Abstract
Background
First-generation highly cross-linked polyethylene liners have reduced the incidence of wear particle-induced osteolysis. However, failed acetabular liners have shown evidence of surface cracking, mechanical failure, and oxidative damage. This has led to the development of second-generation highly cross-linked polyethylene, which has improved wear and mechanical properties and resistance to oxidation in vitro. Owing to its recent introduction, there are no publications describing its clinical performance.
Questions/purposes
We assessed early clinical wear of a second-generation highly cross-linked polyethylene liner and compared its clinical performance with the published results of hip simulator tests and with first-generation highly cross-linked polyethylene annealed liners.
Patients and Methods
Twenty-one patients were enrolled in a prospective cohort study. Clinical outcome and femoral head penetration were measured for 19 patients at 6 months and 1 and 2 years postoperatively.
Results
The median proximal head penetration was 0.009 mm and 0.024 mm at 1 and 2 years, respectively. The median two-dimensional (2-D) head penetration was 0.083 mm and 0.060 mm at 1 and 2 years, respectively. The median proximal wear rate between 1 and 2 years was 0.015 mm/year.
Conclusions
The wear rate calculated was similar to the in vitro wear rate reported for this material; however, it was less than the detection threshold for this technique. Although longer followup is required for wear to reach a clinically quantifiable level, this low level of wear is encouraging for the future clinical performance of this material.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Component loosening is the most common reason for early to midterm revision of hip prostheses [2, 27]. A major contributor to the loosening observed at revision arthroplasty is osteolysis related to wear of UHMWPE [10, 17, 18, 23, 26, 40, 45, 46]. To overcome the problems of wear associated with conventional UHMWPE, highly cross-linked polyethylene (HXLPE) was introduced [11]. The first-generation HXLPEs in clinical use have exhibited markedly less wear than conventional UHMWPE [12, 14, 28, 30, 31]; however, there have been some reports of surface cracking, mechanical failure, and oxidative damage in failed acetabular liners [5, 22, 25].
The reduced mechanical properties of first-generation HXLPE can be attributed to the process of cross-link formation, which is achieved by irradiation and heating of the polyethylene [16, 37]. Materials that are heated above their melting temperature (remelted) have reduced fatigue strength [41, 42] owing to alteration of the material’s crystalline structure [38]. Heating to just below the melting point (annealing) maintains the mechanical properties of the material; however, the ability to eliminate free radicals using this technique is reduced as a consequence of their limited mobility in the polymer, which increases the propensity for late oxidative damage to the material [42, 43]. To improve the efficiency of free radical elimination, a new process of sequential irradiation and annealing has been introduced in a new second-generation material X3™ (Stryker Orthopaedics, Mahwah, NJ). A hip simulator study has shown, in addition to excellent mechanical properties, acetabular liners made from this material have superior wear properties in comparison to conventional UHMWPE and clinically successful first-generation HXLPE [16].
Unfortunately, the ability to translate positive findings from hip simulator studies to equally good results clinically has proven challenging [29, 32, 39]. This highlights the importance of confirming the safety and wear performance of new materials in clinical studies using a sensitive evaluation technique. There is currently no published data describing the clinical performance of the second-generation highly cross-linked polyethylene X3™ acetabular liner. Therefore, we assessed the early clinical wear properties of the X3™ liner using radiostereometric analysis (RSA) to compare its clinical performance with the results of hip simulator tests and with those of first-generation annealed acetabular liners. We hypothesize the X3™ liner will have a clinical wear rate similar to that reported from hip simulator tests and less than that reported for first-generation annealed acetabular liners.
Patients and Methods
We recruited a prospective consecutive series of 21 patients with osteoarthritis of their hip for the trial. Inclusion criteria were the consultant surgeon selecting cementless components with the Trident® acetabular system (Stryker Orthopaedics) matched with an X3™ acetabular liner (Stryker Orthopaedics) as the preferred choice of implant and surgery scheduled at the Calvary Wakefield Hospital, which is equipped for RSA. Ethics approval was obtained for this study from the Wakefield Hospital ethics committee. All patients provided informed consent for the insertion of tantalum markers during surgery and the subsequent RSA radiographs. Exclusion criteria were residence outside the metropolitan area, abnormal gross anatomy of the hip, age older than 80 years, and inflammatory arthritis or severe osteoporosis. Two patients were excluded from the study owing to incomplete RSA evaluation at 12 months. Therefore, 19 patients were included in the study (10 men, nine women). Their median age was 63 years (range, 47–76 years); median male weight was 84 kg (range, 72–100 kg) and median female weight was 71 kg (range, 60–78 kg). Sixteen patients were Charnley grade A and three were Charnley grade B. The mean cup size was 54.6 mm (range, 48–62 mm). The mean inclination was 45.6º (range, 39°–58º).
