Abstract
Alcoholics Anonymous participation has been measured in addiction research, but few validated tools distinguish components of this multi-dimensional construct. This study provides psychometric findings for the scale “Service to Others in Sobriety (SOS)”, a brief assessment of AA-related helping (AAH). Data are derived from a sample of treatment-seeking alcoholics, and SOS validity and response stability is reported by using a test-retest sample. Findings demonstrated adequate psychometric properties of the SOS, including convergent validity, internal consistency (alpha=0.92) and test-rest reliability (r=0.94). The SOS is a valid measure of AAH activities pertinent to the daily lives of recovering alcoholics.
Keywords: service, AA-related helping, substance use disorders, 12-step programs
Giving, helping, volunteering, being of service, unselfishness, goodwill—whatever the term, human beings worldwide engage in generous, altruistic behavior toward others. While such acts are, by definition, performed without expectation of external reward or reciprocation (Zemore & Pagano, 2009), they nonetheless provide specific benefits to the helper.
A growing body of research shows evidence of the health benefits to helpers across the lifespan. Youths have been shown to enjoy lower levels of disciplinary problems (Calabrese & Schumer, 1986), better values, and educational improvement as a result of volunteer work (Calabrese & Schumer, 1986; Astin & Sax, 1998; Johnson, Beebe, Mortimer, & Snyder, 1998; Uggen & Janikula, 1999). Adults have been shown to enjoy greater happiness and life satisfaction (Ellison, 1991; Keyes, 1998), better social functioning (Keyes, 1998), decreased depression and anxiety (Brown, Gary, Greene, & Milburn, 1992; Rietschlin, 1998), and better mental health (Schwartz, Meisenhelder, Ma, & Reed, 2003) as the result of altruistic behavior. Older adults have been shown to enjoy positive affect, self esteem and social integration (Midlarsky & Kahana, 1994) as well as increased longevity (Brown, Nesse, Vinokur, & Smith, 2003; Moen, Dempster-McClain, & Williams, 1989; Post, 2007) as the result of volunteering and providing instrumental and emotional support.
Researchers have begun to investigate the sobriety benefit to alcoholic helpers and to consider the helping activities professed to be salient to the recovery process. Alcoholics Anonymous (AA) was established on a foundation of prosocial behavior (Humphreys & Kaskutas, 1995; Zemore, Kaskutas & Ammon, 2004). AA’s preamble states its “primary purpose is to stay sober and help other alcoholics to achieve sobriety,” and its Twelfth Step states, “Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics, and to practice these principles in all our affairs” (A.A. World Service, 1987). In addition to the emphasis on service, AA literature cites the opposite of service--self-centeredness and self-involvement--as the alcoholic’s chief problem: “Above everything, we alcoholics must be rid of this selfishness. We must, or it kills us!” (A.A. World Services, 2001, p. 62).
Several investigations of 12-step programs have linked AA-related helping (AAH) with improved drinking outcomes. Early work identified two forms of AAH, sponsorship and practice of the 12th Step, to be reliable predictors of better drinking outcomes (Emrick, 1987; Emrick, Tonigan, Montgomery, & Little, 1993; Sheeren, 1988). When interviewing alcoholics, Crape, Latkin, Laris, and Knowlton (2002) found that being a sponsor was associated with an almost seven-fold increase in odds of abstinence at the initial interview, and a three-fold increase in odds of abstinence at the one-year follow-up interview. When analyzing Project MATCH data, Pagano, Friend, Tonigan, and Stout (2004) found that those who sponsored others and/or worked the 12th step during treatment were twice as likely to remain sober in the 12 months post-treatment. Zemore and Kaskutas (2004) found that sponsorship and step-work were positively associated with longer sobriety, while other components of AA involvement were not. Pagano and colleagues (2009a) retrospectively studied the course of AAH among alcoholics with 20 or more years of sobriety. These “old timers” were found to participate in AAH in a pattern that increased linearly over time--not just in the first few months or years of sobriety, but throughout the next 20 years sober.
Collectively, this body of work represents significant advances in the empirical study of AAH. However, as highlighted in a recent review by Zemore and Pagano (2009), work to date has been limited by a lack of consensus about how to define helping, among other factors. For instance, some researchers focus on emotional support, such as listening, while others focus on instrumental support, such as lending money. Some define helping by the absence of, or the degree to which one avoids, hurting others. Some define helping as actively giving (such as providing advice or information) and others define helping as being receptive (such as being patient with another person). Some define helping as interpersonal and intimate, while others define helping to include solitary environmental improvements such as picking up trash (Zemore & Pagano, 2009).
