Abstract
Background
There has been an increasing role of advanced minimally invasive procedures in hepatopancreatobilliary (HPB) surgery. However, there are no set minimum laparoscopic case requirements.
Methods
A 14-question electronic survey was sent to 82 worldwide HPB fellowship programme directors.
Results
Forty-nine per cent (n = 40) of the programme directors responded. The programmes were predominantly university based (83%). Programmes had either one (55%) or two fellows (40%) each year. Programmes (35–48%) had average annual volumes of 51–100 hepatic, 51–100 pancreatic and 25–50 biliary cases. For many programmes, <10% of hepatic (48%), pancreatic (40%) and biliary (70%) cases were done laparoscopically. The average annual fellow case volumes for hepatic, pancreatic and biliary surgeries were 25–50 (62%), 25–50 (47%) and <25 (50%), respectively. The average annual number of hepatic, pancreatic and biliary cases done laparoscopically by a fellow was 9, 9 and 4, which constitutes 36%, 36% and 16%, respectively, of the International Hepato-Pancreato-Billiary Association (IHPBA) requirement.
Conclusion
We surmise that the low average number of surgeries performed by minimally-invasive techniques by HPB fellows is not sufficient in today's practice. Should there be an increase in the minimal number of hepatic, pancreatic and complex biliary cases to 50, 50, and 25, with at least 50% of these performed laparoscopically?
Keywords: HPB fellowship, MIS training, minimum requirements, laparoscopy
Introduction
Sub-specialization has changed the way that general surgery is practiced. Hepatobiliary and pancreatic surgery is maturing as a subspecialty.1 There has been an increasing role of advanced minimal invasive procedures in hepatopancreatobilliary (HPB) surgery such as laparoscopic, robotic and natural orifice surgery (NOTES). Hence HPB fellowship in today's world should provide expertise in both minimally invasive and open HPB surgery. According to the International Hepato-Pancreato-Biliary Association (IHPBA), the minimum number of cases required to graduate from HPB fellowship is 25 cases of each hepatic, pancreatic and complex biliary procedures. However, there are no set minimum laparoscopic case requirements. We conducted a survey to look at the current state of minimal invasive techniques training in the HPB fellowship programmes worldwide.
Methods
A 14-question electronic survey was created using http://www.surveymonkey.com. This was sent to 82 worldwide HPB fellowship programme directors (PDs). This included 30 programmes from the United States and Canada, and 52 international programmes mentioned in the fellowship register on the IHPBA website. We looked into the number of fellows each year, duration of fellowship, HPB trained faculty, annual case volume, fellow case volumes, percentages of minimally invasive procedures and the use of robotic surgery and NOTES.
Results
Forty-nine per cent (n = 40) of the programme directors responded. The programmes were predominantly university based (University/Community, 33 : 7). Most of the programmes had either one (55%) or two fellows (40%) each year (Fig. 1a). The duration of fellowship was 1 year (45%), 2 years (40%) and >2 years (15%) (Fig. 1b). Number of faculties with formal HPB training in most of the programmes was 4–6 (45%) (Fig. 1c). The majority of the programmes were functional for less than 5 years (45%, n = 17), this was followed by programmes functional for 6–10 years (39%, n = 15) and only 16% (n = 6) were functional for >10 years (Fig. 1d).
Figure 1.
