Abstract
Objective
To determine the training needs and interests of volunteer pharmacy preceptors.
Methods
Volunteer preceptors (n=576) were surveyed on various aspects of precepting and their needs related to additional training.
Results
Two hundred thirty-six preceptors (40.9%) responded. Preceptors were less confident about enforcing attendance policies, identifying and managing unmotivated or failing students, identifying dishonesty or plagiarism, and handling conflict. While only 29.5% of respondents agreed that having an APPE student decreased their overall workload, approximately half (48.1%) indicated that student pharmacists helped them complete their daily tasks and 67.8% agreed that APPE students extended patient care. Respondents who had received training were significantly more confident than preceptors who had not received training in their abilities to clarify expectations, evaluate a student's knowledge, and foster skills related to critical thinking and problem solving.
Conclusions
Training programs for pharmacy preceptors are effective; however, important areas in which additional training is needed or desired were identified among both new and experienced preceptors.
Keywords: advanced pharmacy practice experience, continuing education, faculty development, preceptors
INTRODUCTION
A substantial portion of the doctor of pharmacy (PharmD) curriculum is devoted to experiential education, and colleges and schools rely heavily upon preceptors' knowledge, skills, and experience to help students identify their learning needs and to develop the competencies required for practice. Often these preceptors are volunteer faculty members. To ensure that these pharmacists are prepared for their role as preceptors of introductory and advanced pharmacy practice experiences (IPPEs and APPEs, respectively), colleges and schools provide faculty development programs, as mandated by the Accreditation Council for Pharmacy Education (ACPE).1 Preceptor development programs should ideally assist individual pharmacists with the integration of clinical practice and precepting, and provide the knowledge, skills, and resources required to effectively and efficiently mentor and assess student pharmacists in experiential educational settings. In addition, programs should provide preceptors with opportunities to meet their individual/specific learning needs related to both precepting and academic career development. A comprehensive preceptor development program also could help colleges and schools increase preceptor productivity, satisfaction, and retention.2
To augment live preceptor development programming, the University of California, San Francisco (UCSF) School of Pharmacy developed The Effective Clinical Preceptor continuing education home-study course in 2004. This written course provides new preceptors with information related to the school's educational philosophies, curriculum, and policies. The course also provides new and experienced preceptors with a comprehensive resource for topics related to effective and efficient clinical teaching, including managing different adult learning styles, creating a supportive learning environment, providing effective feedback, identifying and managing poor student performance, and evaluating and assessing students. Since 2004, preceptors have been required to complete this home study course to obtain a faculty appointment (paid or volunteer) with the school.
In contrast to current requirements for continuing professional education,3 The Effective Clinical Preceptor course and the school's live preceptor development programs were not developed based on a structured needs assessment of preceptors. Furthermore, no specific tools designed to identify the development needs of pharmacy preceptors have been described in the literature.
The objective of this study was to survey the school's volunteer preceptors to determine their training needs and desires as they relate to clinical teaching in order to refine The Effective Clinical Preceptor course and to develop and provide targeted, ongoing continuing professional development opportunities.
METHODS
Principles for survey research were verified based on published best practices.4,5 A variety of resources were used to develop domain areas, individual questions, and response options for the survey instrument. Questions related to the preceptors' confidence in precepting students were based upon learning objectives and content from The Effective Clinical Preceptor. Questions related to the preceptors' confidence in evaluating and assessing students were based on Bloom's taxonomy of learning.6 Other sections included questions on preceptors' opinions on incorporating student pharmacists into the workplace, and their experiences and preferences related to preceptor training. A 5-point Likert scale (strongly agree, agree, not sure, disagree, strongly disagree) was used for responses to questions related to confidence or opinions. Preceptor demographic information collected included gender; age; race/ethnicity; educational degrees or certificates obtained; number of years in pharmacy practice, at current APPE site, and precepting UCSF and other students; primary practice setting; and geographic region of practice. Some demographic items were modeled after elements from a national survey of volunteer pharmacy preceptors.7
Survey Monkey (Palo Alto, CA), a Web-based application, was used to develop and administer the survey instrument. The survey instrument and study methods were approved by the UCSF Committee on Human Research. The survey instrument was pilot tested with a small convenience sample of paid and volunteer preceptors and then further refined based on their feedback.
