Abstract
Objective
To analyze the cost avoidance resulting from clinical interventions made by pharmacy students completing an advanced pharmacy practice experience (APPE) at a psychiatric hospital.
Methods
A retrospective database review of documented clinical interventions by pharmacy students was conducted to classify interventions by type and significance. Interventions were assigned a cost avoidance value determined by an evaluation of the literature.
Results
Three hundred-twenty interventions were documented by 15 pharmacy students during the 1-year study period. The majority of interventions were related to psychiatric medication classes and most (n = 197; 61.6%) were classified as being of moderate significance. The most common interventions included patient education (13.1%), order clarification (11.6%), therapeutic dosing adjustments (10.9%), and laboratory order monitoring (8.8%). The estimated cost avoidance from all interventions made by pharmacy students was approximately $23,000.
Conclusions
Pharmacy students completing APPEs at a psychiatric hospital contributed to a variety of significant clinical interventions and provided considerable cost avoidance value to the institution.
Keywords: clinical intervention, pharmacy student, psychiatry, cost avoidance, experiential education
INTRODUCTION
The benefit of clinical pharmacy services has been well established.1-16 Interventions made by pharmacists involved with multidisciplinary treatment teams result in improved medication use, reduction of adverse drug events, improved patient care, and overall cost reduction. Similar benefits of pharmacist involvement have been seen in the psychiatric setting.17-21 The Accreditation Council for Pharmacy Education (ACPE) mandates that students be educated to practice as competent and independent practitioners upon graduation.22 As a result, colleges and schools of pharmacy have developed APPEs for doctor of pharmacy (PharmD) students in their final year of training. The primary purpose of these experiential opportunities is to foster independent thinking, promote self-confidence, teach collaboration within a multidisciplinary team, and encourage practical application of pharmaceutical knowledge. Students are expected to observe and perform many of the same activities as licensed pharmacists while under direct supervision. While the educational gains for students participating in this training are clear, benefits for the host facility remain less obvious. Few studies have evaluated the potential benefit of pharmacy student participation in clinical activities, and only 1 study has attempted to quantify the cost benefit.23-27
The primary objectives of this study were to describe the clinical interventions documented by pharmacy students completing an APPE at an adult inpatient state psychiatric facility and define the benefit, beyond the utilitarian need for training sites, of APPE students in terms of their impact on cost avoidance.
METHODS
Facility
This study was conducted at Western Missouri Mental Health Center (now named The Center for Behavioral Medicine) in Kansas City, MO. The hospital is a 120-bed, state-operated inpatient psychiatric facility consisting of 2 adult acute care units, 1 adult intermediate care unit, a child and adolescent unit, and a psychiatric emergency department. The pharmacy department was comprised of 2 full-time clinical staff pharmacists, 2 school of pharmacy faculty members using the hospital as their practice site, a pharmacy director, and a postgraduate year 2 (PGY2) resident in psychiatric pharmacy practice. The APPE students at the site trained primarily in 1 of the adult acute care units or the intermediate care unit at the center, working with either faculty members or clinical staff pharmacists.
This study, a retrospective database review of clinical pharmacy interventions conducted at the facility between June 1, 2008, and May 31, 2009, was reviewed and approved by the University of Missouri - Kansas City Adult Health Sciences Investigational Review Board and the State of Missouri Department of Mental Health Research and Review Committee. Data were extracted from the pharmacy department's clinical intervention tracking software, Rx Medi-Trend (Pharmacy Systems Inc, Dublin, OH). Although entering interventions into the database was voluntary, all pharmacy personnel were encouraged to do so. Pharmacy students were required to document their interventions in the database as part of the APPE. Data extracted for each intervention included: who documented the intervention (pharmacist, resident, pharmacy student), intervention type, medications involved, physician acceptance, associated cost avoidance, and any additional comments/descriptions. For the purpose of this study, cost avoidance was defined as the reduction or elimination of additional expenditures that otherwise may have been incurred if an intervention had not occurred.