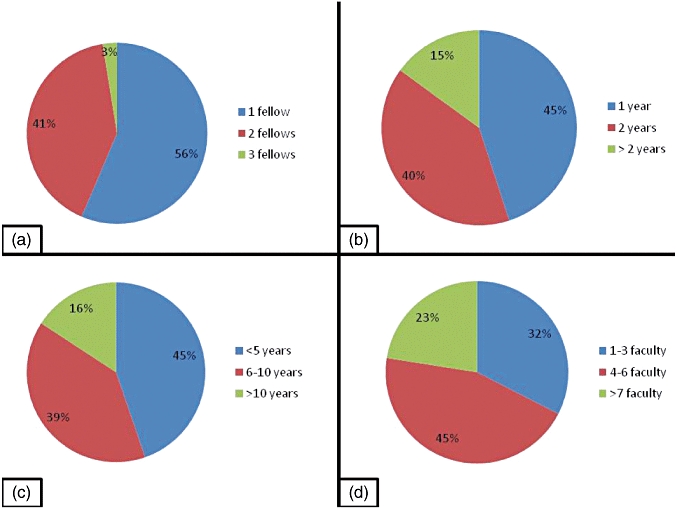
(a) Number of fellows each year. (b) Duration of fellowship. (c) Years programmes were functional. (d) Number of faculty in each programme
The average annual case volumes for most of the programmes were: hepatic 51–100 (35%), pancreatic 51–100 (48%) and complex biliary cases 25–50 (45%) (Fig. 2a). In the majority of the programmes only less than 10% of hepatic, pancreatic and complex biliary cases were done laparoscopically (48%, 40% and 70%, respectively) (Fig. 2b). The majority of the average annual fellow case volume for hepatic, pancreatic and complex biliary surgeries were 25–50 (62%), 25–50 (47%) and <25 (50%), respectively (Fig. 3a). For the majority of the programmes, the fellows performed less than five cases of hepatic, pancreatic and complex biliary surgeries laparoscopically (Fig. 3b). The average annual number of hepatic, pancreatic and complex biliary cases done laparoscopically by a fellow was 9, 9 and 4, respectively. This constitutes 36%, 36% and 16% of the minimum 25 cases in each category as required per IHPBA.
Figure 2.
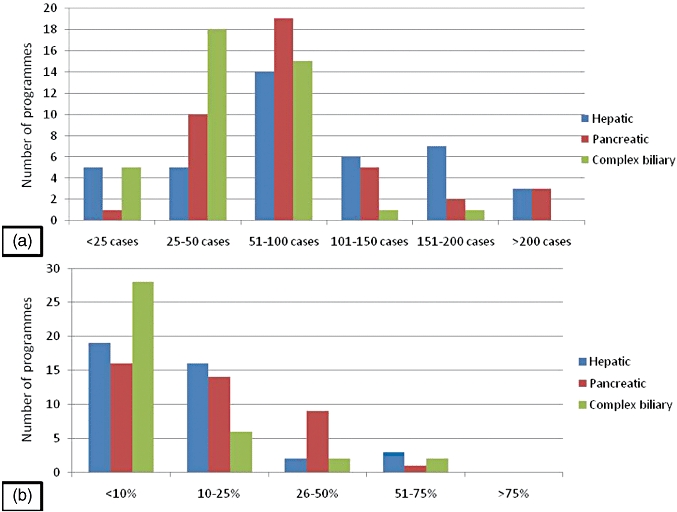
(a) Average annual case volume. (b) Percentage of cases done laparoscopically
Figure 3.
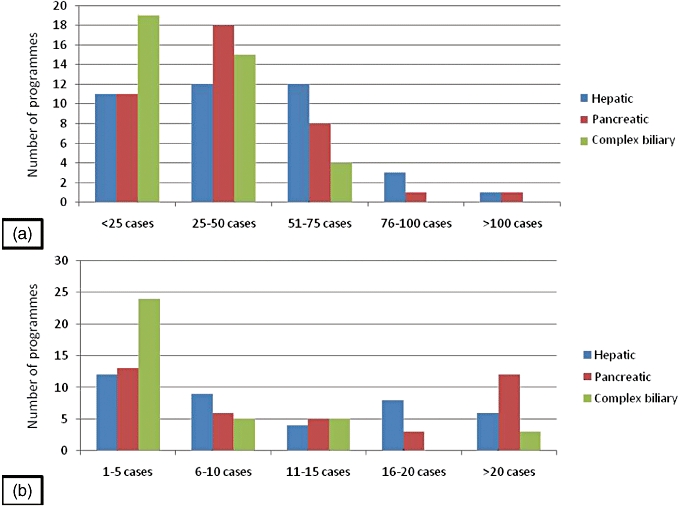
(a) Average annual fellow case volume. (b) Average annual fellow laparoscopic case volume
Only less than half of the programmes were performing robotic (40%), single port (40%) and natural orifice (23%) surgeries. Fifty-five per cent (n = 22) of these programmes had a transplant service and 48% (n = 19) had bariatric services attached to their programmes.