Measurement strategies of AAH also vary. Some researchers measure beliefs about the impact of helping (e.g., Magura et al., 2003) while others measure specific helping behaviors themselves. Some measure time spent helping (Zemore & Kaskutas, 2004; Zemore, Kaskutas, & Ammon, 2004), while others measure the frequency of specific helping behaviors (Pagano, Philips, Stout, Menard, Piliavin, 2007). Some measure helping during treatment (e.g., Zemore, Kaskutas, & Ammon, 2004; Pagano et al., 2004); others have studied the course of AAH over longer periods of time (Pagano et al., 2009a; Pagano et al., 2009b). Researchers have used single items, qualitative coding strategies, quantitative scales, categorical items, and self report measures of varying lengths (Zemore & Pagano, 2009). Some researchers combine several measurement strategies within a single instrument. What these varied AAH measurement strategies all share is a lack of demonstrated psychometric rigor. Although pioneering work has made important inroads, our ability to measure AAH is limited. The first limitation pertains to the confusion that respondents may encounter when ascertaining their completion of the 12th Step. The 12th Step is a triple-barreled construct involving (1) having had a spiritual awakening (2) trying to carry this message to alcoholics and (3) practicing AA’s principles in “all our affairs” (Pagano, Friend, Tonigan, & Stout, 2004). Respondents may not endorse this item if they see themselves as having completed some but not all aspects of the 12th step. Items that ask about 12th step-work may also inadvertently sew problems into measurement by asking whether respondents have completed the 12th step. Respondents may not endorse this item if they see the step as one they will never fully complete but will perform on an ongoing basis throughout their lives. Second, limiting AAH to help given by sponsors excludes the helping behaviors of those in early recovery, given the recommendation of one year of sobriety to provide sponsorship.
Identifying prescribed acts of support to fellow sufferers was a step in the right direction. Zemore, Kaskutas, and Ammon (2004) developed a brief 5-item instrument assessing time spent giving prescribed support to other alcoholics/addicts, including moral support, learned experience on how to stay clean and sober, learned experience about other problems, and how to get help inside and outside of the treatment program. However, these venues of help do not capture all the myriad of ways alcoholics routinely help fellow sufferers, assume that the amount of time giving support relates linearly to positive outcomes, and mainly assess support given within treatment settings. It is high time for the development of a validated assessment tool of AAH.
Helping Defined and Study Aims
Our operationalization of the construct under investigation, service to others within 12-step contexts, was informed in part by AA literature, altruism literature (Monroe, 2002), and pilot focus groups with AA members (source: SOS Research Plan, Phase I 2005. SOS data available on request). The following AA literature guided our careful selection of instrument items: “Working with Others,” a chapter in AA’s central text (A.A World Services, 2001); documented conversations with the founders of AA (A.A. World Services, 1980); formal description of the 12 Steps (A.A. World Services, 1987); and individual stories of recovering AA members (A.A. World Services, 2001). Instrument item selection was also based on theoretical knowledge from the social science disciplines of bioethics and positive psychology. Service-oriented behaviors included in the scale reflect kindness toward and consideration of others (Burnstein, Crandall, & Kitayama, 1994), and embody behaviors recognized as altruistic (Monroe, 2002); the help given is voluntary, intentional, without expectation of external reward or reciprocation, and benefits another as its primary goal.
In this study, we examined the psychometric properties of a 12-item tool “Service to Others in Sobriety (SOS)” that was designed to assess recent participation in AAH. The goals of this study were: 1) to explore the frequency of SOS items as reported by recovering alcoholics three years post treatment, 2) to establish internal consistency and stability of the SOS, 3) to establish preliminary convergent validity of the SOS, 4) to examine the SOS in relation to alcohol outcomes, and 5) to identify the optimal cut-off score for the SOS.
Methods
Procedures
The study sample was derived from Case Monitoring II (CMII) – a prospective, longitudinal investigation of the efficacy of a behavioral treatment for alcohol use disorders that was delivered over 14 months (Stout et al., 1999). The theoretically derived psychosocial intervention selected for use was Case Monitoring, a series of non-confrontational supportive phone calls lasting approximately 15 minutes. A total of 301 CMII participants were recruited directly from five detoxification sites in New England. In the week following the start of a three-day inpatient detoxification, participants were urn randomized (Stout et al., 1994) to treatment as usual, or Case Monitoring as an adjunct to treatment as usual, and followed over the course of three years. Both conditions received encouragement to participate in 12-Step programs. Inclusion criteria included detoxification treatment for alcohol dependency as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), 4th ed., (American Psychiatric Association [APA]), HMO insurance coverage for at least 8 months, telephone service and a stable address, aged 18–65 years, literacy in English, and having no plans to leave the region for the next 2 years. Exclusion criteria included having a current DSM-IV Diagnosis of dependency for sedative/hypnotic drugs, stimulants, cocaine, or opiates; having taken any drugs intravenously during the previous 6 months; being currently dangerous to oneself or others; exhibiting symptoms of acute psychosis; and/or having severe organic impairment. Rational and components of Case Monitoring are detailed elsewhere (Stout et al., 1999; Zweben et al., 2003).
When funding became available for the instrument validity study, a total of 154 CMII participants were due for their 36-month follow-up interview (91% of the 170 CMII participants for whom 36-month data became available). Of these, 94 (61%) were scheduled for an in-person 36-month interview, and thus eligible to provide the required in-person consent to participate in the instrument validity study. This report presents data for the 32 consenting subjects (34% of the eligible sample) enrolled at the 36-month follow-up interview in CMII. In a 60-minute interview, study subjects completed four instrument validity self-report questionnaires in addition to the 36-month interview battery. The sequence of instrument validity self-report questionnaires was rotated to control for order effects. Study subjects completed a second administration of a brief AAH instrument in the week following its first administration. Research study staff was blind to instrument validity measurement scores. The instrument validity study was approved by the University Hospitals Case Medical Center Institutional Review Board (IRB) and Pacific Institute for Research and Evaluation (PIRE) IRB. All subjects voluntarily provided written informed consent for study participation.
