Abstract
Introduction
Studies and reports suggest that both hyperlipidemia and its pharmacologic treatment may lead to an increased risk of erectile dysfunction (ED).
Aims
Our objectives were to examine the association between 1) treated hyperlipidemia and ED; 2) untreated hyperlipidemia and ED.
Methods
Data from 1,899 men aged 30–79 were used from the Boston Area Community Health Survey of community-dwelling residents of Boston, MA, collected during 2002–2005 using an in-person interview, self-administered questionnaires, and a venous blood draw.
Main Outcome Measures
ED was measured using the Short Form International Index of Erectile Function. A case of treated hyperlipidemia was defined by use of anti-lipemics in the past month, while untreated hyperlipidemia was serum total cholesterol ≥240 milligrams per deciliter with no anti-lipemic use. We estimated associations using odds ratios (ORs) and 95% confidence intervals (CIs) from multivariate logistic regression.
Results
Men with treated hyperlipidemia were older, had more comorbidities and used more medications compared to men with untreated hyperlipidemia or no hyperlipidemia. In multivariate models stratified by age and the presence of diabetes and/or cardiovascular disease (CVD), we saw no association between hyperlipidemia drug treatment and ED, except among younger men (<55) who had diabetes and/or CVD, where a strong association with an imprecise confidence interval was observed (OR=10.39, 95% CI: 3.25, 33.20). There was no significant positive association between untreated hyperlipidemia and ED in any multivariate model.
Conclusion
Lipid-lowering medications may be associated with ED among some men. The well-established benefits of lipid-lowering therapy should always be weighed against potential adverse effects.
INTRODUCTION
Lipid regulators for hyperlipidemia and other indications were the most popular prescription drugs sold in the U.S. in 2007.1 A statin, atorvastatin, was the top-selling medication of any class in the U.S. from 2000 to 20062, 3 and was used by 6.7% of adults in 2006.4 Because of their popularity as well as their indication for long-term use,5 the broader physiologic effects of statins are of special clinical and public health importance.
Both hyperlipidemia and erectile dysfunction (ED) are common problems in older men, and may be interrelated.6 As hyperlipidemia may contribute to ED by promoting endothelial dysfunction, it has been suggested that statins could be beneficial in alleviating ED through their pleiotropic effects in improving endothelial function.7, 8 The body of evidence for the complex interrelationships between hyperlipidemia, its treatment, and erectile dysfunction was recently reviewed.9 While the observation that hyperlipidemia is more prevalent among men with ED is largely consistent, existing evidence for a role for lipid-lowering treatments in the alleviation or promotion of ED is at present conflicting. In addition to case reports from drug safety monitoring and a systematic review,10, 11 one recent prospective clinical study of approximately 100 men with cardiovascular risk factors showed a marked worsening of erectile function six months following statin initiation.12
We examined these interrelationships in a population-based study of community-dwelling men. The objectives were 1) to describe the characteristics of those with treated or untreated hyperlipidemia and ED; 2) to estimate the association between treated and untreated hyperlipidemia and ED; and 3) to determine whether any observed association could be explained by potential confounding factors, such as cardiovascular risk factors.
METHODS
Design and data collection
The Boston Area Community Health (BACH) Survey is a population-based observational study of residents of Boston, Massachusetts. A two-stage, stratified cluster sampling design was used to recruit approximately equal numbers of participants to pre-specified age, race/ethnic, and gender groups. Interviews were completed for 63.3% of eligible subjects, with a resulting sample of 2,301 men (age range 30–79) with 700 black, 766 Hispanic and 835 white participants. This analysis used baseline data collected between April 2002 and June 2005 after written informed consent. A non-fasting venous blood sample (20 ml) was also collected as close to awakening as possible. All protocols and informed consent procedures were approved by New England Research Institutes' Institutional Review Board. Further details regarding the study are available.13
Hyperlipidemia and ED definitions
A treated case of hyperlipidemia was defined as a user of any prescription anti-lipemic medications in the past month (statins and/or non-statin anti-lipemics), while an untreated case of hyperlipidemia was defined as no use of anti-lipemics and total serum cholesterol ≥240 milligrams per deciliter (in accordance with National Cholesterol Education Program guidelines to define high total cholesterol).14 Men who did not use anti-lipemics and had total serum cholesterol <240 were considered to have no hyperlipidemia. Serum cholesterol was measured enzymatically15 in a core laboratory certified by the National Heart, Lung, and Blood Institute/Centers for Disease Control and Prevention Lipid Standardization Program. The method combines the specificity of the enzymatic reaction with peroxidase/phenol-4-aminophenazone indicator reaction, and was performed using the Hitachi 917 analyzer using reagents and calibrators from Roche Diagnostics (Indianapolis, IN). At cholesterol concentrations of 132.8 and 280.4 mg/dL, the day-to-day reproducibility reflected by coefficient of variation (CV), was 1.7% (SD=2.4 mg/dL) and 1.6%, respectively.
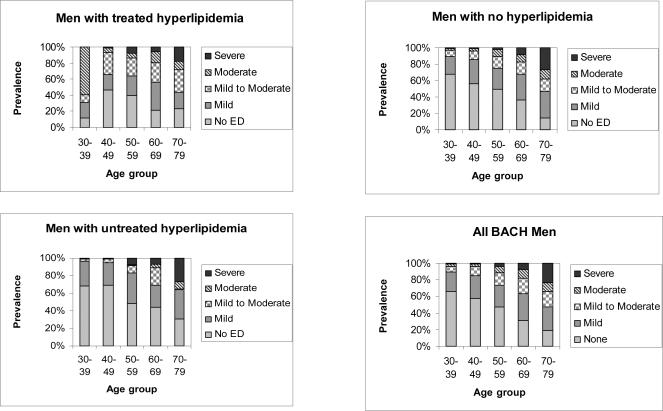
ED was defined using the 5-item short form International Index of Erectile Function (IIEF-5), a self-administered, validated questionnaire.16 The score ranges from 5 to 25, with lower scores indicating poorer erectile function. In Tables 2–3, a case of treated ED was defined as any user of phosphodiesterase inhibitors, papaverine or prostaglandin, a case of untreated ED was defined as IIEF-5 score of ≤16 and no evidence of ED drug treatment, while no ED was defined as IIEF-5 score of ≥17 and no evidence of ED drug treatment. In Tables 5–6, a dichotomous definition of ED was created for use in bivariate analyses and logistic regression, using a cutoff of IIEF-5 ≤16 (combining mild to moderate, moderate, and severe categories to indicate the presence of ED regardless of treatment). In Figure 1, ED was displayed by severity as follows: severe (IIEF-5 score 5–7), moderate (8–11), mild to moderate (12–16), mild (17–21), and no ED (22–25).16.