In only 28% of the programmes, the fellows were involved in basic science research.
Discussion
HPB diseases involve cases of high complexity and generally low volume, with associated high patient morbidity and mortality.2 HPB surgeries have always been a challenge for general surgeons. They require comprehensive knowledge, meticulous surgical technique and a good institutional support system. In 2008, a consensus conference on the international position of laparoscopic liver surgery concluded that laparoscopic liver surgery is a safe and effective approach in the management of surgical liver disease in the hands of trained surgeons with experience in hepatobiliary and laparoscopic surgery. National and international societies, as well as governing boards, should become involved in the goal of establishing training standards and credentialing, to ensure consistent standards and clinical outcome.3
There are merely 82 programmes worldwide that follow IHPBA training recommendations. Advanced training standards are determined by the Educational Committee of the IHPBA. Training is performed over 12 months, or over 24 months when transplant training is included. Duties are divided into clinical and surgical fields. Operative experience must include three categories (hepatic, pancreatic and biliary surgery) with a minimum of 100 operative procedures and a minimum of 25 cases in each category. If transplant experience is included, 30 liver transplants and 25 donor procurements are required.4 There are no set minimum laparoscopic cases requirements for a fellow to graduate a HPB programme.
Accreditation Council of Graduate Medical Education (ACGME), the regulatory body for general surgery residency training in USA, proposes a minimum number of four hepatic cases, three pancreatic cases and an undetermined number of biliary cases that are integrated into the alimentary tract, for a resident to graduate from a general surgery residency. Though there is no specific requirement for any of the HPB cases to be done using minimally invasive approaches, a graduating resident has to do at least 60 basic and 25 advanced laparoscopic cases. Guidelines have been proposed for HPB/UGI training that could be undertaken in a format that provides a multidisciplinary approach to complex malignant and benign diseases of the UGI tract.5 But again, there are no specific requirements for laparoscopic cases in these guidelines as well.
A study by Vigano et al. found the learning curve in laparoscopic liver resections to be 60 cases, and this learning curve was reproducible in a liver unit.6 Also, a review on laparoscopic pancreatic surgery stated that it is an advanced laparoscopic procedure with a significant learning curve, and the surgeon needs to possess advanced laparoscopic skills.7 Studies have concluded that in pancreatic surgeries, laparoscopy may contribute to reduced operation time and peri-operative blood loss, and reduces surgical stress.8 The laparoscopically performed cases by a fellow in HPB category was <5 cases each in most of the programmes. We believe that this number is far too less for today's world, wherein patients demand for keyhole surgeries. The requirement of 25 cases in the hepatic and pancreatic cases category has to be increased to at least 50 cases. At least 50% of the required numbers should be done laparoscopically. For surgeons interested in pursuing a career in minimally invasive HPB surgery, it is currently accepted that expertise in both laparoscopy and HPB surgery would be the sole means to gain the ability to tackle advanced procedures in this complex field.9
The face of surgery has changed over the past two decades with the introduction of laparoscopic techniques. The majority of surgical specialties now perform minimally invasive procedures. Furthermore, in an attempt to reduce the invasive nature of surgery, new surgical techniques such as NOTES and single-port surgery are under development. In a previous study done to analyse patient preferences and expectations of these novel techniques for a hypothetical situation of acute appendicitis, single port surgery laparoscopic surgery was the most preferred choice of surgery among patients.10 In our survey we found that only 40% of programmes were performing single port surgeries. Studies have suggested that Robotic-assisted hepatic and pancreatic surgeries are a feasible and safe alternative, with a potential to reduce surgical trauma and pain. These also tend to improve the surgeon's technical comfort in performing such procedures.11,12 Our survey showed only 40% of the programmes was performing robotic surgeries. Teaching advanced laparoscopic skills is inherently more difficult. HPB training should consider use of cadavers and a simulation laboratory for refining minimally invasive surgical skills. Formulation of a defined curriculum involving simulation and cadaveric dissections would be helpful.