Measures
CMII Measures
Background variables were collected in CMII at baseline. Chemical dependency (CD) treatment utilization and AA meeting attendance were assessed at baseline and annually thereafter for three years.
Background Variables
Background variables included gender, ethnicity, marital status, religious preference, age, and years of education.
Alcohol Severity
Alcohol severity was measured by the number of drinks per drinking day and percent days abstinent in the prior six months to baseline using the Time Line Follow Back Interview (TLFB; Sobell et al., 1986). Standard drink units were calculated based on specific beverage and volume consumed per calendar day. Sobell et al. (1986) have shown this interview to be a reliable method for collecting drinking data.
As another indicator of alcohol severity, the number of chemical dependency (CD) treatments (outpatient counseling, day treatment, employee assistance programs, halfway house) utilized in the past 12 months was assessed with the Health Care Data Form (Larson et al., 1997). Prior work has linked a greater number of CD treatments with higher alcohol severity (Tonigan, Connors, & Miller, 2003).
AA Meeting Attendance
The annual number of AA meetings attended was assessed with a single item from the Health Care Data Form: “How many AA meetings have you attended in the last 12 months?”.
Instrument Validity Measures
Instrument validity study measures were collected at the 36-month follow-up interview in CMII.
Service to Others in Sobriety (SOS)
Service to others within 12-step contexts was assessed with the 12-item SOS (see Table 1). Items are rated on a 5-point Likert-type scale from 1 (“rarely”) to 5 (“always”) with reference to the prior month. SOS items reflect acts of good citizenship as a member of a 12-step program (i.e. putting away chairs at meetings, donating money), formal service positions available in 12-step programs of recovery (i.e., donating money, public outreach, etc.), and AAH activities involving the transmission of one’s personal experience to another (i.e., sharing one’s personal story with another alcoholic, sharing progress with step-work). Prior work with SOS items among a small sample of alcoholics has shown adequate internal consistency (alpha =.82) and feasibility (less than 10 minutes to complete; Pagano et al., 2009a). Intracorrelations between SOS items in the current study were moderate to large (range rs.=0.30–0.90), except for two items. No significant correlations were found for “Donated money to AA/NA” and “Put away chairs after a meeting”.
Table 1.
Service to Others in Sobriety (SOS) Item Responses: Frequency, Internal Consistency, and Stability
| SOS Item a | Frequency | Internal Consistencyg |
Test-Retest Reliabilityh |
|||
|---|---|---|---|---|---|---|
| Median | Mean (SD) | % Lowf | ||||
| 1. | Took calls or spent time with a sponsee | 1.00 | 2.03 (1.36) | 66% | .76*** | .88*** |
| 2. | Guided an alcoholic/addict through the 12-Steps | 1.50 | 2.06 (1.19) | 59% | .76*** | .84*** |
| 3. | Held a service position in a 12-Step programb | 2.00 | 2.56 (1.70) | 53% | .75*** | .96*** |
| 4. | Say something positive to an alcoholic/addict | 4.00 | 3.56 (1.54) | 25% | .74*** | .91*** |
| 5. | Listened to an alcoholic/addictd | 4.00 | 3.22 (1.43) | 28% | .75*** | .82*** |
| 6. | Say hello to a newcomer | 3.00 | 3.19 (1.45) | 28% | .74*** | .88*** |
| 7. | Reached out to an alcoholic/addict having a hard time | 3.50 | 3.06 (1.50) | 38% | .74*** | .86*** |
| 8. | Shared personal story with an alcoholic/addict | 3.00 | 2.88 (1.31) | 31% | .75*** | .90*** |
| 9. | Read program literature to an alcoholic/addicte | 3.00 | 2.67 (1.33) | 31% | .75*** | .88*** |
| 10. | Encourage an alcoholic/addict to go to a meeting | 4.00 | 3.90 (1.39) | 19% | .75*** | .91*** |
| 11. | Donated money to AA/NAc | 4.00 | 3.84 (1.46) | 25% | .77** | .60** |
| 12. | Put away chairs after a meeting | 4.00 | 4.00 (1.16) | 9% | .77*** | .75*** |
| SOS Total Score | 15.00 | 14.34 (6.97) | -- | .92*** | .94** | |
p<.05
p<.01
p<.001
NOTES:
Items are rated as “never (1)”, “rarely (2)”, “sometimes (3)”, “often (4)”, or “always (5)”
Service positions at meetings include: coffee maker, door greeter, chairperson, secretary, treasurer.
Service positions outside of meetings include: service delegate, public outreach organizer (i.e. jails, etc.), literature delegate.
12-Step programs are self supporting through members’ contributions at meetings or local service centers.
Listening qualified as at least 10 minutes of uninterrupted listening
Literature can be read at meetings (the promises, the steps, etc.) or directly when working with another alcoholic/addict.
