Abstract
Introduction: Before the implementation of a multidisciplinary disease-state-management program in the Kaiser Permanente Ohio Region, the primary care physician (PCP) worked with a registered nurse care manager (RNCM) and a clinical pharmacist with the degree of PharmD to control diabetes mellitus (DM). This occurred through PCP referral when patients required a higher level of care than could be achieved during initial PCP office visits and subsequent follow-up visits. However, not all PCPs consistently initiated referrals, and as patients in need of referral were typically identified through office visits, those without routine appointments were often missed. This practice translated into suboptimal 2008 comprehensive DM care Healthcare Effectiveness Data and Information Set (HEDIS) scores.
Methods: A quality-improvement disease-management committee convened for design and implementation of a multidisciplinary DM disease-state-management program, as well as oversight and analysis of the new process. This regional intervention required many members of the health care team to obtain additional education about comprehensive DM care, adopt new work flows, and learn to use tools for evaluating patient care gaps.
Results: Within one year, this regional multidisciplinary intervention resulted in improvements in blood pressure, lipid levels, and glycemic control as indicated by 2009 comprehensive DM-care HEDIS scores.
Discussion: Main contributors to the success of the program included executive support and sponsorship, the leadership of the oversight committee, systematic identification and assignment of patients, the blood-pressure service run by licensed practical nurses, continuous education efforts, dedicated panel-management time, use of a multidisciplinary team, and expanding treatment of the diabetic patient beyond glucose control to include blood pressure and lipid management.
Introduction
Background
The Kaiser Permanente Ohio Region (KPOH) comprises approximately 135,000 members who receive care at 10 medical centers located throughout Northeast Ohio. Typically, each medical center contains an internal medicine team that consists of primary care physicians (PCPs), nurse practitioners (NPs), registered nurse care managers (RNCMs), licensed practical nurses (LPNs), clinical pharmacists with the degree of PharmD, physician assistants, and registered dietitians. In addition, a centralized population care management (PCM) team that consists of RNCMs, LPNs, and analytic staff provides support to each of the 10 medical offices. Although each group has a different role, together they partner to support all aspects of patient care.
As high-quality care of diabetes mellitus (DM) has evolved to include more than just glycemic management, a DM disease-state-management program was initiated at KPOH in an effort to improve patient care and outcomes for those with DM. Primary literature as well as national Care Management Institute guidelines were consulted to construct a program that would reflect current evidence-based medicine.1–7
Problem
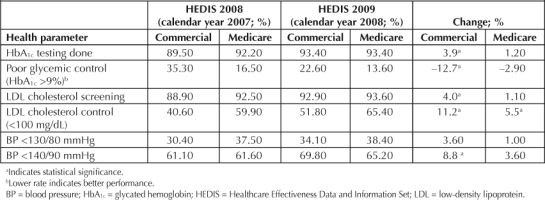
Before the implementation of a multidisciplinary disease-state-management program in KPOH, the PCP worked with an RNCM and a clinical pharmacist with the degree of PharmD to control DM. This occurred through PCP referral when patients required a higher level of care than PCP time allowed during initial office visits and subsequent follow-up visits. Examples of patients who typically received referrals included those with treatment-plan care gaps, multiple comorbid conditions, or previous nonadherence to medication regimens. However, not all PCPs consistently ordered referrals, and as patients in need of referral were typically identified through office visits, those without routine PCP appointments were often missed. This approach translated into suboptimal 2008 comprehensive DM care HEDIS scores,8 as seen in Table 1.
Table 1.
Comprehensive diabetes care 2008 HEDIS results
Intended Improvement
After release and discussion of the 2008 Healthcare Effectiveness Data and Information Set (HEDIS) results (for calendar year 2007), the Medical Group set a goal to improve the 2009 comprehensive DM-care HEDIS scores to at least the 75th percentile with the intention to improve overall patient health. The executive leadership identified an existing quality-improvement team, the Advanced Care Management (ACM) committee, to develop a plan to achieve this goal.
