Abstract
To develop a novel attenuation strategy applicable to all influenza A viruses, we targeted the highly conserved protein-protein interaction of the viral polymerase subunits PA and PB1. We postulated that impaired binding between PA and PB1 would negatively affect trimeric polymerase complex formation, leading to reduced viral replication efficiency in vivo. As proof of concept, we introduced single or multiple amino acid substitutions into the protein-protein-binding domains of either PB1 or PA, or both, to decrease binding affinity and polymerase activity substantially. As expected, upon generation of recombinant influenza A viruses (SC35M strain) containing these mutations, many pseudo-revertants appeared that partially restored PA-PB1 binding and polymerase activity. These polymerase assembly mutants displayed drastic attenuation in cell culture and mice. The attenuation of the polymerase assembly mutants was maintained in IFNα/β receptor knock-out mice. As exemplified using a H5N1 polymerase assembly mutant, this attenuation strategy can be also applied to other highly pathogenic influenza A virus strains. Thus, we provide proof of principle that targeted mutation of the highly conserved interaction domains of PA and PB1 represents a novel strategy to attenuate influenza A viruses.
Keywords: Computer Modeling, Protein Assembly, Protein Domains, Protein-Protein Interactions, Viral Polymerase
Introduction
Infection with influenza viruses annually claims 250,000–500,000 lives worldwide (1). As exemplified by the 1918 influenza pandemic, which resulted in more than 50 million deaths (2), global spread of a pandemic influenza virus strain can lead to high morbidity and mortality. Besides inactivated vaccines, a live attenuated influenza virus vaccine (FluMist) (3, 4) is currently used for vaccination. Importantly, the degree of attenuation is critical for the safety of the live vaccines, but it also affects their efficacy. For safety reasons, children below the age of two and immunocompromised persons are excluded from vaccination with these live vaccines (3). Furthermore, the live vaccine used in the 2007–2008 season was 50% less efficacious than the inactivated vaccine that was used (5). In the currently used influenza A virus (FluA)3 live vaccine, the degree of attenuation is fixed because a specific master strain is used (3). Thus, to vary the degree of attenuation and to identify new sites that contribute to the safety of live vaccines, new attenuation approaches applicable for all FluA strains are desirable.
A promising target for attenuation of all known FluA strains is the trimeric polymerase complex. Its assembly from the subunits PA, PB1, and PB2 is crucial for polymerase activity and thus virus replication (6–8). PB1 represents the central scaffold protein that binds to PA and PB2 (6, 9–11). Several recently published crystal structures have defined the highly conserved protein-protein-binding domains for PA-PB1 and PB1-PB2 (11–13). Alteration of these conserved residues abrogates subunit interactions accompanied by restricted assembly of polymerase heterotrimers, resulting in decreased polymerase activities (6, 14).
We therefore hypothesized that inefficient polymerase assembly would lead to impaired viral growth and thus attenuation. We identified mutations in the PA-binding domain of PB1 (PB1L8N), in the PB1-binding domain of PA (PAW706E), or in both domains simultaneously (PB1L8IPAW706E), all of which reduced PA-PB1 binding affinities, leading to impaired polymerase assembly and activity. We observed a correlation between reduction in polymerase activity and increased attenuation in cell culture and mice. Importantly, the attenuated phenotype of the polymerase assembly mutants was maintained in the IFNα/β receptor knock-out mice. Thus, targeting of the highly conserved protein-protein interaction domains of PA and PB1 represents a novel strategy to attenuate influenza A viruses.
EXPERIMENTAL PROCEDURES
Generation of Recombinant Influenza A Viruses
Generation of the recombinant viruses A/SC35M (H7N7) (15) and A/Thailand/KAN-1/2004 (H5N1) (16) was performed as described (14, 16) in 6-well tissue plates with 106 293T cells per well using the eight pHW2000 plasmids (300 ng of each) expressing the individual segments and the four pCAGGS plasmids (150 ng of each) coding for PA, PB1, PB2, and NP. After 24 h, released virus was used to infect MDCK cells. Sequences of viral genomes were determined from particles released in the supernatant of the MDCK cells 48 h post infection. Rescued viruses were plaque-purified, and MDCK cells were infected for propagation of virus stocks.
Virus Infections and Growth Assays
MDCK cells or human lung cells (A549) were infected at a multiplicity of infection of 0.001 at 37 °C. Virus titers in the cell supernatants were determined at the indicated time points by plaque assay and expressed as plaque-forming units (pfu)/ml. For passaging the mutant viruses 10 times in cell culture, MDCK cells were infected with ∼103 pfu corresponding to a multiplicity of infection of 0.001 for 24–36 h.
Mouse Experiments
BALB/c mice were obtained from JANVIER SAS (Strasbourg, France). IFNα receptor knock-out (IFNAR0/0) mice (17) backcrossed 12 generations to C57BL/6 were generated by J. Sprent and M. Rubinstein (The Scripps Research Institute, La Jolla, CA) and kindly provided by A. Diefenbach (Institute of Medical Microbiology and Hygiene (IMMH), Freiburg, Germany). 6–8-week-old animals were used for all infection experiments, which were performed in accordance with the guidelines of the local animal care committee. Animals were euthanized if severe symptoms developed or body weight loss approached 25% of the initial value. Lung homogenates were prepared using the FastPrep24 system (MP Biomedicals). For passaging the mutant viruses in vivo, 6–8-week-old BALB/c mice were infected with 103 pfu intranasally. 48 h post infection, total lung was homogenized, and an infectious dose of 103 pfu was used for another round of infection of BALB/c mice. In total, three passages were performed.
