Abstract
Objective
To implement a simulation-based educational experience focused on medical emergencies in an ambulatory pharmacy setting.
Design
Second-year student pharmacists were assigned randomly to groups and played the role of pharmacists in a community pharmacy setting in which a simulated patient experienced 1 of 5 emergency scenarios: medication-related allergic reaction, acute asthma attack, hypoglycemia, myocardial infarction, and stroke. The students were expected to use patient assessment techniques to determine which emergency the simulated patient was experiencing and the appropriate intervention. Following each simulation, a debriefing session was conducted.
Assessment
Eighty-two student pharmacists completed the simulation activity. Ninety-three percent of student groups correctly identified the emergency. A post-activity survey instrument was administered, and 83% of responders indicated this activity was effective or very effective.
Conclusion
Simulation of emergencies seen in an ambulatory pharmacy setting allowed students to assert knowledge, practice communication skills, apply assessment techniques, and work as a team in a low-risk environment.
Keywords: patient simulation, community pharmacy, emergency care, ambulatory care
INTRODUCTION
The majority of pharmacists will work in an ambulatory pharmacy setting at some point in their careers1 and thus may encounter a patient having a medical emergency. As future practitioners, student pharmacists also should be prepared to handle emergencies they may encounter when completing advanced pharmacy practice experiences (APPEs) in ambulatory settings. Yet, 116 pharmacy residency candidates stated in onsite interviews that they felt least prepared to handle medical emergencies compared to other areas of pharmacy practice.2 Human patient simulation is one approach to training student pharmacists how to respond to medical emergencies in an ambulatory pharmacy environment. The Accreditation Council for Pharmacy Education (ACPE) has approved the use of simulation to satisfy up to 20% (eg, 60 of the 300-hour requirement) for introductory pharmacy practice experiences (IPPEs).3,4 Thus, human patient simulation could become a more common methodology for providing meaningful patient-focused learning experiences where students can encounter real world patient care scenarios without compromising the care of live patients.
Human patient simulation is used in such medical fields as anesthesiology, critical care, pediatrics, emergency medicine, surgery, trauma, cardiology, nursing, and dentistry.5,6 Pharmacy education also has adopted human patient simulation as a teaching tool.7-9 Basic and complex evaluation and management skills, such as blood pressure assessment, intravenous line insertion, and medication administration, can be taught with simulation. Because simulation scenarios usually are driven by specific patient cases, simulation challenges students to think critically when caring for a patient with a complex medical condition.10 Education with high-fidelity simulators allows educators to provide immediate feedback on student performance with the opportunity for remediation or continued practice until the student performs the task/skill correctly, a controlled environment for students to practice without adverse consequence to their actions, and a variety of realistic experiences permitting students to be exposed to high consequence, low occurrence events like medical emergencies.11
For medical emergencies, human patient simulation has been used to train medical professionals in advanced cardiac life support (ACLS), basic life support (BLS), and patient assessment, including vital signs measurement.7-9,12 In ACLS and BLS scenarios, student pharmacists are placed in a high stress situation where they must apply information previously presented in course lectures. In this environment, students test their knowledge in a safe, learner-centered setting, and have the opportunity to correct deficiencies prior to any real-world experiences.13 To our knowledge, other than BLS training, simulation of medical emergencies in an ambulatory pharmacy setting has not been documented. When a patient has an emergency in an ambulatory setting, even if it is a rare occurrence, student pharmacists must be prepared to respond.
Our program has integrated human patient simulation using a high fidelity manikin into the pharmacy curriculum in the Applied Patient Care course series since 2007. First-year student pharmacists use the manikin to learn about basic physical assessment skills including vital signs, and various heart and lung sounds. During the third year in the curriculum, student pharmacists frequently work with the simulator to experience responding to a wide variety of inpatient issues including Clostridium difficile disease, community-acquired pneumonia, and acute coronary syndrome, as well as code team training. An elective in emergency preparedness also is offered in which student pharmacists have the opportunity to work through a cyanide toxicity case.14 To expand the use of simulation beyond teaching physical assessment skills and acute patient care, an ambulatory pharmacy simulation scenario was developed for second-year students. The simulation scenario was included in the Applied Patient Care III course: Medication Therapy Management. The purpose of this project was to describe and assess the use of human patient simulation to teach management of a variety of medical emergencies that could occur in an ambulatory pharmacy setting.
