Abstract
Background
Short- to medium-term rotator cuff repair reportedly relieves pain in 82% to 97% of patients and provides normal or almost normal shoulder function in 82% to 92%. However, it is unknown whether pain relief and function persist long term.
Questions/purposes
We asked whether, after rotator cuff repair or reconstruction, pain relief, ROM, shoulder strength, and function remained over the long term.
Patients and Methods
We retrospectively reviewed 75 patients who underwent rotator cuff repair between 1980 and 1989. There were 55 men and 20 women. Their mean age at surgery was 52 years. The minimum followup was 16 years (mean, 20 years; range 16–25 years).
Results
Twenty-eight of the 75 patients (37%) had persistent relief of pain lasting for 20 years. In the remaining 47 patients, alleviation of pain lasted, on average, 14 years (range, 0–24 years). Mean flexion and abduction strength increased postoperatively but during long-term followup decreased to less than preoperative levels. External rotation also decreased. At the last followup, the Constant-Murley score averaged 66 (range, 10–98) in men and 60 (range, 29–89) in women. In the Simple Shoulder Test questionnaire, the mean number of yes answers was eight of 12. Of the 75 patients, 32 (43%) reported impairment in activities of daily living owing to an index shoulder complaint. Severe degenerative changes of the glenohumeral joint were evident in 14 patients (19%).
Conclusions
The early high functional scores after primary rotator cuff repair or reconstruction of the types we performed in the 1980s did not persist. The function achieved postoperatively was lost, as ROM and strength decreased to less than preoperative values. However, alleviation of pain was long-standing in most patients. Based on our data, we should warn patients to expect less than permanent relief with those repairs. We cannot say whether the same will apply to currently performed types of repairs.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Symptomatic complete rotator cuff tears refractory to nonoperative treatment usually are treated surgically. Clinical, functional, and radiographic early or midterm (2–9 years) results of rotator cuff repair are well documented [2, 8, 9, 12–14, 16–19, 22, 24, 28, 32, 36–38]. Although surgical repair of the rotator cuff is common, we are aware of only four papers reporting followup of at least 10 years [1, 5, 11, 35]. In addition, we reported our preliminary results in Finnish in 2006 [4]. Adamson and Tibone [1] evaluated 30 patients 10 years after rotator cuff repair. They reported 80% good or excellent results with objective data, results not deteriorating during followup extending to 10 years. Cofield et al. [5] evaluated 81 patients by telephone or questionnaire 13.4 years after surgery. They found satisfactory pain relief in 90%, substantial improvement in active abduction and external rotation and in strength in these directions. These were consistent and lasting. Galatz et al. [11] evaluated 33 patients 10 years after surgery. As they found no change in Constant-Murley score determined at the 2-year examination, they concluded the results of open rotator cuff repair do not deteriorate with time. Sperling et al. [35] evaluated 25 patients 50 years or younger, most by questionnaire a mean of 16.2 years after surgery. Long-term pain relief was marked, but they found no long-term improvement or deterioration in shoulder motion. Various authors suggest rotator cuff surgery yields long-standing pain relief in 38% to 60%, shoulder flexion 144° to 157°, and abduction 139° to 161° [1, 5, 35]. However, based on the 30-year clinical experience of the senior author (MV), we believed results might deteriorate with time.
We therefore evaluated the long-term (1) pain relief, (2) ROM, (3) shoulder strength, (4) functional scores, and (5) satisfaction of rotator cuff repair or reconstruction 16 to 25 years after surgery.
Patients and Methods
We identified 282 patients who had a primary rotator cuff tear treated surgically between January 1980 and May 1989. Of these, 137 (49%) had undergone preoperative ROM and strength measurements with a spring balance [27, 34, 36]. For the other patients, strength testing had been performed only manually. Of these 137, 36 had died and one lived abroad. The remaining 100 were asked to participate in the study, and 75 (27% of the total, 55 of whom were men) agreed to participate. The two main reasons patients refused to participate were poor physical condition and a large travel distance for followup. The mean age of the patients at the time of surgery was 52.3 years (range, 30–65 years). The time from onset of symptoms to surgery was from 0.2 to 19.2 years (mean, 2.4 years; median, 1.0 year). Operative delay was less than 6 months in 14 cases, 6 to 12 months in 21, and more than 12 months in 40. The average age of the patients at last followup was 72.2 years (range, 52–84 years). Preoperative and postoperative data came from patients’ medical records. Preoperative radiographs were available for 42 of 75 shoulders that underwent surgery; we observed slight degenerative changes in five shoulders. Physical and radiographic examinations were performed between June 2005 and April 2006. There were 20 direct repairs and 55 reconstructions using a free tendon graft. The minimum followup was 16 years (mean, 19.9 years; range, 16.9–24.8 years). All patients gave informed consent. We obtained permission to perform this study from the ethics committee of the hospital district where the study was conducted.