All patients had a hemispheric, porous-coated, metal-backed shell (Trident® acetabular system) implanted with a HXLPE liner (X3™). The cross-link formation process of the liner involved three cycles of sequential irradiation and annealing. Each cycle consisted of gamma irradiation at a dose of 3 Mrad followed by annealing at 130°C for 8 hours [16]. The total cumulative radiation dose was 9 Mrad. Terminal sterilization was achieved through a gas plasma process. All patients received a cementless femoral stem (Accolade®; Stryker Orthopaedics) with a 32-mm cobalt-chromium femoral head.
Six tantalum markers (1.0-mm diameter; RSA Biomedical, Umeå, Sweden) were placed in the outer rim of the polyethylene liner at the time of surgery. Baseline RSA examinations were performed within 7 days of surgery and again at 6 months and 1 and 2 years postoperatively. Examinations were taken with each patient in a supine position. Bragdon et al. [8] and von Schewelov et al. [50] reported no statistical difference between the wear measurements made from standing and supine RSA radiographs; therefore, patients in our study were examined in the supine position.
A ceiling-mounted radiographic tube and a mobile radiographic tube were used simultaneously to take exposures of the hip with a calibration cage (Number 43; RSA Biomedical). Wear was measured by penetration of the femoral head inside the polyethylene liner with UmRSA® software (v6.0; RSA Biomedical). The program identifies the center of the outer ellipse of the femoral head and acetabular cup with an edge detection algorithm used in conjunction with tantalum markers placed in the outer rim of the polyethylene liner. This combined measurement technique using edge detection in conjunction with marker beads was proven to have the highest precision clinically in a study by Borlin et al. [4] with a conservative detectable limit for measuring wear of 80 μm.
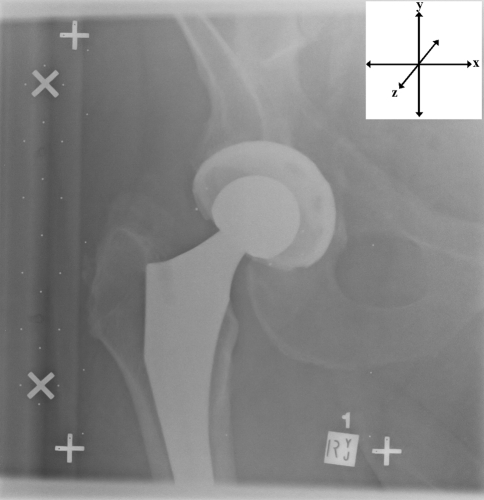
Femoral head penetration into the polyethylene was calculated in three separate ways to enable comparison to other in vitro and in vivo studies. First, proximal head penetration was calculated from translations along the y axis (Fig. 1). Second, the amount of 2-D head penetration was calculated as the vectorial sum of medial-lateral (x axis) and proximal-distal (y axis) migrations. Third, the amount of 3-D head penetration was calculated as the vectorial sum of medial-lateral, proximal-distal, and anterior-posterior (z axis) migrations. These measurements of femoral head penetration used the immediate postoperative radiograph as a baseline and therefore included “bedding-in” of the femoral head. The penetration recorded after 1 year was identified as true wear of the polyethylene liner, and consequently, the proximal wear rate was calculated between 1 and 2 years. Median wear rate was calculated as the difference in head penetration between 1 and 2 years for each individual.
Fig. 1.
A postoperative RSA radiograph of a right hip is shown, with an inset illustrating the three axes used to measure head penetration. Positive x-axis translations represent medial head penetration; positive y-axis translations represent proximal head penetration; and positive z-axis translations represent anterior head penetration.
