Abstract
Objective
To measure agreement between advanced pharmacy practice experience students using a guided interview process and experienced clinical pharmacists using standard practices to identify drug therapy problems.
Methods
Student pharmacists enrolled in an advanced pharmacy practice experience (APPE) and clinical pharmacists conducted medication therapy management interviews to identify drug therapy problems in elderly patients recruited from the community. Student pharmacists used a guided interview tool, while clinical pharmacists' interviews were conducted using their usual and customary practices. Student pharmacists also were surveyed to determine their perceptions of the interview tool.
Results
Fair to moderate agreement was observed on student and clinical pharmacists' identification of 4 of 7 drug therapy problems. Of those, agreement was significantly higher than chance for 3 drug therapy problems (adverse drug reaction, dosage too high, and needs additional drug therapy) and not significant for 1 (unnecessary drug therapy). Students strongly agreed that the interview tool was useful but agreed less strongly on recommending its use in practice.
Conclusions
The guided interview process served as a useful teaching aid to assist student pharmacists to identify drug therapy problems.
Keywords: guided interview, drug therapy, advanced pharmacy practice experience, interview, medication therapy management
INTRODUCTION
Odedina and colleagues found that perceived behavioral control, behavioral intention, and past behaviors were important predictors of a pharmacist's intention to try to implement a more patient-centered practice. The authors called for future studies to operationalize “trying” behaviors to implement a new practice model. Instrumental acts and motivational processes form the steps involved in Trying Theory.1 Instrumental acts consist of 3 implementation processes: (1) planning, (2) monitoring, and (3) guidance and control. In their conclusions, Odedina and colleagues recommended that training programs provide opportunities for pharmacists to gain “recent” experience in the desired, new practice to improve their self-efficacy, beliefs, and intentions to try to implement a patient-centered practice.
Pharmacists must gather patient-specific medical and drug histories competently, evaluate the data collected, identify and prioritize a patient's drug therapy problem(s), develop and implement a care plan, and monitor the outcomes achieved to practice patient-centered pharmacy.2 These steps operationalize the implementation processes of planning, monitoring, and guidance and control. A guided interview process can be used to inculcate these skills in student pharmacists. Several practice tools, such as guided data collection forms, have been proposed to assist development of such expertise.
Documentation and screening tools have been published in both the peer-reviewed and non-peer-reviewed literature.3-13 Collectively, these instruments are widely variable in their design and intended uses. Using a guided interview form may help student pharmacists gain confidence and competence in interviewing patients and identifying drug therapy problems. The model developed by Odedina and colleagues suggests that with repeated practice using a guided interview process, novice (eg, student) pharmacists will become more competent in such skills; however, there is a dearth of peer-reviewed evidence demonstrating the effectiveness of the guided interview process in facilitating the identification of drug therapy problems in experiential practice settings.
Integral to patient-centered pharmacy practice is the process of collecting a patient's history to find and resolve the 7 types of drug therapy problems: no indication for drug therapy; dosage too high; dosage too low; wrong drug (also referred to as ineffective drug); adverse drug reaction; inappropriate compliance; and needs additional drug therapy.6,14 Teaching student pharmacists to identify and resolve drug therapy problems is relevant to both ambulatory and inpatient practice settings and is consistent with recent practice trends and requirements.
Medication therapy management services should include a systematic process of collecting patient-specific information, assessing drug therapy to identify medication-related problems, prioritizing such problems, and creating a care plan to resolve them.15 In addition, Guideline 12.1 of the Accreditation Council for Pharmacy Education Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree states that “graduates are competent to provide patient-centered care, through the ability to design, implement, monitor, evaluate, and adjust pharmacy care plans that are patient-specific; address health literacy, cultural diversity, and behavioral psychosocial issues; and are evidence-based.”16 This study specifically measured agreement between the findings of student pharmacists using a guided interview process and those of experienced clinical pharmacists using their usual and customary practices to identify the presence of drug therapy problems in community-dwelling, older patients. As secondary objectives, student pharmacists' perceptions of the guided interview tool and patients' perceptions of pharmacists' interviews also were measured.