Surgery was performed by eight surgeons, although the senior author (MV) performed 53 (71%) of the 75 repairs. The supraspinatus tendon alone was involved in 40 patients (Table 1). Although 20 tears were repaired directly with nonabsorbable suture (Mersilene®; Ethicon Inc, Somerville, NJ), for 55, repair was performed with a free tendon graft (long plantaris tendon in 42 and long extensor tendon of the second and third toes in 13) [34, 36]. A tendon graft was used mostly as strong suture material to reattach the torn tendon to the bone more accurately. We believed, especially in old retracted rotator cuff tears, a free tendon graft would hold better than rather thin suture material [34, 36]. At least 20 of the surgeries actually were repairs, because 20 to 30 years ago we used a tendon graft in almost all old retracted cases. Today, we see those cases less often. For better observation, anterior acromioplasty according to Neer [29] and Fealy et al. [10] was performed in 20 patients, acromial osteotomy according to DeBeyre et al. [7] in 43, and acromioplasty and acromial osteotomy combined in three; 20 patients had biceps tenodesis.
Table 1.
Surgical characteristics of patients after long-term followup
| Characteristic | Number of patients |
|---|---|
| Ruptured tendons | |
| SSP | 40 (53%) |
| SSP + ISP | 27 (36%) |
| SSP + ISP + SSC | 3 (4%) |
| SSP + SSC | 4 (5%) |
| SSC | 1 (1%) |
| Direct suture | |
| SSP | 17 (23%) |
| SSP + ISP | 3 (4%) |
| Free tendon graft | |
| SSP | 23 (31%) |
| SSP + ISP | 24 (32%) |
| SSP + ISP + SSC | 3 (4%) |
| SSP + SSC | 4 (5%) |
| SSC | 1 (1%) |
SSP = supraspinatus; ISP = infraspinatus; SSC = subscapularis.
Postoperatively, the arm was immobilized in an abduction splint for an average of 6 weeks (range, 5–7 weeks). The elbow was mobilized on the first postoperative day. Passive mobilization of the arm was started at 2 weeks on the splinted arm, ie, the patient, using the other hand or another person lifting the arm 10 to 20 cm upward to prevent adhesions. After immobilization, all patients visited the hospital for 2 to 4 days of intensive supervised physiotherapy including pool exercises. Physiotherapy continued for 1 to 3 months as an outpatient, and in some cases, even longer.
The patients routinely came to their followup visit 1 and 2 months after the mobilization period. Normally, most returned or already had returned to work by the 2-month visit (3.5 months after surgery). The next visit was scheduled after 3 months, but if the patient was unable to work, the visit was scheduled after 1 month. At every visit, active and passive ROM, shoulder strength by manual testing without a spring balance, and pain were recorded.
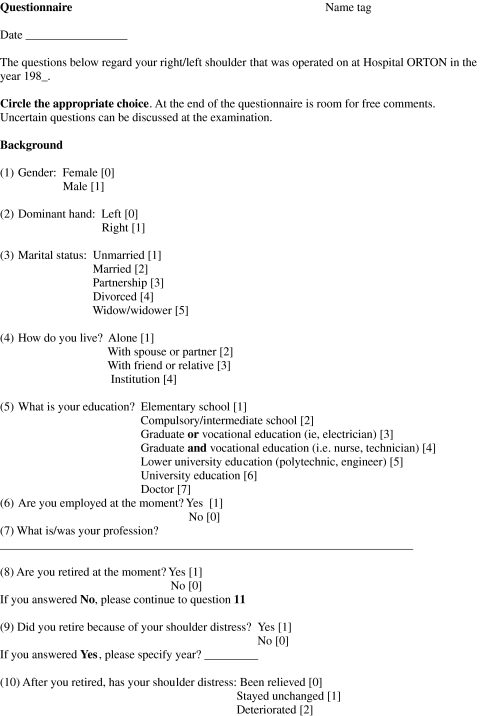
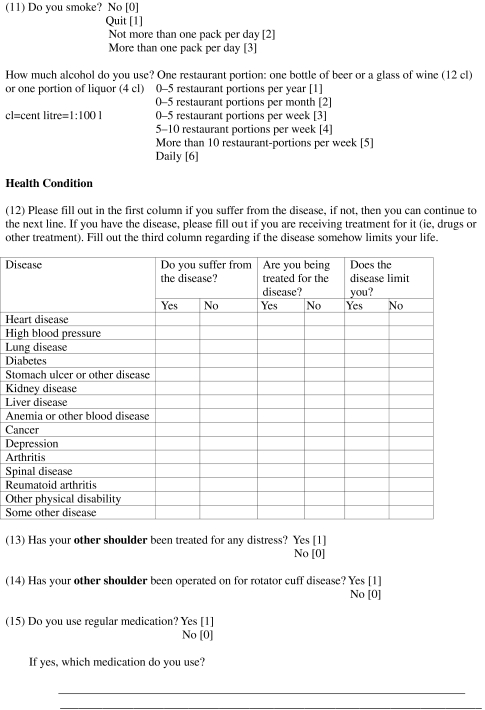
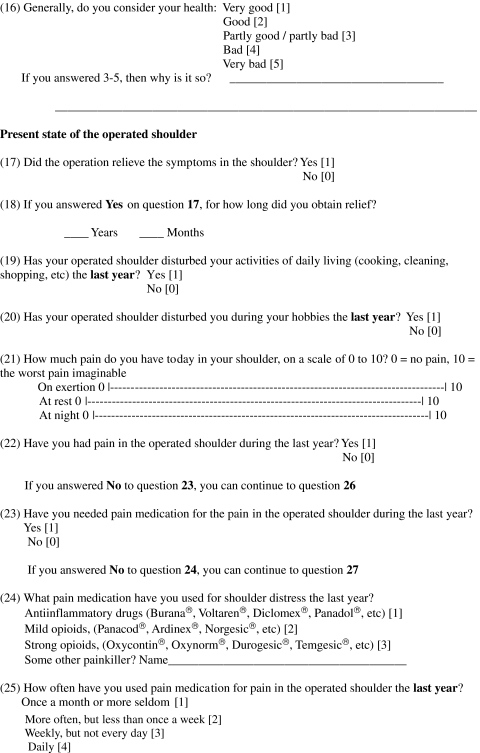
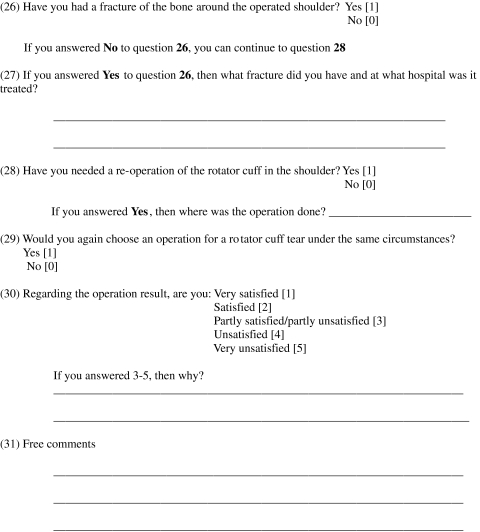
