Abstract
Background
This study aimed to evaluate processes from the mutual maintenance model in relation to daily functioning in patients with both chronic pain and a history of a traumatic experience. The mechanism illustrated the structural relations for daily functioning among pain intensity, hyperarousal, re-experiencing, trauma avoidance, and pain avoidance.
Methods
Archival data (N = 214) was used for this study and data were analyzed for 142 chronic pain patients reporting a traumatic experience and seeking treatment at a tertiary pain clinic in Korea.
Results
The results indicated that pain intensity, hyperarousal, and pain avoidance had significant direct effects on daily functioning. Also, pain intensity showed significant indirect effects on daily functioning through hyperarousal and pain avoidance; and hyperarousal through pain avoidance.
Conclusions
Results suggest a direct contribution of high levels of pain, hyperarousal symptoms of PTSD, and pain avoidance behaviors to reduced daily functioning. Also, elevated pain as reminders of the trauma may trigger high levels of hyperarousal symptoms of PTSD. Subsequently, avoidant coping strategies may be used to minimize pain so that the trauma would not be re-experienced, thus inhibiting the activation of hyperarousal symptoms of PTSD. However, prolonged use of such strategies may contribute to decline in daily functioning.
Keywords: chronic pain, daily functioning, Korean, mutual maintenance model, PTSD
INTRODUCTION
There has been growing evidence of the co-occurrence of chronic pain and posttraumatic stress disorder (PTSD) [1,2]. PTSD is conceptualized as a disorder involving three symptom clusters (re-experiencing the trauma, avoidance of reminders and emotional numbing, and hyperarousal) [3]. It has been well known that major impairment in daily functioning (physical and psychological) is often associated with chronic pain [4,5] as well as PTSD [6,7]. However, relatively little research has examined interactions between chronic pain and PTSD [8-10].
Recently, Sharp and Harvey [11] proposed the mutual maintenance model which postulates that PTSD symptoms maintain or exacerbate chronic pain symptoms and vice versa. They suggested the following seven theoretical mechanisms underlying the interaction between chronic pain and PTSD: "attentional and reasoning biases, anxiety sensitivity, reminders of the trauma, avoidance, depression and reduced activity levels, anxiety and pain perception, and cognitive demand from symptoms limiting use of adaptive strategies". A few studies have supported some of these particular mechanisms, for example attentional biases [12,13], and anxiety and pain perception [8,9,14].
Among the posited mechanisms, reminders of the trauma have been considered to activate PTSD symptoms [15]. According to the mutual maintenance model [11], pain may remind individuals of the traumatic event that led to PTSD. Thus, pain may trigger hyperarousal and consequent re-experiencing symptoms which may then lead to behavioral and/or emotional avoidance as coping strategies for managing pain, intrusive memories and feelings about the traumatic event. Accordingly, persistent avoidance behaviors may contribute to low levels of daily functioning. To our knowledge, certain paths within this particular model have been tested in people with chronic pain, PTSD, or both, but the fully integrated model has not been tested in a chronic pain population reporting traumatic experience.
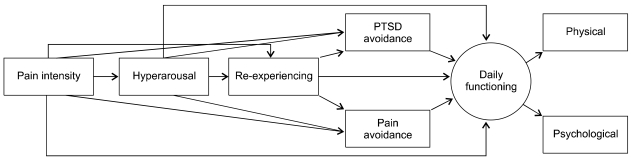
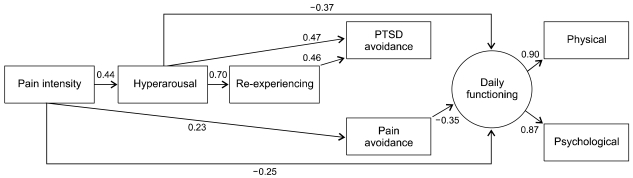
The purpose of the present study was to evaluate the mutual maintenance model [11] in patients with chronic pain reporting traumatic experience. Specifically, the present study examined a structural model illustrating the relations among pain intensity, pain avoidance and PTSD symptoms, for daily functioning. Initially, we generated a full theoretical model (Fig. 1), assuming that all of the study variables have direct and/or indirect effects on daily functioning. Then, we attempted to identify the most parsimonious model with an adequate fitting to the data and without the non-significant path(s).