METHODS
Using a cross-sectional design, consenting patients participated in face-to-face medication therapy management reviews performed by student pharmacists in the second half of their APPEs and experienced clinical pharmacists during a single office visit. The clinical pharmacists all held doctor of pharmacy (PharmD) degrees and were clinical faculty members at the same college of pharmacy. Two clinical pharmacists had completed an accredited first-year residency, and the third had been in clinical practice for over 5 years. Patient interviews were performed independently and sequentially by the students or clinical pharmacists in a randomly assigned order to minimize systematic sequencing bias. The total combined time spent on both student and clinical pharmacists' interviews was 2 hours or less for each patient. Student pharmacists used a guided interview tool, whereas clinical pharmacists' interviews were based on their usual and customary practices. The clinical pharmacists' interviews served as the reference standard for clinical practice. Agreement between student and clinical pharmacists regarding the number and type of drug therapy problems was evaluated and reported. Student pharmacists' perceptions of the guided interview tool and patients' perceptions of the interview with the pharmacist also were assessed. The study was approved by the Drake University Institutional Review Board.
Interview Process
During the interview process, student pharmacists used the guided interview tool (a paper form) to gather a medication history, perform a review of general medication safety (eg, allergies), and determine the need for additional therapy. After completing the initial assessment, student pharmacists reviewed the indication, safety, compliance, efficacy, and cost for each of the 4 medications they determined to be of highest priority using the guided interview tool. The number of medications reviewed by the student was limited to 4 to reduce patient fatigue in the study sample of elderly patients. Per protocol, student and clinical pharmacists were given the freedom to determine which medications were the highest priority for review. Therefore, the student and clinical pharmacist did not necessarily assess the same drugs for a given patient.
The questions in the guided interview tool were linked to specific drug therapy problems. For example, to evaluate whether the drug therapy problem of inappropriate compliance existed, the student pharmacist was prompted by the form to ask questions, such as whether the patient found it difficult to pay for medications, ever refilled his/her prescriptions late, or had ever considered discontinuing the medication. For most questions, the student pharmacist then documented the answer as yes, no, or unsure. Questions answered yes or no suggested the presence/absence of the problem, respectively. In such cases, the student pharmacist documented on the included checklist whether the problem did not exist or chose from several suggested interventions to resolve the problem (eg, “Use a device to help you remember to take your medication.”). Questions answered as unsure were intended to trigger the student pharmacist to probe with follow-up questions that more definitively identify the presence/absence of a given drug therapy problem.
Participants
Patient participants were recruited from a community-dwelling patient population at 3 ambulatory care practice sites in Polk County, IA. Patients ≥ 65 years of age who were taking at least 4 prescription medications and had no conditions precluding them from effectively communicating with study personnel in English were targeted for recruitment. Patients were offered a $50 grocery store gift card as reimbursement for the time they spent participating in the interviews. Student pharmacists were recruited from the 3 experiential ambulatory care practice sites where the patients were recruited and the clinical pharmacists worked. Student pharmacists were offered a $25 grocery store gift card for their participation.
Measurements
Separate data collection forms were used for each interview to ensure independent data collection by the students and clinical pharmacists. Patient demographics (date of birth, sex, race/ethnicity); a medical problem list; drug therapy problem list; the number, type, and priority of drug therapy problems; and a medication list associated with the highest priority drug therapy problem were recorded by the first interviewer. With the exception of patient demographics, the second interviewer completed the same clinical information categories as the first interviewer. Interviewers identified themselves as a student or clinical pharmacist on their respective data collection forms. All data collection forms were placed in sealed envelopes and returned to the principal investigators for data entry and analysis. Subsequent to completing all data collection forms, the student and clinical pharmacist who interviewed a patient met to discuss that patient's case and adjudicate drug therapy problems consistent with accepted clinical practice.