Molecular Modeling
Based on the structural model of PB1 (aa 1–15) bound to PA (Protein Data Bank (PDB) 2znl), a homology model was derived for SC35M using Prime (Schroedinger Suite 9.1.107) on an Intel 6600 Core2Duo processor machine (3 GB of RAM) running openSUSE 11.2. To accurately reflect conformational shifts in PA and PB1 induced by the V12I exchange, the side chains of amino acids forming the proximate shell around this residue were refined using Prime Refinement with default settings. Thereby, mainly a shift of the side chain of Met-595 is observed, which is displaced by the bulkier substituent of V12I.
Plasmid Constructions
The pHW2000 plasmid system (18) was used for influenza A virus rescue. To obtain rescue plasmids containing the mutant PB1 or PA genes, site-directed mutagenesis was performed. To generate the pCAGGS expression plasmids encoding PA or PB1 mutants, parts of the corresponding open reading frames were PCR-amplified, digested with AgeI and NotI (PB1) or CFR9I and Bsp119I (PA), and subsequently cloned into pCAGGS-SC35M-PB1-HA and pCAGGS-SC35M-PA-HA.
Co-immunoprecipitation and Immunoblot Analysis
293T cells were transfected with the indicated plasmids in 6-well plates using METAFECTENE (Biontex, Martinsried, Germany). Cells were incubated 24 h post transfection with lysis buffer (20 mm Tris, pH 7.5, 100 mm NaCl, 0.5 mm EDTA, 0.5% Nonidet P-40, 1% protease inhibitor mix G, (Serva, Heidelberg, Germany), 1 mm DTT) for 15 min on ice. After centrifugation by 13,000 rpm at 4 °C, supernatant was incubated with HA- or FLAG M2-specific antibodies (Sigma) coupled to agarose beads, respectively, for 1 h at 4 °C. After three washes with 1 ml of washing buffer (lysis buffer without protease inhibitor mix), bound material was eluted under denaturing conditions, separated on SDS-PAGE gels, and transferred to PVDF membranes. Viral polymerase subunits were detected with antibodies directed against the HA (Covance, Berkeley, CA) or His (Qiagen) or FLAG tag (Sigma).
Enzyme-linked Immunosorbent Assay (ELISA)
ELISA was essentially performed as described previously (19) using biotinylated PB11–15 peptides bound to streptavidin-coated microwell plates and cell extract containing HA-tagged PA WT or mutant proteins.
Cells
293T, A549, and MDCK cells were grown in Dulbecco's modified Eagle's medium supplemented with 10% fetal calf serum, 2 mm l-glutamine, and 1% penicillin/streptomycin. All cells were maintained at 37 °C and 5% CO2.
Peptides
Peptides were synthesized as described in Ref. 19 using a Pioneer automatic peptide synthesizer (Applied Biosystems, Foster City, CA).
Reconstitution of the Influenza Virus Polymerase Activity
293T cells were transiently transfected with a plasmid mixture containing the influenza A virus-derived PB1, PB2, PA, and NP expression plasmids and a polymerase I-driven plasmid transcribing an influenza A virus-like RNA coding for the reporter protein firefly luciferase to monitor viral polymerase activity (14). The transfection mixture also contained a plasmid constitutively expressing Renilla luciferase, which served to normalize variation in transfection efficiency. The reporter activity was determined 24 h post transfection and normalized using the Dual-Glu® luciferase assay system (Promega).
Statistical Analysis
With the exception of the mouse experiments, error bars represent S.E. from at least three independent experiments. For the animal experiments, the indicated number of mice was used for calculating S.E.
Ethics Statement
All animal experiments were performed in compliance with the German animal protection law (Tierschutzgesetz). The mice were housed and handled in accordance with good animal practice as defined by the Federation of Laboratory Animal Science Associations (FELASA) and the national animal welfare body GV-SOLAS. The animal welfare committees of the University of Freiburg (Regierungspräsidium Freiburg) approved all animal experiments.
RESULTS
Mutation at the PA-PB1-binding Interface Leads to Escape Mutants with Impaired Viral Replication
To identify mutations in PA or PB1 that attenuate FluA to a desirable level, we devised an experimental procedure to force spontaneous escape mutants (Fig. 1A). The first step is the generation of PA or PB1 mutant proteins with substantially impaired polymerase activity and subunit interaction. In a second step, viruses expressing these mutant proteins are created by reverse genetics techniques. Taking into account the rapid mutability of FluA, we expected, dependent on the severity of the introduced mutations, the following possible outcomes: (i) maintenance of the inserted mutations, resulting in attenuated viruses; (ii) maintenance of the inserted mutations, leading to non-viable viruses; or (iii) introduction of compensatory mutations. These mutations could restore wild-type (WT) viability or display an attenuated phenotype (Fig. 1A).