Questionnaires (Appendix) were mailed to the patients along with the invitation to participate in the study. The questionnaire comprised questions concerning demographics, subjective satisfaction measured on a 5-point Likert scale (1 = very satisfied and 5 = very unsatisfied), and symptoms of the surgically treated shoulder including pain evaluation on a visual analog scale (VAS) (range, 0–10; 0 = no pain and 10 = maximal, intensive pain) [31]. Patients also received the Simple Shoulder Test questionnaire [25]. The patients completed these questionnaires at home and returned them at followup. Their answers were checked during the followup visit.
All 75 patients underwent a physical examination preoperatively, postoperatively, and at the final followup. ROM of both shoulders was measured with a goniometer, and muscle strength was measured with the same Salter spring balance used preoperatively [27, 34, 36]. During measurements, the patient was seated, but abduction strength measurement of the arm at a 30° angle was performed with the patient standing. The last postoperative routine clinical followup was approximately 6 months after surgery. At the final followup, the physical examination was performed by an independent observer (NB). Presence of a painful arc sign was indicated by yes or no. Shoulder function was assessed with the Constant-Murley score [6]; absolute and age- and gender-related scores were calculated [21].
Analysis of the radiographs was performed by independent blinded experienced observers (ML, KT) who did not know the history or clinical signs of the patients and did not see the patients. AP radiographs of the shoulder in internal and external rotation of the arm and a supraspinatus outlet view were taken at the last followup. The presence of acromial nonunion was yes or no. Classification of acromioclavicular osteoarthritis was by the three-grade classification of Bonsell et al. [3]. For evaluation of osteoarthritis in the glenohumeral joint, we used a modified version of the grading system of Samilson and Prieto [33], placing moderate and severe osteoarthritis in the same group, and resulting in a three-grade classification for the glenohumeral joint.
We computed the means of continuous data (ranges in parentheses). A paired t test was used to compare differences in continuous outcomes (VAS, ROM, muscle strength) between the different evaluation periods. ANOVA was used to evaluate the association between patient satisfaction and ROM, muscle strength, or function. The same procedure was used to analyze the association between radiographic findings and ROM, painful arc, or function.
Results
Alleviation of pain seemed to be the most important factor concerning patient satisfaction at the last followup. The mean pain score on the VAS was 3.7 (range, 0–10) during activity, 1.5 (range, 0–10) at rest, and 2.1 (range, 0–10) at night (Table 2). Alleviation of pain lasted, on average, 14 years. For 28 patients (37%), at the last followup 20 years after surgery, symptoms were still absent. In nine of 47 patients, the shoulder had been asymptomatic more than 20 years; one patient had been without symptoms until 24.4 years and had been symptomatic only a few months.
Table 2.