DESIGN
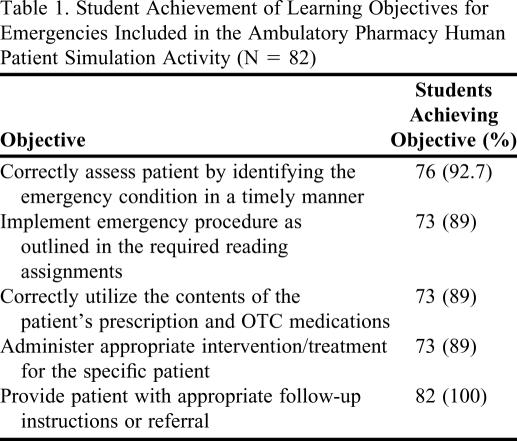
The “Emergencies in the Ambulatory Pharmacy” patient case scenario was developed at an appropriate difficulty level for second-year doctor of pharmacy (PharmD) students. Student pharmacists were expected to use communication and patient assessment skills, and apply relevant content learned from previous coursework on the Top 200 Drugs, pharmacology, and pharmacotherapy to care for a simulated patient appropriately. All of the disease states included in the scenario had been presented to the student pharmacists as part of lectures in various courses in the first- and second-year curriculum prior to the emergencies simulation laboratory. Specific learning objectives identified for this simulation scenario were based on Bloom's taxonomy of learning (Table 1).15
Table 1.
Student Achievement of Learning Objectives for Emergencies Included in the Ambulatory Pharmacy Human Patient Simulation Activity (N = 82)
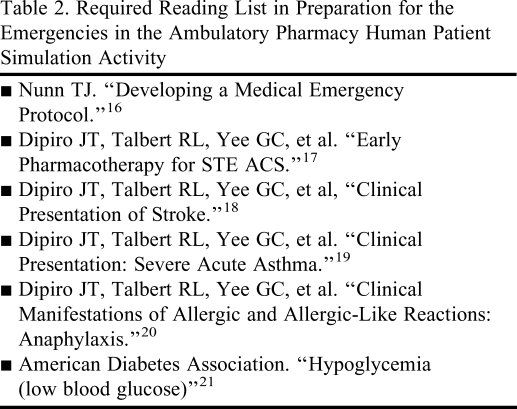
Prior to participating in the scenario, student pharmacists received a laboratory overview that provided them with learning objectives and relevant required readings, which included information on assessment and management of specific emergencies (Table 2).16-21 Additionally, students were instructed to bring the following supplies to the simulation: stethoscope, blood pressure cuff, and pencil. Students also were told to be able to identify correctly and implement the appropriate intervention for the following emergencies: acute chest pain, allergy, asthma, hypoglycemia, and stroke. SimMan (Laerdal Medical Corporation, Wappingers Falls, NY), an advanced patient simulator with realistic anatomy and clinical capability was used for the scenario.
Table 2.
Required Reading List in Preparation for the Emergencies in the Ambulatory Pharmacy Human Patient Simulation Activity
Simulation
Prior to the simulation, students were assigned to preselected groups of 3. Their patient's emergency condition also was assigned randomly but students remained blinded to the condition. One faculty facilitator was assigned to each group. Facilitator responsibilities included observing the scenario, evaluating group performance, and leading the debriefing session.
The Applied Patient Care laboratory was set up to simulate a community pharmacy setting, and included a pharmacy counter, prescription and nonprescription medications, prescriptions ready to be picked up, and a computer with prescription profile information. As the students entered the setting, they randomly were assigned the roles of counseling pharmacist, pharmacist checking refills at the end of his/her shift, and pharmacist just starting his/her shift at the pharmacy. The counseling pharmacist was instructed to be the initial contact for the patient. The other 2 group members were instructed to assist as needed.