Low = SOS items endorsed “never” or “rarely”
Cronbach’s alpha (raw)
Spearman Rank-Order Correlation
AA Involvement (AAI)
Study subjects completed the 13-item AA Involvement (AAI) scale, a brief, well-validated measure of AA affiliation (Tonigan et al., 1996). At the time of this study, the available “gold standard” criterion for AAH was endorsement of either of two AAI items: 1) being a sponsor and 2) completion of the 12th step in the prior 90 days. Subjects endorsing either of these two binary (yes/no) AAI items were considered to be participating in AAH. This 2 AAI-item criterion of AAH has been used in large, clinical trial investigations with alcohol populations (Pagano et al., 2004; Pagano et al., 2009b).
Prosocial Personality Battery (PSB)
The PSB is a commonly used scale in social psychology for assessing prosocial tendencies from a personality trait perspective (Penner et al., 1995). Thirty items are rated on a 5-point Likert-type scale from strongly disagree (1) to strongly agree (5) and are summed to form 2 subscales: helpfulness and other-oriented empathy. High helpfulness scores reflect behavioral tendencies towards responsibility for and concern about the welfare of others. High other-oriented scores primarily reflect prosocial cognitions and empathetic affect. Both subscales have demonstrated internal consistency greater than 0.80 and test-retest reliability (alpha=0.77 for other-oriented empathy; alpha=0.85 for helpfulness; Penner & Finkelstein, 1998).
Hypersensitivity Narcissism Scale (HSNS)
At the opposite end of other-oriented behavior, covert narcissistic behaviors were measured with the Hypersensitivity Narcissism Scale (HSNS; Hendin & Cheek, 1997). Covert narcissistic behaviors were measured in this study due to its correlation with high levels of neuroticism and concomitant likelihood of greater alcohol severity (Atlas & Them, 2008; Khan et al., 2005; Malouff et al., 2007; Webb et al., 1990). Each of the 10 HSNS items are scored on a 5-point Likert-type scale from 1 (very uncharacteristic or untrue; strongly disagree) to 5 (very characteristic or true; strongly agree) and summed. Higher HSNS scores reflect higher susceptibility to feelings of belittlement, hypersensitivity to criticism, delusions of persecution, and anxious self-preoccupation. The HSNS has demonstrated good internal consistency with alphas ranging from .62 to.76 (Hendin & Cheek, 1997). The HSNS was found to highly correlate with the MMPI-based composite measure of covert narcissistic behaviors (r=0.60) and the exploitiveness/entitlement subscale of the Narcissistic Personality Inventory (r=0.30; Hendin & Cheek, 1997).
Length of Time Sober
Length of time sober and three demographic items repeated from the baseline assessment (age, gender, and race) were included on the first page of the SOS instrument. At the time of enrollment into the instrument validity study, subjects reported the length of time (in months) from their last drink or drug. This item was assessed again one week later at the time of the second administration of the SOS. Test-retest reliability of subjects’ reports of length of time sober was excellent (r=0.95). Because the distribution of length of time sober was negatively skewed, this variable received an arcsine transformation, as was done in primary MATCH outcome analysis (Project MATCH Research Group, 1997).
Statistical Analysis
Statistical analyses were conducted with SAS version 9.1.3 (SAS Institute Inc., 2004). Non-parametric analyses were performed for group comparisons, using Fisher’s Exact Test for binary variables and Kruskal-Wallis Chi-Square Test for continuous variables. Non-parametric analyses were conducted to address the study aims, as these statistical approaches are distribution free and more robust tests when sample sizes are not large. Psychometric analyses with the SOS included item analysis, internal consistency, test-retest reliability, convergent validity, and Receiver Operator Curve (ROC) analysis. Internal consistency was determined by calculating Cronbach’s alpha. Test-retest reliability was determined by comparing two administrations of the SOS using the Spearman rank-order correlation, a nonparametric measure of association based on the rank of the data values. For convergent validity and outcome analysis, the SOS was compared to the PSB, HSNS, and length of time sober using nonparametric Kruskal-Wallis chi-square tests. To identify the optimal cut-off score for the SOS, an ROC curve was constructed based on the SOS’s performance compared with the 2 AAI-item criterion of AAH. For the purposes of interpretation, Cohen (1988) considers r=0.10 “small”, r=0.30 “medium” and r=0.50 “large.” All tests were double-sided, and partial-Bonferroni of p<.01 was used to avoid inflating the risk of Type 1 error.
Results
Sample
The majority of study subjects were male (69%) and from non-Hispanic/Latino backgrounds (97%). Approximately half of the study sample was married (44%) with a Catholic religious preference (56%). The mean age of the study sample was 45.86 years (SD=8.07) and the mean level of education was 14.25 years (SD=2.68). Study subjects reported heavy drinking on drinking days (mean drinks per drinking day=17.03, SD=7.35), an average of 25.24 (SD=27.11) percent days abstinent, and attended an average of 43 AA meetings (SD=60.16) in the 12 months prior to baseline. There were no significant baseline differences between study subjects and non-study CMII participants in terms of gender, ethnicity, marital status, religious preference, age, education, drinks per drinking day, and percent days abstinent. During follow-up, no significant differences were found between study participants and non-study participants in terms of treatment utilization (12-month assessment, X2=0.47, p=0.49; 24-month assessment, X2=2.26, p=0.13; 36-month assessment, X2=1.44. p=0.23), or AA attendance 12-month assessment, X2=2.76, p=.0.10; 24-month assessment, X2=0.01, p=0.97; 36-month assessment, X2=0.94. p=0.33). At the time of enrollment into the instrument validity study (i.e. 36-month assessment), one-third of the study sample reported continuous sobriety since the baseline interview. The mean length of time sober was 21.58 months (SD=14.73, range=0–36).