Long-term results after rotator cuff surgery
| Study | Number of shoulders | Followup (years) | Patients with and without pain | Motion (°) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No pain | In motion | At night | At rest | Flexion | Abduction | External rotation | Internal rotation | ||||
| Adamson & Tibone [1] | 30 | 10 | 60% | 30% (slight) | 7% (moderate) | 3% (severe) | 157 | 161 | 62 | T9 | |
| Cofield et al. [5] | 105 | 13.4 | 52% | 30% | 17% | 1% | 154 | 69 | T10 | ||
| Galatz et al. [11] | 33 | 10 | |||||||||
| Sperling et al. [35] | 29 | 16.2 | 38% | 31% | 10% | 21% | 153 | 55 | L5 | ||
| Current study | 75 | 19.9 | 3.7 (VAS 0–10) | 2.1 (VAS 0–10) | 1.5 (VAS 0–10) | 144 | 139 | 49 | |||
| Study | Strength | Function (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Objective assessment | Subjective assessment | ||||||||||
| Flexion | Abduction | External rotation | Internal rotation | Other | Excellent | Good | Fair | Poor | Excellent + good | ||
| Adamson & Tibone [1] | Manual muscle test (kg) | Excellent 20 Good 44 Fair 16 Poor 20 |
37 | 33 | 23 | 7 | 70 | ||||
| 4.7 | 4.5 | 4.5 | |||||||||
| Cofield et al. [5] | Manual muscle test (%) Normal 50 Good 34 Fair 14 Poor 2 |
Neer system [28] Excellent 65 Satisfactory 15 Unsatisfactory 20 |
73 | 19 | 5 | 3 | 92 | ||||
| Galatz et al. [11] | Mean raw Constant-Murley [6] score 81.2 Mean normalized Constant-Murley score 95.2 |
93 | |||||||||
| Sperling et al. [35] | Manual muscle test (%) Normal 34 Good 31 Fair 21 Poor 14 |
Neer system Excellent 38 Satisfactory 17 Unsatisfactory 45 |
55 | ||||||||
| Current study | Spring balance (kg) | Mean raw Constant-Murley score 64.4 | 53 | 28 | 11 | 8 | 71 | ||||
| 4.1 | 3.7 | 5.2 | 9.2 | Mean normalized Constant-Murley score 81.3 Mean raw Constant-Murley score 81–100: 17 66–80: 39 < 65: 44 |
|||||||
VAS = visual analog scale.
Subjective satisfaction was high, although many patients had mild or moderate pain; 40 (53%) were very satisfied and 21 (28%) were satisfied (Table 3).
Table 3.
Patients’ subjective satisfaction with the long-term end result
| Satisfaction | Flexion (°)* | Abduction (°)† | External rotation (°)‡ |
|---|---|---|---|
| Very satisfied (n = 40) | 155 (70–180) | 155 (70–180) | 56 (0–95) |
| Satisfied (n = 21) | 147 (35–180) | 135 (40–180) | 50 (10–100) |
| Partially satisfied/dissatisfied (n = 8) | 133 (60–170) | 121 (60–180) | 32 (10–60) |
| Dissatisfied (n = 3) | 85 (35–165) | 85 (50–155) | 33 (20–50) |
| Very dissatisfied (n = 3) | 75 (30–100) | 60 (45–70) | 15 (0–30) |
| All | 144 (30–180) | 139 (40–180) | 49 (0–100) |
Values are expressed as means, with ranges in parentheses; * p < 0.001; †p < 0.001; ‡p < 0.006.
Active range of flexion and abduction improved postoperatively but at final followup again had deteriorated (Table 4). ROM in external rotation decreased (p < 0.004) between preoperative ROM and last followup. ROM measurements were associated with patients’ satisfaction at last followup (Table 3). The better the flexion, abduction, and external rotation were, the more satisfied the patient was.
Table 4.
Results of physical examinations of patients with long-term followup after rotator cuff repair
| Variable | Preoperative values | Postoperative values | Followup values |
|---|---|---|---|
| Index shoulder | |||
| ROM (º) | |||
| Flexion | 140 (0–180) | 155 (70–180) | 144 (30–180) |
| Abduction | 148 (15–180) | 154 (30–180) | 139 (40–180) |
| External rotation | 60* (0–90) | 53 (0–90) | 49* (0–100) |
| Strength (kg) | |||
| Flexion | 4.9† (0.6–10) | 6.3 (1.9–10) | 4.1†,** (0–10) |
| Abduction | 4.4‡ (0.4–10) | 5.6 (1.1–10) | 3.7‡,** (0–10) |
| External rotation | 6.4§ (1.4–10) | 7.7 (1.6–12) | 5.2§,** (0–10) |
| Internal rotation | 9.5 (5.3–10) | 9.8 (7.4–10) | 9.2 (3.4–10) |
| Contralateral shoulder | |||
| ROM (º) | |||
| Flexion | 159 (110–180) | 151 (50–180) | |
| Abduction | 175|| (100–180) | 151|| (60–180) | |
| External rotation | 73¶ (10–90) | 57¶ (0–110) | |
| Strength (kg) | |||
| Flexion | 8.8¶ (3.5–10) | 5.0¶,** (0–10) | |
| Abduction | 8.4¶ (3.2–10) | 4.7¶,** (0–10) | |
| External rotation | 9.1¶ (3.4–10) | 6.1¶,** (0–10) | |
| Internal rotation | 9.9 (7–10) | 9.6 (3.8–10) | |
Mean followup was 19.9 years (range, 16.9–24.8 years); values are expressed as means, with ranges in parentheses; on the contralateral side, no difference emerged in ROM between patients with or without previous rotator cuff surgery; differences between preoperative and followup values (Wilcoxon signed rank sum test): * p < 0.006; †p < 0.004; ‡p < 0.01; §p < 0.003; ||p < 0.002; ¶p < 0.0001; difference between index shoulder and contralateral shoulder (Mann-Whitney U test): ** p < 0.0001.