Fig. 1.
Full theoretical model.
MATERIALS AND METHODS
1. Participants
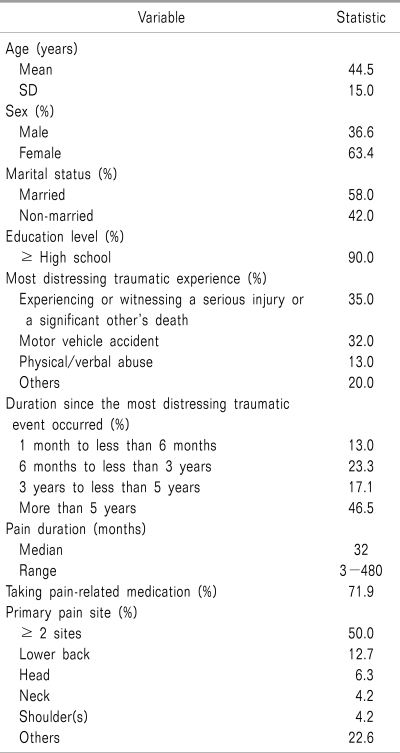
This present study used archival data obtained from the Korean Pain Study: Phase II. The primary objective of this study (Phase II) was to introduce frequently used pain-related questionnaires to Korea and thus develop the infrastructure for research in psychosocial aspects of pain. A total of 214 patients with pain, seeking treatment at a university-based pain management center located in Seoul, Korea participated in this study (Phase II). The inclusion criteria for the present study were having traumatic experiences and pain duration of 3 months or more, resulting in a final sample of 142 patients (63.4% female). The mean age of the sample was 44.5 years (SD = 15.0), the majority were married (58.0%), and most had at least a high school education (90.0%). Demographic characteristics of the sample are presented in Table 1. The inclusion criteria for the present study were having traumatic experience(s) and pain duration of 3 months or more, resulting in a final sample of 142 patients. Demographic characteristics of the sample is presented in Table 1. The entire sample reported that their most distressing traumatic experience involved injury or life threat and intense fear, helplessness, or horror. The entire sample reported that their PTSD symptoms have persisted for more than 1 month. This study (Phase II) was approved by the IRB and informed consent was properly acquired from the study participants.
Table 1.
Demographic Characteristics of the Sample
2. Measures
Pain intensity was measured as current, average, least, and worst, on an 11-point numeric rating scale where 0 represented 'no pain' and 10 'worst pain imaginable.' Total score ranges from 0 to 40, with a higher score indicating greater pain. Psychometric properties of this scale have been well established [16].
Posttraumatic Diagnostic Scale (PDS) [17] is a 49-item self-report measure of assisting the diagnosis of PTSD and consists of four subsections. In the first subsection, the PDS asks respondents to report traumatic event(s) that they have experienced or witnessed. In the second subsection, the PDS asks the respondents to describe the most distressing traumatic event (if two or more traumatic events are indicated) in the past month. In the third subsection, the PDS asks the respondents to indicate the frequency of 17 PTSD symptoms in relation to the most distressing traumatic event. Each item is rated on a 4-point scale where 0 represents 'not at all' and 3 'almost always'. Total score ranges from 0 to 51, with a higher score indicating greater PTSD symptoms. Finally, the PDS asks the respondents to indicate the presence of impairment in life functioning. The PDS has yielded adequate psychometric properties [17]. This study utilized a Korean language version of the PDS (KPDS) which has shown good reliability and validity [18]. Given the purpose of the present study, only the 3 PTSD symptom clusters were entered in the structural equation model.