FIGURE 1.
Characterization of influenza A viruses with mutations in the PA-binding domain of PB1. A, flowchart of the experimental procedure used to identify attenuated influenza A virus mutants. B, graphic depicting the PB1 mutants used in panel C with single or multiple Asp substitutions within or near the core PA-binding domain (gray box). 8D, L8D; 11D, K11D; 13D, P13D; 4D,5D, N4D,P5D; 6D,7D, T6D,L7D; 8D,9D, L8D,F9D; 10D,11D, L10D,K11D; 4D,8D,11D, N4D,L8D,K11D 4D,5D,10D,11D, N4D,P5D,L10D,K11D; 6D,7D,8D,9D, T6D,L7D,L8D,F9D. C, determination of FluA polymerase activity in the presence of the indicated PB1 mutants. The activity observed with PB1 WT was set to 100%. The omission of PB1 (−PB1) in the transfection mixture served as a negative control. D, emergence of revertants after rescue of PB1 mutants with impaired polymerase activity. PB1 sequences were determined from individual rescue attempts, indicated by #. Virus mixtures with polymorphisms in PB1 were further subjected to plaque purification (indicated by pp and the number of the picked plaque). The arrows indicate the site of polymorphism in the PB1 sequence. PB16D7D, PB1T6D,L7D; PB18D, PB1L8D; PB18D9D, PB1L8D,F9D; PB110D11D, PB1L10D,K11D. E, viral growth of PB1 mutant viruses. MDCK cells were infected with the indicated SC35M mutants at a multiplicity of infection of 0.001, and virus titers in the cell supernatant were determined by plaque assay. PB18N, PB1D8N; PB18V, PB1D8V.
To efficiently disrupt the highly hydrophobic binding interface between PA and PB1 (12, 13), we replaced either single or multiple aa in the PA-binding domain of PB1 by the charged aa aspartic acid (Fig. 1B) and determined viral polymerase activity in human 293T cells (Fig. 1C). Single substitutions by Asp outside (P13D) or at the border (K11D) of the PA-binding core region (12, 13, 19) resulted in a moderately decreased or unchanged polymerase activity (Fig. 1C). In contrast, replacement of the leucine at position 8 (L8D), which lies within the core-binding 310 helix and is known to be essential for binding to PA (9, 19), abrogated polymerase activity to a level below 1% of WT activity (Fig. 1C). Double substitutions at other positions in the N terminus of PB1 (PB11–15) reduced the polymerase activity below 3% of WT activity (Fig. 1C). Next, rescue experiments were performed to generate recombinant SC35M viruses encoding for the above mentioned PB1 mutants. To prevent simple reversion to the WT sequence, 2–3 nucleotide exchanges were performed to mutate the individual aa positions in PB1 (supplemental Fig. S2). As expected, we could generate the mutant virus coding for PB1K11D without compensatory mutations (Table 1) and impaired growth (supplemental Fig. S1A). However, besides the PB1K11D mutant, we were also able to generate recombinant SC35M mutated to PB1T6D,L7D, PB1L8D, PB1L8D,F9D, and PB1L10D,K11D, respectively (Table 1, Fig. 1D). However, the majority of these viruses represented pseudo-revertants, which we defined as viruses containing a non-introduced, non-WT mutation at the site of the mutated residue, which partially or fully restores the WT phenotype. Specifically, during the rescue of SC35M coding for PB1T6D,L7D, the pseudo-revertant PB1T6D,D7Y emerged frequently (Fig. 1D), whereas rescue of the PB1L10D,K11D mutant virus produced two viruses coding for PB1L10D,K11D and PB1L10D,D11V (Fig. 1D, Table 1). Importantly, several independent attempts to rescue mutant viruses coding for PB1L8D resulted exclusively in virus mutants harboring changes to PB1D8A, PB1D8V, or PB1D8N (Fig. 1D, Table 1). PB1D8V or PB1D8A mutant viruses showed only slightly reduced viral growth (Fig. 1E, data not shown), whereas the mutant virus coding for PB1D8N displayed a pronounced attenuation at 12 h p.i. (Fig. 1E). No additional mutations were found in the polymerase genes of this virus (Table 1, supplemental Fig. S2A). Independent attempts to generate SC35M coding for PB1L8D,F9D yielded three virus mutants: PB1D8N,D9F, PB1D8V,D9F, and PB1L8D,F9D* (Fig. 1D). Because PB1D9F represents the wild-type aa at this position, the PB1D8N,D9F and PB1D8V,D9F mutants were phenotypically indistinguishable from the PB1D8V or PB1D8N mutants, respectively. However, the PB1L8D,F9D* mutant represents a recombination event that resulted in restoration of the PB1 open reading frame downstream of the mutated PB1 site (supplemental Fig. S3). As shown in Fig. 1E, the PB1L8D,F9D* mutant showed no attenuation in cell culture (Fig. 1E).
TABLE 1.