Table 2.
Characteristics of those with treated, untreated and no erectile dysfunction (ED)* among men contributing blood samples in Boston Area Community Health Survey, 2002–2005, N=1899.
| Continuous covariates† | Treated ED (n=40) (Mean, Standard Error) | Untreated ED (n=472) (Mean, Standard Error) | No ED (n=1387) (Mean, Standard Error) |
|---|---|---|---|
| Age | 52.6 (2.3) | 55.3 (1.1) | 45.5 (0.5) |
| Median | 52.3 | 56.2 | 43.2 |
| Years education | 17.3 (0.6) | 12.9 (0.4) | 15.2 (0.2) |
| Total cholesterol (mg/dl) | 195.5 (7.0) | 188.8 (2.8) | 201.5 (1.8) |
| Categorical covariates† | Treated ED % | Untreated ED % | No ED % |
|---|---|---|---|
| Socioeconomic status | |||
| Low | 6.4 | 49.4 | 18.4 |
| Middle | 40.2 | 36.8 | 52.1 |
| High | 53.4 | 13.8 | 29.5 |
| Race/ethnicity | |||
| Black | 17.6 | 31.1 | 23.9 |
| Hispanic | 10.7 | 16.8 | 12.2 |
| White | 71.7 | 52.1 | 64.0 |
| Health insurance | |||
| Private | 82.9 | 47.1 | 70.6 |
| Public | 12.6 | 38.1 | 13.8 |
| None | 4.5 | 14.8 | 15.5 |
| Current smoker | |||
| Never | 53.3 | 33.7 | 48.1 |
| Former | 29.1 | 37.7 | 26.7 |
| Current | 17.6 | 28.6 | 25.1 |
| Alcohol use | |||
| None | 9.9 | 43.2 | 22.7 |
| <1/day | 49.1 | 31.5 | 42.0 |
| 1–2/day | 37.4 | 16.7 | 25.8 |
| 3+/day | 3.5 | 8.6 | 9.5 |
| Physical activity score (PASE) | |||
| Low (<100) | 16.1 | 46.1 | 20.9 |
| Medium (100–249) | 65.5 | 40.5 | 49.4 |
| High (250+) | 18.4 | 13.4 | 29.7 |
| BMI categories | |||
| <25.0 | 35.4 | 23.1 | 27.3 |
| 25.0–29.9 | 41.5 | 38.8 | 39.6 |
| 30.0+ | 23.2 | 38.1 | 33.1 |
| Cardiovascular disease ‡ | 43.7 | 34.7 | 15.2 |
| Hypertension | 53.7 | 44.5 | 21.1 |
| Diabetes (Type I and/or Type II) | 32.0 | 19.4 | 6.5 |
| Depression | 17.3 | 24.6 | 11.4 |
| Self-reported history of hyperlipidemia | 53.8 | 42.8 | 24.7 |
| Treated hyperlipidemia § | 48.4 | 29.2 | 10.2 |
| Untreated hyperlipidemia § | 5.5 | 5.8 | 15.0 |
| No hyperlipidemia § | 46.0 | 65.1 | 74.8 |
Treated ED was defined as any use of phosphodiesterase inhibitors, papaverine or prostaglandin, untreated ED was defined as an IIEF-5 score of ≤16 and no evidence of ED drug treatment, while no ED was defined as an IIEF-5 score ≥17 and no evidence of ED drug treatment.
Variable names marked with bold were significantly different (P<0.05) across groups by the chisquare test of heterogeneity or Wald F test (for continuous variables); all estimates were weighted by the inverse of the probability of being sampled. Percents shown are column percents.
Any history of coronary artery bypass surgery or angioplasty, heart attack, angina, having a pacemaker, congestive heart failure, transient ischemic attack, stroke, carotid artery surgery, intermittent claudication, surgery or angioplasty for arterial disease of the leg, pulmonary embolism, aortic aneurysm, heart-rhythm disturbance, deep vein thrombosis, Reynaud's disease or peripheral vascular disease.
Treated hyperlipidemia was defined as taking prescription anti-lipid medication, untreated hyperlipidemia was measured serum total cholesterol of ≥240 mg/dL without taking prescription anti-lipid medication, and no hyperlipidemia was defined as no use of anti-lipid medications and total serum cholesterol <240.
Table 3.
Prevalence of use of medications by hyperlipidemia* and erectile dysfunction (ED)† status among men contributing blood samples in Boston Area Community Health Survey, 2002–2005, N=1899.