The Pain Anxiety Symptoms Scale-20 (PASS-20) [19] is a 20-item self-report measure of pain anxiety and consists of four subscales (cognitive anxiety, avoidance behaviors, fear of pain, physiological symptoms). Each item is rated on a 6-point scale where 0 represents 'never' and 5 'always'. Total scores range from 0 to 100, with a higher score indicating greater pain anxiety. The PASS-20 has shown adequate psychometric properties [19,20]. This study utilized a Korean language version of the PASS-20 (KPASS-20) which has been found to have three subscales (fearful thinking, physiological response, avoidance) rather than four. The KPASS-20 has shown good reliabilities and validities in a tertiary pain clinic sample in Korea [21]. Given the purpose of the present study, only the avoidance subscale was used.
The Short Form-36 (SF-36) [22] is a 36-item self-report measure of daily functioning. The SF-36 consists of four physical functioning subscales (physical functioning, role limitation due to physical problems, bodily pain, general health) and four psychological functioning subscales (role limitation due to emotional problems, vitality, social functioning, emotional well-being). Each subscale score can range from 0 to 100, with a higher score indicating greater daily functioning. Also, physical and psychological composite scores can be obtained by averaging all of the scores for four physical functioning and four psychological functioning subscales, respectively [23]. In the present study, two composite scores were employed but the composite score of physical functioning was calculated excluding the bodily pain subscale as pain intensity was used as one of the (observed) variables in the models. The SF-36 has shown good psychometric properties [24,25]. This study employed a Korean language version of the SF-36 (KSF-36), which has shown good reliabilities and validities across clinical [26,27] and non-clinical samples [26].
3. Statistical analyses
The SPSS 17.0 and Amos 7.0 were used for statistical analyses in the present study. Structural equation analysis using maximum likelihood estimation was employed for testing whether the full theoretical model (Fig. 1) for daily functioning has a good-fit to data. When the full theoretical model showed adequate goodness-of-fit indices, we attempted to identify the most parsimonious model with an adequate fit, based on non-significant paths and/or modification indices. The models were evaluated using goodness-of-fit indices which includes root-mean square error of approximation (RMSEA), the comparative fit index (CFI), and the standardized root mean square residual (SRMR). A good fit to the data is indicated for the RMSEA, values below 0.10 [28], for the CFI, values above 0.9 [29], and for the SRMR, values below 0.06 [30]. Chi-square difference tests were performed to compare the full theoretical model and the parsimonious model(s) [31]. Once the most parsimonious model was identified, bootstrapping was used to inspect the significance of the indirect effects in the model [32].
RESULTS
1. Descriptive statistics and correlation analyses
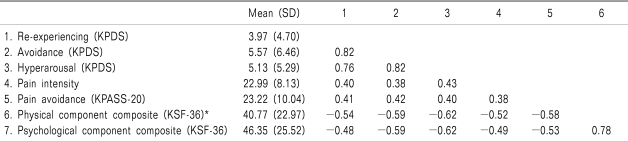
Means and standard deviations of the PTSD symptoms, pain intensity, pain avoidance, and daily functioning scores and their correlations are presented in Table 2. Correlation coefficients indicated that all of the study variables were significantly correlated at P < 0.001. Especially, large correlations were found among 3 PTSD symptom variables (average r = 0.80) and between daily functioning variables (r = 0.78).
Table 2.
Descriptive Statistics and Correlations among Study Variables
All correlations are significant at P < 0.001 KPDS indicates a Korean language version of the Posttraumatic Stress Diagnostic Scale, KPASS-20 indicates a Korean language version of the Pain Anxiety Symptoms Scale KSF-36 indicates a Korean language version of the Short Form-36, *Since pain intensity was used as one of the (observed) variables in the present study, the bodily pain subscale of the KSF-36 was not included inthe physical component composite score.