Characteristics of SC35 M mutant viruses
ND, not determined; −. no mutations.
| Mutation | Minireplicon activity | Successful rescue attempts/attempts | Compensatory mutations |
|---|---|---|---|
| % | |||
| PB1 | |||
| L8D | 0.5 | 4/6 | D8N (1×); D8V (2×); D8A (1×) |
| L8Na | 67 | 2/2 | No |
| K11D | 113 | 2/2 | No |
| L4D,L5D | 0.2 | 0/4 | − |
| T6D,L7D | 0.4 | 3/4 | D7Y(3×) |
| L8D,F9D | 0.6 | 2/5 | L8N,D9F (1×); L8D,F9D (1×) |
| L10D,K11D | 1.6 | 6/8 | D10V (2×) |
| L4D,L8D,K11D | 0.2 | 0/3 | − |
| L4D,L5D,L10D, 11D | 1.0 | 0/4 | − |
| L6D,L7D,L8D,F9D | 0.2 | 0/3 | − |
| PA | |||
| W706E | 10 | 2/2 | No |
| W706R | 2 | 1/2 | W706G (1×) |
| PB1 + PA | |||
| L8N + W706E | 12 | 2/2 | PB1 N8I (1×); PB1 N8L (1×) |
| L8I + W706Ea | ND | 2/2 | No |
a Direct rescue.
Pseudo-reversions in PB1 Partially Restore Polymerase Activity and Trimeric Polymerase Complex Assembly
We reasoned that the pseudo-reversions PB1D8N and PB1D8V would rescue polymerase activity through restoration of PA-PB1 binding and thus polymerase complex assembly. Indeed, 60% of WT polymerase activity was achieved with PB1D8N, whereas PB1D8V even exceeded WT activity (Fig. 2A). Using an ELISA-based binding assay (19) and peptides corresponding to the 15 N-terminal aa of PB1 (pPB1x), we determined that PA did not bind to pPB1L8D, whereas binding was observed to both pPB1D8N and pPB1D8V, although with significantly lower affinity than pPB1WT (Fig. 2B). To test whether the pseudo-reversions affect the formation of PA-PB1 dimers, we performed co-immunoprecipitation studies. Although PB1D8N weakly interacted with PA, no interaction was detected between PB1L8D and PA (Fig. 2C). In contrast, complex formation between PA and PB1D8V was comparable with that of PA and WT PB1 (Fig. 2C). When co-immunoprecipitation was performed with all three polymerase subunits, both PB1D8N and PB1D8V supported trimeric polymerase complex assembly, whereas PB1L8D did not (Fig. 2D). Consistent with earlier observations (14), lack of trimeric polymerase assembly was accompanied by reduced levels of PB2 (Fig. 2D, cell extract). We speculate that the reduced levels of PB2 are the result of an enhanced degradation of the unbound PB2. To better understand the reason for the diminished binding, we modeled the PA-binding domain of PB1L8D, PB1D8V, and PB1D8N into the PA-PB1 crystal structure. Within the hydrophobic groove of PA (12, 20), Leu-8 plays a key role in protein binding affinity by mediating contacts to Ile-621, Val-636, and Leu-640 (Fig. 2E). Most strikingly, mutation to L8D causes total affinity loss by repulsion of the charged amino acid from this non-polar region (Fig. 2F). L8N still places hydrophilic chemical functionalities unfavorably in this binding groove but may establish a hydrogen-bond interaction with Pro-620 that likely increases the binding affinity (Fig. 2G). In contrast, the D8V mutation apparently causes a reduction of the hydrophobic interaction area due to its smaller dimensions when compared with 8L (Fig. 2H), resulting in weaker binding but not in a complete loss of binding affinity.
FIGURE 2.
Effect of PB1 mutations on polymerase activity and formation of the trimeric polymerase complex. A, determination of FluA polymerase activity in the presence of the indicated PB1 mutants. The activity observed with PB1 WT was set to 100%. The omission of PB1 (PB1−) in the transfection mixture served as a negative control. 8D, L8D; 8N, D8N; 8V, D8V. B, determination of the PA binding affinities of the PB1 mutants. An ELISA-based binding assay was carried out with biotinylated peptides corresponding to the N-terminal 15 aa of the indicated PB1 mutants and a cell extract containing HA-tagged PA. * and ** indicate p values (Student's t test) of <0.05 and <0.01, respectively. OD, optical density. C and D, dimer (C) and trimer (D) formation in the presence of the indicated PB1 mutants was assayed by immunoprecipitation (IP). CE, cell extract. The PB1 mutant 6789D, T6D,L7D,L8D,F9D served as a negative control. E–H, four helices of PA (gray/brown drawings) are involved in the formation of the binding interface for PB1; nitrogen atoms are in blue, and oxygen atoms are in red. E, crystal structure of the WT PB18L. F–H, model of the interface containing the mutations PB1L8D (F), PB1D8N (G), and PB1D8V (H). In H, the surface complementarity between the binding partners is illustrated by visualization of the surface of PA in opaque style and of the surface of PB18L in mesh style.