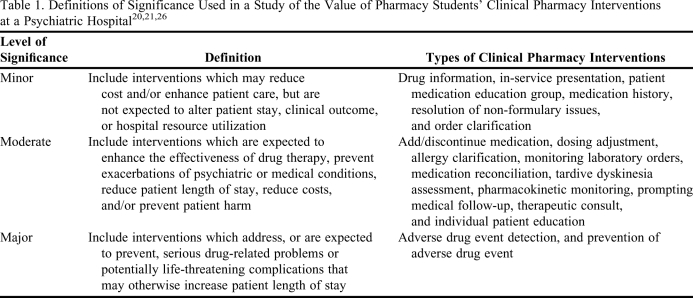
Once extracted, the data were sorted to determine all interventions made by pharmacy students. The type of interventions and medications involved were classified as being either psychiatric or medical in nature. Psychiatric interventions included only activities and medications related to the treatment of an Axis I or Axis II psychiatric disorder according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR).28 Medical interventions included all activities and medications related to an Axis III disorder. Interventions were classified also as minor, moderate, or major in significance based upon their potential impact on patient outcome. The definitions for minor, moderate, and major significance used in this study are found in Table 1. These definitions are based on studies previously published which analyzed the significance of clinical pharmacy interventions.20,21,26 Additionally, Table 1 outlines the various types of interventions evaluated by this study and their assigned significance level. Physician acceptance rate of pharmacy student interventions was also evaluated.
Table 1.
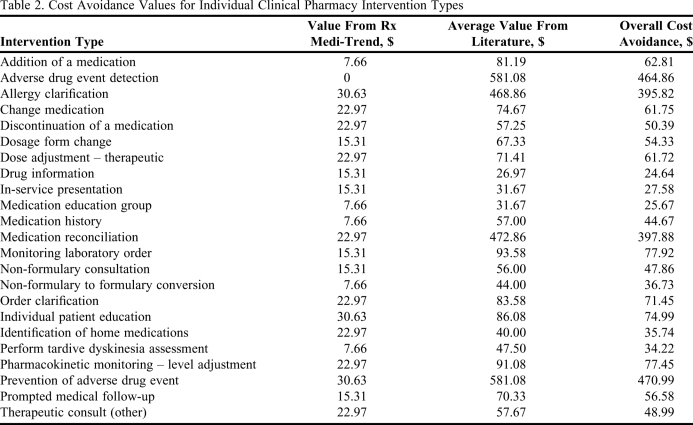
Cost avoidance values used in this study were derived using 2 methods. First, the Rx Medi-Trend system had assigned a predetermined cost avoidance value to all clinical interventions. These values were based on literature reporting the frequency and average cost of an adverse drug event (ADE).29-33 The Rx Medi-Trend system reports the excess hospital cost associated with an ADE to be between $1,939 and $4,685, and occur in 3.1% of all hospital stays. Using this information, the system multiplied the average cost of an ADE by a probability factor, which was a predetermined percent likelihood that an ADE would occur if no intervention had been made. Probability factors were organized into levels ranging from very low probability (1%) to very high probability (10%). Multiplying these values yielded the estimated cost avoidance. However, because our hospital was exclusively a psychiatric facility and had limited resources for providing other services, a fraction of this value was used to calculate cost avoidance. The result was a conservative estimate of the cost avoidance for an intervention.
To increase the validity of these values, a second method for determining cost avoidance was used. This method involved analysis of peer-reviewed literature. A comprehensive MEDLINE search yielded 4 studies which evaluated cost avoidance for different types of clinical pharmacy interventions.26,27,34,35 Each study was reviewed to establish an average cost avoidance value for the types of clinical interventions performed. These studies then were compared and the results averaged with those of Rx Medi-Trend to yield an overall cost avoidance value for each type of clinical intervention. In cases where all resources did not evaluate the same type of intervention, only those studies with a reported value were used. The resulting cost avoidance values for individual clinical pharmacy intervention types are listed in Table 2.
Table 2.
Cost Avoidance Values for Individual Clinical Pharmacy Intervention Types
The primary outcome measures for this study were: (1) to describe the clinical pharmacy interventions documented by pharmacy students during their APPEs at a state psychiatric facility, and (2) to calculate the estimated cost avoidance for the clinical interventions made. The secondary outcome measure of this study was calculation of physician acceptance rates of clinical pharmacy interventions recommended by pharmacy students.