Frequency of SOS items
The first goal of the study was to explore participation patterns in AAH three years post treatment as measured by the SOS. Table 1 shows the frequency of endorsed responses to SOS items from low to high levels of participation. At the 36-month interview, the least common forms of low AAH activity (i.e., SOS items rated “never” or “rarely”) were taking calls or spending time with a sponsee (a member of the 12-step program with a selected sponsor, 66%), guiding another through the 12-steps (59%), and holding a service position (53%). In contrast, the most common forms of high AAH activity (i.e., SOS items rated “often” or “always”) were putting away chairs after a meeting (75%), encouraging a newly sober alcoholic to go to a meeting (72%), and donating money to 12-step organizations (63%). In comparison to participation in AAH activities, engagement in other involvement components of the 12-step program (i.e. fellowship, meeting attendance) was higher: 81% endorsed “yes” to the AAI item “do you have a sponsor”, and 76% had attended at least one meeting in the prior 90 days. The mean SOS score was 14.34 (SD=6.97, range 12–56).
Internal Consistency and Stability of the SOS
Table 1 shows the results of psychometric analyses addressing the second goal of the study. With regards to internal consistency, the Cronbach’s alpha for the SOS total score was 0.92, and ranged from 0.74–0.77 for individual SOS items. Test-retest reliability of the SOS was next examined among all subjects (100%) who completed both administrations of the SOS with complete item responses. As shown in Table 1, test-retest item comparisons found large effect size correlations between administrations for all SOS items (rs=.60–.96). The Spearman rank-order correlation was 0.94 (p<.001) between the first and second administration of the SOS total score.
Convergent Validity of the SOS
The third goal of the study was to establish preliminary convergent validity of the SOS. Comparisons between SOS total scores and the two PSB subscales are presented in Table 2. The Spearman correlation was 0.62 (p<.001) between the SOS total score and “other-oriented empathy” PSB subscale. A trend emerged between the SOS total score and “helpfulness” PSB subscale (r=0.33, p=0.07).
Table 2.
| Measure | Total | SOS Total Score | Confidence Limits |
|---|---|---|---|
| Mean (SD) | Spearman r | 95% Confidence Interval | |
| PSB Subscale: Other-Oriented Empathy | 72.25 (2.40) | 0.62*** | 0.35, 0.80 |
| PSB Subscale: Helpfulness | 23.96 (4.54) | 0.33t | −0.03, 0.60 |
| HNSM Total Score | 29.97 (4.54) | −0.60*** | −0.79,−0.32 |
| Length of Time Sober | 21.58 (14.73) | 0.40** | 0.22, 0.64 |
PSB = Prosocial Personality Battery
HSNS = Hypersensitivity Narcissism Scale
p<.10
p<.01
p<.001
As shown in Table 2, a large negative relationship was found between the SOS total score and the HSNS total score (r=−0.60, p<.001). To examine levels of covert narcissistic behaviors among alcoholics in relation to the general population, HSNS scores of the study sample were next compared to a normative sample. Using a one-sample sign test, HSNS scores of the study sample (M=29.16, SD=7.78) were found to be comparable to Hendin and Cheek’s (1997) sample of 101 male adults (M=29.80, SD=6.00, p=.61). In the study sample, the Spearman correlation was −0.60 (p<.001) between the SOS and HSNS total scores.
Comparison of the SOS and drinking outcomes
Addressing the fourth goal of the study, the SOS total score was next examined in relation to concurrent drinking outcomes. As shown in Table 2, a significant positive relationship was found between the SOS and subjects’ reports of length of time sober (r=0.40, p<.01).