2. Model testing
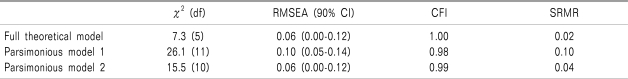
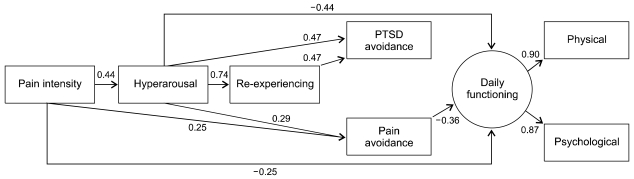
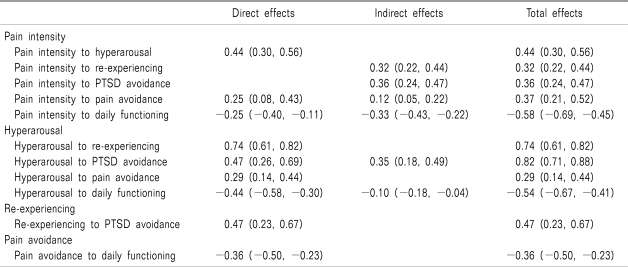
In the first step, the full theoretical model (Fig. 1) was tested for daily functioning. The results indicated that the full theoretical model has adequate goodness-of-fit indices (Table 3). Also, measured variables (physical, psychological) were significantly loaded on their latent variable (i.e., daily functioning), indicating that daily functioning is adequately measured by its measured variables. In the second step, we attempted to identify the most parsimonious model with an adequate fit to the data. The full theoretical model revealed several non-significant paths (defined as P > 0.05) which include pain intensity-to-re-experiencing, pain intensity-to-PTSD avoidance, hyperarousal-to-pain avoidance, re-experiencing-to-pain avoidance, and re-experiencing-to-daily functioning. Thus, in the alternative model (parsimonious model 1) (Fig. 2), these paths were removed. However, this model showed non-adequate goodness-of-fit indices (Table 3). In addition, a chi-square difference test showed a significant difference between the full theoretical model and parsimonious model 1, indicating that the full theoretical model is preferred. Thus, another alternative model (parsimonious model 2) (Fig. 3) was identified based on modification indices which suggest retaining the hyperarousal-to-pain avoidance path. This model yielded adequate goodness-of-fit indices (Table 3) and all paths were significant at P = 0.01 (Fig. 3). Also, a chi-square difference test showed a non-significant difference between the full theoretical model and parsimonious model 2, indicating that the parsimonious model 2 was preferred. Thus, parsimonious model 2 was selected as a final model in the present study.
Table 3.
Goodness-of-fit Indices for the Models
RMSEA: root-mean-square error of approximation, CFI: comparative fit index, SRMR: standardized root mean square residual.
Fig. 2.
Parsimonious model 1. All correlations are significant at P < 0.01.
Fig. 3.
Final model (Parsimonious model 2). All correlations are significant at P < 0.01.
Table 4 presents the direct, indirect, and total effects of the final parsimonious model 2. The findings indicated that the final model shows significant direct effects of pain intensity, hyperarousal, and pain avoidance on daily functioning at P = 0.01, indicating that daily functioning would be reduced as pain, hyperarousal symptoms of PTSD, and pain avoidance behaviors increase. In addition, the final model yielded significant indirect effects of pain intensity through hyperarousal and pain avoidance and hyperarousal through pain avoidance on daily functioning at P = 0.01. However, neither pain intensity nor hyperarousal yielded significant indirect effects on daily functioning through either re-experiencing or PTSD avoidance. These indicated that increased pain would lead to reduced daily functioning, partially due to increased hyperarousal symptoms and pain avoidance behaviors; and increased hyperarousal symptoms would lead to reduced daily functioning, partially due to increased pain avoidance behaviors. In addition, the final model indicated significant total effects of pain intensity, hyperarousal, and pain avoidance on daily functioning at P = 0.01. Pain intensity and hyperarousal were found to have overall strong effects on daily functioning.
Table 4.
Standardized Effects for Final Model (Parsimonious Model 2)
Confidence intervals (90%) are included in parentheses, all effects were significant at P = 0.01.