RESULTS
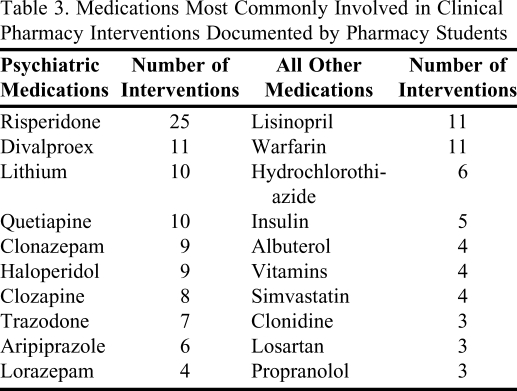
Fifteen pharmacy students documented 320 clinical interventions between June 1, 2008, and May 31, 2009. Students performed APPEs for 8 months out of the 1-year study period. On average, each student documented approximately 21 clinical interventions during an APPE. Of the 320 interventions, 258 (80.6%) were classified as either psychiatric or medical in nature, based on the type of intervention and medications involved. One hundred forty-six of these interventions (45.6%) were classified as psychiatric, and 112 (35.0%) were classified as medical. The remaining 62 interventions (19.4%) were not classified due to lack of information or the nature of the intervention (ie, conducting a patient medication group). Antipsychotics were the most common class of medications involved, and were associated with 68 student interventions. Antihypertensives were the second most common class of medications involved and were listed in 29 separate interventions. Mood stabilizers, antidepressants, and anxiolytics ranked as the next most common medication classes and were involved in 24, 21, and 16 interventions, respectively. The specific medications most commonly involved in clinical pharmacy interventions documented by pharmacy students are listed in Table 3. Only medications with a documented psychiatric or nonpsychiatric indication were included.
Table 3.
Medications Most Commonly Involved in Clinical Pharmacy Interventions Documented by Pharmacy Students
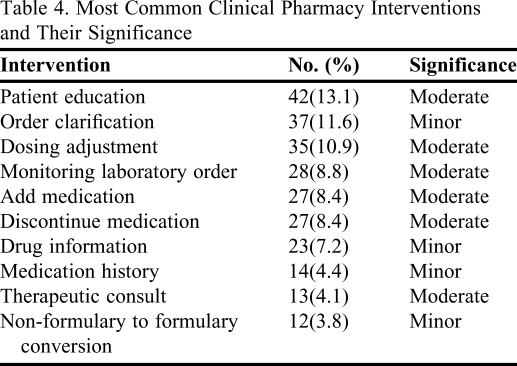
Based on this study's definitions, the majority of interventions (n = 197, 61.6%) documented by pharmacy students were classified as moderate in significance, with an additional 114 (35.6%) interventions considered to be minor in significance. Nine interventions (2.8%) were classified as having major significance and consisted of either detection or prevention of an adverse drug event. A list of the most common types of interventions and their significance is described in Table 4.
Table 4.
Most Common Clinical Pharmacy Interventions and Their Significance
Eighty-three of the 320 clinical interventions made by pharmacy students were for information purposes only and could not be labeled as accepted or rejected by physicians. These interventions included activities such as patient education and providing drug information to staff members. For the remaining 237 clinical interventions documented by students, a physician acceptance rate of 97% was observed. Rejected interventions consisted primarily of student recommendations to add, discontinue, or adjust the dose of a medication.
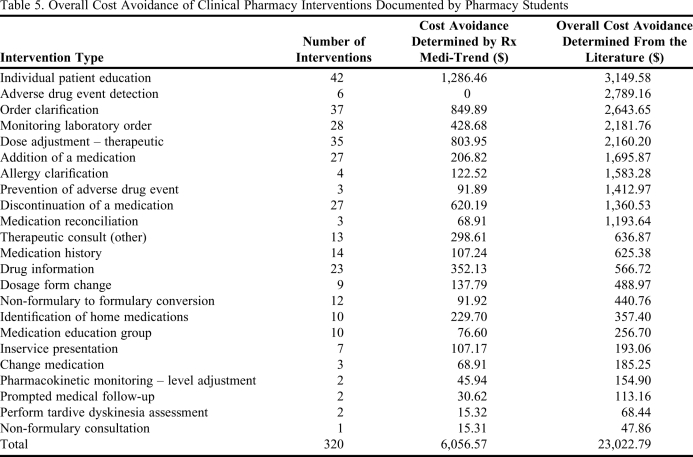
Rx Medi-Trend estimated the cost avoidance of all accepted clinical interventions made by pharmacy students at $6,056, which equates to each pharmacy student saving the center an average of $404. However, when these same interventions were estimated using the average cost avoidance figures generated from the literature, the values nearly quadrupled. The predicted total cost avoidance using the second method of calculation was determined to be $23,023 for all clinical interventions, or approximately $1,535 savings achieved by each student. A comparison of the specific cost avoidance data for both methods of calculation is provided in Table 5.
Table 5.