Selection of SOS Cut-Off Score
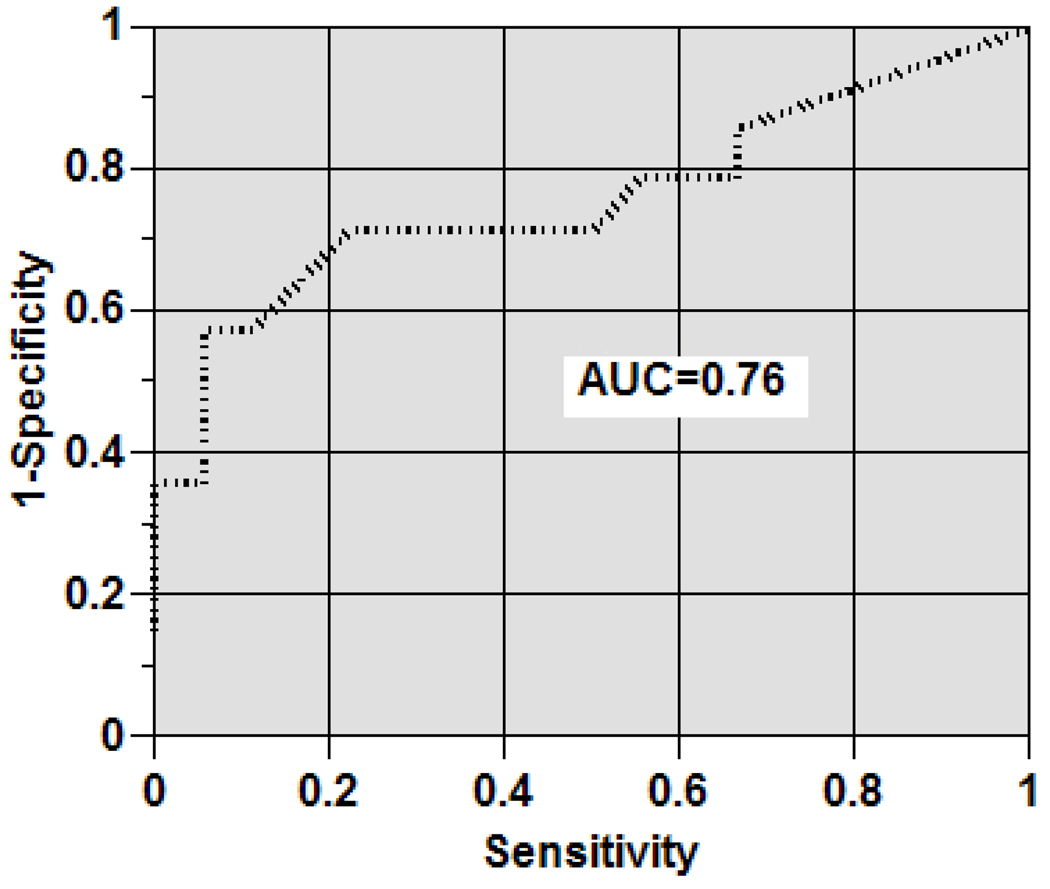
The fifth goal of the study was to establish the optimal cut-off score for the SOS using the ROC curve. Figure 1 shows the ROC curve for the SOS against the 2-AAI item criterion of AAH. The area under the curve (AUC) equals 0.76 with a standard error of 0.03, which compares favorably with AUC data for other psychiatric assessment tests (Pagano et al., 2000; Wyshak et al., 1991). A cut-off score of 45 or higher was found to provide the highest average of sensitivity and specificity (SN=.78; SP=.64), the highest Phi coefficient (phi=.50), and the highest degree of concordance (k=.54). Using this cut-off score to indicate high versus low AAH, high AAH participation was found among 28% of the sample at the 36-month interview.
Figure 1.
Receiver-operator characteristics curve of sos scores versus AAI report of AAH
Discussion
Results from this study indicate that the SOS possesses the requisite psychometric qualities to be useful as a brief assessment of AAH. The internal consistency of the SOS was acceptable, and test-retest reliability was excellent. The SOS is easy to administer: respondents completed the assessment tool in less than 5 minutes with no items left missing.
Preliminary convergent validity was also established using a multi-method assessment approach. The SOS was strongly associated with the “other-oriented empathy” PSB subscale, and associated at a trend level with the “helpfulness” PSB subscale. The large correlation between the SOS and the PSB other-oriented empathy subscale may be due to similar shared experiences with the alcoholic being helped. The stronger link to other-oriented empathy rather than helpfulness in general is consistent with prior work demonstrating the particular salience of service within 12-step contexts as opposed to other life domains (Pagano et al., 2009a).
A significant, negative relationship was also found between the SOS and covert narcissistic behaviors. Self-absorption is one theorized root of alcoholism, the solution to which requires getting out of oneself through service (AA, 2001). Given the correlation between the SOS and HSNS was not zero, covert narcissism appears to be an oblique rather than orthogonal construct to AAH. Hypersensitivity to perceived criticism may diminish with higher service participation, yet still be present. While pre-treatment HSNS scores were not collected, it is interesting that HSNS scores reported at three years post-treatment were in the same range of a normative sample of college students. A longitudinal examination of the course of AAH in relation to covert narcissistic tendencies is warranted.
When examining the SOS in relation to length of time sober, a significant relationship emerged. Our study provides preliminary discriminate validity of the SOS in relation to drinking outcomes. A prospective study of the SOS in relation to biomarkers of alcohol is warranted to ascertain the salient forms of AAH in relation to sobriety.
When compared against the 2-AAI item criterion of AAH, the SOS showed acceptable sensitivity and specificity in identifying high AAH. The SOS captures a broad array of helping behaviors commonly practiced within the context of 12-step programs. Examination of SOS items revealed that help given in response to another alcoholic’s personal distress was common amongst participants 3 years following treatment. Instrumental forms of behavior, such as putting away chairs, were frequently practiced. Less engagement was found in programmatic 12-step service activities, such as facilitating the step-work of another, or being a sponsor. Our findings parallel earlier work by Tonigan and colleagues (1996) who noted lower participation in programmatic components of 12-step programs as compared to fellowship-oriented activities. The low facilitation of others’ step-work may be considered in light of the phrase “you cannot transmit something that you haven’t got” (AA, 2001, p.164). Few had completed steps beyond the initial three, which could limit step-work experience to share with others. Nonetheless, SOS items are each rated from low to high to reflect the reality of degrees of participation as opposed to definitive yes/no activity.