| Medicationsठ| Treated hyperlipidemia (n=290) % | Untreated hyperlipidemia (n=251) % | No hyperlipidemia (n=1358) % | Treated ED (n=40) % | Untreated ED (n=472) % | No ED (n=1387) % |
|---|---|---|---|---|---|---|
| Statins d e | 89.8 | 0 | 0 | 48.4 | 26.4 | 8.9 |
| Non-statin antilipemics e | 17.4 | 0 | 0 | 5.2 | 5.9 | 1.7 |
| Beta blockers d e | 30.8 | 1.7 | 6.2 | 13.4 | 25.1 | 5.3 |
| Calcium channel blockers d e | 19.7 | 4.1 | 3.6 | 13.9 | 14.1 | 3.9 |
| ACE inhibitors d e | 37.9 | 3.9 | 6.5 | 42.4 | 22.6 | 6.9 |
| Angiotensin II receptor agonists d | 6.2 | 0.8 | 0.9 | 4.1 | 3.2 | 1.2 |
| Loop diuretics d e | 5.6 | 0.2 | 1.3 | 2.3 | 6.6 | 0.6 |
| Thiazide diuretics d e | 12.7 | 2.9 | 4.2 | 1.0 | 9.6 | 4.4 |
| Miscellaneous diuretics d e | 6.0 | 0.7 | 0.6 | 0 | 3.0 | 1.1 |
| Any anti-hypertensive drug d e | 50.0 | 6.1 | 12.6 | 48.6 | 33.5 | 12.3 |
| SSRI anti-depressants e | 10.6 | 8.0 | 9.7 | 0.4 | 13.0 | 9.1 |
| Tricyclic anti-depressants e | 9.8 | 1.9 | 1.6 | 14.6 | 7.8 | 1.3 |
| Anti-psychotics e | 4.3 | 2.1 | 3.5 | 0.4 | 6.7 | 2.7 |
| Anti-ED drugs d e | 9.1 | 1.2 | 1.8 | 100 | 0 | 0 |
| Alpha blockers or 5-alpha reductasede inhibitors | 7.9 | 0.4 | 2.7 | 7.9 | 6.4 | 2.2 |
Treated hyperlipidemia was defined as taking prescription anti-lipid medication, untreated hyperlipidemia was measured serum total cholesterol of ≥240 mg/dL without taking prescription anti-lipid medication, and no hyperlipidemia was defined as no use of anti-lipid medications and total serum cholesterol <240.
Treated ED was defined as any use of phosphodiesterase inhibitors, papaverine or prostaglandin, untreated ED was defined as an IIEF-5 score of ≤16 and no evidence of ED drug treatment, while no ED was defined as an IIEF-5 score ≥17 and no evidence of ED drug treatment.
Estimates were weighted by the inverse of the probability of being sampled. Percents shown are column percents.
Variable names marked with bold were significantly different (P<0.05) across groups by the chisquare test of heterogeneity
represents statistical significance for hyperlipidemia comparison
represents statistical significance for ED comparison.
Table 5.
Prevalence of erectile dysfunction (ED)* by hyperlipidemia†, age and comorbidity status among men contributing blood samples in Boston Area Community Health Survey, 2002–2005, N=1899.
| Prevalence of ED (%‡) | |||||
|---|---|---|---|---|---|
| Subgroup | Total N | Overall | Treated hyperlipidemia | Untreated hyperlipidemia | No hyperlipidemia |
| Age <55 | 1291 | 14.1% | 39.5% | 3.9% | 13.5% |
| N with ED | 234 | 41 | 21 | 172 | |
|
| |||||
| Age 55+ | 608 | 38.1% | 47.4% | 29.7% | 34.0% |
| N with ED | 257 | 91 | 25 | 141 | |
|
| |||||
| Age <55 and CVD§ and/or diabetes | 239 | 23.1% | 60.7% | 3.8% | 13.0% |
| N with ED | 66 | 29 | 4 | 34 | |
|
| |||||
| Age <55, no CVD or diabetes | 1052 | 12.1% | 13.7% | 3.9% | 13.6% |
| N with ED | 168 | 12 | 17 | 139 | |
|
| |||||
| Age 55+ and CVD and/or diabetes | 267 | 51.4% | 52.8% | 50.4% | 49.9% |
| N with ED | 143 | 65 | 10 | 68 | |
|
| |||||
| Age 55+, no CVD or diabetes | 341 | 27.5% | 36.5% | 22.5% | 25.7% |
| N with ED | 114 | 25 | 15 | 73 | |
Erectile dysfunction was defined as an IIEF-5 score of ≤16.
Treated hyperlipidemia was defined as taking prescription anti-lipid medication, untreated hyperlipidemia was measured serum total cholesterol of ≥240 mg/dL without taking prescription anti-lipid medication, and no hyperlipidemia was defined as no use of anti-lipid medications and total serum cholesterol <240.
Prevalence percentages were weighted by the inverse of the probability of being sampled.
Any history of coronary artery bypass surgery or angioplasty, heart attack, angina, having a pacemaker, congestive heart failure, transient ischemic attack, stroke, carotid artery surgery, intermittent claudication, surgery or angioplasty for arterial disease of the leg, pulmonary embolism, aortic aneurysm, heart-rhythm disturbance, deep vein thrombosis, Reynaud's disease or peripheral vascular disease.
Table 6.
Odds ratios and 95% confidence intervals from multivariate logistic regression models for ED* and hyperlipidemia status† by age and comorbidity subgroups among men contributing blood samples in Boston Area Community Health Survey, 2002–2005, N=1899.
| Odds ratios for ED (95% confidence interval) | |||||
|---|---|---|---|---|---|
| Subgroup | N | Model | Treated hyperlipidemia | Untreated hyperlipidemia | No hyperlipidemia (referent) |
| Age <55 and CVD* and/or diabetes | 239 | 1‡ | 10.39 (3.25, 33.20) | 0.59 (0.12, 2.97) | 1.00 |
| 2§ | 10.65 (3.11, 36.45) | 0.40 (0.07, 2.22) | 1.00 | ||
|
| |||||
| Age <55, no CVD or diabetes | 1052 | 1¶ | 1.03 (0.36, 2.92) | 0.24 (0.10, 0.56) | 1.00 |
| 2§ | 1.02 (0.35, 3.02) | 0.24 (0.10, 0.57) | 1.00 | ||
|
| |||||
| Age 55+ and CVD and/or diabetes | 267 | 1∥ | 1.10 (0.48, 2.52) | 1.18 (0.30, 4.60) | 1.00 |
| 2§ | 1.04 (0.43, 2.55) | 1.10 (0.29, 4.14) | 1.00 | ||
|
| |||||
| Age 55+, no CVD or diabetes | 341 | 1** | 1.84 (0.76, 4.43) | 0.89 (0.23, 3.40) | 1.00 |
| 2§ | 1.84 (0.68, 5.02) | 0.85 (0.23, 3.15) | 1.00 | ||
Erectile dysfunction was defined as an IIEF-5 score of ≤16, while CVD was defined as any history of coronary artery bypass surgery or angioplasty, heart attack, angina, having a pacemaker, congestive heart failure, transient ischemic attack, stroke, carotid artery surgery, intermittent claudication, surgery or angioplasty for arterial disease of the leg, pulmonary embolism, aortic aneurysm, heart-rhythm disturbance, deep vein thrombosis, Reynaud's disease or peripheral vascular disease.