Molecular Modeling Reveals Attenuating Mutations in the PB1-binding Site of PA
To test whether mutations in the PB1-binding domain of PA have the potential to cause attenuation of FluA, we mutated the highly conserved tryptophan at aa position 706 (Fig. 3A) to either glutamine (PAW706E) or arginine (PAW706R). Molecular modeling suggests that the negatively charged carboxylate moiety of W706E will attract Lys-643 of PA to form a salt bridge (Fig. 3B). This mutation abrogated binding of PA to PB1 in a biochemical pulldown assay (12). We also expected that the mutation W706R would abrogate the interaction with PB1 because W706R positions a positively charged group in the close vicinity of Lys-643 of PA, resulting in the destabilization of the PA protein conformation (Fig. 3C). Both mutants, PAW706E and PAW706R, failed to bind to peptides comprising the N-terminal 15 aa of WT PB1 (Fig. 3D). When compared with WT PA, the polymerase activity was reduced by ∼90% for PAW706E and 98% for PAW706R (Fig. 3E). SC35M coding for PAW706E could be generated by reverse genetics without further compensatory mutations in PA (Fig. 3F) or both PB1 and PB2 (Table 1). As expected, this mutant virus was significantly attenuated by 2.5 log10 24 h p.i. in MDCK (Fig. 3G) and A549 cells (supplemental Fig. S1B). Attempts to rescue SC35M-PAW706R revealed a pseudo-reversion (PAW706G) (Fig. 3F), which was barely impaired in viral growth in MDCK cells (Fig. 3G) and attenuated by 2 log10 24 h p.i. in A549 cells (supplemental Fig. S1B).
FIGURE 3.
Mutations in the PB1-binding site of PA affect viral growth properties. A–C, Trp-706 contributes to PA-PB1 binding by formation of surface contacts with PB1 Asn-4 and PB1 Pro-5 to PA. A, a model of these contacts as in Fig. 2H. The surface of PA around Trp-706 is shown in mesh style, and the surface of PB1 is shown in opaque style, respectively. B, the negatively charged carboxylate moiety introduced by the PA W706E mutation may attract PA Lys-643 to form a salt bridge (wild-type model in gray; conformation predicted for the mutant in green). C, the positive charge introduced by the W706R mutation is likely to have a repulsive effect due to the positive charge of Lys-643. D, determination of the PB1 binding affinities of the PA mutants by ELISA using cell extracts containing mutant PA-HA. OD, optical density; 706E, W706E; 706R, W706R. E, determination of the FluA polymerase activity in the presence of the indicated PA mutants. PA−, omission of PA. F, rescue of SC35M mutants coding for PA mutants. The arrow indicates the site of polymorphism. 706G, W706G. G, viral growth of PA mutant viruses in MDCK cells. H, rescue of a SC35M mutant with mutations in PA and PB1. 8N, D8N; 8I, L8I. I, viral growth curve of SC35M-PAW706EPB1L8I in MDCK cells.
To test the feasibility of generating viruses harboring mutations in both PB1 and PA, we tried to rescue a virus coding for both PAW706E and PB1D8N. In one rescue attempt, we obtained a virus mutant harboring a reversion to WT PB1 and no changes in PA (Table 1). In a second independent rescue attempt, we obtained a virus mutant (SC35M-PAW706EPB1L8I) harboring a mutation in PB1 to N8I without changes in PA (Fig. 3H), which displayed considerably impaired growth in MDCK (Fig. 3I) and A549 cells (supplemental Fig. S1C) with 3–4 log10 titer reduction 24 h p.i., corresponding to a small plaque phenotype of SC35M-PAW706EPB1L8I when compared with WT virus (supplemental Fig. S4). Thus, virus mutants with aa changes in both PB1 and PA can be generated and show impaired growth properties.
Polymerase Assembly Mutants Are Attenuated in Mice
To evaluate the degree of attenuation of our mutant viruses in vivo, we infected BALB/c mice with SC35M mutants. Following intranasal infection, we monitored for weight loss and survival and determined viral lung titers. Although WT-infected mice succumbed to death following infection with 103 pfu, all mice infected with 104 pfu of SC35M-PB1D8N survived despite an initial weight loss (Fig. 4A). Consistent with the lack of attenuation in cell culture, infection with SC35M-PB1D8V was as pathogenic as WT SC35M (supplemental Fig. 5). Mice infected with 103 or 104 pfu of SC35M-PAW706E (Fig. 4B) or SC35M-PAW706EPB1L8I (Fig. 4C) survived with only marginal reduction of body weight, whereas at 105 pfu, 25 and 37.5% of the animals survived infection with SC35M-PAW706E and SC35M-PAW706EPB1L8I, respectively. The degree of attenuation observed with the polymerase assembly mutant viruses correlates with decreased viral lung titers (Fig. 4D).
FIGURE 4.
Polymerase assembly mutants are attenuated in mice. A–C, survival (right) and weight loss (left) of 6–8-week-old female BALB/c mice (n = 6/group) after intranasal infection with the indicated doses of SC35M mutant viruses encoding PB1D8N (PB18N) (A), PAW706E (PA706E) (B), or both PAW706E and PB1L8I (PB18I) (C). WT, wild-type virus SC35M. D, BALB/c mice (n = 5) were infected with 103 pfu of the indicated virus mutants. 48 h p.i., lung titers were determined by plaque assay. E, weight loss and survival of 6–8-week-old female BALB/c mice (n = 10/group) after intranasal infection with the indicated doses of KAN-1 or KAN-1-PAW706E. F, lung titers in mice (n = 5) infected with 103 pfu of either KAN-1 or KAN-1-PAW706E at 48 h p.i. G, weight loss and survival of 8–10-week-old IFNAR0/0 mice (n = 7/group) infected with the indicated doses of WT virus or SC35M-PAW706E. H, lung titer in IFNAR0/0 mice (n = 3) infected with 10 pfu of either WT or SC35M-PAW706E at 48 h p.i.