Methods
Planning the Intervention
The ACM committee consisted of nursing, pharmacy, and physician leaders, as well as information technology staff. They met for four hours each week to design, implement, and review current DM care at KPOH, with a mission to develop a strategy for diabetes care that used and reallocated existing resources. A review of current staff activities was conducted. It was determined that several work-flow changes had to take place to create an effective disease-management program with the currently available resources. These changes affected the PCPs, RNCMs, LPNs, PCM team, and clinical pharmacists. Before the restructuring, RNCMs worked on disease management for only a small percentage of their day, largely focusing on in-office procedures such as injections and blood-pressure checks. Clinical pharmacists' involvement in disease management occurred through referrals typically centered only on cholesterol management. The PCM team's primary function was to perform member outreach to patients in need of preventive care such as mammography, colorectal cancer screening, or laboratory updates without participation in disease management.
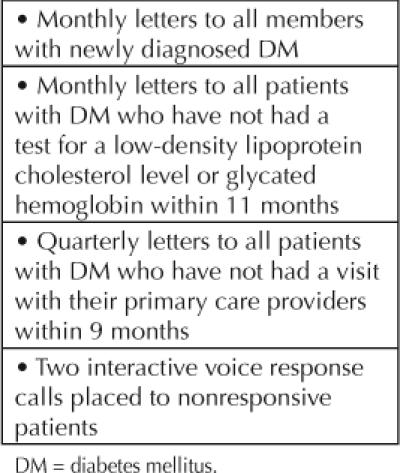
To accommodate patient telephone and office visits for disease management, RNCMs shifted several in-office duties to the LPNs. One important change was initiation of an LPN-run blood-pressure clinic; blood-pressure checks were previously done by the RNCMs. Clinic LPNs booked blood-pressure-check appointments at 15-minute intervals. Protocols were developed for management of out-of-range blood pressure, including immediate or electronic consultation with the patient's PCP or an NP, depending on the degree of elevation of the recorded blood pressure. The clinical pharmacists' referral capacity was expanded by minimizing nonclini-cal functions. Through restructuring, three RNs on the PCM team transferred to a central location to participate only in telephonic DM-related disease-care management. Additionally, outreach by the team was increased and standardized, as seen in Table 2.
Table 2.
Population care management—Diabetes mellitus-care outreach schedule
Patient Identification and Assignment
The first task was to identify members with DM-related care gaps using a database tool called the Permanente Online Interactive Network Tools (POINT), a suite of applications with the capability to filter and sort all patients in KPOH by outcome data. Initial inclusion criteria were patients between the ages 18 and 80 years with a diagnosis of DM, which yielded approximately 12,000 people. Members were then placed into groups according to their PCP facility location and were further subcategorized by glycated hemoglobin (HbA1c) value and blood pressure, as seen in Table 3. The ACM committee generated new patient lists through POINT monthly and distributed them to the care managers.
Table 3.
Workload distribution
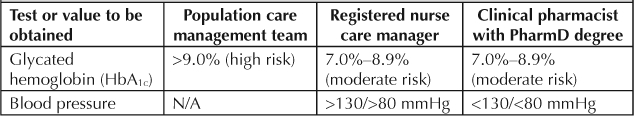
The high-risk patient group (HbA1c >9%) was the smallest group and was therefore assigned to the three PCM RNs who were dedicated exclusively to DM management. The moderate-risk group (HbA1c = 7.0%–8.9%), was divided between the RNCMs and the clinical pharmacists on the basis of specific blood-pressure criteria. Patients with a controlled blood pressure (<130/<80mmHg) were assigned to the clinical pharmacists. Patients with an uncontrolled blood pressure were assigned to the RNCMs, who could more easily schedule patients for follow-up blood-pressure checks after medication adjustments. Patients with an HbA1c of <7.0% were considered low risk and were not included in the initial management strategy.