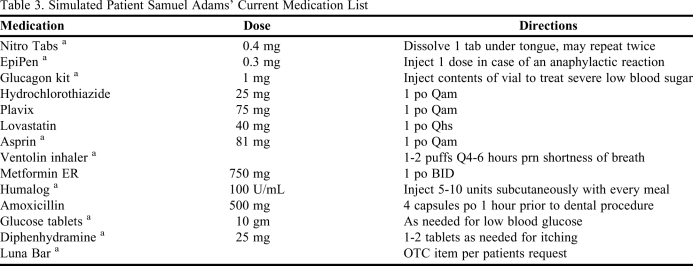
The simulated patient, Mr. Samuel Adams, a 55-year old white male, was dropped off at the community pharmacy to pick up his refills. He was seated in a wheel chair. Mr. Adams was allergic to penicillin (rash) and bee stings (anaphylaxis). His past medical history included hypertension, diabetes, and asthma. His medication profile is shown in Table 3. Each scenario began the same way with Mr. Adams at the counter speaking with the student pharmacist about how to correctly use an inhaler. As the student pharmacist counseled Mr. Adams he began complaining of not feeling well, at which point, the student pharmacists evaluated Mr. Adams' condition. The students clarified his acute symptoms, which varied depending on the assigned emergency; reviewed his current medications, medical conditions, allergies, and past medical history; and conducted a relevant physical assessment which included monitoring of blood pressure, pulse, respirations, lung sounds, and blood glucose. From this evaluation, the student pharmacists determined the type and severity of the medical emergency. Once identified, it became their responsibility to implement the appropriate intervention. Appropriate interventions varied depending on the patient's condition, but could include administering the patient's own medications, calling for emergency services, and/or monitoring the patient until emergency responders arrived on the scene. In addition to addressing Mr. Adams' acute emergency, when appropriate, the student pharmacists provided the patient with follow-up information for referral or education. Each group spent 15 to 20 minutes actively engaged in the scenario. At the end of the scenario, the group moved to a conference room for the debriefing session.
Table 3.
Simulated Patient Samuel Adams' Current Medication List
a Medication was prepared for pick-up to use during the simulation.
Debriefing
During debriefing, student pharmacists were asked to reflect on their individual roles and performances, evaluate the effectiveness of the team, review the learning objectives, and discuss the clinical points of the case. The simulation was graded as a pass or remediate activity. Based on the stated learning objectives for the scenario, student groups were expected to demonstrate competency in 2 areas: (1) correctly identify the emergency, and (2) initiate appropriate medical treatment for the patient. If a group did not demonstrate competency in both areas, the entire group was required to participate in another scenario where they experienced a different emergency condition. Following the debriefing session, students moved to another location and wrote independent subjective, objective, assessment, and plan (SOAP) notes to document the incident. The time limit to complete the SOAP note was 30 minutes.
All simulation activities were assessed by the same 4 faculty members during 2 days of laboratory sessions. A fourth-year student pharmacist functioned as the simulation technician for all groups to maintain consistency and decrease the variability of the students' experiences. One week prior to the laboratory session, the faculty facilitators were provided with the debriefing key/grading rubric and case scenarios. The key/grading rubric's content was previously validated by community pharmacists and educators. To decrease variations in grading, each faculty facilitator participated in a mock scenario with other faculty facilitators. In addition, each faculty facilitator observed a scenario and debriefing conducted by an experienced faculty member prior to independently monitoring and grading student simulations. A new student team started a scenario every 20 minutes. Each facilitator monitored a scenario (20 minutes), conducted the debriefing (20 minutes), and then took a break (40 minutes) to complete grading and prepare for the next group. The educational protocol was reviewed by the University Institutional Review Board and determined to be exempt from further review.
EVALUATION AND ASSESSMENT
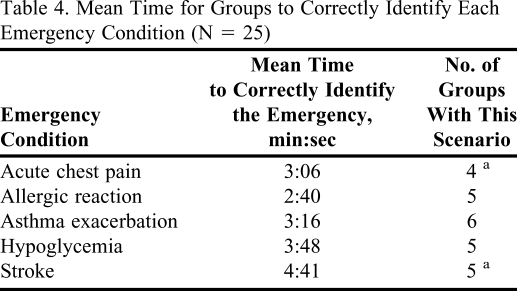
Eighty-two student pharmacists completed the simulation, debriefing, and SOAP note activities. Table 1 shows the rates at which each learning objective was achieved. The emergency was correctly identified by 25 of 27 groups (93%). The mean time to correctly identify the emergency was shortest for the allergic reaction emergency and longest for the stroke emergency (Table 4). One group indicated that the patient was having a stroke when he reported symptoms of acute chest pain. Another group initially assessed the patient as having a stroke, but then changed the assessment to acute chest pain, which was the correct condition.