To demonstrate that our findings apply to other influenza A viruses, we introduced the W706E mutation in PA of the highly pathogenic H5N1 virus A/Thailand/(KAN-1)/2004 (clade 1) (21). When compared with infection with WT KAN-1, this mutant virus (KAN-1-PAW706E) was attenuated by 4 log10 24 h p.i. in MDCK cells (supplemental Fig. 1D) and showed an increase in LD50 of ∼10,000-fold (Fig. 4E, data not shown) as well as significantly lower lung titers (>5 log10) in BALB/c mice (Fig. 4F).
To determine the safety of our mutant viruses, we infected IFNAR0/0 mice, which are highly susceptible to virus infection (17, 22, 23), with up to 103 pfu of the attenuated strain SC35M-PAW706E or 10 pfu of WT virus. All SC35M-PAW706E-infected mice survived, whereas all animals infected with WT virus succumbed to infection (Fig. 4G). At an infection dose of 104 pfu, 66% of the SC35M-PAW706E-infected mice survived. As expected, the viral lung titer of mice infected with 103 pfu SC35M-PAW706E for 48 h was at least 1000-fold reduced when compared with WT-infected mice (Fig. 4H).
Polymerase Assembly Mutants Remain Attenuated after Passaging in Cell Culture and Mice
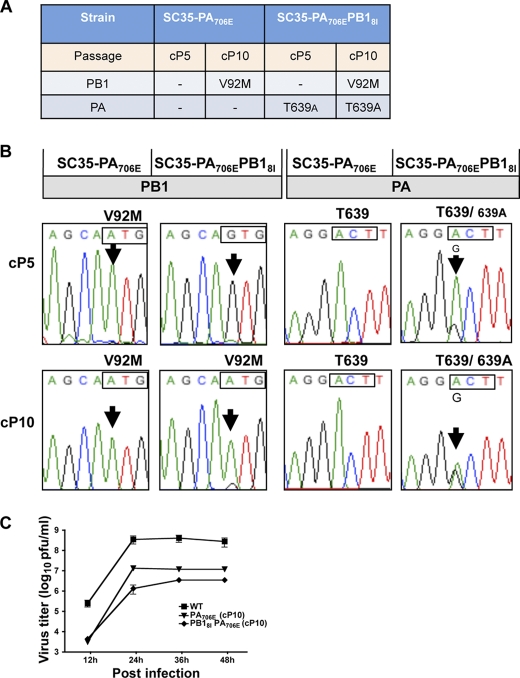
To determine whether the polymerase assembly mutants can easily revert to WT, we performed three serial lung passages of SC35M-PB1D8N, SC35M-PAW706E, and SC35M-PAW706EPB1L8I in BALB/c mice. No changes were observed in PA, whereas mutations to either V92M or V92L outside the PA-binding domain (12, 13, 19) appeared in PB1 of SC35M-PAW706E and SC35M-PAW706EPB1L8I, respectively (Fig. 5, A and B). Infection of IFNAR0/0 mice with 100 pfu of SC35M-PAW706E passaged three times in mice resulted only in a transient weight loss (Fig. 5C), demonstrating that this virus was still strongly attenuated. Furthermore, serially passaging SC35M-PAW706E and SC35M-PAW706EPB1L8I 10 times in MDCK cells also led to a mutation to PB1V92M (Fig. 6, A and B), as well as PAT639A. Importantly, growth of both passaged viruses remained impaired in MDCK cells (Fig. 6C). Together, these results indicate that the polymerase assembly mutants can acquire mutations in the viral genome during the passages in mice or cell culture but that these mutations do not reverse their attenuated phenotype. Therefore, the polymerase assembly mutants are phenotypically stable.
FIGURE 5.
Characterization of polymerase assembly mutants after serial passages in mice. A, mutations in PB1 and PA observed after serial passages of the indicated virus mutants in BALB/c mice. mP1–3, mouse passage 1–3. −, no mutations found. B, electropherogram of PB1 and PA sequences after serial passages of the indicated viruses in BALB/c. The arrows indicate the site of mutation or polymorphism. SC35M-PB18N, SC35M-PB1D8N; SC35M-PA706E, SC35M-PAW706E. C, survival and weight loss of 8–10-week-old IFNAR0/0 mice (n = 6) infected with the SC35M-PAW706E passaged three times in mice (PA706E (mP3)).
FIGURE 6.
Characterization of polymerase assembly mutants after serial passages in cell culture. A, mutations in PB1 and PA observed after serial passages of the indicated virus mutants in MDCK cells. cP5 and cP10, cell passage 5 and 10. −, no mutations found. B, electropherogram of PB1 and PA sequences after serial passages of the indicated viruses in MDCK cells. The arrows indicate the sites of mutation or polymorphism. SC35M-PA706E, SC35M-PAW706E; SC35M-PA706EPB181, SC35M-PAW706EOPB1L8I; C, viral growth of the indicated mutant viruses in MDCK cells.