To document that this series of patients achieved a typical outcome with usual physical activity after TKA, clinical outcome was measured using Oxford Hip and SF-12 scores recorded preoperatively and postoperatively.
Sample size was based on a power calculation made using the Altman normogram [1, 52]. Previous RSA studies [22, 41] showed wear of conventional polyethylene of 0.1 to 0.085 mm and a standard deviation less than 0.07. RSA studies on cross-linked polyethylenes support in vitro observations that wear would be less than the detection threshold of 0.80 mm. A power calculation indicated a total of less than 20 subjects was required to detect a target difference of less than 50% wear compared with published results of noncross-linked polyethylene (α = 0.05, β = 0.9). A post hoc power calculation [33, 52] with 2-year results showed a β value greater than 90% for vertical, 2-D, and 3-D wear. Changes in clinical outcomes scores assessed preoperatively and at 1 year followup were compared using the Wilcoxon’s matched pairs signed-ranks test. Significance was set at p = 0.05.
Results
There were no mechanical failures or reoperations in any of the patients. All patients showed improvement in preoperative and 1-year postoperative clinical scores (p < 0.5, Wilcoxon’s matched pairs signed-ranks test). Oxford Hip Score improved from a preoperative median of 36 (range, 26–54) to a postoperative median of 18 (range, 12–30). The median preoperative SF-12 scores for pain and motivation were 30 (range, 21–43) and 42 (range, 31–61), respectively. Postoperatively, the median SF-12 scores for pain and motivation were 39 (range, 25–56) and 52 (range, 34–65), respectively. SF-12 scores were comparable to those of age-matched population normals [3]: in subjects aged 55 to 64 years, the mean physical component is 46.7 (range, 45.4–48.0) and the mean mental component is 53.4 (range, 52.4–54.5).
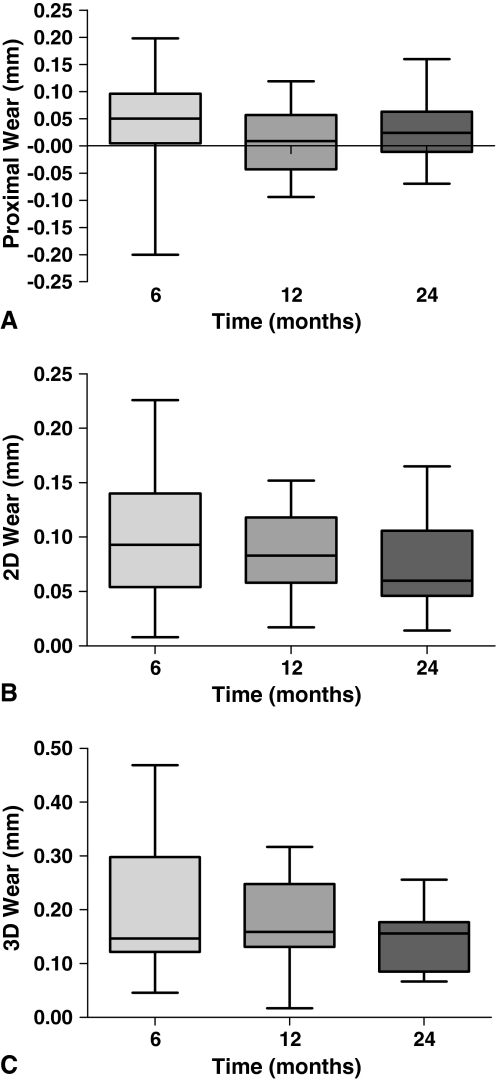
Femoral head penetration was observed during the initial 6 months, which plateaued with minimal wear at 1 and 2 years of followup. The median proximal head penetrations were 0.009 mm (range, −0.094–0.119 mm; SD, 0.063 mm) and 0.024 mm (range, −0.070–0.160 mm; SD, 0.061 mm) at 1 and 2 years, respectively (Fig. 2A). The median proximal wear rate calculated between 1 and 2 years was 0.015 mm/year. The median 2-D head penetration showed most of the migration occurred during the first 12 months. The median 2-D head penetrations were 0.083 mm (range, 0.017–0.152 mm; SD, 0.040 mm) at 1 year and 0.060 mm (range, 0.014–0.165 mm; SD, 0.040 mm) at 2 years (Fig. 2B). The median 2-D wear rate between 1 and 2 years was 0.009 mm/year. The median 3-D head penetrations were 0.159 mm (range, 0.017–0.317 mm; SD, 0.080 mm) and 0.156 mm (range, 0.067–0.256 mm; SD, 0.059 mm) at 1 and 2 years, respectively (Fig. 2C). The median 3-D wear rate between 1 and 2 years was −0.043 mm/year.