Table 4.
Mean Time for Groups to Correctly Identify Each Emergency Condition (N = 25)
aThe student group that did not correctly identify this emergency was not included in the calculation of mean time to identify the emergency.
When administering treatment, 24 of 27 groups (89%) managed the patient appropriately. Appropriate treatment consisted of a timely assessment according to the patient's signs and symptoms, and administration of treatment or patient referral based on current guidelines. Two of the groups initiated/recommended the wrong treatment for the patient due to an inaccurate assessment (stroke and acute chest pain scenarios). One group correctly identified acute chest pain, but did not treat the patient according to current guidelines outlined in the required readings. Seventy-one of the students (87%) completed a competent SOAP note. Of the 11 students who did not reach competency with the SOAP note, 2 were in groups that also were required to remediate the simulation.
In the week following the simulation scenario, an anonymous post-laboratory survey instrument was administered to students to obtain feedback about learning through human patient simulation. Of 82 students, 41 survey instruments were returned for a 50% response rate. The survey instrument included the following items: (1) indicate 1 important skill and/or concept that you learned from the Emergencies in the Ambulatory Pharmacy human patient simulation laboratory; (2) indicate how we can make the Emergencies in the Ambulatory Pharmacy human patient simulation laboratory better in the future; (3) rate the Emergencies in the Ambulatory Pharmacy laboratory and indicate the degree to which you feel this laboratory helped you apply the information.
For item 1 on the survey instrument, 42 responses were collected. The comments were categorized into 5 separate themes: knowledge, teamwork, patient assessment, importance of remaining calm, and other. The skill or concept that was most commonly cited was the use of patient assessment skills (33%), followed by knowledge (21%), the importance of remaining calm (20%), other (16.5%), and teamwork (9.5%). Results of survey item 3 demonstrated that a majority of the survey respondents found the laboratory to be effective (51.2%) and very effective (31.7%), while only 2.4% of the students surveyed found the laboratory to be not effective. Recorded comments reflected that “the lab simulated a real-life situation and was a great opportunity to learn,” and that “communication and teamwork” are integral to the process of caring for patients.
DISCUSSION
The purpose of this activity was to use a human patient simulation to immerse student pharmacists in a simulated medical emergency in a community pharmacy setting. Human patient simulation has been used to conduct patient care scenarios in inpatient and acute care settings, and have primarily focused on cardiopulmonary resuscitation and BLS training.6-9,12,14 Other health care disciplines, such as dentistry and pediatrics, have developed training to prepare office personnel to handle medical emergencies.16,22-24 To our knowledge, no pharmacy education literature exists which reports on the use of human patient simulation to prepare student pharmacists for potential medical emergencies in the ambulatory pharmacy setting. This learning activity provided an opportunity for student pharmacists to apply their patient assessment skills in a way that could not be measured by written or multiple-choice examinations.
Because approximately 93% of the student groups correctly identified the medical emergency, and 89% of the student groups initiated the appropriate treatment, the simulation was considered effective in meeting the stated learning objectives. The 2 groups who remediated the activity demonstrated competency during a second scenario. Additionally, the high proportion of students that individually completed the SOAP note correctly indicated that the student pharmacists understood the clinical scenario independent of input from their group members.
In addition to allowing students to assess their ability to apply knowledge, human patient simulation experiences allow students to practice such patient care skills as empathy and compassion. Fink's taxonomy of significant learning emphasizes the importance of integrating this human dimension and caring into academic education.25 Fink's taxonomy is an expansion of Bloom's taxonomy.15 Within Fink's taxonomy, students are challenged to look beyond simply acquiring and applying knowledge by also evaluating their roles in interacting with patients and peers. Using human patient simulation with a community-based simulated patient allowed student pharmacists to experience the caring, compassion, and ethical issues involved in patient care. Observing the student pharmacists interact during the simulation indicated that they considered Mr. Adams' medical emergency as something more than just a simple patient case scenario. To make Mr. Adams comfortable, various techniques were initiated independently by the student pharmacists. For example, one student removed her laboratory coat and placed it on Mr. Adams' lap after Mr. Adams complained of being cold. Because Mr. Adams was in a wheelchair, many student pharmacists kneeled next to him so they could be at eye level while talking with him. Chairs were moved for students to sit next to Mr. Adams to help calm him down. One student sat and held Mr. Adams' hand while waiting for emergency services to arrive. In debriefing, the students acknowledged the compassion and caring that team members showed during the simulation.