DISCUSSION
The objective of this study was to generate attenuated influenza A viruses based on defects in the assembly of the polymerase complex. Accordingly, we reasoned that alteration of key amino acids involved in the subunit interactions would force the virus to escape by acquisition of new mutations, some of which would fail to restore efficient polymerase complex assembly and activity. Indeed, the majority of the rescued mutant viruses represent pseudo-revertants with various degrees of attenuation. Only a few intentionally introduced mutations (e.g. PB1L10D,K11D and PAW706E) were tolerated and, as predicted, recombinant viruses expressing these proteins were attenuated. However, the occurrence of compensatory mutations at other aa positions in PA or PB1 was not observed. This strongly suggests that only few aa exchanges are tolerated within these binding domains without loss of affinity. The lack of compensatory mutations especially in the relatively small core PA-binding domain might be caused by the involvement of several aa of the 310 helix in mediating contact to PA (12, 13, 19).
The amino acids within the PA-binding domain of PB1 (e.g. Leu-8) and the PB1-binding domain of PA (e.g. Trp-706), which are essential for polymerase subunit interaction, are highly conserved and identical among all known influenza A virus strains (12–14, 24). We therefore infer that targeting these key residues results in attenuation of virtually all influenza A virus strains. As exemplified by two unrelated viruses, the highly pathogenic H5N1 strain KAN-1 and the mouse-adapted strain SC35M (H7N7) mutation in PA (W706E) resulted in severe attenuation of both viruses in mice. However, the degree of attenuation is higher for the H5N1 mutant virus. This might reflect differences in intrinsic PA/PB1 binding affinities between these virus strains, as described recently for FluA and influenza B viruses (14).
We also observed that targeting different key residues within the PA- or PB1-binding domains could vary the degree of attenuation because the mutation L8N in PB1 resulted in a less attenuated phenotype of SC35M in cell culture and mouse models when compared with the W706E mutation in PA or a combination of both mutations. The possibility to fine-tune the individual degree of attenuation by defined substitutions in PA or PB1 represents a unique tool to avoid over-attenuation. The repertoire of suitable mutations could possibly be extended to the similarly conserved PB2-PB1-binding site (11).
The polymerase assembly mutant viruses are also drastically attenuated in mice with immune system defects, as demonstrated in IFNAR0/0 mice, which are highly susceptible to virus infection (17, 22, 23). We attribute this observation to the host-independent polymerase assembly defect of these viruses, which forces attenuation under all conditions. Our findings suggest that live vaccines harboring these mutations should possess a good safety profile in patients with impaired antiviral defense mechanisms.
Several reasons might account for the genetic stability of the polymerase assembly mutants in mice and cell culture. The observed reduction in growth kinetics of these mutants further decreases the population size and thus the likelihood that viable escape mutants will emerge. Furthermore, the PB1/PA-binding interface is highly conserved and cannot tolerate many aa changes without reducing the binding affinity (12–14, 24). Thus, we speculate that point mutations, which cause reversions to wild-type polymerase activity, are unlikely.
Live attenuated viruses confer several advantages as vaccines over traditionally used inactivated viruses, including induction of cellular as well as humoral immunity, broader protection among influenza virus subtypes, and better protection in children (3). However, the currently used cold-adapted influenza vaccine (FluMist) is not approved for children under the age of two or immunocompromised patients (3). Our attenuation strategy might contribute to a better safety profile for these viruses, as demonstrated by infection of IFNAR0/0 mice. Furthermore, the cold-adapted master strain A/AnnArbor/6/60 H2N2 contains a fixed degree of attenuation (3), whereas we have developed a strategy to easily identify new mutations, which allow attenuation to be fine-tuned.
Overall, generation of polymerase assembly mutants can be applied to all influenza A viruses, resulting in adjusted degrees of attenuation. Thus, this novel approach may also contribute to the development of phenotypically stable live vaccines against seasonal and pandemic influenza. Furthermore, this attenuation strategy could also be used to make successful reassortment between attenuated live vaccines and circulating influenza A viruses less probable. Such reassortment events are of great concern because the resulting viruses might have an increased pathogenicity. By targeting a protein-protein interaction domain encoded on two segments, exchange of only one segment should maintain attenuation. However, our mutations could be combined with several other attenuation strategies, which have been described (3, 25–28).
We provide proof of principle that disruption of a protein-protein interaction site essential for polymerase complex formation results in an attenuation of influenza viruses. Thus, targeting the interaction domains of viral proteins that are essential for productive infection may represent a universal approach that could be applied to many other viruses.
Supplementary Material
Acknowledgment
We thank Friedemann Weber for critical reading of the manuscript.
This study was supported by grants from the Deutsche Forschungsgemeinschaft (DFG) and the Bundesministerium für Bildung und Forschung (BMBF, FluResearchNet). This study was also supported by a grant from the Excellence Initiative of the German Research Foundation (GSC-4, Spemann Graduate School) (to K. W.).

The on-line version of this article (available at http://www.jbc.org) contains supplemental Figs. S1–S5.