Overall Cost Avoidance of Clinical Pharmacy Interventions Documented by Pharmacy Students
DISCUSSION
This study is the first to describe in detail the types and associated cost avoidance of clinical pharmacy interventions performed by pharmacy students completing their APPEs at a state psychiatric facility. The types of interventions performed by students were primarily related to the psychiatric specialty setting and focused largely on patient education activities, order clarification, medication dosing adjustments, and laboratory monitoring. These results are not surprising given the patient population served in an inpatient psychiatric facility and the focus on patient counseling and ADE prevention by pharmacy curricula.22
The majority of interventions were considered to be at least moderately significant, meaning that students likely had substantial impact on improving medication management as well as patient outcomes. The rating of intervention types as minor, moderate, or major was based largely on literature from similar studies evaluating these factors.20,21,26 However, investigators felt several types of interventions, most notably order clarifications, should be classified at a lower significance level than that reported in the literature. In the case of order clarification, an intervention often regarded as ADE prevention, consideration was given to the fact that APPE students at our site do not input or verify physician orders. Rather, interventions in this category often are initiated by a pharmacist and passed on to the student before team meetings. Given this, investigators felt the APPE students' impact on patient care was much less than if they had initiated this type of intervention themselves.
The present study also suggests that the contributions made by students during their APPEs yielded substantial economic benefits for the host facility. Using conservative methods for calculating cost avoidance, pharmacy students saved an estimated $6,000 to $24,000 over an 8-month period. This savings benefit, while similar to values reported in other studies, is still comparatively low given the significance of most interventions.23-27 This is due primarily to the extreme subjectivity in calculating cost avoidance values. Because no standardized guidelines for economic evaluation of clinical interventions exist, the ability to generalize results from one study to another is difficult. The methods used for calculating cost savings in this study, while based upon the literature, were kept conservative on purpose. The investigators felt a conservative approach, rather than evaluating costs associated with worst-case scenarios, would provide a more realistic and believable estimation of cost avoidance.
This study had several important limitations. Clinical intervention data were self-reported by students, which introduces a potential for bias in results (ie, reporting of some intervention types may have been inflated while others may have been underreported). This may have contributed to the high physician acceptance rate of pharmacy student interventions. Given that other studies have reported physician acceptance rates of student interventions of 60% to 95%, the probability of a 97% acceptance rate may be an overestimate and the result of decreased reporting of rejected interventions.23,26,27 There could be several reasons for the high acceptance rate. Students may have felt that documenting a rejected intervention in essence was documenting a failure on their part. Another explanation could be the perception of patient harm. For example, if an intervention was rejected but did not pose risk to the patient, students may have been less likely to document it. With respect to the reporting of all interventions, another factor should be considered. APPE students typically spend much of the first week at a new practice site becoming oriented to the facility and may not have had a clear understanding of what was considered a clinical intervention requiring documentation, leading to a decreased reporting of interventions during their first week and overall. Additionally, as documentation of interventions was a required component of this APPE and assessed in their midpoint and final evaluations, the potential for over-documentation existed, especially because students entered their own data into the database.
An additional limitation of the study is inherent to its retrospective design, which did not allow for the evaluation of certain outcomes, such as the impact of physician acceptance of these interventions. For this reason, the actual benefits to patient care made by pharmacy students were difficult to demonstrate. Although no definitive proof can be offered to support that patient care improved as a direct result of student interventions, the data presented in this study suggests a positive impact.
One final consideration is the qualitative description of student interventions. The interventions evaluated in this study were not intended to be an all-inclusive list of student activities. Pharmacy students routinely performed a variety of tasks, such as medication use evaluations, assisting pharmacists with research activities, patient care interactions with other health care professional students, and education of pharmacy staff members through journal club and topic presentations, which indirectly could have had a positive effect on patient care and which were not evaluated by this study. While valuable, these activities do not have an associated cost avoidance value and are difficult to document accurately in an intervention database.
CONCLUSIONS
Clinical interventions made by pharmacy students completing APPEs at a psychiatric hospital were moderately significant and primarily related to medications used in the psychiatric specialty setting. Pharmacy students were able to demonstrate reasonable cost avoidance potential in a relatively short period of time. These results demonstrate there may be an economic benefit to the host facility in providing a practice site for APPEs/precepting APPE students.