Fig. 2A–C.
Box-and-whisker plots show (A) proximal, (B) 2-D, and (C) 3-D head penetration measured at 6, 12, and 24 months. Horizontal bar = median; box = upper and lower quartiles; error bars = range.
Discussion
As a consequence of its recent introduction to clinical use, there currently are no publications describing the clinical wear properties of the X3™ acetabular cup insert. One hip simulator study reports the in vitro wear of this insert [16], and therefore our purpose was to compare these in vitro wear results with those after clinical use during a 2-year period. Furthermore, as this is the first report of the clinical wear characteristics of a second-generation HXLPE acetabular liner, we were interested in comparing the results from this study with literature reports of first-generation annealed highly cross-linked UHMWPE liners. We hypothesized the findings of this study would be consistent with the in vitro wear results and show clinical wear comparable or less than wear for first-generation HXLPE liners.
The high sensitivity of the RSA measurement technique, in conjunction with the ability to extrapolate results of short-term average linear wear rate to the average long-term linear wear rate for a population, makes this a useful tool for screening newly introduced prostheses [13, 29, 49]. Despite this, the RSA technique has limitations in accuracy and precision [4, 7, 51] that make it challenging to measure very small amounts of wear that are less than the detection threshold. In an optimal experimental setup, the accuracy of RSA is reported to range from 0.022 mm to 0.086 mm depending on the vector direction [7]. Our study is further limited in that no measurement of precision was made for this data set. The precision of our results should be similar to those validated previously for the combined liner and marker technique [4].
Dowd et al. [15] reported a linear increase in true wear with time is characteristic of polyethylene acetabular liners. However, we measured an uncharacteristic pattern of proximal femoral head penetration in that numerous patients had negative wear, particularly within the first year of the study. This finding has been reported previously [6, 20, 34–36] and is a result of femoral head penetration measurements lying within the accuracy limit of the technique and therefore being outside the limit of detection. The migration calculated between 1 and 2 years represents the actual rate of wear, but the numerical value of this should be interpreted with caution as it also lies within the detection threshold of the RSA technique.
The calculation of annual wear in this study was based only on wear that occurred between 1 and 2 years. Although the amount of head penetration was recorded at three times, the measurements were relative to the immediate postoperative radiographs and consequently included the initial creep and bedding-in of the liner. Studies have shown the majority of bedding-in occurs within 2.5 million cycles [21], which usually is complete after approximately 1 year [47]. This being the case, only wear measured between the first and second years was considered true wear. This is supported by the findings of Glyn-Jones et al. [24] in an RSA study of the creep and wear characteristics of HXLPE. They concluded femoral head penetration within the first 6 months was dominated by creep whereas penetration after 1 year was virtually all attributable to wear.
In the only published hip simulator study comparing the X3™ liner with conventional UHMWPE and a first-generation annealed HXLPE liner (Crossfire®; Stryker Orthopaedics), the X3™ liners had a markedly lower wear rate than the conventional and first-generation HXLPE liners [16]. Based on their findings, Dumbleton et al. [16] predicted the clinical wear rate of the X3™ liners should be 14 μm/year. The wear rate of 15 μm/year of median proximal wear measured in our study between 1 and 2 years is consistent with the predicted wear rate of 14 μm/year but should be considered a serendipitous result as this amount of wear is within the limits of accuracy for RSA and is not valid at this time. If we assume a conservative detectable limit for measuring wear of 80 μm, which is consistent with the precision measurements reported by Borlin et al. [4] for this technique (68 μm, 98 μm, 138 μm in the x, y, z axes, respectively), it would take more than 5 years before there is evidence of measurable wear. Similar findings have been reported for first-generation HXLPE liners, which highlights the need to evaluate HXLPE over a period of at least 5 years [9, 35]. The annual 2-D wear rate calculated in our study was considerably less than for proximal wear; however, linear measurements of 2-D wear are thought to underestimate the true wear rate [17, 48] and therefore may not truly represent the wear rate for this type of polyethylene.