Treated hyperlipidemia was defined as taking prescription anti-lipid medication, untreated hyperlipidemia was measured serum total cholesterol of ≥240 mg/dL without taking prescription anti-lipid medication, and no hyperlipidemia was defined as no use of anti-lipid medications and total serum cholesterol <240.
Parsimonious model solution controlled for age, socioeconomic status, insurance status, physical activity, depression, alcohol use, and use of other CVD drugs and other drugs that contribute to ED.
Full model solution controlled for age, socioeconomic status, race/ethnicity, insurance, physical activity, body mass index category, depression, health status, pack-years smoking & use of CVD drugs & drugs that may cause ED.
Parsimonious model solution controlled for age, socioeconomic status, and use of other CVD drugs.
Parsimonious model solution controlled for age, socioeconomic status, body mass index category, depression, and use of other CVD drugs.
Parsimonious model solution controlled for age, socioeconomic status, depression, and use of other drugs that contribute to ED.
Figure 1.
Severity of erectile dysfunction, by age and hyperlipidemia treatment status.
Covariates
The choice of covariates was informed by prior analyses.17 Socioeconomic status (SES) was constructed as a function of standardized income and education variables for the Northeastern U.S.18 Body mass index (BMI) was calculated from interviewer-measured weight and height. Physical activity level was defined using the Physical Activity for the Elderly (PASE) scale.19 Persons reporting at least 5 of 8 symptoms on the abridged Center for Epidemiologic Studies Depression Scale were considered to have depression.20 Cardiovascular disease (CVD) was a composite variable (Table 1). Other comorbidities were defined as a `yes' response to “Have you ever been told by a health care provider that you have or had….?”.
Table 1.
Characteristics of those with treated, untreated and no hyperlipidemia* among men contributing blood samples in Boston Area Community Health Survey, 2002–2005, N=1899.
| Continuous covariates† | Treated hyperlipidemia (n=290) (Mean, Standard Error) | Untreated hyperlipidemia (n=251) (Mean, Standard Error) | No hyperlipidemia (n=1358) (Mean, Standard Error) |
|---|---|---|---|
| Age | 58.3 (1.0) | 44.9 (1.0) | 45.8 (0.5) |
| Median | 59.8 | 42.4 | 43.2 |
| Years education | 14.2 (0.4) | 14.5 (0.4) | 15.0 (0.2) |
| Total cholesterol (mg/dl) | 187.5 (4.1) | 268.0 (2.5) | 188.8 (1.2) |
| Categorical covariates† | Treated hyperlipidemia % | Untreated hyperlipidemia % | No hyperlipidemia % |
|---|---|---|---|
| Socioeconomic status | |||
| Low | 32.8 | 17.5 | 23.2 |
| Middle | 36.9 | 58.4 | 49.7 |
| High | 30.2 | 24.0 | 27.1 |
| Race/ethnicity | |||
| Black | 23.1 | 20.0 | 26.4 |
| Hispanic | 7.5 | 16.0 | 13.6 |
| White | 69.4 | 64.0 | 60.0 |
| Health insurance | |||
| Private | 67.5 | 69.3 | 65.9 |
| Public | 28.0 | 12.9 | 17.4 |
| None | 4.5 | 17.8 | 16.8 |
| Current smoker | |||
| Never | 31.8 | 37.5 | 49.8 |
| Former | 44.5 | 28.7 | 25.7 |
| Current | 23.7 | 33.7 | 24.5 |
| Alcohol use | |||
| None | 39.1 | 19.0 | 24.8 |
| <1/day | 41.2 | 34.4 | 41.0 |
| 1–2/day | 15.9 | 31.3 | 24.9 |
| 3+/day | 3.9 | 15.3 | 9.2 |
| Physical activity score (PASE) | |||
| Low (<100) | 40.8 | 21.3 | 23.1 |
| Medium (100–249) | 41.0 | 47.9 | 49.7 |
| High (250+) | 18.2 | 30.8 | 27.2 |
| BMI categories | |||
| <25.0 | 16.6 | 22.2 | 29.6 |
| 25.0–29.9 | 37.8 | 36.4 | 40.4 |
| 30.0+ | 45.6 | 41.4 | 29.9 |
| Cardiovascular disease ‡ | 46.0 | 12.7 | 15.6 |
| Hypertension | 58.2 | 16.4 | 21.7 |
| Diabetes (Type I and/or Type II) | 31.7 | 1.8 | 6.5 |
| Depression | 15.0 | 10.0 | 14.5 |
| Erectile dysfunction (IIEF-5 score ≤16) | 44.4 | 8.9 | 17.9 |
| Self-reported history of hyperlipidemia | 85.3 | 37.7 | 15.8 |
**Treated hyperlipidemia was defined as taking prescription anti-lipid medication, untreated hyperlipidemia was measured serum total cholesterol of ≥240 mg/dL without taking prescription anti-lipid medication, and no hyperlipidemia was defined as no use of anti-lipid medications and total serum cholesterol <240.
Variable names marked with bold were significantly different (P<0.05) across groups by the chisquare test of heterogeneity or Wald F test (for continuous variables). All estimates were weighted by the inverse of the probability of being sampled. Percents shown are column percents.
Any history of coronary artery bypass surgery or angioplasty, heart attack, angina, having a pacemaker, congestive heart failure, transient ischemic attack, stroke, carotid artery surgery, intermittent claudication, surgery or angioplasty for arterial disease of the leg, pulmonary embolism, aortic aneurysm, heart-rhythm disturbance, deep vein thrombosis, Reynaud's disease or peripheral vascular disease.