Intervention Work Flow
The care manager work flow initially consisted of a chart review followed by a patient interview. Patient interviews were conducted primarily as telephone visits and were supplemented with office visits when clinically necessary. After an interview was completed, a care plan was developed. The care plan included an assessment of blood-sugar control (as represented by HbA1c values and patient-reported, self-monitored blood-glucose values), blood-pressure control, lipid control (as represented by low-density lipid [LDL] cholesterol), immunizations (with a focus on pneumococcal vaccinations), diet, exercise, and medication-regimen adherence. In addition, an emphasis was placed on starting all patients with DM on the ALL regimen, consisting of an aspirin, a lipid-lowering agent, and lisinopril (any angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker was acceptable), as clinically appropriate. Care plans were sent to the patient's PCP for review, modification (if needed), and approval. After approval by the PCP, plans were communicated to the patient through the care managers during subsequent telephone or of-fice visits. Follow-up care was given as needed, until patients attained therapeutic goals regarding HbA1c values, LDL cholesterol levels, and blood pressure.
To assist with documentation of care plans and order entry and to increase efficiency, SmartSets were created within the electronic medical record. Figure 1 is an example of a small portion of a comprehensive DM care SmartSet.
Figure 1.
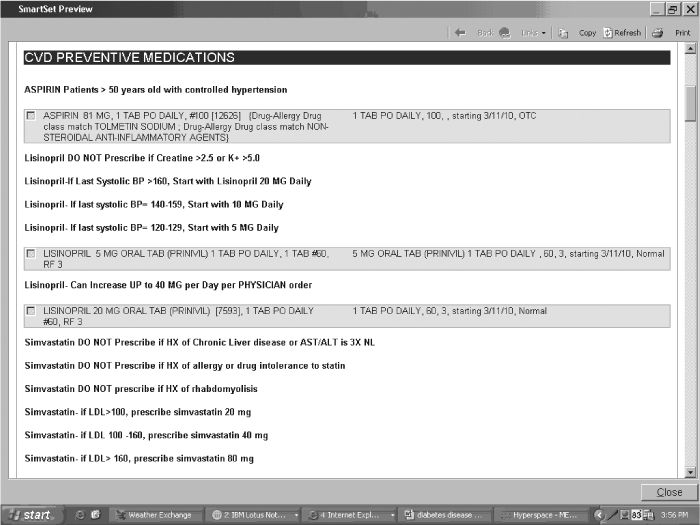
Example of a comprehensive diabetes care SmartSet.
Intervention Assessment
Several tools were used to assess the intervention. On a regional level, a PCP dashboard tool produced a monthly summary of the PCP's patient panel and allowed comparison with the panels of their peers. Dashboard calculations were based only on the individual physician's panel of patients with DM. Measures related to DM performance included yearly HbA1c screening, HbA1c >9%, HbA1c <7.5%, yearly LDL cholesterol screening, LDL cholesterol <100 mg/dL, blood pressure <130/80 mmHg, blood pressure <140/90 mmHg, and presence of ALL meds. On a national level, HEDIS measures related to DM were reviewed yearly.
The largest improvement was seen in the “poor control >9%” patient population. This can be attributed to an increase in screening frequency, as well as increased glycemic control.
Training and Time
Extensive education of the health care team regarding patient assignments and standards of care for DM disease-state management occurred through both departmental and interdisciplinary team meetings. This included formal reviews of current American Diabetes Association guidelines,1 preferred medication use and titration schedules, patient-counseling techniques, and lifestyle-intervention coaching. Patients were also educated through diabetes group classes led by either a member of PCM or a RNCM and a registered dietitian. Classes addressed diet and lifestyle changes, medication management, and disease-state progression.
For the first few months, clinical pharmacists mentored RNCMs through the process of developing and implementing a comprehensive DM-care plan. Panel-management time was created by blocking off two 20-minute patient-appointment slots each day. During this time, physicians met face-to-face or telephonically with RNCMs, the PCM team, and clinical pharmacists to review, discuss, modify, and approve the increased volume of care plans. When smaller facilities contacted and completed interventions for all patients on their assigned lists, they partnered with larger facilities with larger DM patient panels to complete those lists. Because dashboard assessments allowed real-time feedback from individual physicians, the ACM committee could evaluate which physicians needed additional resources dedicated to their patient panel. Patients who could not be contacted after three phone attempts and one letter mailing were placed in a holding pattern for six months, and then another attempt at contact was made. The ACM committee addressed all barriers in their review of dashboards and work flows and analyzed outcome trends to ensure progress.