First-generation annealed Crossfire® liners are reported to have an annual wear rate of 36 μm/year based on a 5-year evaluation of plain radiographs [12]. The annual wear rate for the X3™ liner found in our study (15 μm/year) is 58% less than this, which is consistent with the hip simulator results of Dumbleton et al. [16], who found the X3™ material had 62% less wear than Crossfire® liners. Rohrl et al. [44] reported a mean wear of 23 μm between 2 and 24 months for Crossfire® inserts. This is similar to the mean proximal head penetration we found (28 μm) for the X3™ liner; however, an accurate comparison requires a longer study to quantify the potential differences in wear between these materials.
A low rate of polyethylene wear is advantageous as it reduces the likelihood of wear particle-induced osteolysis and the subsequent need for revision arthroplasty owing to aseptic loosening. Dumbleton et al. [17] have assigned an osteolysis threshold for wear of 0.1 mm/year, below which osteolysis occurs infrequently, and a rate of 0.05 mm/year, which is considered safe, as the occurrence of osteolysis is almost eliminated. The annual wear rate calculated in our study was well below this threshold. We can expect the need for revision arthroplasty attributable to wear particle-induced osteolysis to be unlikely at least in the short term. The functional biologic activity of this material is likely to be lower than conventional polyethylene owing to a combination of similar specific biologic activity and lower wear rate [16, 19].
Our study showed that wear of X3™ acetabular liners after 2 years is less than a clinically quantifiable level, making accurate comparison with first-generation Crossfire® liners challenging. A longer period of evaluation is required until wear reaches a level that is clinically detectable. However, it is clear X3™ liners have wear properties superior to those of conventional polyethylene. Our measurements between 1 and 2 years followup suggest wear is nearly undetectable, which is encouraging for the future clinical performance of this material.
Acknowledgments
The authors thank Meegan Bartell for her assistance with collection of patient data in this study, Yvonne Johnston for her skills with RSA imaging, and Alexandra Pearce for her assistance in preparing the manuscript.
Footnotes
One or more of the authors (DGC) has received funding from Stryker Orthopaedics, Mahwah, NJ.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Wakefield Orthopaedic Clinic.
References
- 1.Altman DG. Practical Statistics for Medical Research. London, UK: Chapman and Hall; 1991. [Google Scholar]
- 2.Annual Report. Adelaide, Australia: AOA; 2008. [Google Scholar]
- 3.Avery J, Dal Grande E, Taylor A. Quality Of Life in South Australia as Measured by the SF12 Health Status Questionnaire Population Norms For 2003 Trends From 1997–2003. Adelaide, South Australia: Population Research and Outcome Studies Unit Department of Human Services; 2004. [Google Scholar]
- 4.Borlin N, Rohrl SM, Bragdon CR. RSA wear measurements with or without markers in total hip arthroplasty. J Biomech. 2006;39:1641–1650. doi: 10.1016/j.jbiomech.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Bradford L, Baker DA, Graham J, Chawan A, Ries MD, Pruitt LA. Wear and surface cracking in early retrieved highly cross-linked polyethylene acetabular liners. J Bone Joint Surg Am. 2004;86:1271–1282. doi: 10.2106/00004623-200406000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Bragdon CR, Barrett S, Martell JM, Greene ME, Malchau H, Harris WH. Steady-state penetration rates of electron beam-irradiated, highly cross-linked polyethylene at an average 45-month follow-up. J Arthroplasty. 2006;21:935–943. doi: 10.1016/j.arth.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Bragdon CR, Malchau H, Yuan X, Perinchief R, Karrholm J, Borlin N, Estok DM, Harris WH. Experimental assessment of precision and accuracy of radiostereometric analysis for the determination of polyethylene wear in a total hip replacement model. J Orthop Res. 2002;20:688–695. doi: 10.1016/S0736-0266(01)00171-1. [DOI] [PubMed] [Google Scholar]
- 8.Bragdon CR, Thanner J, Greene ME, Malchau H, Digas G, Harris WH, Karrholm J. Standing versus supine radiographs in RSA evaluation of femoral head penetration. Clin Orthop Relat Res. 2006;448:46–51. doi: 10.1097/01.blo.0000224012.50292.67. [DOI] [PubMed] [Google Scholar]
- 9.Campbell D, Mercer G, Nilsson K, Wells V, Field JR, Callary SA. Wear of a highly cross-linked polyethylene liner: a preliminary RSA study. Eur J Orthop Surg Traumatol. 2009; DOI 10.1007/s00590-009-0486-y.