Once finalized, an e-mail containing a link to the online survey instrument was forwarded to program directors for dissemination to volunteer preceptors in 6 regional APPE programs throughout California. Volunteer preceptors were defined as individuals who were not employed by UCSF to teach APPE student pharmacists. Each program director sent the original e-mail message and 2 follow-up reminders over a 4-week period in the fall of 2009. Only volunteer preceptors who had precepted or co-precepted at least 1 student over the past 2 years were included in the study. Paid faculty members who precepted APPEs were excluded. Respondents who completed the survey were eligible to enter a raffle for one of two $50 gift cards, however, survey responses were anonymous.
Survey Monkey tools were used for initial quantitative data analyses. For statistical analysis, responses of “strongly agree” and “agree” were combined into a single “agree” category, while responses of “not sure,” “strongly disagree,” and “disagree” were combined into a single “not sure/disagree” category. Depending on the sample size of the outcome variable, Fisher's exact test or Pearson's chi-square test were conducted using Predictive Analytics SoftWare (PASW) Statistics, 17.0 (SPSS Inc., Chicago, IL) to determine which demographic variables significantly influenced preceptor confidence and perceptions. A p value less than 0.05 was considered significant.
RESULTS
The survey instrument was sent by e-mail to 576 volunteer APPE preceptors. Two hundred forty individuals responded to the e-mail. Of these, 4 respondents opted out of the study and 236 completed all or portions of the survey instrument (overall response rate, 40.9%).
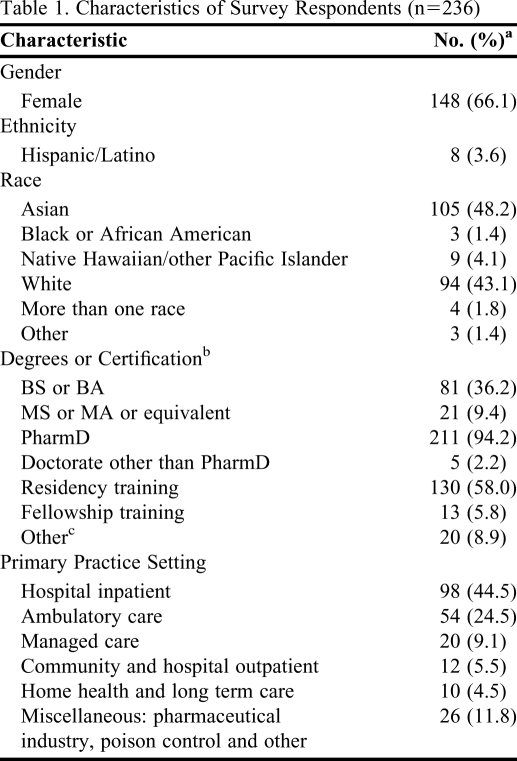
The mean age of the respondents was 40.6 ± 9.2 years (range, 25-70 years), and they had been practicing pharmacy for an average of 14.1 years (range, 1-44 years). Additional characteristics of the survey respondents are summarized in Table 1.
Table 1.
Characteristics of Survey Respondents (n=236)
a Values might not sum to 236 because respondents were not required to answer all questions
b Categories are not mutually exclusive; therefore, totals exceed 100%
c Includes respondents who specified additional certification credentials (eg, board-certified pharmacotherapy specialist, certified geriatrics pharmacist)
In addition to precepting UCSF students, the majority of respondents (70.7%) indicated they were current preceptors for other schools of pharmacy in California, including the University of the Pacific (54.9%), the University of Southern California (53.6%), Western University of Health Sciences (43.1%), the University of California, San Diego (15.7%), Touro University (10.5%), and Loma Linda University (8.5%). A smaller percentage (13.7%) indicated they had precepted students from colleges and schools of pharmacy outside of California. On average, respondents reported having 10.4 ± 8.0 years of experience as a preceptor for student pharmacists.