Mean abduction and shoulder strength increased during the first 6 months postoperatively by 20% to 29%. However, strength decreased over long-term followup, so that at the last followup strength had decreased by 16% to 19% compared with preoperative strength. However, the strength of the contralateral shoulder also decreased during followup, even more than that of the treated shoulder (by 33% to 44%). No association emerged between patients’ subjective satisfaction and muscle strength.
Of the 75 patients, the Constant-Murley score was 81 to 100 points in 13 patients and 66 to 80 points in 29. Male patients scored, on average, 66 points (range, 10–98 points) and female patients scored 60 points (range, 29–89 points). Age- and gender-related scores were 81 points (range, 13–100 points) for men and 82 points (range, 42–100 points) for women. No association emerged between patients’ subjective satisfaction and Constant-Murley score (absolute or adjusted). In the Simple Shoulder Test questionnaire, the mean number of yes answers was eight of 12 (range, 0–12) (Table 5). Most commonly, patients reported problems with throwing. Of the 75 patients, 32 (43%) reported some kind of impairment in activities of daily living attributable to an index shoulder complaint.
Table 5.
Results from Simple Shoulder Test questionnaire for patients with 20 years of followup
| Question | Percentage of patients answering yes |
|---|---|
| 1. Is your shoulder comfortable with your arm at rest by your side? | 67% |
| 2. Does your shoulder allow you to sleep comfortably? | 67% |
| 3. Can you reach the small of your back to tuck in your shirt with your hand? | 84% |
| 4. Can you place your hand behind your head with the elbow straight out to the side? | 85% |
| 5. Can you place a coin on a shelf at the level of your shoulder without bending your elbow? | 84% |
| 6. Can you lift 1 pound (a full pint container) to the level of your shoulder without bending your elbow? | 83% |
| 7. Can you lift 8 pounds (a full gallon container) to the level of your shoulder without bending your elbow? | 48% |
| 8. Can you carry 20 pounds at your side with the affected extremity? | 67% |
| 9. Do you think you can toss a softball underhand 20 yards with the affected extremity? | 69% |
| 10. Do you think you can toss a softball overhand 20 yards with the affected extremity? | 35% |
| 11. Can you wash the back of your opposite shoulder with the affected extremity? | 91% |
| 12. Would your shoulder allow you to work full-time at your regular job? | 49% |
| Mean (range) of the yes answers of 12 questions per patient | 8 (0–12) |
Under the same circumstances, 73 patients (97%) would have chosen surgery again. Of the 75 patients, 37 had been treated and 32 (43%) operated on for a rotator cuff tear of the contralateral shoulder.
We observed severe degenerative changes of the glenohumeral joint in 14 patients, including three of those with slight preoperative arthrosis. Twelve patients with reconstructions and two with repaired shoulders had severe arthrosis. At last followup, glenohumeral osteoarthritis correlated only with ROM in external rotation (rs = −0.42; 95% CI, −0.59 to −0.21). Any degenerative changes seen on radiographs showed no correlation with a painful arc or with Constant-Murley score.
Four of the 75 patients each sustained one complication. Two had had a postoperative hematoma and underwent wound exploration, one had a superficial infection treated with oral antibiotics, and one had a deep venous thrombosis in the lower leg. The acromial osteotomy did not heal in six patients (14%). Four of them had severe degenerative changes, but only two had Constant-Murley scores less than 50. In addition, 10 patients (13%) had a second surgery because of a rerupture during followup. Six of those patients had a relevant trauma before the second surgery.
Discussion
Results of rotator cuff repair are mostly favorable. In the early 1980s, the senior author (MV) reported the results of operative repair of the rotator cuff at a mean 3.5-year followup [36]. We now wished to know the long-term results of cuff repairs performed by the same methods. We asked whether (1) pain relief, (2) ROM, (3) shoulder strength, and (4) function remained over the long term after rotator cuff repair or reconstruction in 75 patients evaluated 16 to 24 years after surgery.