Participants were asked to gather all medications used in the past four weeks for label recording, and were asked if they were taking drugs for specific indications such as asthma. Medications were coded using a modified form of the American Hospital Formulary Service (AHFS) Drug Pharmacologic Therapeutic Classification System.21 22 We considered use of medications thought to exacerbate symptoms of ED23–25 and created a count variable (0, 1, 2+) that included any use of beta blockers, selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, anti-psychotics, and diuretics. Similarly, we created a three-level count variable for use of other CVD medications.
Analytic sample and statistical analysis
Of 2,301 men in BACH, 402 men were excluded for missing blood, leaving 1899 in the analysis sample. To account for design effects and to allow generalizability to the Boston, MA, population, all analyses were weighted by the inverse of the probability of selection, and conducted using SUDAAN (version 9.0.1).26, 27 Missing data were replaced by plausible values using 25 multiple imputations; <1% were missing overall except for ED, where 13.3% of values were imputed. The distribution of covariates was examined within hyperlipidemia status (treated, untreated and none) and ED status (treated, untreated, and none) and tests for significant differences (p<0.05) were conducted using the chi-squared test and the Wald test. Mean IIEF-5 score and standard errors within subgroups were also examined; due to low frequencies, statistical testing was not emphasized in all groups.
We used multivariate logistic regression models to quantify the association between hyperlipidemia status and ED (defined as an IIEF-5 score of ≤16 regardless of ED treatment) using adjusted odds ratios (ORs) and 95% confidence intervals (CIs). We built parsimonious models that controlled confounding of the hyperlipidemia-ED relationship and full models containing all covariates of interest (regardless of statistical significance). All models were backwards-selected and always adjusted for age. Confounders were identified using a change-in-estimate criterion28 with a 10% as a threshold for confounding. Because we had very large differences by age between treated and untreated hyperlipidemia making it difficult to properly adjust for age, we also ran separate models among older (55+) and younger men (<55). In exploratory models, we identified a significant statistical interaction term (p<0.01) between the presence of comorbidity (diabetes and CVD) and hyperlipidemia status among men aged <55; consequently, we present all models stratified by both age and diabetes/CVD status.
Results
Men excluded from the analysis sample for missing blood were not different from included men on self-reported health, depression, smoking status, diabetes, body mass index, and SES (all overall p>0.12) but were more likely to be older, to be black and to have CVD (all overall p<0.03). Men with imputed IIEF-5 scores were more likely to be older, to have fair/poor self-reported health, to be Hispanic, of low SES, and to have CVD (all overall p<0.04) but were not different on other variables above (all overall p<0.24). In the analysis sample, the overall prevalence of treated hyperlipidemia was 14.8%, while 13.0% of the sample had untreated hyperlipidemia and 72.2% had no hyperlipidemia. The prevalence of treated ED was 2.8%, while 18.8% had untreated ED (IIEF-5 score ≤16 and no use of ED medications) and 78.4% had no ED by our definition (IIEF-5 score of 17+). The characteristics of men by hyperlipidemia status and ED status are presented in Tables 1 and 2, respectively. There were substantial age differences by hyperlipidemia status (Table 1), while men with treated or untreated ED were older than men without ED (means of 52.6 and 55.3 vs. 45.5 years, respectively) (Table 2). Socioeconomic differences were stronger considering ED status compared to hyperlipidemia status, while the treated hyperlipidemia and treated ED groups had the highest proportion of white men. Men with treated or untreated hyperlipidemia were more likely to have a BMI ≥30 compared to men without hyperlipidemia, while BMI category was not related to ED status.
Men with treated hyperlipidemia were more than twice as likely to report CVD, erectile dysfunction, hypertension, and diabetes compared to men with no hyperlipidemia or men with untreated hyperlipidemia (Table 1) and accordingly, were much more likely to use cardiovascular and antihypertensive medications (Table 3). Men with untreated hyperlipidemia reported a generally lower proportion of comorbidities and had lower use of medications compared to men without hyperlipidemia. Men with ED (treated or untreated) had higher proportions of all comorbidities in Table 2 and used more medications compared to men without ED (Table 3). In this comparison, differences were especially pronounced for statins, beta blockers, ACE inhibitors, and calcium channel blockers.
Table 4 shows mean erectile function scores (IIEF-5) within strata of age and hyperlipidemia status. IIEF-5 scores declined from 21.9 among those aged 30–39 to 14.9 among those aged 70–79 (p<0.001), indicating poorer function with increasing age. The mean for all ages among those treated for hyperlipidemia (17.0) was lower than those with untreated hyperlipidemia (21.6) and no hyperlipidemia (20.6) (p<0.001). Among the two youngest age groups, there were larger differences in mean score between men treated for hyperlipidemia and men without hyperlipidemia compared to the older age groups, with the most marked difference by treatment status among men 30–39 (13.7 among treated vs. 22.1 among those with no hyperlipidemia, p<0.001). At every age group, men with untreated hyperlipidemia had higher mean IIEF-5 scores than men without hyperlipidemia. Although there were few men treated with statins plus another class of anti-lipemics (n=14), these men had the lowest mean score (13.5) compared to 32 men treated with non-statin anti-lipemics only (19.5) (data not shown), or statins only (17.0).
Table 4.
Mean (standard error) IIEF-5 score for erectile dysfunction by age group and hyperlipidemia status* among men contributing blood samples in the Boston Area Community Health Survey, 2002–2005, N=1899.