DISCUSSION
The mutual maintenance model suggests some possible interactive processes between chronic pain and PTSD, contributing to the maintenance or exacerbation of the symptoms of both conditions [11]. The present study examined its relevance for daily functioning where pain serves as a reminder of the traumatic event, which triggers hyperarousal and re-experiencing symptoms of PTSD and consequent avoidance of pain and intrusive memories and feelings about such event, leading to decline in daily functioning among patients with both chronic pain and a history of a traumatic experience. Although certain paths have been examined from among the processes described here in a chronic pain, PTSD, or both populations, no prior studies have tested the full comprehensive theoretical model in a chronic pain population having a history of traumatic experience. Thus, we assumed at first that all study variables may have direct and/or indirect effects on daily functioning (Fig. 1) and then attempted to minimize the model's complexity.
The findings indicated that parsimonious model 2 (Fig. 2) has good fit and advantage over the full theoretical model (Fig. 1) and parsimonious model 1. In parsimonious model 2, pain intensity, hyperarousal, and pain avoidance, but not re-experiencing and trauma avoidance, had the significant direct effects on daily functioning. Also, pain intensity showed the significant indirect effects on daily functioning through hyperarousal and pain avoidance; and hyperarousal through pain avoidance. However, neither pain intensity nor hyperarousal yielded significant indirect effects on daily functioning through either re-experiencing or trauma avoidance. They suggest the direct contribution of high levels of pain, hyperarousal symptoms of PTSD, and pain avoidance behaviors to decline in daily functioning. In addition, elevated pain as reminders of the trauma may trigger high levels of hyperarousal symptoms. Subsequently, avoidant coping strategies may be used to minimize pain so that the trauma would not be reminded, thus inhibiting the activation of hyperarousal symptoms of PTSD. However, prolonged use of such strategies may contribute to decline in daily functioning. Although re-experiencing and trauma avoidance did not show direct and/or indirect effects on daily functioning, overall these structural relations were consistent with the posited theoretical mechanism of the mutual maintenance model [11].
It was noted that the strongest total effects on daily functioning was found for pain intensity (β = -0.58) and hyperarousal (β = -0.54). They suggest that pain and hyperarousal symptoms of PTSD may play a major role in impacting daily functioning among patients with both chronic pain and a history of a traumatic experience. There is significant evidence that pain has negative effects on daily functioning in the pain literature. For example, pain often directly restricts movement and elicits physical and psychological discomfort, and thus interferes with activities of daily living and social activities [33,34]. Also, pain encourages avoidance behaviors by eliciting fear of movement and re-injury. Persistent long-term use of such coping strategies may contribute to physical deconditioning and feed more fear of movement and re-injury, consequently deteriorating daily functioning [35-37]. On the other hand, there is emerging evidence that pain influences daily functioning through hyperarousal symptoms of PTSD and subsequent pain avoidance behaviors. Some of these findings were consistent with a recent study [8] demonstrating marginal interactions between pain intensity and hyperarousal (among other PTSD symptoms) in predicting quality of life. This recent study suggested that high levels of pain may be one of the strongest factors contributing to worsening quality of life, by intensifying hyperarousal symptoms of PTSD. Given this, the findings of the present study imply that in addition to such established features of pain, elevated pain may have additional features of evoking memories of the trauma, thus activating and intensifying hyperarousal symptoms of PTSD in patients with both chronic pain and a history of a traumatic experience. Further studies can clarify this additional feature of pain using an experimental design.