After completing all of their interviews, each student pharmacist was asked to complete a brief survey instrument about their experience using the guided interview tool during the guided interview process. Four statements using a 5-point Likert-type agreement scale (1 = strongly disagree and 5 = strongly agree) allowed student pharmacists to express their perceptions about the interview tool's ease of use, usefulness in practice, and practicality, and recommend whether the tool should be used in community pharmacy practice.
A 4-item survey instrument with a 5-point Likert-type rating scale (1 = strongly disagree and 5 = strongly agree) was used to assess patients' perceptions of the interview process. Statements were derived and adapted from a previously validated questionnaire related to patient satisfaction with pharmaceutical care.17 Statements were related to the pharmacist's effort to: (1) improve or maintain health; (2) ensure that medications were doing what they were intended to do; (3) help in managing medications; and (4) solve problems with medications. Patients were not asked to discern any differences between the students' and clinical pharmacists' interviews.
Analysis
Data from completed case report forms were entered into a relational database and exported to Stata Version 10.1 (Stata Corp, College Station, TX) for analysis. Descriptive statistics were used to profile the study patient participants regarding demographic characteristics, most important medical problem identified, number of medications used (including prescription, nonprescription, vitamins, herbals, samples, etc), and the number and type of drug therapy problems identified. To address the first research objective, the proportion of patients classified by the student and clinical pharmacist as having each of the 7 drug therapy problems was determined. Agreement between the students' and clinical pharmacists' classification of the presence of each drug therapy problem was evaluated by describing the proportion of cases with observed agreement, and calculating the kappa statistic with a 95% confidence interval (CI).18,19 CIs containing 0 were interpreted as not significant. The kappa statistic is represented as a fraction (ie, actual agreement beyond chance/potential agreement beyond chance) and falls between -1 and 1. Kappa is interpreted according to common guidelines as poor (≤ 0), slight (> 0 – 0.2), fair (> 0.2 – 0.4), moderate (> 0.4 – 0.6), substantial (> 0.6 – 0.8), and almost perfect (> 0.8 – 1). To address the second and third research objectives, student pharmacists' perceptions about the use of the guided interview tool and study patient participants' perceptions about their interview experience were profiled using descriptive statistics.
RESULTS
Sixty-two patients, 30 student pharmacists, and 3 experienced clinical pharmacists participated in this study. Although 64 patients were recruited and consented to participate in the study, only 62 had complete data and were included in the analysis. The study sample was predominantly white, with a similar number of men and women. Participants' mean age was 74.6 years and ranged from 62.9 to 87.9 years. Two participants less than 65 years of age were enrolled in the study and retained for analysis given their close proximity to 65 years of age.
Clinical pharmacists reported a higher median number of medications (12; range 4-25 versus 11; range 4-21) and drug therapy problems (3; range 0-6 versus 2; range 0-5) compared to student pharmacists. The most important medical problems associated with patients' drug therapy problems also were identified by student and clinical pharmacists (Table 1).
Table 1.
Most Important Medical Problems Identified in Patient Interviews
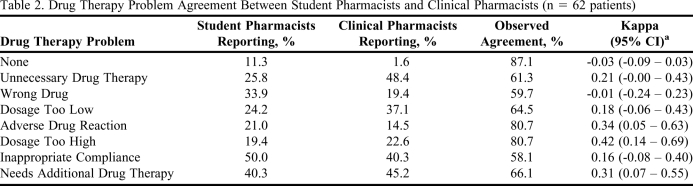
The types of drug therapy problems identified by the students and the clinical pharmacists are reported in Table 2. Compared to the clinical pharmacists, student pharmacists were more likely to report no drug therapy problem, wrong drug (also known as ineffective drug), adverse drug reaction, and inappropriate compliance. Clinical pharmacists were more likely than the student pharmacists to report unnecessary drug therapy, dosage too low, dosage too high, and the need for additional therapy.
Table 2.
Drug Therapy Problem Agreement Between Student Pharmacists and Clinical Pharmacists (n = 62 patients)
a Confidence intervals containing 0 are considered not significant.
