzisarantis NL. Ego depletion and the strength model of self-control: a meta-analysis. Psychol Bull. 2010 Jul;136(4):495–525. doi: 10.1037/a0019486. [DOI] [PubMed] [Google Scholar]
- Annesi JJ, Unruh JL. Relations of exercise, self-appraisal, mood changes and weight loss in obese women: testing propositions based on Baker and Brownell's (2000) model. Am J Med Sci. 2008 Mar;335(3):198–204. doi: 10.1097/MAJ.0b013e318152010c. [DOI] [PubMed] [Google Scholar]
- Mata J, Silva MN, Vieira PN, et al. Motivational “spill-over” during weight control: increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol. 2009 Nov;28(6):709–16. doi: 10.1037/a0016764. [DOI] [PubMed] [Google Scholar]
- McNair DM, Heuchert JWP. Profile of Mood States (POMS), technical update. North Tonawanda, NY: Multi-Health Systems; 2009. [Google Scholar]
- Saelens BE, Gehrman CA, Sallis JF, Calfas KJ, Sarkin JA, Caparosa S. Use of self-management strategies in a 2-year cognitive-behavioral intervention to promote physical activity. Behav Ther. 2000;31(2):365–79. [Google Scholar]
- Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992 Mar;63(1):60–6. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- McAuley E, Mihalko SL. Measuring exercise-related self-efficacy. In: Duda JL, editor. Advances in sport and exercise psychology measurement. Morgantown, WV: Fitness Information Technology; 1998. pp. 371–90. editor. p. [Google Scholar]
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991 Oct;59(5):739–44. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985 Sep;10(3):141–6. [PubMed] [Google Scholar]
- Jacobs DR, Jr, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993 Jan;25(1):81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]
- Miller DJ, Freedson PS, Kline GM. Comparison of activity levels using Caltrac accelerometer and five questionnaires. Med Sci Sports Exerc. 1994 Mar;26(3):376–82. [PubMed] [Google Scholar]
- Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007 Aug;39(8):1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- Kaiser Permanente Health Education Services. Cultivating health weight management kit. 8th ed. Portland, OR: Kaiser Permanente; 2008. [Google Scholar]
- Annesi JJ, Gorjala S. Changes in theory-based psychological factors predict weight loss in women with class III obesity initiating supported exercise. J Obes. 2010;2010:171957. doi: 10.1155/2010/171957. Epub 2010 Jun 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakicic JM, Wing RR, Winters-Hart C. Relationship of physical activity to eating behaviors and weight loss in women. Med Sci Sports Exerc. 2002 Oct;34(10):1653–9. doi: 10.1097/00005768-200210000-00018. [DOI] [PubMed] [Google Scholar]
- Després J, Lamarche B. Physical activity and the metabolic complications of obesity. In: Bouchard C, editor. Physical activity and obesity. Champaign, IL: Human Kinetics; 2000. pp. 331–54. editor. p. [Google Scholar]
- Tanofsky MB, Wilfley DE, Spurrell EB, Welch R, Brownell KD. Comparison of men and women with binge eating disorder. Int J Eat Disord. 1997 Jan;21(1):49–54. doi: 10.1002/(sici)1098-108x(199701)21:1<49::aid-eat6>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York, NY: Guilford; 2005. [Google Scholar]
- Hall KD. What is the required energy deficit per unit weight loss? Int J Obes (Lond) 2008 Mar;32(3):573–6. doi: 10.1038/sj.ijo.0803720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–33. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J. Medicare's search for effective obesity treatments: diets are not the answer. Am Psychol. 2007 Apr;62(3):220–33. doi: 10.1037/0003-066X.62.3.220. [DOI] [PubMed] [Google Scholar]