There are several limitations of this study that should be noted. First, the generalizability of findings should be considered in light of the characteristics of the CMII sample from which the study sample was drawn (i.e., outpatient, mostly Caucasian, well-educated, and insured). Second, the prevalence of high AAH as measured by the SOS at three years post treatment may be overly inflated (28%) due to the study design. Although representative of the larger CMII sample at baseline and during follow-up, the instrument validity study sample size was small to allow for comprehensive data collection, and warrants replication in an epidemiological sample. However, this study had sufficient power to detect the medium to large effect size correlations reported in this study. The 28% rate may also reflect the true prevalence of AAH at 3 years, given the linear extension from an 8% rate during treatment (Pagano et al., 2004) and 15% rate at 15 months (Pagano et al., 2009b) when assessed more narrowly with the 2-AAI item criterion of AAH. Third, the link between low AAH and high covert narcissistic behaviors scores may not generalize to a link between low AAH and high overt narcissistic behaviors, a condition characterized by boisterous, self-aggrandizing, and interpersonally exploitive characteristics (Wink, 1991). Further, causation of this link cannot be established in this study, given the cross-sectional data collection of the instrument validity study measures. Future work is warranted to measure both covert and overt narcissism in relation to AAH over time. Fourth, the impact of the social environment on SOS responses may vary according to the importance of social conditions to the alcoholic helper (see Longabough, 2003). The SOS does not measure the contextual impact of the help received on either the recipient or the helper, given the emphasis in AA for members to help others regardless of recipient outcomes (AA World Services, 1984). Fifth, the instrument validity study enrolled subjects at the last follow-up interview in CMII, which curtailed examination of SOS items in relation to later outcomes. Longitudinal research is underway to explore the forms of AAH that predict better treatment outcomes. Lastly, as with any self-report measure, social desirability bias may be present in the SOS assessment. This potential bias is likely to be minimal, however, given the high correlation of SOS items when completed in person and one week later when completed independently. Developing methodologies, such as using web-based surveys that remove the response bias to an interviewer may further reduce this potential bias.
Conclusion
Despite these limitations, this study is the first to validate a brief assessment of Alcoholics Anonymous-related helping. Findings were drawn from the application of robust analytic methods and detectable in a small representative sample of recovering alcoholics. Building upon pioneering prior work (Zemore & Kaskutas, 2004; Zemore, Kaskutas, & Ammon, 2004), the “Service to Others in Sobriety” captures additional forms of service that may be encouraged at any stage of recovery. AA-related helping activities assessed by the “Service to Others in Sobriety” are not limited by education, gender, race, socioeconomic class, severity of substance use, transportation accessibility, place of residence, or level of meeting attendance. The “Service to Others in Sobriety” assesses formal service positions in 12-step programs, such as public outreach, as well as non-formal forms of AA-related helping, such as reaching out to a fellow sufferer. Service activities assessed are relevant to the daily lives of newcomers and old-timers alike, do not require special training, and, with one exception (being a sponsor), are independent of length of time sober.
The “Service to Others in Sobriety” can be used as an evaluation instrument to assess the degree to which a client is partaking in helping as part of a diversified treatment plan. A score below 20 (out of a range of 5–30) can indicate room for improvement for alcoholics with short-term or long-term sobriety. In sum, use of the “Service to Others in Sobriety” instrument can inform treatment planning, clinical decisions, group interventions, and the ways in which alcoholics, clinicians, administrators, and researchers think about helping.
Acknowledgements
The authors would like to thank Amy Lagasse, Joy LaGrutta, Connie Lawson, and Rebecca Ionescu for their assistance with this research.