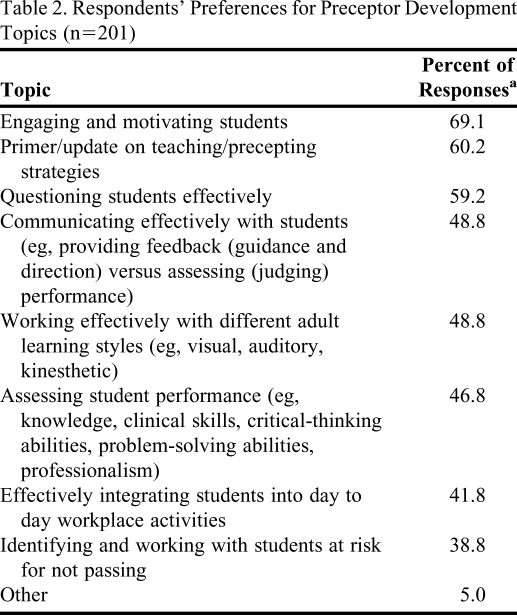
While 78.4% of respondents had received previous preceptor training (eg, through residencies/fellowships, live or written continuing education programs), nearly three quarters (73.5%) expressed interest in obtaining additional training. The respondents' preferences for preceptor development topics are listed in Table 2.
Table 2.
Respondents' Preferences for Preceptor Development Topics (n=201)
a Categories are not mutually exclusive; therefore totals exceed 100%.
The majority of respondents (70.7%) specified interest in attending live preceptor development training programs. Fewer were interested in self-study Web-based courses (55.1%), written training programs (43.9%), or Web-based courses with discussion boards (26.8%). Of those who selected the live training format, 46.0% preferred that the training be offered annually, with topics varying from year to year; while 38.1% preferred multiple training sessions throughout the year with various topics that built upon each other to develop precepting skills. The majority of respondents (71.9%) preferred that live training programs be offered locally, within their region of practice; whereas fewer respondents preferred training programs held in conjunction with state/local professional association meetings (14.4%) or conducted on the UCSF campus (13.7%).
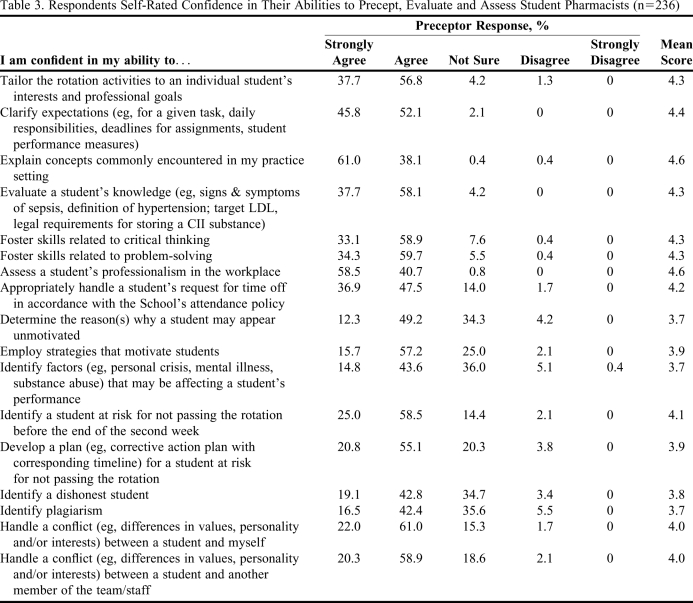
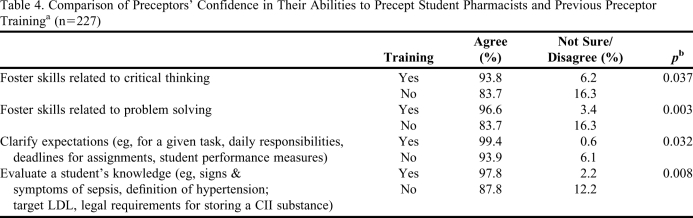
The majority of respondents agreed or strongly agreed that they were confident in their abilities to precept, evaluate, and assess student pharmacists (Table 3). Areas in which respondents were less likely to agree/strongly agree they were confident in their preceptor abilities included: identifying a dishonest student (61.9%), determining the reason(s) why a student may appear unmotivated (61.5%), identifying plagiarism (58.9%), and identifying factors (eg, personal crisis, mental illness, substance abuse) that may be affecting a student's performance (58.4%). When responses were stratified by the respondents' previous exposure to preceptor training programs, significant differences were observed for several areas (Table 4). Respondents who had received formal preceptor training were significantly more confident in their abilities to clarify expectations, evaluate a student's knowledge, and foster skills related to critical thinking and problem solving.