REFERENCES
- 1.Knapp KK, Okamoto MP, Black BL. ASHP survey of ambulatory care pharmacy practice in health systems–2004. Am J Health-Syst Pharm. 2005;62(3):274–284. doi: 10.1093/ajhp/62.3.274. [DOI] [PubMed] [Google Scholar]
- 2.Schumock GT, Butler MG, Meek PD, et al. Evidence of the economic benefit of clinical pharmacy services: 1996-2000. Pharmacotherapy. 2003;23(1):113–132. doi: 10.1592/phco.23.1.113.31910. [DOI] [PubMed] [Google Scholar]
- 3.Gattis WA, Hasselbad V, Whellan DJ, et al. Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team: results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) Study. Arch Intern Med. 1999;159(16):1939–1945. doi: 10.1001/archinte.159.16.1939. [DOI] [PubMed] [Google Scholar]
- 4.Taylor CT, Byrd BC, Krueger K. Improving primary care in rural Alabama with a pharmacy initiative. Am J Health-Syst Pharm. 2003;60(11):1123–1129. doi: 10.1093/ajhp/60.11.1123. [DOI] [PubMed] [Google Scholar]
- 5.Perez A, Doloresco F, Hoffman J, et al. Economic evaluations of clinical pharmacy services: 2001-2005. Pharmacotherapy. 2008;28(11):285e–323e. doi: 10.1592/phco.29.1.128. [DOI] [PubMed] [Google Scholar]
- 6.Lee AJ, Boro MS, Knapp KK, et al. Clinical and economic outcomes of pharmacist recommendations in a Veterans Affairs medical center. Am J Health-Syst Pharm. 2002;59(21):2070–2077. doi: 10.1093/ajhp/59.21.2070. [DOI] [PubMed] [Google Scholar]
- 7.Dorevitch A, Perl E. The impact of clinical pharmacy intervention in a psychiatric hospital. J Clin Pharm Ther. 1996;21(1):45–48. doi: 10.1046/j.1365-2710.1996.89575895.x. [DOI] [PubMed] [Google Scholar]
- 8.Powell BJ, Ekkehard O, Sinkhorn C. Pharmacological aftercare for homogeneous groups of patients. Hosp Community Psychiatry. 1977;28(2):125–127. doi: 10.1176/ps.28.2.125. [DOI] [PubMed] [Google Scholar]
- 9.Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):481–493. doi: 10.1592/phco.27.4.481. [DOI] [PubMed] [Google Scholar]
- 10.Leape LL, Cullen DJ, Clapp MD, et al. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282(3) doi: 10.1001/jama.282.3.267. 267–270. Erratum: JAMA. 2000;283(10):1293. [DOI] [PubMed] [Google Scholar]
- 11.Canales PI, Dorson PG, Crismon MI. Outcomes assessment of clinical pharmacy services in a psychiatric inpatient setting. Am J Health-Syst Pharm. 2001;58(14):1309–1316. doi: 10.1093/ajhp/58.14.1309. [DOI] [PubMed] [Google Scholar]
- 12.Suh DC, Woodall BS, Shin SK, Hermes-De Santis ER. Clinical and economic impact of adverse drug reaction in hospitalized patients. Ann Pharmacother. 2000;34(12):1373–1379. doi: 10.1345/aph.10094. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman JM, Meek PD, Touchette DR, et al. Transparent and reproducible reports on economic evaluations of clinical pharmacy services: a goal for the future? Amer J Health-Syst Pharm. 2009;66(5):442–444. doi: 10.2146/ajhp080435. [DOI] [PubMed] [Google Scholar]
- 14.Classen DC, Pestotnik SL, Evans RS, Lloyd JF, Burke JP. Adverse drug events in hospitalized patients: excess length of stay, extra cost, and attributable mortality. JAMA. 1997;227(4):301–306. [PubMed] [Google Scholar]
- 15.Terceros Y, Chahine-Chakhtoura C, Malinowski JE, Rickley WF. Impact of a pharmacy resident on hospital length of stay and drug-related costs. Ann Pharmacother. 2007;41(5):742–747. doi: 10.1345/aph.1H603. [DOI] [PubMed] [Google Scholar]
- 16.De Rijdt T, Willems L, Simoens S. Economic effects of clinical pharmacy interventions: a literature review. Am J Health-Syst Pharm. 2008;65(12):1161–1172. doi: 10.2146/ajhp070506. [DOI] [PubMed] [Google Scholar]
- 17.Dolder C, Symanski B, Wooton T, McKinsey J. Pharmacist interventions in an inpatient geriatric psychiatry unit. Am J Health-Syst Pharm. 2008;65(19):1795–1796. doi: 10.2146/ajhp060448. [DOI] [PubMed] [Google Scholar]