Hyperarousal symptoms of PTSD include the increased physiological arousal (e.g., difficulty sleeping, feeling tense, being easily startled) representing high levels of anxiety. Such symptoms may be adaptive in traumatic situations by getting the body ready for defense, but persistent physiological arousal after the trauma can develop maladaptive patterns of behaviors, emotions, and cognitions, consequently deteriorating daily functioning [38,39]. Interestingly, hyperarousal was found to be the strongest direct path to daily functioning. Given that insomnia is not only one of the major hyperarousal symptoms in a PTSD population [3], but one of the major complaints in a chronic pain population [40], it is possible that cumulative sleep loss from long-term persistent physiological arousal may greatly impact daily functioning [41]. Another interesting finding was that hyperarousal showed no significant indirect effects on daily functioning through either re-experiencing or trauma avoidance, but through pain avoidance. Such findings can be explained by characteristics of the study sample. For example, the total and subscale mean scores and standard deviations of the KPDS were comparable to those obtained from the sub-threshold PTSD group in Korea [18]. This suggests that the study sample may primarily consist of patients with chronic pain who have experienced the traumatic event and consequent some but not enough symptoms of PTSD for a diagnosis. Given this, pain seemed to be a relatively major issue, compared to PTSD, and thus it is possible that avoidance coping strategies for pain reduction and consequent deactivation of hyperarousal symptoms of PTSD made relatively large harmful effects on daily functioning in this particular study sample. It would be valuable to investigate differences in the mechanism between patients with chronic pain having a PTSD diagnosis and those having sub-threshold PTSD symptoms.
Potential treatment interventions can be considered in patients with both chronic pain and a history of a traumatic experience. Considering the reciprocal interactions between chronic pain and PTSD, it is essential to break the link(s) between them. Furthermore for effective interventions, it is of great importance in assisting the patients to understand and be aware of the links between them [11]. Thus, the study findings suggest that interventions for enhancing daily functioning may primarily involve cutting into the links among pain, hyperarousal symptoms of PTSD, and pain avoidance behaviors. In particular, it would be beneficial to use exposure strategies (e.g., in vivo, imaginal) [42] for discouraging pain avoidance behaviors in response to fear of trauma reminders (i.e., pain) and subsequent activation of hyperarousal symptoms of PTSD as well as fear of movement and re-injury. Simultaneously, it would be important to encourage physical activities using pacing and activity scheduling strategies [42]. Such combined strategies would help the patients to deal with their fear in situations where it is elicited and to engage in physical activities, thereby preventing physical deconditioning and consequent physical disability and psychological problems and simultaneously facilitating daily functioning [42].
Despite the benefits of the present study, its shortcomings should be acknowledged. First, a sample size for the present study was relatively small (N = 142), possibly increasing a risk of overfitting [2]. Second, an alternative competing model(s) was not used for comparison purpose in the present study, even with possibilities that the alternative competing model(s) may provide a comparable or improved fit [43]. Also, the design of the present study was cross-sectional and correlational, from which the results do not imply causal relations among the study variables. Thus, the findings of the present study need to be interpreted with caution and further research may benefit from investigating our favored model, together with alternative competing models in a study design proving causal relations (e.g., longitudinal, experimental, treatment) [43]. Third, the study sample consisted of patients with chronic pain with heterogeneous pain complaints and a history of a traumatic event in a tertiary care pain clinic. Thus, the findings of the present study may limit its generalizability to those with specific pain complaints (e.g., rheumatoid arthritis), those experiencing or witnessing specific trauma event (e.g., motor vehicle accident), or those receiving care in other settings (e.g., primary care clinic).
In conclusion, the findings of the study generally provided support for the mutual maintenance model of chronic pain and PTSD [11]. Specifically, they provided evidences that pain as reminders of the trauma may trigger hyperarousal symptoms of PTSD and subsequent pain avoidance behaviors, resulting in deterioration in both physical and psychological aspects of functioning among patients with chronic pain who also have had traumatic experiences. This study is a relatively preliminary study of the theoretical processes of the mutual maintenance model [11] in an integrated manner (i.e., pain as reminders of the trauma and avoidance of pain and intrusive memories and feelings about the traumatic event), particularly given its cross-sectional design. Further studies examining this model in other situations, and with large samples, may lead to the development of appropriate treatment approaches for people who suffer with both chronic pain and a history of traumatic experience.
ACKNOWLEDGEMENTS
This work was supported by the National Research Foundation of Korea grant funded by the Korea government (MEST) (No. 2010-0020633) and by the Postdoctoral Research Program of Chung-Ang University 2010 year. We have no any financial or other relationships that might lead to a conflict of interest.