Table 3.
Respondents Self-Rated Confidence in Their Abilities to Precept, Evaluate and Assess Student Pharmacists (n=236)
Abbreviations: LDL = low density lipoprotein
Response scale range: 1=strongly agree to 5=strongly disagree
Table 4.
Comparison of Preceptors' Confidence in Their Abilities to Precept Student Pharmacists and Previous Preceptor Traininga (n=227)
Abbreviations: LDL = low density lipoprotein
Includes training received during a pharmacy residency or fellowship or through completion of a live or written continuing education program.
b Both 1-sided and 2-sided Fisher's Exact tests were performed.
Response scale range: 1=strongly agree to 5=strongly disagree
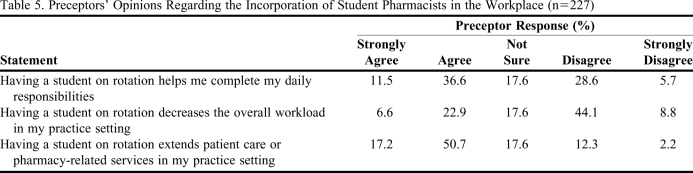
Respondents' opinions regarding the incorporation of students into the workplace are given in Table 5. Almost half (48.1%) of the respondents agreed or strongly agreed that student pharmacists helped them complete their daily responsibilities. Similarly, approximately two-thirds (67.8%) agreed or strongly agreed that student pharmacists extend patient care or pharmacy-related services in the practice setting. A smaller percentage of respondents (29.5%) agreed or strongly agreed that having a student decreased the overall workload in the practice setting; more preceptors (52.9%) disagreed or strongly disagreed with this statement or were unsure (17.6%). Preceptor perceptions regarding the incorporation of students into the workplace were not significantly different when analyzed by the primary pharmacy practice setting, prior preceptor training, or the number of years the preceptor had been practicing as a pharmacist or pharmacy preceptor.
Table 5.
Preceptors' Opinions Regarding the Incorporation of Student Pharmacists in the Workplace (n=227)
Response scale range: 1=strongly agree to 5=strongly disagree
DISCUSSION
Our school has developed and presented a wide variety of preceptor development programs to volunteer faculty members. The topics and content, however, were generally determined based on the information the APPE program directors believed preceptors needed. Few programs were developed based on topics requested by preceptors. For example, many programs were provided to present the revised curriculum so that the preceptors would be aware of the changes and learn their new roles and responsibilities. The primary program and resource for paid and volunteer preceptors is a written self-study module (The Effective Clinical Preceptor), which includes important information about the school and curriculum, the roles and responsibilities of clinical faculty members, effective clinical teaching strategies, and evaluation of student performance. Ideally, preceptor development programs should meet the needs and interests of both the preceptors and the college or school.2 This survey was our first attempt to collect information from volunteer faculty members to determine their confidence and abilities to precept student pharmacists, and to assess their preceptor training needs and interests. The information obtained will assist us to develop future preceptor programs.