Results
As implementation of the intervention progressed, health parameters for dashboard panels began to improve; the release of the 2009 HEDIS results confirmed the progress seen internally. Table 1 compares 2008 with 2009 HEDIS data. The largest improvement was seen in the “poor control >9%” patient population. This can be attributed to an increase in screening frequency, as well as increased glycemic control. Improvement in control of blood pressure and lipid levels were also seen, serving as a testament to the KPOH strategy of treating the DM patient with a multidisciplinary approach.
In addition to improved HEDIS scores, decreases in several DM-related clinical hospital-admission parameters were seen, as shown in Figures 2 and 3. Short-term complications were defined as hospital admission rates for patients with a diagnosis of diabetic ketoacidosis, diabetic coma, or diabetic hyper-osmolar state. Long-term complications, also based on hospital admission rates, were defined as renal, eye, neurologic, or circulatory complications. All definitions were based on specific codes from International Classification of Diseases, 9th Revision.
Figure 2.
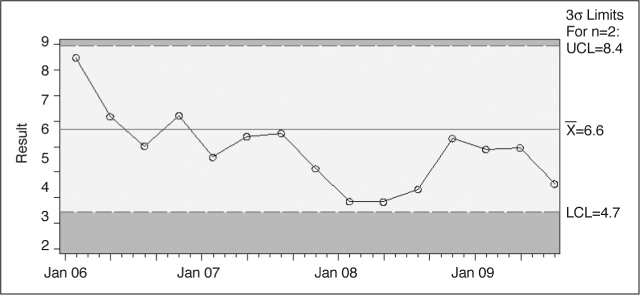
Long-term complications of diabetes mellitus (DM) per 1000 members per year with DM in the Kaiser Permanente Ohio Region.
Figure 3.
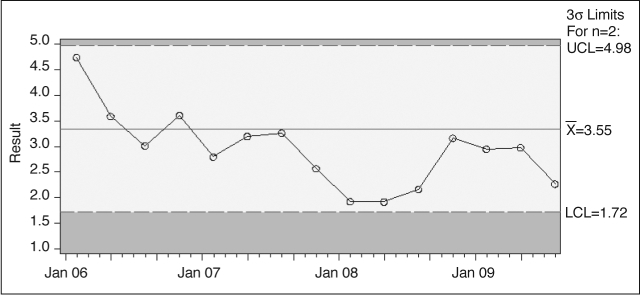
Short-term complications of diabetes mellitus (DM) per 1000 members per year with DM in the Kaiser Permanente Ohio Region.
Discussion
Main contributors to the success of the program included executive support and sponsorship, the leadership and composition of the ACM committee, systematic identi-fication and assignment of patients, the LPN-run blood-pressure clinic, continuous education efforts, dedicated panel-management time, use of a multidisciplinary team, and expansion of treatment of patients with DM beyond glucose control to include blood-pressure and lipid-level management.
Patient panel assignments to care managers helped create accountability for the total patient population and their care gaps. However, no system was in place to generate care-manager-specific outcome and productivity data reports. In addition, as seen in Table 3, although patient workload distribution was clearly structured, problems arose when PCP referrals deviated from the established work flow. These deviations occurred when PCPs were learning the new work flow or were more comfortable with their prior in-office referral processes.
The LPN-run blood-pressure clinic increased access to screening without a copay. Increased blood-pressure measurement opportunities enabled a more rapid medication-titration process. Also, the adoption of a strictly LPN-run clinic freed time in the RNCM schedule to engage in disease management.
Because many shifts in roles had occurred and a new process was being implemented, a strong emphasis was placed on education of the entire disease-state-management team. These efforts were repeated in multiple forums and venues. Algorithms, national guidelines, and standards of care were distributed and reviewed at physician, pharmacist, and RNCM team meetings on an ongoing basis. These concepts were again reviewed at interdisciplinary team meetings. Patients were also educated through group diabetes classes led by either a member of the PCM team or an RNCM and registered dietitian. Classes addressed diet and lifestyle changes, medication management, and disease-state progression.