References
- 1.Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47:930–937. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 2.Tomarken AJ, Waller NG. Potential problems with "well fitting" models. J Abnorm Psychol. 2003;112:578–598. doi: 10.1037/0021-843X.112.4.578. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington DC: American Psychiatric Association; 2000. [Google Scholar]
- 4.Laursen BS, Bajaj P, Olesen AS, Delmar C, Arendt-Nielsen L. Health related quality of life and quantitative pain measurement in females with chronic non-malignant pain. Eur J Pain. 2005;9:267–275. doi: 10.1016/j.ejpain.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 5.McCracken LM, Gauntlett-Gilbert J, Vowles KE. The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain. 2007;131:63–69. doi: 10.1016/j.pain.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Schnurr PP, Hayes AF, Lunney CA, McFall M, Uddo M. Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. J Consult Clin Psychol. 2006;74:707–713. doi: 10.1037/0022-006X.74.4.707. [DOI] [PubMed] [Google Scholar]
- 7.Zayfert C, Dums AR, Ferguson RJ, Hegel MT. Health functioning impairments associated with posttraumatic stress disorder, anxiety disorders, and depression. J Nerv Ment Dis. 2002;190:233–240. doi: 10.1097/00005053-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Clapp JD, Beck JG, Palyo SA, Grant DM. An examination of the synergy of pain and PTSD on quality of life: additive or multiplicative effects? Pain. 2008;138:301–309. doi: 10.1016/j.pain.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katz J, Asmundson GJ, McRae K, Halket E. Emotional numbing and pain intensity predict the development of pain disability up to one year after lateral thoracotomy. Eur J Pain. 2009;13:870–878. doi: 10.1016/j.ejpain.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 10.Tsui P, Stein T, Sonty N. The relationship among PTSD symptoms, chronic pain acceptance, and disability. J Pain. 2010;11:S58. [Google Scholar]
- 11.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. 2001;21:857–877. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- 12.Beck JG, Freeman JB, Shipherd JC, Hamblen JL, Lackner JM. Specificity of Stroop interference in patients with pain and PTSD. J Abnorm Psychol. 2001;110:536–543. doi: 10.1037//0021-843x.110.4.536. [DOI] [PubMed] [Google Scholar]
- 13.MacLeod CM. Half a century of research on the Stroop effect: an integrative review. Psychol Bull. 1991;109:163–203. doi: 10.1037/0033-2909.109.2.163. [DOI] [PubMed] [Google Scholar]
- 14.Geisser ME, Roth RS, Bachman JE, Eckert TA. The relationship between symptoms of post-traumatic stress disorder and pain, affective disturbance, and disability among patients with accident and non-accident related pain. Pain. 1996;66:207–214. doi: 10.1016/0304-3959(96)03038-2. [DOI] [PubMed] [Google Scholar]
- 15.Blanchard EB, Kolb LC, Geradi RJ, Ryan P, Pallmeyer TP. Cardiac response to relevant stimuli as an adjunctive tool for diagnosing post-traumatic stress disorder in Vietnam veterans. Behav Ther. 1986;17:592–606. [Google Scholar]
- 16.Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of pain assessment. 2nd ed. New York: Guilford Press; 2001. pp. 15–34. [Google Scholar]
- 17.Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9:445–451. [Google Scholar]
- 18.Nam B, Kwon HI, Kwon JH. Psychometric qualities of the Korean version of the Post-traumatic Diagnosis Scale (PDS-K) Korean J Clin Psychol. 2010;29:147–167. [Google Scholar]
- 19.McCracken LM, Dhingra L. A short version of the Pain Anxiety Symptoms Scale (PASS-20): preliminary development and validity. Pain Res Manag. 2002;7:45–50. doi: 10.1155/2002/517163. [DOI] [PubMed] [Google Scholar]