| Age group | Total | Treated hyperlipidemia (any treatment)* | Treated with statins‡ only | Untreated hyperlipidemia | No hyperlipidemia |
|---|---|---|---|---|---|
| Mean† (SE) | Mean† (SE) | Mean† (SE) | Mean† (SE) | Mean† (SE) | |
| Total | 20.2 (0.2) | 17.0 (0.6) | 17.0 (0.6) | 21.6 (0.4) | 20.6 (0.2) |
| N | 1899 | 290 | 244 | 251 | 1358 |
|
| |||||
| 30–39 | 21.9 (0.3) | 13.7 (2.4) | 15.3 (2.9) | 22.5 (0.6) | 22.1 (0.2) |
| N | 512 | 11 | 7 | 72 | 429 |
|
| |||||
| 40–49 | 21.0 (0.2) | 19.3 (0.9) | 19.1 (0.9) | 22.3 (0.5) | 21.0 (0.3) |
| N | 554 | 62 | 54 | 86 | 406 |
|
| |||||
| 50–59 | 19.4 (0.5) | 18.1 (1.0) | 17.7 (1.2) | 20.2 (1.0) | 19.6 (0.6) |
| N | 436 | 81 | 65 | 55 | 300 |
|
| |||||
| 60–69 | 17.6 (0.6) | 16.7 (0.9) | 16.6 (1.0) | 18.9 (1.5) | 18.1 (0.8) |
| N | 260 | 91 | 77 | 27 | 142 |
|
| |||||
| 70–79 | 14.9 (0.8) | 15.2 (1.3) | 15.5 (1.4) | 16.4 (2.8) | 14.5 (1.0) |
| N | 137 | 45 | 41 | 11 | 81 |
Treated hyperlipidemia was defined as taking prescription anti-lipid medication, untreated hyperlipidemia was measured serum total cholesterol of ≥240 mg/dL without taking prescription anti-lipid medication, and no hyperlipidemia was defined as no use of anti-lipid medications and total serum cholesterol <240.
All means were weighted by the inverse of the probability of being sampled.
Statins were atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, or simvastatin.
We also examined severity of ED by hyperlipidemia treatment status (Figure 1). Overall, the prevalence and severity of ED increased with age; however, this pattern was not consistent by treatment status. Men aged 30–39 with treated hyperlipidemia had a higher prevalence of moderate or severe ED (58.8%) compared to men in the same age group who had untreated hyperlipidemia or no hyperlipidemia (1% and 2.7% had moderate or severe ED, respectively). Compared to men with untreated hyperlipidemia and no hyperlipidemia, men with treated hyperlipidemia had a greater prevalence of moderate or severe ED at every age group except 70–79.
Table 5 shows the prevalence of ED (combining mild to moderate, moderate and severe ED) by age and presence of CVD and/or diabetes by hyperlipidemia treatment status. Of all strata, the highest prevalence of ED was among men <55 who were being treated for hyperlipidemia (60.7%) and had CVD disease and/or diabetes. Among those 55+ who had CVD and/or diabetes, the prevalence of ED did not differ by hyperlipidemia status. Table 6 shows estimated ORs and 95% CIs for ED by hyperlipidemia status using logistic regression models. Among those aged <55 with diabetes and/or CVD, we observed a large OR for ED comparing treated hyperlipidemia to no hyperlipidemia (Model 1: OR=10.39, 95% CI: 3.25, 33.20). Although confidence intervals were imprecise, they excluded 1.00 and the association was persistent across modeling strategies. Considering those <55 without CVD or diabetes, there was no association for treated hyperlipidemia in any models but we observed an inverse association that persisted across modeling strategies between untreated hyperlipidemia and ED (Model 1: OR= 0.24, 95% CI: 0.10, 0.56). Considering those aged 55+ with diabetes and/or CVD, we saw no association between treated or untreated hyperlipidemia and ED in any model. Finally, among those age 55+ without CVD or diabetes, there were elevated ORs for treated hyperlipidemia and ED but confidence intervals included 1.00 (Model 1: OR=1.84, 95% CI: 0.76, 4.43), while ORs for untreated hyperlipidemia showed no association (Model 1: OR=0.89, 95% CI: 0.23, 3.40).
To consider whether the observed association between treated hyperlipidemia and ED among younger men with chronic illness would change if the analysis was restricted to particular anti-lipemic drug classes, we reran our Model 1s excluding those 46 men who were not exclusively using statins. In this statins-only analysis, the OR for treated hyperlipidemia was still substantial (OR=8.86, 95% CI: 2.69, 29.20), while the other estimates for treated hyperlipidemia remained statistically insignificant. The inverse association between untreated hyperlipidemia and ED among men aged <55 with no diabetes or CVD was unchanged in the statins-only analysis (OR=0.24, 95% CI=0.10, 0.56).
DISCUSSION
We examined the characteristics of men with treated and untreated hyperlipidemia, and estimated the association between use of lipid-lowering medications and ED, as well as the association between untreated hyperlipidemia and ED (compared to men without ED) in a population-based sample of community-dwelling men. We observed that men taking lipid-lowering drugs had lower mean erectile function scores compared to men with untreated hyperlipidemia and no hyperlipidemia. However, men on hyperlipidemia drug treatment were more likely to have comorbidities and take relevant medications, suggesting confounding by other risk factors for ED. In multivariate analyses that included other risk factors, we observed a large association between use of lipid-lowering medications and erectile dysfunction but only among men who were <55 and had diabetes and/or CVD. We were unable to examine all of our classes of lipid-lowering medications due to sample size, but repeating this analysis among those taking only statins did not change our conclusions. It is important to note that this result was based on relatively small numbers in the hyperlipidemia treatment group (n=60), as reflected in the imprecise confidence interval. Finally, our multivariate results suggest lipid-lowering medications were not independently associated with ED among older men (55+), with or without comorbidities.
Our results are novel in that we find an association of lipid-lowering medications and ED only among younger men with comorbidities. In this group, we further considered whether testosterone levels were lower among men with ED on anti-lipemics compared to treated men without ED, but this was not explanatory (data not shown). Despite our multivariate adjustment including adjustment for additional medications for CVD as a proxy for CVD severity, we cannot rule out that the association we observed in this group could be due to interactions with other medications, or confounding by severity of pre-existing hyperlipidemia, ED, or other co-morbid disease as the severity of these at drug initiation was unknown. Because younger men with comorbidities who are prescribed anti-lipemics may be more mindful of their disease at a time when their peers may be healthier, they may have more of the psychological covariants that negatively affect sexual function. However, the possibility of a lipid-lowering drug effect among younger, sicker men should not be dismissed, and could be addressed in future clinical trials. Clinical trials of statins have not reported ED as an adverse event, except one that found no statistically significant difference in reporting between treatment and placebo.29 Other authors have pointed out that ED is generally underreported and patients in trials were not specifically queried about ED.11 A prior longitudinal study of men with existing cardiovascular risk factors found that statin initiation caused median IIEF-5 scores to fall from 21.0 to 6.5 at evaluation six months later. Although these men were generally older than BACH participants (mean age 61), the results support our findings by suggesting that statins may have a greater adverse impact on ED among men with comorbidities.12 A clinical study of younger men that excluded those with CVD and diabetes but matched on other risk factors found an increased association of statins with ED (OR=1.46, 95% CI: 1.27, 1.68).30 In contrast, a clinical trial of atorvastatin to improve lower urinary tract symptoms and benign prostatic enlargement among men aged 50+ included two questions from the IIEF but concluded there was no impact of atorvastatin on erectile function compared to placebo after 26 weeks.31 A small study of 74 hyperlipidemic men receiving atorvastatin reported a trend towards improvement in IIEF score over one year; however the difference in score from baseline was small (<2) and there was no comparison group.32 Prior epidemiologic studies have not found statins to be associated with ED in longitudinal33 or cross-sectional analyses,25 although the proportion of subjects taking statins in these studies was small.