We acknowledge several limitations. First, acromial osteotomy according to DeBeyre et al. [7] rarely is used today. Although we cannot tell from our data whether these osteotomies influenced the long-term outcome, it is possible they could. Second, many of the patients in this series had quite large and complicated ruptures, and in many cases, the patient had been referred to our hospital from another hospital. The time from onset of symptoms to surgery 30 years ago, was, on average, 2.4 years (median, 1.0 year), making the ruptures difficult to repair. Free tendon grafts therefore were used in as many as 55 patients of the total 75. Our patients therefore may not represent a typical patient population in the current-day clinical setting with current widespread awareness of this condition and demand for accurate diagnosis and treatment without delay. However, we believe our patients represent, from the era before common use of MRI, typical patients with rotator cuff ruptures and with distinct clinical findings and functional disorders. Third, the patients were selected to include only those with preoperative ROM and strength measurements performed with a spring balance. We could include only ½ of the patients who had surgery, and only ½ of these patients fulfilled our requirements, owing to death or other reasons. Fourth, the Constant-Murley score and Simple Shoulder Test were not in use at the time of these surgeries. Although we place great value on longitudinal assessment of outcome measures, only ROM and strength measurements were available preoperatively and postoperatively. Fifth, although the Likert scale has not been validated for satisfaction, we used it to compare our data with data from some earlier studies reporting patients’ subjective satisfaction [1, 5, 17, 18, 36]. Sixth, the scale of the spring balance was from 0 to 10.2 kg with 0.2-kg increments. The strength of a healthy shoulder in men often is greater than 10.2 kg, especially in internal rotation. This fact surely causes errors in such measurements, but regarding injured shoulders and especially those in women, our results can be considered accurate. Finally, the interpretation of radiographs by only two examiners can be subjective, with poor interobserver reliability [30]. However, we consider the consensus opinion of two experienced orthopaedic radiologists to be a sufficiently objective system to interpret such films.
Pain alleviation lasted, on average, 14.3 years, but in 37% of the patients, pain still was absent after 20 years. Adamson and Tibone [1] evaluated 30 shoulders in 30 patients 10 years after rotator cuff repair. They reported pain with ROM in 27% but night pain in only 7%. Cofield et al. [5] evaluated 105 shoulders in 97 patients by physical examination an average 4.2 years after rotator cuff surgery. They evaluated 81 of those patients again by telephone and questionnaire 13.4 years after surgery, when 52% of the shoulders were not painful and 30% were only slightly painful. Galatz et al. [11] evaluated 33 shoulders in 33 patients 10 years after surgery but did not report on pain alone. Sperling et al. [35] evaluated 29 shoulders in 25 patients 50 years or younger (five by physical examination, 24 by questionnaire) 16.2 years after surgery. The pain score decreased from 4.8 to 2.6 points. That 11 shoulders had no pain (38%) is in accordance with our results (37% without pain after 20 years).
Although active range of flexion and abduction improved postoperatively, it deteriorated over long-term followup. Postoperative improvement was similar to what we reported earlier in the series of 126 patients with a rotator cuff rupture treated by the same methods from 1969 to 1980 and followed for 3.5 years [36]. Adamson and Tibone [1] reported, at 10 years’ followup, ROM (flexion 157°, abduction 161°, external rotation 62°) similar to what we observed at 6 months’ followup (155°, 154°, and 53°, respectively), but at 20 years, our results were substantially lower (144°, 139°, and 49°, respectively). Cofield et al. [5] reported, at their 13.4-year followup, 154° active abduction and 69° external rotation, but these figures were based on a telephone interview and questionnaire. In addition, Sperling et al. [35] reported active abduction of 153° and external rotation of 55° at 16.2 years after surgery, also based only on telephone interview and questionnaire.
Among long-term followup studies, there exist only results by manual muscle testing as in the study by Adamson and Tibone [1], reporting normal 5/5 strength occurred in flexion in 91% and in abduction in 77% 10 years after surgery. Cofield et al. [5] reported normal strength as determined by questionnaire 13.4 years after surgery in 62% of patients for flexion, 50% for abduction, and 59% for external rotation. Sperling et al. [35] reported normal strength assessed by the patient in 10 shoulders and good strength in nine, ie, normal or good strength in a total of 66%. Thirty years ago few shoulder surgeons routinely used a spring balance to measure shoulder strength, but manual testing mostly was adopted using the 5-point Highet scale. We routinely used the same Salter spring balance from 1980.
We measured functional outcome in this study using the Constant-Murley score and Simple Shoulder Test, unfortunately, tests that did not exist at the time of surgery. The Constant-Murley score was 66 or greater for 42 patients (56%). Scores of 81 to 100 are considered excellent and 66 to 80 good [6]. Adamson and Tibone [1] combined the subjective and objective results and reported 64% excellent plus good results after 10 years. Cofield et al. [5] used the Neer system [29] and rated 65% as excellent. Concerning the study by Cofield et al., we had problems understanding the numbers they reported. They had operated on 105 shoulders in 97 patients, and the first evaluation was, on average, 4.2 years after surgery. At the time of the latest followup by questionnaire at an average 13.4 years after surgery, they still report answers from 97 patients with 105 shoulders regarding pain. However, they report 16 patients had died during the followup period, with time to death averaging 6.5 years. Galatz et al. [11] reported an average Constant-Murley score of 81.2 points at 10 years, which is much better than the average score for our patients. Their normalized Constant-Murley score was good or excellent in 30 shoulders (91%), as in our series.
Subjective satisfaction has been one tool, albeit inaccurate, to measure outcome of surgery in the past. Because our patients were treated many years ago, we wanted to compare our results with the results of those times. Subjective satisfaction in our series was high, although many patients had mild or moderate pain; 81% of the patients were very satisfied or satisfied. Our observations were similar to those of Adamson and Tibone [1], (70%), Cofield et al. [5] (92%), Hawkins et al. [17] (94%) and Jost et al. [18] (85%). In contrast, the senior author reported excellent or good subjective results after 3.5 years followup in only 35% of the patients treated between 1969 and 1980 [36].