The highest observed agreement between the student and clinical pharmacists was related to no drug therapy problem (87.1%), followed by adverse drug reaction (80.7%), dosage too high (80.7%), and needs additional drug therapy (66.1%) (Table 2). With the exception of no drug therapy problem, the observed agreement for each of these problems was significantly higher than the expected agreement. Kappa statistics ranged from slight for inappropriate compliance (k = 0.16, 95% CI: -0.08 – 0.40), to fair for needs additional drug therapy (k = 0.31, 95% CI: 0.07 – 0.55), to moderate for dosage too high (k = 0.42, 95% CI: 0.14 – 0.69). Thirty student pharmacists completed the assessment of their experience with the interview tool. They reported the highest level of agreement with the statement that the interview tool was easy to use (3.7), followed by the statement that the interview tool was useful in the practice environment in which it was used (3.4). The student pharmacists reported less agreement with the statement that the interview tool was practical in the practice environment in which it was used (3.1) and the statement that they would recommend its use in a community pharmacy practice setting (3.1). The observed alpha reliability of the 4-item student perceptions scale was 0.88.
Sixty of the 62 patients provided their perceptions of the guided interview process. They strongly agreed that the pharmacists' efforts would help to: improve or maintain their health (4.8); ensure that their medications were doing what they were intended to do (4.8); manage their medications (4.8); and solve problems with their medications (4.8). The observed alpha reliability of the 4-item patient perceptions scale was 0.95.
DISCUSSION
This study reports the agreement between student pharmacists using a guided interview process and experienced clinical pharmacists in identifying drug therapy problems in a sample of community-dwelling elderly patients. Differences in the types of drug therapy problems reported by student and clinical pharmacists were observed. In addition, fair to moderate agreement on 4 of the 7 drug therapy problems studied was observed. The level of agreement was significant for 3 of the 4 drug therapy problems (adverse drug reaction; dosage too high; needs additional drug therapy).
The authors anticipated that most student pharmacists would readily report the drug therapy problems of wrong drug/ineffective drug, adverse drug reaction, and inappropriate compliance, because the knowledge to identify these problems is taught early in pharmacy school and reinforced throughout the curriculum. Medications have definitive indications, approved uses, and commonly associated risk profiles. Thus, a wrong drug or adverse drug reaction may be identified by comparing the patient medical problem list to the drug information found in most textbooks or compendia. Relying on patients' self-reporting of their medication-taking behavior also may be suggestive of a less complex task because it can be easily confirmed by reviewing a computerized medication profile. In contrast, refining a drug therapy plan may require discontinuation or addition of a drug as well as dosage adjustments, and thus requires more complex decision-making skills. The problems of dose too high, dose too low, needing additional drug therapy, or having no indication for drug therapy require significant clinical judgment and are less likely to be identified by simply comparing an indication or dosage suggestion to what the patient is actually taking. Therefore, these problems would be expected to be reported less frequently by student pharmacists and more frequently by experienced clinicians, as was observed in this study.
Observing that a greater than chance agreement existed for student pharmacists' identification of 3 drug therapy problems was encouraging (ie, adverse drug reaction, dosage too high, and needs additional drug therapy). Differentiating between an adverse drug reaction and a patient who has a problem caused by a dose being too high can be difficult. The clinician must assess the temporality of the event and consider the issues that would be involved with a drug rechallenge as well as the dose-response effects of the drug.20 The significant agreement observed on identification of these 2 drug therapy problems in this study suggests that the guided interview process may help discern the differences between these problems. Determining whether a patient actually requires drug therapy (ie, need for additional drug therapy) is probably the most complex problem to identify because pharmacists must integrate everything they know about the patient's drug therapy and the patient's social history, as well as considerable knowledge of pathophysiology and pharmacotherapeutics. Significant agreement on this drug therapy problem suggests that the guided interview process may have encouraged the student pharmacists to provide a more complete assessment of their patient's drug therapy needs.
In this study, the guided interview process appeared to facilitate the instrumental acts of trying as described by Odedina et al.1 The guided interview process directs a pharmacist to plan an interview effectively, allows for monitoring of the pharmacist's activities by supervisors or mentors, and guides the pharmacist in determining what to do and how to do it.