In the debriefing sessions, students reflected on the simulation and on what areas they as a group or as individuals could improve. Many different issues were identified: (1) students recognized that they tended to develop “tunnel vision” with the initial assessment of the patient (if Mr. Adams' initial complaints seemed related to one of the outlined emergencies, the students would hone in on that specific issue prior to ruling out other possible causes); (2) allergies were often not reviewed or questioned even if allergy status was pertinent to the case; (3) in a few instances, 911 was called before the patient was showing true signs of distress (ie, the patient reported that he was itchy and emergency services were requested); (4) in some scenarios, the cause of the medical emergency was not determined so the patient was not educated on how to prevent the same issue in the future. For example, a possible cause of the patient's hypoglycemia could have been a low carbohydrate intake at breakfast with his insulin dose. During the debriefings, students were able to articulate the importance of patient education along with proper treatment of the medical emergency in the community setting.
During the debriefings, student pharmacists indicated that they were unclear about which assigned roles were expected to interact with the patient when he started exhibiting concerning symptoms. Although we specified that the counseling pharmacist would have the initial contact with the patient, we did not tell the students who was in charge of the patient assessment once it became apparent there was a problem, as we wanted to see who would step forward and take the lead. In real life, the specific roles that pharmacists and other employees would have in an emergency would not be predefined. The lack of predefined leadership roles allowed us to see how the team members assumed leadership in the simulation.
This simulation exercise could be translatable to other institutions and settings. If a pharmacy program wanted to incorporate a module covering the management of a medical emergency in the ambulatory pharmacy setting, it would be possible, even without a high fidelity simulator. A standardized patient could replace the simulator and would allow the participants to practice their verbal assessment skills. The advantage of using a high fidelity simulator is that students can use physical assessment skills (blood pressure, pulse, respirations, lung sounds) set to specific parameters to assess the emergency. Special consideration should be given to legal limitations and practice guidelines for participants' roles during the scenario. For example, within this scenario, according to Washington State law, a pharmacist can assist a patient in administering the patient's own medications, but cannot administer nonprescribed medications to the patient, as that would exceed the scope of practice for a pharmacist (could be considered prescribing by the Revised Code of Washington, 18.64.011). In addition to being used in a pharmacy setting, this emergencies in the ambulatory setting scenario potentially could be useful for training in nursing, medicine, dental, and physical/occupational therapy settings, and in school systems (elementary through postsecondary).
As with every new educational activity, adjustments will be made in the future. During the simulations, the voice responses from the simulator were sometimes delayed, and in some instances the inflection or tone of the voice response was inappropriate for the question. To help resolve these issues, we will either reorganize our prerecorded responses into a more user-friendly format or have the simulation operator respond to questions live via a microphone during the simulation.
CONCLUSION
Using human patient simulation to introduce an ambulatory pharmacy-based emergency scenario immersed the student pharmacists in a stressful situation that challenged them in various ways. Throughout the experience the students relied upon patient assessment techniques, communication skills, therapeutic knowledge application, and teamwork. During debriefing, the student pharmacists determined where gaps in care and in their individual and group performances occurred, and identified strategies for changing behaviors to improve care in the future. ACPE allows colleges and schools of pharmacy to use simulation for IPPEs when the simulation experiences meet specific criteria. One guideline noted that simulations are to be appropriate for high risk, low occurrence medical situations such as cardiopulmonary resuscitation, medical emergencies, and medication errors.4 The Emergencies in the Ambulatory Pharmacy scenario is an example of the type of activity that should qualify as appropriate for IPPE credit.
REFERENCES
- 1. Bureau of Labor Statistics, US Department of Labor. Occupational Outlook Handbook, 2010-2011 ed. Pharmacists. http://www.bls.gov/oco/ocos079.htm. Accessed May 17, 2010.