At the final followup, the average age of our study population was 72 years. In the general population of similar age, the prevalence of asymptomatic full-thickness rotator cuff tears ranges from 28% to 51% [26, 28]. In our study, aging may explain a considerable proportion of the decrease in absolute values of ROM and strength during 20 years of followup. Kuhlman et al. [23] reported there are substantial differences in strength between younger and older men attributable to aging. The average age of the participants in our study increased from 52 years at surgery to 72 years at followup. Thus, the age- and gender-adjusted Constant-Murley scores were good, and at the same time, strength decreased more in the contralateral shoulder than in the surgically treated one.
In the elderly, a rotator cuff rupture is largely a degenerative process [13, 15, 29], with its clinical manifestations dependent on rupture size and compensation mechanisms. There appears to be considerable variation in the functional deficit associated with tears, with some patients having full movement and others having considerable limitation, including pseudoparalytic limb. Some authors suggest degeneration is a major cause of rerupture after surgical repair [20]. Some authors have reported high rates of rerupture (range, 20%–54%) [2, 8, 18] with a much shorter followup than ours, with some showing a correlation between rerupture and poorer outcome [11] and some less so [7, 17]. We believe, in large retracted tears with poor tendon material, a free tendon graft may play a beneficial role. However, today we rarely see tears of this type.
We observed the early high functional scores after primary rotator cuff repair or reconstruction do not persist. Alleviation of pain is long-standing in many cases but our data suggest many patients do not experience permanent relief. However, our material is partly historical, because free tendon grafting is seldom necessary today.
Acknowledgments
We thank Professor Kaj Tallroth, MD, PhD, for help in radiographic analysis, Ilkka Helenius, MD, PhD, for statistical analysis, and Carol Norris, PhD, for language revision.
Appendix
Footnotes
One or more of the author (NB) have received funding from the Finnish Orthopaedic and Traumatology Research Foundation.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at ORTON Orthopaedic Hospital.
References
- 1.Adamson G, Tibone J. Ten-year assessment of primary rotator cuff repairs. J Shoulder Elbow Surg. 1993;2:57–63. doi: 10.1016/1058-2746(93)90001-W. [DOI] [PubMed] [Google Scholar]
- 2.Bigliani LU, Cordasco FA, McIlveen S, Musso ES. Operative treatment of failed repairs of the rotator cuff. J Bone Joint Surg Am. 1992;74:1505–1515. [PubMed] [Google Scholar]
- 3.Bonsell S, Pearsall AW, 4th, Heitman RJ, Helms CA, Major NM, Speer KP. The relationship of age, gender, and degenerative changes observed on radiographs of the shoulder in asymptomatic individuals. J Bone Joint Surg Br. 2000;82:1135–1139. doi: 10.1302/0301-620X.82B8.10631. [DOI] [PubMed] [Google Scholar]
- 4.Borgmästars N, Remes V, Lohman M, Tallroth K, Vastamäki M. Kiertäjäkalvosimen repeämän leikkaushoidon pitkäaikaistulokset: alustava analyysi 75 potilaan pitkäaikaisseurannasta [in Finnish] Suomen Ortopedia ja Traumatologia. 2006;29:325–330. [Google Scholar]
- 5.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears: a prospective long-term study. J Bone Joint Surg Am. 2001;83:71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 7.Debeyre J, Patte D, Elmelik E. Repair of ruptures of the rotator cuff of the shoulder. J Bone Joint Surg Br. 1965;47:36–42. [PubMed] [Google Scholar]
- 8.Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14:121–127. doi: 10.1016/j.jse.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Ellman H, Hanker G, Bayer M. Repair of the rotator cuff: end-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 10.Fealy S, April EW, Khazzam M, Armengol-Barallat J, Bigliani LU. The coracoacromial ligament: morphology and study of acromial enthesopathy. J Shoulder Elbow Surg. 2005;14:542–548. doi: 10.1016/j.jse.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Galatz LM, Griggs S, Cameron BD, Iannotti JP. Prospective longitudinal analysis of postoperative shoulder function: a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2001;83:1052–1056. [PubMed] [Google Scholar]
- 12.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43–53. [PubMed] [Google Scholar]
- 13.Goutallier D, Postel JM, Radier C, Bernageau J, Zilber S. Long-term functional and structural outcome in patients with intact repairs 1 year after open transosseous rotator cuff repair. J Shoulder Elbow Surg. 2009;18:521–528. doi: 10.1016/j.jse.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff: correlation of functional results with integrity of cuff. J Bone Joint Surg Am. 1991;73:982–989. [PubMed] [Google Scholar]