We did not observe an independent effect of untreated hyperlipidemia on ED compared to men without hyperlipidemia, rather; we observed that younger men (<55) with untreated hyperlipidemia reported significantly less ED than men with no hyperlipidemia. While this finding remains unexplained, we note small numbers in this subgroup, and do not suggest that untreated hyperlipidemia could potentially reduce the risk of erectile dysfunction. Men in this group were not severely hyperlipidemic; it is possible that hyperlipidemia may take many years to induce the endothelial dysfunction thought to be related to ED. Supporting this is the observation that the “protective effect” of untreated hyperlipidemia was only observed among those <55.
Strengths of our study include a racially/ethnically and socioeconomically diverse sample of a broad age range, for whom comorbidities and medication information were systematically collected. We captured ED using a validated scale34 and had the ability to consider use of other medications. Study limitations are also present. We had missing data for ED, although were able to use other information to impute ED status. In addition, we had small numbers in some subgroups, which led to imprecise confidence intervals. We did not collect a fasting blood sample, which may have caused misclassification of our untreated hyperlipidemia group, where we were relying on serum measures alone. In our study, there were differences in the characteristics of those giving a blood sample versus not, and the observed proportion of men who had high cholesterol as measured in serum and/or who were using lipid-lowering medications was 27.8%. However, this proportion is similar to that observed in the National Health Examination and Nutrition Survey (1999–2000): 24.9% for men aged 20–75.35 In this cross-sectional analysis, we were unable to determine the severity of hyperlipidemia or the presence of ED before treatment, but when we excluded men on multiple types of hyperlipidemia treatment (a potential proxy for severity) our conclusions remained unchanged. Similarly, we were not able to control the severity of CVD, although we included current use of CVD medications as a severity proxy and we were able to consider variables other than lipids included in the validated Framingham coronary heart disease risk score (age, smoking, diabetes (self-reported) and blood pressure (self-reported).36, 37 We do not capture recommendations for lifestyle changes as treatment for hyperlipidemia; our analysis only includes drug treatments. Because lipid-lowering medications are specific for hyperlipidemia, we do not feel we have overestimated the proportion treated with drugs, however. Finally, we have previously studied the effects of statins on testosterone in this population, and concluded there was no effect that was independent of comorbidity and body size, suggesting that statins are not inducing ED via reduction of testosterone.38
CONCLUSION
Our results add to the available evidence that suggests that lipid-lowering agents, including statins, may be associated with erectile dysfunction among certain men (in our analysis, these were men <55 with CVD and/or diabetes), but our overall results may be reassuring for older men both with and without comorbidities, in whom no association was found in multivariate analyses. Given available treatments for erectile dysfunction and the body of clinical evidence for statins' reduction of major coronary events, all-cause mortality and other outcomes,39 adverse effects of statins should always be weighed against the well-established benefits. The body of available evidence suggests that hyperlipidemia itself is an important part of the increased global cardiometabolic risk profile9 and when present in patients with ED should prompt management with diet and exercise as well as appropriate pharmacotherapy. Research is on-going to determine whether timely identification and aggressive treatment of ED and hyperlipidemia will lower cardiovascular morbidity and mortality.
Acknowledgements
The authors would like to thank Amy B. O'Donnell, Gretchen R. Esche and Andre B. Araujo for assistance in the preparation of the manuscript.
Footnotes
Conflict of interest: Susan A. Hall is a former employee of GlaxoSmithKline and a former consultant to GlaxoSmithKline but has no equity interest in GlaxoSmithKline. Raymond Rosen is a consultant to, and investigator for Eli Lilly, Bayer Schering Pharma, and Pfizer. Martin Miner is a consultant to GlaxoSmithKline and has received funds for research from GlaxoSmithKline and Indevus. Peter Ganz has received speaker fees, fees for consulting and funds for research from Pfizer, and fees for consulting from GlaxoSmithKline. All other authors have no conflict of interest.