Panel-management time assisted in gaining physician buy-in and reduced the burden of increased DM-related in-basket messages. Although over time, it was found that panel-management time was not always strictly used for DM disease-state management, it did consistently allow physicians to feel more comfortable with integrating more disease management into their daily work flow.
One of the components most important to the improvement in HEDIS measures and patient care came from the strategy of treating all parameters of the patient with DM. Before the initiation of this program, less emphasis was placed on the control of blood pressure and lipid levels in patients with DM; care centered on lowering blood-glucose levels. With the use of the ALL mnemonic, emphasis shifted from a glucose-centered approach to one that started and titrated all applicable medications to reach comprehensive diabetic goals. However, as a consequence of the focused effort on diabetes care in 2008, less focus was placed on several other chronic diseases. Thus, not all 2009 HEDIS measures showed as large of an improvement as the DM related measures.
Despite the improvement seen in diabetes care, several limitations to this analysis exist. First, no demographic data for the cohort were available for collection. Therefore, it is unclear what role changing demographics might have had on the reported results. KPOH is currently implementing a process for demographic data collection. Second, the goal of this article was to describe the efforts and results of a multidis-ciplinary disease-state-management team, not to analyze cost savings or financial implications of such an intervention. Although we do believe that a strong DM-management program does decrease long-term health care costs, this hypothesis cannot be validated by the current analysis. It is possible that because of increased screening, medication dispensing, and DM-related office visits, short-term costs may have increased in the KPOH region, but those data were not analyzed.
Because of the success of this program, DM disease management has been integrated into daily work flows. In addition, the multidisci-plinary approach to disease-state management has expanded to include hypertension, coronary artery disease, chronic obstructive pulmonary disease, and asthma. Increased teamwork has led to improved communication between departments and a greater understanding of each discipline's strengths.
The opportunity to provide more effective diabetes care has fostered a personal connection and sense of increased job satisfaction, although no employee surveys were administered to validate these findings.
Conclusion
A multidisciplinary intervention resulted in large improvements in blood pressure, lipid levels, and gly-cemic control. Although not likely attributable to the DM disease-state-management program alone, values for several regionwide measures of DM-related clinical hospital admission rates decreased.
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Acknowledgments
We are grateful for the invaluable contributions of Ronald Adams, MD, and Audrey Callahan, RN, in their capacity as chairpersons of the ACM committee, and for the work of the entire ACM committee.
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
References
- American Diabetes Association. Standards of medical care in diabetes—2008. Diabetes Care. 2008 Jan;31(Suppl 1):S12–54. doi: 10.2337/dc08-S012. [DOI] [PubMed] [Google Scholar]
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002 Jul 6;360(9326):7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep 12;352(9131):837–53. Erratum in: Lancet 1999 Aug 14;354(9178):602. [PubMed] [Google Scholar]
- Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes (UKPDS 38) UK Prospective Diabetes Study Group. BMJ. 1998 Sep 12;317(7160):703–13. Erratum in: BMJ 1999 Jan 2;318(7175):29. [PMC free article] [PubMed] [Google Scholar]
- Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003 Jan 30;348(5):383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000 Jan 20;342(3):145–53. doi: 10.1056/NEJM200001203420301. Erratum in: N Engl J Med 2000 Mar 9;342(10):748. [DOI] [PubMed] [Google Scholar]
- Adult diabetes national guideline summary [monograph on the Internet] Oakland, CA: Kaiser Permanente Care Management Institute; © 1995–2010 [cited 2010 Oct 2]. Available from: http://providers.kp.org/oh/pdf/oh_diabetescmi_0310.pdf. [Google Scholar]
- HEDIS 2008 Volume 2: Technical specification: Appendix 1: Summary table of measures, product lines and changes [table on the Internet] Washington, DC: National Committee for Quality Assurance; © 2005–2010 [cited 2010 Oct 10]. Available from: www.ncqa.org/Portals/0/HEDISQM/HEDIS2008/2008_Measures.pdf. [Google Scholar]