- FluA
- influenza A virus
- MDCK
- Madin-Darby canine kidney
- IFNAR
- IFNα receptor
- aa
- amino acid(s)
- p.i.
- post infection.
REFERENCES
- 1. Salomon R., Webster R. G. (2009) Cell 136, 402–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tumpey T. M., Belser J. A. (2009) Annu. Rev. Microbiol. 63, 79–98 [DOI] [PubMed] [Google Scholar]
- 3. Ambrose C. S., Luke C., Coelingh K. (2008) Influenza Other Respi. Viruses 2, 193–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Maassab H. F. (1967) Nature 213, 612–614 [DOI] [PubMed] [Google Scholar]
- 5. Monto A. S., Ohmit S. E., Petrie J. G., Johnson E., Truscon R., Teich E., Rotthoff J., Boulton M., Victor J. C. (2009) N. Engl. J. Med. 361, 1260–1267 [DOI] [PubMed] [Google Scholar]
- 6. Perez D. R., Donis R. O. (2001) J. Virol. 75, 8127–8136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brownlee G. G., Sharps J. L. (2002) J. Virol. 76, 7103–7113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Perales B., Ortín J. (1997) J. Virol. 71, 1381–1385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pérez D. R., Donis R. O. (1995) J. Virol. 69, 6932–6939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ohtsu Y., Honda Y., Sakata Y., Kato H., Toyoda T. (2002) Microbiol. Immunol 46, 167–175 [DOI] [PubMed] [Google Scholar]
- 11. Sugiyama K., Obayashi E., Kawaguchi A., Suzuki Y., Tame J. R., Nagata K., Park S. Y. (2009) EMBO J. 28, 1803–1811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Obayashi E., Yoshida H., Kawai F., Shibayama N., Kawaguchi A., Nagata K., Tame J. R., Park S. Y. (2008) Nature 454, 1127–1131 [DOI] [PubMed] [Google Scholar]
- 13. He X., Zhou J., Bartlam M., Zhang R., Ma J., Lou Z., Li X., Li J., Joachimiak A., Zeng Z., Ge R., Rao Z., Liu Y. (2008) Nature 454, 1123–1126 [DOI] [PubMed] [Google Scholar]
- 14. Wunderlich K., Juozapaitis M., Mänz B., Mayer D., Götz V., Zöhner A., Wolff T., Schwemmle M., Martin A. (2010) J. Biol. Chem. 285, 16704–16712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gabriel G., Dauber B., Wolff T., Planz O., Klenk H. D., Stech J. (2005) Proc. Natl. Acad. Sci. U.S.A. 102, 18590–18595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mänz B., Matrosovich M., Bovin N., Schwemmle M. (2010) J. Virol. 84, 8316–8321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Müller U., Steinhoff U., Reis L. F., Hemmi S., Pavlovic J., Zinkernagel R. M., Aguet M. (1994) Science 264, 1918–1921 [DOI] [PubMed] [Google Scholar]
- 18. Hoffmann E., Neumann G., Kawaoka Y., Hobom G., Webster R. G. (2000) Proc. Natl. Acad. Sci. U.S.A. 97, 6108–6113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wunderlich K., Mayer D., Ranadheera C., Holler A. S., Mänz B., Martin A., Chase G., Tegge W., Frank R., Kessler U., Schwemmle M. (2009) PLoS One 4, e7517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liu H., Yao X. (2010) Mol. Pharm. 7, 75–85 [DOI] [PubMed] [Google Scholar]
- 21. Puthavathana P., Auewarakul P., Charoenying P. C., Sangsiriwut K., Pooruk P., Boonnak K., Khanyok R., Thawachsupa P., Kijphati R., Sawanpanyalert P. (2005) J. Gen. Virol. 86, 423–433 [DOI] [PubMed] [Google Scholar]
- 22. García-Sastre A., Durbin R. K., Zheng H., Palese P., Gertner R., Levy D. E., Durbin J. E. (1998) J. Virol. 72, 8550–8558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hwang S. Y., Hertzog P. J., Holland K. A., Sumarsono S. H., Tymms M. J., Hamilton J. A., Whitty G., Bertoncello I., Kola I. (1995) Proc. Natl. Acad. Sci. U.S.A. 92, 11284–11288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ghanem A., Mayer D., Chase G., Tegge W., Frank R., Kochs G., García-Sastre A., Schwemmle M. (2007) J. Virol. 81, 7801–7804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stech J., Garn H., Wegmann M., Wagner R., Klenk H. D. (2005) Nat. Med. 11, 683–689 [DOI] [PubMed] [Google Scholar]
- 26. Muster T., Subbarao E. K., Enami M., Murphy B. R., Palese P. (1991) Proc. Natl. Acad. Sci. U.S.A. 88, 5177–5181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Talon J., Salvatore M., O'Neill R. E., Nakaya Y., Zheng H., Muster T., García-Sastre A., Palese P. (2000) Proc. Natl. Acad. Sci. U.S.A. 97, 4309–4314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mueller S., Coleman J. R., Papamichail D., Ward C. B., Nimnual A., Futcher B., Skiena S., Wimmer E. (2010) Nat. Biotechnol. 28, 723–726 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.