- 2.Garris K, Wellein MG, Wessell A, Ragucci D, Blair MM. First-year residency candidates' experience in various areas of pharmacy practice. Am J Pharm Educ. 2008;72(1) doi: 10.5688/aj720106. Article 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Chicago, Ill: 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed April 22, 2010.
- 4. ACPE. Addendum #1 Clarifications of Current Standards 1.3 Simulations for Introductory Pharmacy Practice Experiences.32-34(28-30CS) Approved June 2010. http://www.acpe-accredit.org/pdf/cs_policiesandprocedures.pdf Accessed September 14, 2010.
- 5.Rosen KR. The history of medical simulation. J Crit Care. 2008;23(2):157–166. doi: 10.1016/j.jcrc.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Pacsi AL. Human simulator in nursing education. J NY State Nurses Assoc. Fall/Winter 2008-2009:8–11. [PubMed] [Google Scholar]
- 7.Mieure KD, Vincent WR, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740222. Article 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710348. Article 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720237. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Good ML. Patient simulation for training basic and advanced clinical skills. Med Educ. 2003;37(S1):14–21. doi: 10.1046/j.1365-2923.37.s1.6.x. [DOI] [PubMed] [Google Scholar]
- 11.Issenberg SB, McGaghie WC, Petrusa ER, Gorgon DL, Scalese RJ. Features and uses of high-fidelity medical simulation that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 12.Bjørshol CA, Lindner TW, Søreide E, Moen L, Sunde K. Hospital employees improve basic life support skills and confidence with a personal resuscitation manikin and a 24-min video instruction. Resuscitation. 2009;80(8):898–902. doi: 10.1016/j.resuscitation.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 13.Gordon JA, Wilkerson WM, Shaffer DW, Armstrong EG. Practicing medicine without risk: students' and educators' responses to high-fidelity patient simulation. Acad Med. 2001;76(5):469–472. doi: 10.1097/00001888-200105000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Willson M, Bray BS, Terriff C, Garrison MW. Abstract ACCP: Anaheim, CA; 2009. Integration of a human patient simulation mannequin into a doctor of pharmacy curriculum. [Google Scholar]
- 15.Bloom BS. Taxonomy of Educational Objectives, Handbook I: The Cognitive Domain. New York, NY: David McKay; 1956. [Google Scholar]
- 16.Nunn TJ. Developing a medical emergency protocol. Access. 2006:12–15. [Google Scholar]
- 17.Dipiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy: A Pathophysiologic Approach. New York, NY: McGraw Hill Medical; 2008. Early Pharmacotherapy for STE ACS; p. 255. Table 18-1 and 18-4. [Google Scholar]
- 18.Dipiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy: A Pathophysiologic Approach. New York, NY: McGraw Hill Medical; 2008. Clinical presentation of stroke; p. 375. [Google Scholar]
- 19.Dipiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy: A Pathophysiologic Approach. New York, NY: McGraw Hill Medical; 2008. Clinical presentation: severe acute asthma. 469 and Table 28-6. [Google Scholar]
- 20.Dipiro JT, Talbert RL, Yee GC, et al. Pharmacotherapy: A Pathophysiologic Approach. New York, NY: McGraw Hill Medical; 2008. Clinical manifestations of allergic and allergic-like reactions: anaphylaxis; pp. 1451–1456. [Google Scholar]
- 21. Hypoglycemia: American Diabetes Association; http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/hypoglycemia-low-blood.html. Accessed December 10, 2010.
- 22. American Academy of Pediatrics. Preparation for Emergencies in the Offices of Pediatricians and Pediatric Primary Care Providers. http://www.pediatrics.org/cgi/content/full/120/1/200. Accessed October 27, 2010.
- 23.Toback SL, Fiedor M, Kilpela B, Reis EC. Impact of a pediatric primary care office-based mock code program on physician and staff confidence to perform life-saving skills. Pediatr Emerg Care. 2006;22(6):416–422. doi: 10.1097/01.pec.0000221342.11626.12. [DOI] [PubMed] [Google Scholar]
- 24.Toback SL. Medical emergency preparedness in office practice. Am Fam Physician. 2007;75(11):1679–1684. [PubMed] [Google Scholar]
- 25.Fink LD. Creating Significant Learning Experiences. An Integrated Approach to Designing College Courses. San Francisco, CA: Jossey-Bass; 2003. [Google Scholar]