Research and multidisciplinary training enhance fellowship training. In our survey we noted that in only 28% of the programmes, the fellows were involved in basic science research. Hence, the programmes should provide facilities and set forth defined time in their curriculum for pursuit of these endeavours.
Conclusions
The average numbers of hepatic, pancreatic and complex biliary surgeries performed by minimally invasive techniques by fellows are less than 10. This is not sufficient in today's practice. We conclude that there should be an increase in the minimal number of hepatic, pancreatic and complex biliary cases to 50, 50 and 25, with at least 50% of these to be performed laparoscopically. Attempts should be made at increasing the fellows' exposure to robotic and natural orifice surgeries.
Conflicts of interest
None declared.
References
- 1.Dixon E, Vollmer CM, Jr, Bathe O, Sutherland F. Training, practice, and referral patterns in hepatobiliary and pancreatic surgery: survey of general surgeons. J Gastrointest Surg. 2005;9:109–114. doi: 10.1016/j.gassur.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Granger SR, Glasgow RE, Battaglia J, Lee RM, Scaife C, Shrieve DC, et al. Development of a dedicated hepatopancreaticobiliary program in a university hospital system. J Gastrointest Surg. 2005;9:891–895. doi: 10.1016/j.gassur.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009;250:825–830. doi: 10.1097/sla.0b013e3181b3b2d8. [DOI] [PubMed] [Google Scholar]
- 4.Chang YJ, Mittal VK. Hepato-pancreato-biliary training in general surgery residency: is it enough for the real world? Am J Surg. 2009;197:291–295. doi: 10.1016/j.amjsurg.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Rassadi R, Dickerman RM, EL Dunn, Tarnasky PR, Linder JD, Mejia A, et al. Hepatopancreaticobiliary (HPB) surgery: what is the right fellowship for the right training? J Surg Educ. 2008;65:186–190. doi: 10.1016/j.jsurg.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg. 2009;250:772–782. doi: 10.1097/SLA.0b013e3181bd93b2. [DOI] [PubMed] [Google Scholar]
- 7.Nakeeb A. Laparoscopic pancreatic resections. Adv Surg. 2009;43:91–102. doi: 10.1016/j.yasu.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 8.Fernández-Cruz L, Cesar-Borges G, López-Boado MA, Orduña D, Navarrro S. Minimally invasive surgery of the pancreas in progress. Langenbecks Arch Surg. 2005;390:342–354. doi: 10.1007/s00423-005-0556-5. [DOI] [PubMed] [Google Scholar]
- 9.Gumbs AA, Gayet B. The medical and surgical department of digestive diseases and minimally invasive hpb fellowship at IMM. HPB (Oxford) 2007;9:470–471. doi: 10.1080/13651820701729978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rao A, Kynaston J, Macdonald ER, Ahmed I. Patient preferences for surgical techniques: should we invest in new approaches? Surg Endosc. 2010;24:3016–3025. doi: 10.1007/s00464-010-1078-y. [DOI] [PubMed] [Google Scholar]
- 11.Giulianotti PC, Sbrana F, Bianco FM, Addeo P, Caravaglios G. Robot-assisted laparoscopic middle pancreatectomy. J Laparoendosc Adv Surg Tech A. 2010;20:135–139. doi: 10.1089/lap.2009.0296. [DOI] [PubMed] [Google Scholar]
- 12.Choi SB, Park JS, Kim JK, Hyung WJ, Kim KS, Yoon DS, et al. Early experiences of robotic-assisted laparoscopic liver resection. Yonsei Med J. 2008;49:632–638. doi: 10.3349/ymj.2008.49.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]