- 18.Finley PR, Crimson ML, Rush AJ. Evaluating the impact of pharmacists in mental health: a systemic review. Pharmacotherapy. 2003;23(12):1634–1644. doi: 10.1592/phco.23.15.1634.31952. [DOI] [PubMed] [Google Scholar]
- 19.Finley PR, Rens HR, Pont JT, et al. Impact of a collaborative pharmacy practice model on the treatment of depression in primary care. Am J Health-Syst Pharm. 2002;59(16):1518–1526. doi: 10.1093/ajhp/59.16.1518. [DOI] [PubMed] [Google Scholar]
- 20.Mutnick AH, Sterba KJ, Peroutka JA, Sloan NE, Beltz EA, Sorenson MK. Cost savings and avoidance from clinical interventions. Am J Health-Syst Pharm. 1997;54(4):392–396. doi: 10.1093/ajhp/54.4.392. [DOI] [PubMed] [Google Scholar]
- 21.Alderman CP. A prospective analysis of clinical pharmacy interventions on an acute psychiatric inpatient unit. J Clin Pharm Ther. 1997;22(1):27–32. doi: 10.1046/j.1365-2710.1997.95975959.x. [DOI] [PubMed] [Google Scholar]
- 22. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program Leading to the Doctor of Pharmacy Degree. Adopted 2007. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards. Accessed December 9, 2010.
- 23.McCollum M, Nuffer W, Ellis SL, Turner CJ. Physician acceptance of pharmacotherapy recommendations made by pharmacy students in a rural pharmacy-based diabetes care and education clinic. Am J Pharm Educ. 2009;73(2) doi: 10.5688/aj730224. Article 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mueller BA, Abel SR. Impact of college of pharmacy-based educational services within the hospital. Ann Pharmacother. 1990;24(4):422–425. doi: 10.1177/106002809002400416. [DOI] [PubMed] [Google Scholar]
- 25.Brockmiller H, Abel SR, Koh-Knox CP, Birk CW. Cost impact of PharmD candidates' drug therapy recommendations. Am J Health-Syst Pharm. 1999;56(9):882–884. doi: 10.1093/ajhp/56.9.882. [DOI] [PubMed] [Google Scholar]
- 26.Taylor CT, Church CO, Byrd DC. Documentation of clinical interventions by pharmacy faculty, residents, and students. Ann Pharmacother. 2000;34(78):843–847. doi: 10.1345/aph.19310. [DOI] [PubMed] [Google Scholar]
- 27.Marino J, Caballeo J, Liosent M, Hinkes R. Differences in pharmacy interventions at a psychiatric hospital: comparison of staff pharmacists, pharmacy faculty, and student pharmacists. Hosp Pharm. 2010;45(4):314–319. [Google Scholar]
- 28. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed. text rev.) Washington, DC: 2000.
- 29.Bates DW, Spell N, Cullen DJ, et al. The costs of adverse drug events in hospitalized patients. JAMA. 1997;277(4):307–311. [PubMed] [Google Scholar]
- 30.Nesbit TW, Shermock KM, Bobek MB, et al. Implementation and pharmacoeconomic analysis of a clinical staff pharmacist practice model. Am J Health-Syst Pharm. 2001;58(9):784–790. doi: 10.1093/ajhp/58.9.784. [DOI] [PubMed] [Google Scholar]
- 31.Moore TJ, Cohen MR, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167(16):1752–1759. doi: 10.1001/archinte.167.16.1752. [DOI] [PubMed] [Google Scholar]
- 32.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. JAMA. 1995;274(6):29–34. [PubMed] [Google Scholar]
- 33.Lazarou J, Pmeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients. JAMA. 1998;279(15):1200–1205. doi: 10.1001/jama.279.15.1200. [DOI] [PubMed] [Google Scholar]
- 34.Patel R, Butler K, Garrett D, Badger N, Cheoun D, Hallman L. The impact of a pharmacist's participation on hospitals' rounds. Hosp Pharm. 2010;45(2):129–134. [Google Scholar]
- 35.Crowson K, Collette D, Dang M, Rittase N. Transformation of a pharmacy department: impact on pharmacist interventions, error prevention, and cost. The Joint Commission. J Qual Improve. 2002;28(6):324–330. doi: 10.1016/s1070-3241(02)28032-3. [DOI] [PubMed] [Google Scholar]