- 20.Coons MJ, Hadjistavropoulos HD, Asmundson GJ. Factor structure and psychometric properties of the Pain Anxiety Symptoms Scale-20 in a community physiotherapy clinic sample. Eur J Pain. 2004;8:511–516. doi: 10.1016/j.ejpain.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 21.Cho S, Lee SM, McCracken LM, Moon DE, Heiby EM. Psychometric properties of a Korean version of the Pain Anxiety Symptoms Scale-20 in chronic pain patients. Int J Behav Med. 2010;17:108–117. doi: 10.1007/s12529-010-9080-2. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med care. 1992;30:473–483. [PubMed] [Google Scholar]
- 23.Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Econ. 1993;2:217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- 24.Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garratt AM, Ruta DA, Abdalla MI, Buckingham JK, Russell IT. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ. 1993;306:1440–1444. doi: 10.1136/bmj.306.6890.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M. Development of the Korean version of Short-Form 36-Item Health Survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med. 2004;203:189–194. doi: 10.1620/tjem.203.189. [DOI] [PubMed] [Google Scholar]
- 27.Koh SB, Chang SJ, Kang MG, Cha BS, Park JK. Reliability and validity on measurement instrument for health status assessment in occupational workers. Korean J Prev Med. 1997;30:251–266. [Google Scholar]
- 28.Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behav Res. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 29.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 30.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 31.Loehlin JC. Latent variable models: an introduction to factor, path, and structural analysis. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1992. [Google Scholar]
- 32.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- 33.Leveille SG, Guralnik JM, Ferrucci L, Hirsch R, Simonsick E, Hochberg MC. Foot pain and disability in older women. Am J Epidemiol. 1998;148:657–665. doi: 10.1093/aje/148.7.657. [DOI] [PubMed] [Google Scholar]
- 34.Unruh AM, Henriksson C. Psychological, environmental and behavioural dimensions ofthe pain experience. In: Strong J, Unruh AM, Wright A, Baxter GD, editors. Pain: A textbook for therapists. London: Churchill Livingstone; 2002. pp. 65–79. [Google Scholar]
- 35.Asmundson GJ, Norton PJ, Norton GR. Beyond pain: the role of fear and avoidance in chronicity. Clin Psychol Rev. 1999;19:97–119. doi: 10.1016/s0272-7358(98)00034-8. [DOI] [PubMed] [Google Scholar]
- 36.McCracken LM, Gross RT, Aikens J, Carnrike CL., Jr The assessment of anxiety and fear in persons with chronic pain: a comparison of instruments. Behav Res Ther. 1996;34:927–933. doi: 10.1016/s0005-7967(96)00057-5. [DOI] [PubMed] [Google Scholar]
- 37.McCracken LM, Zayfert C, Gross RT. The pain anxiety symptoms scale: development and validation of a scale to measure fear of pain. Pain. 1992;50:67–73. doi: 10.1016/0304-3959(92)90113-P. [DOI] [PubMed] [Google Scholar]
- 38.Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. Trauma and the Vietnam War generation: report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner/Mazel; 1990. [Google Scholar]
- 39.Resick PA, Calhoun KS. Posttraumatic stress disorder. In: Barlow DH, editor. Clinical handbook of psychological disorders. 3rd ed. New York: Guilford Press; 2001. pp. 60–113. [Google Scholar]
- 40.Bigatti SM, Hernandez AM, Cronan TA, Rand KL. Sleep disturbances in fibromyalgia syndrome: relationship to pain and depression. Arthritis Rheum. 2008;59:961–967. doi: 10.1002/art.23828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.American Psychiatric Association. Insomnia: Both Symptom and Syndrome. Psychiatr News. 2005;40:30. [Google Scholar]
- 42.Sharp TJ. The prevalence of post-traumatic stress disorder in chronic pain patients. Curr Pain Headache Rep. 2004;8:111–115. doi: 10.1007/s11916-004-0024-x. [DOI] [PubMed] [Google Scholar]
- 43.Breckler SJ. Applications of covariance structure modeling in psychology: cause for concern. Psychol Bull. 1990;107:260–273. doi: 10.1037/0033-2909.107.2.260. [DOI] [PubMed] [Google Scholar]