The time burden/inconvenience of using the guided interview tool must be balanced against the practicality of its use. Because a new form had to be used for every medication evaluated by the student pharmacists, there were concerns that the tool might not be practical for routine use, but better serve as a training tool. Student pharmacists' perceptions of the tool suggested these concerns were well founded. Although student pharmacists found the guided interview tool to be useful and easy to use, they were less likely to recommend that the tool be adopted for routine use in a community pharmacy practice.
Accordingly, the guided interview tool may be of particular value in teaching student pharmacists how to identify drug therapy problems, especially complex ones. The guided interview tool also may be useful to include in training, residency, and/or quality improvement programs for practitioners who lack the clinical experience to identify more complex drug therapy problems.
Patients expressed considerable satisfaction with the pharmacists' interviews. Although no effort was made to differentiate between student pharmacists' and clinical pharmacists' interviews, patients reported that the interaction with a pharmacist would improve or maintain their health, ensure that their medications do what they are supposed to do, manage their medications, and solve problems with their medications. Training pharmacists to use a guided interview process may reinforce patients' positive perceptions of pharmacists' patient-centered services.
Limitations
This study included a small number of patients in 3 ambulatory clinic pharmacy settings in Polk County, IA. Studying the guided interview process in more diverse patient samples and settings are necessary. Given that the median number of medications patients were taking was between 11 and 12, the level of observed agreement is likely to be lower than expected as, in the interest of time, student pharmacists were restricted to using the guided interview process for only 4 medications. If the guided interview process were used for all medications, observed agreement would likely be higher. Moreover, multiple drug therapy problems may have been identified for a given patient, making it difficult to discern medications specific to each drug therapy problem. Data collection in future research should be more specific to capture this important information.
The study design did not include a student pharmacist group not using the guided interview process. This would have required a factorial design and necessitated that each patient be interviewed 3 times, and likely would have imposed an undue burden on the study sample of elderly adults.
The clinical practice skills of student pharmacists in APPEs should improve during the experiential year and this factor could introduce bias. Data were gathered by students during the last half of their experiential year to control for this possibility. Also, clinical pharmacists may possess different skill levels. Therefore, only 3 clinical faculty members with similar experience and practice settings were included in the research study.
Student pharmacists' perceptions about the practicality of the guided interview process may be a function of the study methods rather than the guided interview process. Student pharmacists were instructed to use the guided interview tool for each of the 4 medications reviewed. Thus, they were required to ask all medication assessment questions 4 times. Had students used the screening questions to evaluate all the patient's medications simultaneously, they may have found the guided interview process to be more practical for routine use. However, the ability of a student pharmacist to integrate all information simultaneously is limited and develops over time with guided experience. Thus, the guided interview tool may assist with refining these skills. Finally, while the guided interview tool is comprehensive, adhering strictly to the protocol and script of the study may have resulted in missed opportunities that may have been identified if additional questions had been used. This limitation is underscored by the finding that student pharmacists were more likely than clinical pharmacists to report that a patient had no drug therapy problems.
Conclusions
The guided interview process may assist student pharmacists in identifying drug therapy problems more effectively. An improved ability to identify drug therapy problems will allow pharmacists to provide more effective patient-centered care. Additionally, the guided interview process may be useful as a teaching aid.
ACKNOWLEDGEMENTS
This study was funded by the Community Pharmacy Foundation and the John R. Ellis Research Endowment. We gratefully acknowledge the contributions of Harry Hagel, MS, RPh, for his work in the original design of the guided interview tool.