- 10.Clohisy JC, Calvert G, Tull F, McDonald D, Maloney WJ. Reasons for revision hip surgery: a retrospective review. Clin Orthop Relat Res. 2004;429:188–192. doi: 10.1097/01.blo.0000150126.73024.42. [DOI] [PubMed] [Google Scholar]
- 11.Collier JP, Currier BH, Kennedy FE, Currier JH, Timmins GS, Jackson SK, Brewer RL. Comparison of cross-linked polyethylene materials for orthopaedic applications. Clin Orthop Relat Res. 2003;414:289–304. doi: 10.1097/01.blo.0000073343.50837.03. [DOI] [PubMed] [Google Scholar]
- 12.D’Antonio JA, Manley MT, Capello WN, Bierbaum BE, Ramakrishnan R, Naughton M, Sutton K. Five-year experience with Crossfire highly cross-linked polyethylene. Clin Orthop Relat Res. 2005;441:143–150. doi: 10.1097/00003086-200512000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Derbyshire B, Prescott RJ, Porter ML. Notes on the use and interpretation of radiostereometric analysis. Acta Orthop. 2009;80:124–130. doi: 10.1080/17453670902807474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dorr LD, Wan Z, Shahrdar C, Sirianni L, Boutary M, Yun A. Clinical performance of a Durasul highly cross-linked polyethylene acetabular liner for total hip arthroplasty at five years. J Bone Joint Surg Am. 2005;87:1816–1821. doi: 10.2106/JBJS.D.01915. [DOI] [PubMed] [Google Scholar]
- 15.Dowd JE, Sychterz CJ, Young AM, Engh CA. Characterization of long-term femoral-head-penetration rates: association with and prediction of osteolysis. J Bone Joint Surg Am. 2000;82:1102–1107. doi: 10.2106/00004623-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Dumbleton JH, D’Antonio JA, Manley MT, Capello WN, Wang A. The basis for a second-generation highly cross-linked UHMWPE. Clin Orthop Relat Res. 2006;453:265–271. doi: 10.1097/01.blo.0000238856.61862.7d. [DOI] [PubMed] [Google Scholar]
- 17.Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17:649–661. doi: 10.1054/arth.2002.33664. [DOI] [PubMed] [Google Scholar]
- 18.Dunbar MJ, Blackley HR, Bourne RB. Osteolysis of the femur: principles of management. Instr Course Lect. 2001;50:197–209. [PubMed] [Google Scholar]
- 19.Endo M, Tipper JL, Barton DC, Stone MH, Ingham E, Fisher J. Comparison of wear, wear debris and functional biological activity of moderately crosslinked and non-crosslinked polyethylenes in hip prostheses. Proc Inst Mech Eng H. 2002;216:111–122. doi: 10.1243/0954411021536333. [DOI] [PubMed] [Google Scholar]
- 20.Engh CA, Jr, Stepniewski AS, Ginn SD, Beykirch SE, Sychterz-Terefenko CJ, Hopper RH, Jr, Engh CA. A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked marathon and non-cross-linked Enduron polyethylene liners. J Arthroplasty. 2006;21((6 suppl 2)):17–25. doi: 10.1016/j.arth.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Estok DM, II, Bragdon CR, Plank GR, Huang A, Muratoglu OK, Harris WH. The measurement of creep in ultrahigh molecular weight polyethylene: a comparison of conventional versus highly cross-linked polyethylene. J Arthroplasty. 2005;20:239–243. doi: 10.1016/j.arth.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 22.Furmanski J, Gupta S, Chawan A, Kohm A, Lannutti J, Jewett B, Pruitt LA, Ries MD. Aspherical femoral head with highly cross-linked ultra-high molecular weight polyethylene surface cracking: a case report. J Bone Joint Surg Am. 2007;89:2266–2270. doi: 10.2106/JBJS.F.00428. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Cimbrelo E, Munuera L. Early and late loosening of the acetabular cup after low-friction arthroplasty. J Bone Joint Surg Am. 1992;74:1119–1129. [PubMed] [Google Scholar]