When developing preceptor training and enrichment programs, it is important to consider the background and experience of the preceptors. The majority (94.2%) of respondents had a PharmD degree, and over 60% had received residency or fellowship training. Further, almost 80% of respondents had received preceptor training. Some respondents may not have been aware that The Effective Clinical Preceptor program for new preceptors was considered preceptor training. Even among a highly educated and trained group of volunteer preceptors, approximately three quarters were interested in receiving additional preceptor training. “Engaging and motivating students” was the most common topic that respondents selected for future programs, which is provocative given that these preceptors work with APPE students in their last year of professional training.
In general, respondents were very confident in their teaching abilities and responsibilities. They were less confident, however, in some of their administrative responsibilities as an instructor, such as attendance issues, identifying dishonesty or plagiarism, and handling conflict. Respondents who had received preceptor training were significantly more confident than those who had not in their ability to clarify expectations, evaluate a student's knowledge, and foster skills related to critical thinking and problem solving. This information provides potential topics for future preceptor development programs.
Our philosophy has been to inculcate into preceptors that student pharmacists should be resources to them and their institutions, and they should be used as “pharmacist extenders” during their APPEs. This theme has been incorporated in many of the preceptor training programs that we have conducted. Thus, we had great interest in the survey questions regarding this issue. Less than half of the respondents (41.8%) were interested in a future program regarding “effectively integrating students into day-to-day workplace activities.” While only 29.5% of respondents agreed or strongly agreed that having an APPE student in their practice decreased their overall workload, approximately half (48.1%) indicated that student pharmacists helped them complete their daily tasks. This does not necessarily indicate that having an APPE student increased their overall workload. In fact, slightly more than two-thirds (67.8%) of the respondents indicated that student pharmacists extended patient care. A previous study was conducted at a teaching hospital at one of our satellite APPE programs and found that student pharmacists contributed to the productivity of the pharmacy department by performing 42.5% of the initial patient work-ups, 34.0% of the patient information and education episodes, and 24.6% of the in-service programs for physicians.8 Based on these findings, the pharmacy department expanded the APPE program. Other studies have reported that student pharmacists participating in APPEs enhanced care by identifying drug-related issues, suggesting interventions, and documenting patient outcomes.9-12 Thus, student pharmacists may be able to extend patient care by assisting and completing clinical activities that preceptors may not complete due to time constraints or other competing priorities. We believe this is true for non-patient care APPEs as well. When stratified by practice setting (eg, acute care, community practice, managed care, etc), there were no significant differences in the responses regarding the incorporation of students into the workplace due to the small sample sizes in some settings. The ability for student pharmacists to serve as a resource at APPE sites is certainly an advantage to pharmacy colleges and schools, preceptors, and affiliated teaching sites. The results from this survey suggest that we should put further efforts into motivating and training preceptors to use student pharmacists as a resource in future preceptor development programs.
Approximately 70% of respondents indicated that they preferred live preceptor development courses, and that they preferred them to be held locally. This is important feedback for the regional APPE program directors who have conducted many local programs and workshops already. The advantage of this is not only convenience but also the ability to network with other local preceptors and faculty members. Videoconferencing technology also could be used to extend preceptor training by providing interactive programs to APPE sites throughout the state.
Limitations of this study include the response rate of 40.9% and the small sample sizes when we stratified the data by the number of years the respondent had been precepting and by the practice setting. Nonresponse bias prevented us from drawing conclusions regarding the volunteer preceptors as a whole. However, the response rate was significantly higher than that for other preceptor surveys reported, including the annual preceptor survey conducted by the American Association of Colleges of Pharmacy (AACP).13,14
CONCLUSION
This study describes how one school determined their preceptors' training needs and desires related to clinical teaching. We found that preceptors had less confidence and desired additional training in the following: working effectively with different learning styles, engaging and motivating students, and communicating with and questioning students effectively. Preceptors who had received previous training were more confident in clarifying expectations, evaluating a student's knowledge base, and fostering skills related to critical thinking and problem solving. Despite the imperative that feedback from preceptor needs assessments be used to shape continuing faculty development programs, no prior published description of tools, processes, or results was available. Future preceptor development programs should address identified needs and desires and be formatted to reach the largest possible audience based on their preferences for format and venue of continuing professional development programs.