REFERENCES
- 1.IMS Health Incorporated Top 10 Therapeutic Classes by U.S. Sales. 2007;2008 [Google Scholar]
- 2.IMS Health Incorporated . IMS Health Reports 5.4 Percent Dollar Growth in 2005 U.S. Prescription Sales Forbes. Vol. 2008. IMS Health Incorporated; Norwalk: 2006. [Google Scholar]
- 3.IMS Health Incorporated . IMS Reports 5% Growth in Retail Pharmacy Drug Sales for the 12 Months to December 2006. Vol. 2008. IMS Health Incorporated; 2007. [Google Scholar]
- 4.Slone Epidemiology Center . Patterns of Medication Use in the United States, 2006: A Report from the Slone Survey. Vol. 2008. Boston University; 2006. [Google Scholar]
- 5.American Society of Health-System Pharmacists . HMG-CoA Reductase Inhibitors. In: GK M, editor. AHFS Drug Information 2006. American Society of Health-System Pharmacists, Inc.; Bethesda: 2006. p. 1674. [Google Scholar]
- 6.Mulhall J, Teloken P, Brock G, Kim E. Obesity, dyslipidemias and erectile dysfunction: a report of a subcommittee of the sexual medicine society of North America. J Sex Med. 2006;3:778–86. doi: 10.1111/j.1743-6109.2006.00286.x. [DOI] [PubMed] [Google Scholar]
- 7.Ferrer E, Moral MA, Bozzo J. The role of statins in erectile dysfunction. Drugs Today (Barc) 2007;43:55–9. doi: 10.1358/dot.2007.43.1.1062672. [DOI] [PubMed] [Google Scholar]
- 8.Vrentzos GE, Paraskevas KI, Mikhailidis DP. Dyslipidemia as a risk factor for erectile dysfunction. Curr Med Chem. 2007;14:1765–70. doi: 10.2174/092986707781058931. [DOI] [PubMed] [Google Scholar]
- 9.Miner M, Billups KL. Erectile dysfunction and dyslipidemia: relevance and role of phosphodiesterase type-5 inhibitors and statins. J Sex Med. 2008;5:1066–78. doi: 10.1111/j.1743-6109.2008.00783.x. [DOI] [PubMed] [Google Scholar]
- 10.Carvajal A, Macias D, Sainz M, et al. HMG CoA reductase inhibitors and impotence: two case series from the Spanish and French drug monitoring systems. Drug Saf. 2006;29:143–9. doi: 10.2165/00002018-200629020-00004. [DOI] [PubMed] [Google Scholar]
- 11.Rizvi K, Hampson JP, Harvey JN. Do lipid-lowering drugs cause erectile dysfunction? A systematic review. Fam Pract. 2002;19:95–8. doi: 10.1093/fampra/19.1.95. [DOI] [PubMed] [Google Scholar]
- 12.Solomon H, Samarasinghe YP, Feher MD, et al. Erectile dysfunction and statin treatment in high cardiovascular risk patients. Int J Clin Pract. 2006;60:141–5. doi: 10.1111/j.1742-1241.2006.00793.x. [DOI] [PubMed] [Google Scholar]
- 13.McKinlay JB, Link CL. Measuring the Urologic Iceberg: Design and Implementation of the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52:389–96. doi: 10.1016/j.eururo.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 15.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–5. [PubMed] [Google Scholar]
- 16.Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Pena BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 17.Kupelian V, Link CL, McKinlay JB. Association between smoking, passive smoking, and erectile dysfunction: results from the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52:416–22. doi: 10.1016/j.eururo.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green LW. Manual for scoring socioeconomic status for research on health behavior. Public Health Rep. 1970;85:815–27. [PMC free article] [PubMed] [Google Scholar]
- 19.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 20.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11:139–48. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- 21.Kelley KE, Kelley TP, Kaufman DW, Mitchell AA. The Slone Drug Dictionary: A research driven pharmacoepidemiology tool. Pharmacoepidemiol Drug Safety. 2003;12:168–9. [Google Scholar]
- 22.American Society of Health-System Pharmacists . AHFS Drug Information. American Society of Health-System Pharmacists, Inc.; Bethesda: 2007. [Google Scholar]
- 23.Francis ME, Kusek JW, Nyberg LM, Eggers PW. The contribution of common medical conditions and drug exposures to erectile dysfunction in adult males. J Urol. 2007;178:591–6. doi: 10.1016/j.juro.2007.03.127. discussion 596. [DOI] [PubMed] [Google Scholar]
- 24.Rosen RC, Marin H. Prevalence of antidepressant-associated erectile dysfunction. J Clin Psychiatry. 2003;64(Suppl 10):5–10. [PubMed] [Google Scholar]
- 25.Ricci E, Parazzini F, Mirone V, et al. Current drug use as risk factor for erectile dysfunction: results from an Italian epidemiological study. Int J Impot Res. 2003;15:221–4. doi: 10.1038/sj.ijir.3901008. [DOI] [PubMed] [Google Scholar]
- 26.Cochran W. Sampling Techniques. John Wiley and Sons; New York, NY: 1977. [Google Scholar]
- 27.Research Triangle Institute . SUDAAN Language Manual Release 9.0. Research Triangle Park, NC: 2004. [Google Scholar]
- 28.Rothman KJ, Greenland S. Modern Epidemiology. Second Edition Lippincott-Raven Publishers; Philadelphia: 1998. pp. 256–7. [Google Scholar]
- 29.Pedersen TR, Faergeman O. Simvastatin seems unlikely to cause impotence. Bmj. 1999;318:192. doi: 10.1136/bmj.318.7177.192a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruckert E, Giral P, Heshmati HM, Turpin G. Men treated with hypolipidaemic drugs complain more frequently of erectile dysfunction. J Clin Pharm Ther. 1996;21:89–94. doi: 10.1111/j.1365-2710.1996.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 31.Mills IW, Crossland A, Patel A, Ramonas H. Atorvastatin treatment for men with lower urinary tract symptoms and benign prostatic enlargement. Eur Urol. 2007;52:503–9. doi: 10.1016/j.eururo.2007.02.032. [DOI] [PubMed] [Google Scholar]
- 32.Dogru MT, Basar MM, Simsek A, et al. Effects of statin treatment on serum sex steroids levels and autonomic and erectile function. Urology. 2008;71:703–7. doi: 10.1016/j.urology.2007.11.059. [DOI] [PubMed] [Google Scholar]
- 33.Derby CA, Barbour MM, Hume AL, McKinlay JB. Drug therapy and prevalence of erectile dysfunction in the Massachusetts Male Aging Study cohort. Pharmacotherapy. 2001;21:676–83. doi: 10.1592/phco.21.7.676.34571. [DOI] [PubMed] [Google Scholar]
- 34.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 35.Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation. 2003;107:2185–9. doi: 10.1161/01.CIR.0000066320.27195.B4. [DOI] [PubMed] [Google Scholar]
- 36.D'Agostino RB, Sr., Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 37.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 38.Hall SA, Page ST, Travison TG, Montgomery RB, Link CL, McKinlay JB. Do statins affect androgen levels in men? Results from the Boston area community health survey. Cancer Epidemiol Biomarkers Prev. 2007;16:1587–94. doi: 10.1158/1055-9965.EPI-07-0306. [DOI] [PubMed] [Google Scholar]
- 39.Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]