- 24.Glyn-Jones S, McLardy-Smith P, Gill HS, Murray DW. The creep and wear of highly cross-linked polyethylene: a three-year randomised, controlled trial using radiostereometric analysis. J Bone Joint Surg Br. 2008;90:556–561. doi: 10.1302/0301-620X.90B5.20545. [DOI] [PubMed] [Google Scholar]
- 25.Halley D, Glassman A, Crowninshield RD. Recurrent dislocation after revision total hip replacement with a large prosthetic femoral head: a case report. J Bone Joint Surg Am. 2004;86:827–830. doi: 10.2106/00004623-200404000-00025. [DOI] [PubMed] [Google Scholar]
- 26.Harris WH. The problem is osteolysis. Clin Orthop Relat Res. 1995;311:46–53. [PubMed] [Google Scholar]
- 27.Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73, 000 arthroplasties. Acta Orthop Scand. 2000;71:337–353. doi: 10.1080/000164700317393321. [DOI] [PubMed] [Google Scholar]
- 28.Heisel C, Silva M, dela Rosa MA, Schmalzried TP. Short-term in vivo wear of cross-linked polyethylene. J Bone Joint Surg Am. 2004;86:748–751. doi: 10.2106/00004623-200404000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Hopper RH, Jr, Young AM, Orishimo KF, McAuley JP. Correlation between early and late wear rates in total hip arthroplasty with application to the performance of marathon cross-linked polyethylene liners. J Arthroplasty. 2003;18((7 suppl 1)):60–67. doi: 10.1016/s0883-5403(03)00294-8. [DOI] [PubMed] [Google Scholar]
- 30.Krushell RJ, Fingeroth RJ, Cushing MC. Early femoral head penetration of a highly cross-linked polyethylene liner vs a conventional polyethylene liner: a case-controlled study. J Arthroplasty. 2005;20((7 suppl 3)):73–76. doi: 10.1016/j.arth.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Leung SB, Egawa H, Stepniewski A, Beykirch S, Engh CA, Jr, Engh CA., Sr Incidence and volume of pelvic osteolysis at early follow-up with highly cross-linked and noncross-linked polyethylene. J Arthroplasty. 2007;22((6 suppl 2)):134–139. doi: 10.1016/j.arth.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Livingston BJ, Chmell MJ, Spector M, Poss R. Complications of total hip arthroplasty associated with the use of an acetabular component with a Hylamer liner. J Bone Joint Surg Am. 1997;79:1529–1538. doi: 10.2106/00004623-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Lochner HV, Bhandari M, Tornetta P., III Type-II error rates (beta errors) of randomized trials in orthopaedic trauma. J Bone Joint Surg Am. 2001;83:1650–1655. doi: 10.2106/00004623-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Manning DW, Chiang PP, Martell JM, Galante JO, Harris WH. In vivo comparative wear study of traditional and highly cross-linked polyethylene in total hip arthroplasty. J Arthroplasty. 2005;20:880–886. doi: 10.1016/j.arth.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 35.McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2009;91:773–782. doi: 10.2106/JBJS.H.00244. [DOI] [PubMed] [Google Scholar]
- 36.McCalden RW, Naudie DD, Yuan X, Bourne RB. Radiographic methods for the assessment of polyethylene wear after total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2323–2334. doi: 10.2106/JBJS.E.00223. [DOI] [PubMed] [Google Scholar]
- 37.McKellop H, Shen FW, Lu B, Campbell P, Salovey R. Development of an extremely wear-resistant ultra high molecular weight polyethylene for total hip replacements. J Orthop Res. 1999;17:157–167. doi: 10.1002/jor.1100170203. [DOI] [PubMed] [Google Scholar]
- 38.Muratoglu OK, Bragdon CR, O’Connor DO, Jasty M, Harris WH. A novel method of cross-linking ultra-high-molecular-weight polyethylene to improve wear, reduce oxidation, and retain mechanical properties. Recipient of the 1999 HAP Paul Award. J Arthroplasty. 2001;16:149–160. doi: 10.1054/arth.2001.20540. [DOI] [PubMed] [Google Scholar]