ACKNOWLEDGEMENTS
This study was funded, in part, by the Vince Isnardi Opportunity Fund as a gift to the School of Pharmacy at the University of California, San Francisco. The authors wish to thank and acknowledge Aimee Dawson, PharmD, and Carolyn Victoria, PharmD, who at the time of the study were student pharmacists who contributed to the survey project. In addition, the authors would like to thank Ronna Mallios, PhD, for her contributions to statistical analysis of the data.
REFERENCES
- 1. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Chicago, IL: Accreditation Council for Pharmacy Education: 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed January 5, 2011.
- 2.Boyce EG, Burkiewicz JS, Haase MR, et al. Essential components of a faculty development program for pharmacy practice faculty. Pharmacotherapy. 2008;28(10):145e–268e. doi: 10.1592/phco.29.1.127. [DOI] [PubMed] [Google Scholar]
- 3. Accreditation Council for Pharmacy Education. Accreditation Standards for Continuing Pharmacy Education. Chicago, IL: Accreditation Council for Pharmacy Education: 2007. http://www.acpe-accredit.org/pdf/CPE_Standards_Final.pdf. Accessed January 5, 2011.
- 4.Draugalis JR, Coons SJ, Plaza CM. Best practices for survey research reports: a synopsis for authors and reviewers. Am J Pharm Educ. 2008;72(1) doi: 10.5688/aj720111. Article 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Draugalis JR, Plaza CM. Best practices for survey research reports revisited: implications of target population, probability sampling, and response rate. Am J Pharm Educ. 2009;73(8) doi: 10.5688/aj7308142. Article 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bloom BS. Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook I: Cognitive Domain. New York: Longmans, Green; 1956. [Google Scholar]
- 7.Skrabal MZ, Jones RM, Nemire RE, et al. National survey of volunteer pharmacy preceptors. Am J Pharm Educ. 2008;72(5) doi: 10.5688/aj7205112. Article 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sauer BL, Heeren DL, Walker RG, King JH, Musallam NA. Computerized documentation of activities of Pharm.D. clerkship students. Am J Health-Syst Pharm. 1997;54(15):1727–1732. doi: 10.1093/ajhp/54.15.1727. [DOI] [PubMed] [Google Scholar]
- 9.Briceland LL, Kane MP, Hamilton RA. Evaluation of patient-care interventions by Pharm.D. clerkship students. Am J Hosp Pharm. 1992;49(5):1130–1132. [PubMed] [Google Scholar]
- 10.Slaughter RL, Erickson SR, Thomson PA. Clinical interventions provided by doctor of pharmacy students. Ann Pharmacother. 1994;28(5):665–670. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 11.Skrabal MZ, Kahaleh AA, Nemire RE, et al. Preceptors' perspectives on benefits of precepting student pharmacists to students, preceptors, and the profession. J Am Pharm Assoc. 2006;46(5):605–612. doi: 10.1331/1544-3191.46.5.605.skrabal. [DOI] [PubMed] [Google Scholar]
- 12.Dennehy CE, Kroon LA, Byrne M, Koda-Kimble MA. Increase in number and diversity of clinical interventions by Pharm D students over a clerkship rotation. Am J Pharm Educ. 1998;62(4):373–379. [Google Scholar]
- 13. American Association of Colleges of Pharmacy. Pharmacy preceptor survey summary report - 2009. http://www.aacp.org/resources/research/institutionalresearch/Documents/2009_Preceptor_Summary_All%20Schools_56.pdf. Accessed January 5, 2011.
- 14. American Association of Colleges of Pharmacy. Pharmacy preceptor survey summary 2009 report – public schools. http://www.aacp.org/resources/research/institutionalresearch/Documents/2009_Preceptor_Summary_public_32.pdf. Accessed January 5, 2011.