- 15.Hashimoto T, Nobuhara K, Hamada T. Pathologic evidence of degeneration as a primary cause of rotator cuff tear. Clin Orthop Relat Res. 2003;415:111–120. doi: 10.1097/01.blo.0000092974.12414.22. [DOI] [PubMed] [Google Scholar]
- 16.Hattrup SJ. Rotator cuff repair: relevance of patient age. J Shoulder Elbow Surg. 1995;4:95–100. doi: 10.1016/S1058-2746(05)80061-8. [DOI] [PubMed] [Google Scholar]
- 17.Hawkins RJ, Misamore GW, Hobeika PE. Surgery for full-thickness rotator cuff tears. J Bone Joint Surg Am. 1985;67:1349–1355. [PubMed] [Google Scholar]
- 18.Jost B, Pfirrmann CW, Gerber C. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82:304–314. doi: 10.1302/0301-620X.82B2 .10931. [DOI] [PubMed] [Google Scholar]
- 19.Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88:472–479. doi: 10.2106/JBJS.E.00003. [DOI] [PubMed] [Google Scholar]
- 20.Kannus P, Jozsa L. Histopathological changes preceding spontaneous rupture of a tendon: a controlled study of 891 patients. J Bone Joint Surg Am. 1991;73:1507–1525. [PubMed] [Google Scholar]
- 21.Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14:279–285. doi: 10.1016/j.jse.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Klepps S, Bishop J, Lin J, Cahlon O, Strauss A, Hayes P, Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722. doi: 10.1177/0363546504265262. [DOI] [PubMed] [Google Scholar]
- 23.Kuhlman JR, Iannotti JP, Kelly MJ, Riegler FX, Gevaert ML, Ergin TM. Isokinetic and isometric measurement of strength of external rotation and abduction of the shoulder. J Bone Joint Surg Am. 1992;74:1320–1333. [PubMed] [Google Scholar]
- 24.Lähteenmäki HE, Virolainen P, Hiltunen A, Heikkilä J, Nelimarkka OI. Results of early operative treatment of rotator cuff tears with acute symptoms. J Shoulder Elbow Surg. 2006;15:148–153. doi: 10.1016/j.jse.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 25.Matsen FA. Simple Shoulder Test. February 10, 2005. Available at: http://www.orthop.washington.edu/shoulder_elbow/technical/shouldertest/01. Accessed April 24, 2005.
- 26.Matthews TJ, Hand GC, Rees JL, Athanasou NA, Carr AJ. Pathology of the torn rotator cuff tendon: reduction in potential for repair as tear size increases. J Bone Joint Surg Br. 2006;88:489–495. doi: 10.1302/0301-620X.88B4.16845. [DOI] [PubMed] [Google Scholar]
- 27.Moseley HF. Examination of the shoulder. In: Moseley HF, ed. Shoulder Lesions. Ed 3. Edinburgh, UK: Churchill Livingstone; 1972:22–30.
- 28.Murray TF, Jr, Lajtai G, Mileski RM, Snyder SJ. Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to 6-year follow-up. J Shoulder Elbow Surg. 2002;11:19–24. doi: 10.1067/mse.2002.120142. [DOI] [PubMed] [Google Scholar]
- 29.Neer CS., 2nd Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 30.Petersson CJ, Redlund-Johnell I. Radiographic joint space in normal acromioclavicular joints. Acta Orthop Scand. 1983;54:431–433. doi: 10.3109/17453678308996596. [DOI] [PubMed] [Google Scholar]
- 31.Polgar S, Thomas SA, eds. Section 4: Data collection: questionnaire design. Introduction to Research in the Health Sciences. Ed 2. Melbourne, Australia: Churchill Livingstone; 1991:114–119.
- 32.Romeo AA, Hang DW, Bach BR, Jr, Shott S. Repair of full thickness rotator cuff tears: gender, age, and other factors affecting outcome. Clin Orthop Relat Res. 1999;367:243–255. doi: 10.1097/00003086-199910000-00031. [DOI] [PubMed] [Google Scholar]
- 33.Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456–460. [PubMed] [Google Scholar]
- 34.Solonen KA, Vastamaki M. Reconstruction of the rotator cuff. Int Orthop. 1983;7:49–53. doi: 10.1007/BF00267559. [DOI] [PubMed] [Google Scholar]
- 35.Sperling JW, Cofield RH, Schleck C. Rotator cuff repair in patients fifty years of age and younger. J Bone Joint Surg Am. 2004;86:2212–2215. doi: 10.2106/00004623-200410000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Vastamäki M. Rupture of the Rotator Cuff: Operative Repair. An Analysis of 128 Consecutive Cases [thesis]. Helsinki, Finland: Proceedings of the Orthopaedic Hospital of the Invalid Foundation. 1983;Supplement 1;1–112. (ISBN 951-99469-1).
- 37.Wolfgang GL. Surgical repair of tears of the rotator cuff of the shoulder: factors influencing the result. J Bone Joint Surg Am. 1974;56:14–26. [PubMed] [Google Scholar]
- 38.Worland RL, Arredondo J, Angles F, Lopez-Jimenez F. Repair of massive rotator cuff tears in patients older than 70 years. J Shoulder Elbow Surg. 1999;8:26–30. doi: 10.1016/S1058-2746(99)90050-2. [DOI] [PubMed] [Google Scholar]