REFERENCES
- 1.Odedina FT, Hepler CD, Segal R, Miller D. The pharmacists' implementation of the pharmaceutical care (PIPC) model. Pharm Res. 1997;14(2):135–144. doi: 10.1023/a:1012032223328. [DOI] [PubMed] [Google Scholar]
- 2.Rovers JP. Patient data collection. In: Rovers JP, Currie JD, editors. A Practical Guide to Pharmaceutical Care: A Clinical Skills Primer. 3rd ed. Washington DC: American Pharmacists Association; 2007. pp. 47–88. [Google Scholar]
- 3.Strand LM, Cipolle RJ, Morley PC. Documenting the clinical pharmacists' activities: back to basics. Drug Intell Clin Pharm. 1988;22(1):63–67. doi: 10.1177/106002808802200116. [DOI] [PubMed] [Google Scholar]
- 4.Bennett M, Jacobson-Wedret JE. Building a Successful Collaborative Pharmacy Practice: Guidelines and Tools. Washington DC: American Pharmacists Association; 2004. [Google Scholar]
- 5.Goode J-V, Roman LM, Weitzel KW. Community Pharmacy Practice Case Studies. Washington DC: American Pharmacists Association; 2009. [Google Scholar]
- 6.Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: The Clinician's Guide. 2nd ed. New York, NY: McGraw-Hill; 2004. pp. 119–170. [Google Scholar]
- 7.Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice. New York, NY: McGraw-Hill; 1998. pp. 121–175. [Google Scholar]
- 8.Kassam R, Farris KB, Cox CE, et al. Tools used to help community pharmacists implement comprehensive pharmaceutical care. J Am Pharm Assoc. 1999;39(6):843–856. [PubMed] [Google Scholar]
- 9.Farris KB, Kassam R, Cox CE, Volume CI, Tessier G. Evaluation of a practice enhancement program to implement pharmaceutical care. Am J Pharm Educ. 1999;63(3):277–284. [Google Scholar]
- 10.Levy HB. Self-administered medication-risk questionnaire in an elderly population. Ann Pharmacother. 2003;37(7):982–987. doi: 10.1345/aph.1C305. [DOI] [PubMed] [Google Scholar]
- 11.Paulino EM, Bouvy ML, Gastelurrtia MA, Guerreiro M. Drug related problems identified by European community pharmacists in patients discharged from hospital. Pharm World Sci. 2004;26(6):353–360. [PubMed] [Google Scholar]
- 12.Gordon KJ, Smith FJ, Dhillon S. The development and validation of a screening tool for the identification of patients experiencing medication-related problems. Int J Pharm Pract. 2005;13(3):187–193. [Google Scholar]
- 13.Hugtenburg JG, Blom AThG Gopie CTW, Beckeringh JJ. Communicating with patients the second time they present their prescription at the pharmacy. Pharm World Sci. 2004;26(6):328–332. doi: 10.1007/s11096-004-0560-9. [DOI] [PubMed] [Google Scholar]
- 14.Strand LM, Morley PC, Cipolle RJ, Ramsey R, Lamsam GD. Drug related problems: their structure and function. DICP Ann Pharmacother. 1990;24(11):1093–1097. doi: 10.1177/106002809002401114. [DOI] [PubMed] [Google Scholar]
- 15.Anon. Medication therapy management in pharmacy practice: core elements of an MTM service model (version 2.0) JAPhA. 2008;48(3):341–353. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 16. Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. The Accreditation Council for Pharmacy Education, Inc., 2007. http://www.acpe-accredit.org/standards/default.asp Accessed January 12, 2011.
- 17.Larson LN, Rovers JP, MacKeigan LD. Patient satisfaction with pharmaceutical care: update of a validated instrument. J Am Pharm Assoc. 2002;42(1):44–50. doi: 10.1331/108658002763538062. [DOI] [PubMed] [Google Scholar]
- 18.Sim J, Wright CC. The kappa statistic in reliability studies: use of interpretation and sample size requirements. Phys Ther. 2005;85(3):257–268. [PubMed] [Google Scholar]
- 19.Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical Epidemiology – A Basic Science for Clinical Medicine. 2nd ed. Boston, MA: Little Brown and Co; 1985. p. 30. [Google Scholar]
- 20.Frick P, Cohen LG, Rovers JP. Algorithms used in adverse drug event reports: a comparative study. Ann Pharmacother. 1997;31(2):164–167. doi: 10.1177/106002809703100205. [DOI] [PubMed] [Google Scholar]