- 39.Norton MR, Yarlagadda R, Anderson GH. Catastrophic failure of the Elite Plus total hip replacement, with a Hylamer acetabulum and Zirconia ceramic femoral head. J Bone Joint Surg Br. 2002;84:631–635. doi: 10.1302/0301-620x.84b5.12679. [DOI] [PubMed] [Google Scholar]
- 40.Oparaugo PC, Clarke IC, Malchau H, Herberts P. Correlation of wear debris-induced osteolysis and revision with volumetric wear-rates of polyethylene: a survey of 8 reports in the literature. Acta Orthop Scand. 2001;72:22–28. doi: 10.1080/000164701753606644. [DOI] [PubMed] [Google Scholar]
- 41.Oral E, Malhi AS, Muratoglu OK. Mechanisms of decrease in fatigue crack propagation resistance in irradiated and melted UHMWPE. Biomaterials. 2006;27:917–925. doi: 10.1016/j.biomaterials.2005.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oral E, Wannomae KK, Hawkins N, Harris WH, Muratoglu OK. Alpha-tocopherol-doped irradiated UHMWPE for high fatigue resistance and low wear. Biomaterials. 2004;25:5515–5522. doi: 10.1016/j.biomaterials.2003.12.048. [DOI] [PubMed] [Google Scholar]
- 43.Ries MD, Pruitt L. Effect of cross-linking on the microstructure and mechanical properties of ultra-high molecular weight polyethylene. Clin Orthop Relat Res. 2005;440:149–156. doi: 10.1097/01.blo.0000185310.59202.e5. [DOI] [PubMed] [Google Scholar]
- 44.Rohrl S, Nivbrant B, Mingguo L, Hewitt B. In vivo wear and migration of highly cross-linked polyethylene cups: a radiostereometry analysis study. J Arthroplasty. 2005;20:409–413. doi: 10.1016/j.arth.2004.09.040. [DOI] [PubMed] [Google Scholar]
- 45.Saleh KJ, Thongtrangan I, Schwarz EM. Osteolysis: medical and surgical approaches. Clin Orthop Relat Res. 2004;427:138–147. [PubMed] [Google Scholar]
- 46.Schmalzried TP, Kwong LM, Jasty M, Sedlacek RC, Haire TC, O’Connor DO, Bragdon CR, Kabo JM, Malcolm AJ, Harris WH. The mechanism of loosening of cemented acetabular components in total hip arthroplasty: analysis of specimens retrieved at autopsy. Clin Orthop Relat Res. 1992;274:60–78. [PubMed] [Google Scholar]
- 47.Silva M, Shepherd EF, Jackson WO, Dorey FJ, Schmalzried TP. Average patient walking activity approaches 2 million cycles per year: pedometers under-record walking activity. J Arthroplasty. 2002;17:693–697. doi: 10.1054/arth.2002.32699. [DOI] [PubMed] [Google Scholar]
- 48.Sychterz CJ, Engh CA, Jr, Shah N, Engh CA., Sr Radiographic evaluation of penetration by the femoral head into the polyethylene liner over time. J Bone Joint Surg Am. 1997;79:1040–1046. doi: 10.2106/00004623-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 49.Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop. 2005;76:563–572. doi: 10.1080/17453670510041574. [DOI] [PubMed] [Google Scholar]
- 50.Schewelov T, Onsten I, Markusson P, Carlsson A. Weight bearing radiographs are not necessary for measurement of polyethylene penetration in total hip prostheses: a radiostereometric study of 111 patients examined in weight-bearing and supine position. Acta Orthop. 2006;77:104–108. doi: 10.1080/17453670610045768. [DOI] [PubMed] [Google Scholar]
- 51.Schewelov T, Sanzen L, Borlin N, Markusson P, Onsten I. Accuracy of radiographic and radiostereometric wear measurement of different hip prostheses: an experimental study. Acta Orthop Scand. 2004;75:691–700. doi: 10.1080/00016470410004058. [DOI] [PubMed] [Google Scholar]
- 52.Whitley E, Ball J. Statistics review 4: sample size calculations. Crit Care. 2002;6:335–341. doi: 10.1186/cc1521. [DOI] [PMC free article] [PubMed] [Google Scholar]