Supported by federal grants K01 AA015137 to Dr. Pagano and R01 AA009907 to Dr. Stout from the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Appendix
Abbreviations Referenced
| Abbreviation | Construct |
|---|---|
| SOS | Service to Others in Sobriety |
| AAH | AA-related helping |
| AA | Alcoholics Anonymous |
| CMII | Case Monitoring II |
| DSMIV | Diagnostic and Statistical Manual of Mental Disorders, 4th edition |
| APA | American Psychiatric Association |
| HMO | Health Maintenance Organization |
| IRB | Institutional Review Board |
| PIRE | Pacific Institute for Research and Evaluation |
| CD | Chemical Dependency |
| TLFB | Time Line Follow Back Interview |
| AAI | Alcoholics Anonymous Involvement |
| PSB | Prosocial Personality Battery |
| HSNS | Hypersensitivity Narcissism Scale |
| MMPI | Minnesota Multiphasic Personality Inventory |
| ROC | Receiver Operator Curve |
| SD | Standard Deviation |
| 2-AAI | 2-Item AA Involvement Scale |
| AUC | Area under the Curve |
| SN | Sensitivity |
| SP | Specificity |
Contributor Information
Maria E. Pagano, Case Western Reserve University, Department of Psychiatry, Division of Child Psychiatry, Cleveland, OH
Amy R. Krentzman, University of Michigan Addiction Research Center, Ann Arbor, MI
Casey C. Onder, Case Western Reserve University, Department of Psychiatry, Division of Child Psychiatry, Cleveland, OH
Justina L. Baryak, Case Western Reserve University, Department of Psychiatry, Division of Child Psychiatry, Cleveland, OH
Jennifer L. Murphy, Case Western Reserve University, Department of Psychiatry, Division of Child Psychiatry, Cleveland, OH
William H. Zywiak, Decision Sciences Institute, Pacific Institute for Research Evaluation (PIRE), Providence, RI
Robert L. Stout, Decision Sciences Institute, Pacific Institute for Research Evaluation (PIRE), Providence, RI
References
- A.A World Services. Alcoholics Anonymous: The story of how many thousands of men and women have recovered from alcoholism. 4th ed. New York: A.A World Services; 2001. [Google Scholar]
- A.A. World Services. Dr. Bob and the Good Oldtimers. New York: A. A. World Services; 1980. [Google Scholar]
- A.A. World Services. Pass it On: The story of Bill Wilson and how the A.A. message reached the world. New York: A.A. World Services; 1984. [Google Scholar]
- A.A. World Services. Twelve Steps and Twelve Traditions. New York: A.A. World Services; 1987. [Google Scholar]
- American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Publishing; 1994. [Google Scholar]
- Astin AW, Sax LJ. How undergraduates are affected by service participation. Journal of College Student Development. 1998;39(3):251–263. [Google Scholar]
- Atlas GD, Them MA. Narcissism and sensitivity to criticism: A preliminary investigation. Current Psychology. 2008;27:62–76. [Google Scholar]
- Brown DR, Gary LE, Greene AD, Milburn NG. Patterns of social affiliation as predictors of depressive symptoms among urban blacks. Journal of Health & Social Behavior. 1992;33(3):242–253. [PubMed] [Google Scholar]
- Brown SL, Nesse RM, Vinokur AD, Smith DM. Providing social support may be more beneficial than receiving it: Results from a prospective study of mortality. Psychological Science. 2003;14(4):320–327. doi: 10.1111/1467-9280.14461. [DOI] [PubMed] [Google Scholar]
- Burnstein E, Crandal C, Kitayama S. Some neo-Darwinism decision rules for altruism: Weighing cues for inclusive fitness as a function of the biological importance of the decision. Journal of Personality and Social Psychology. 1994;67(5):773–789. [Google Scholar]
- Calabrese RL, Schumer H. The effects of service activities on adolescent alienation. Adolescence. 1986;XXI No. 8:675–687. [PubMed] [Google Scholar]
- Crape BL, Latkin CA, Laris AS, Knowlton AR. The effects of sponsorship in 12-step treatment of injection drug users. Drug and Alcohol Dependence. 2002;65(3):291–301. doi: 10.1016/s0376-8716(01)00175-2. [DOI] [PubMed] [Google Scholar]
- Ellison CG. Religious involvement and subjective well-being. Journal of Health & Social Behavior. 1991;32(1):80–99. [PubMed] [Google Scholar]
- Emrick CD. Alcoholics Anonymous: Affiliation processes and effectiveness as treatment. Alcoholism: Clinical & Experimental Research. 1987;11(5):416–423. doi: 10.1111/j.1530-0277.1987.tb01915.x. [DOI] [PubMed] [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics Anonymous: what is currently known? In: McCrady B, Miller W, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. New Brunswick, NJ: Rutgers Center of Alcohol Studies; 1993. pp. 41–78. [Google Scholar]
- Hendin HM, Cheek JM. Assessing Hypersensitive Narcissism: A Re-examination of Murray's Narcissism Scale. Journal of Research in Personality. 1997;31:588–599. [Google Scholar]
- Humphreys K, Kaskutas LA. World view of Alcoholics Anonymous, Women for Sobriety, and Adult Children of Alcoholics/Al-Anon mutual help groups. Addiction Research. 1995;3:231–243. [Google Scholar]
- Johnson MK, Beebe T, Mortimer JT, Snyder M. Volunteerism in adolescence: a process perspective. Journal of Research on Adolescence. 1998;8(3):309–332. [Google Scholar]
- Keyes CLM. Social well-being. Social Psychology Quarterly. 1998;61(2):121–140. [Google Scholar]
- Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. British Journal of Psychiatry. 2005;186:190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- Larson MJ, Shepard DS, Zwyiak W, Stout R. Validity of health care utilization reporting systems. Alcohol Clin Exp Res. 1997;21(S):2360. [Google Scholar]
- Longabaugh R. Involvement of support networks in treatment. In: Galanter M, editor. Recent Developments in Alcoholism: Research on Alcoholism Treatment. Vol. XVI. Plenum Press; 2003. pp. 133–147. [DOI] [PubMed] [Google Scholar]
- Magura S, Laudet AB, Mahmood D, Rosenblum A, Vogel HS, Knight EL. Role of self-help processes in achieving abstinence among dually diagnosed persons. Addictive Behaviors. 2003;28(3):399–413. doi: 10.1016/s0306-4603(01)00278-7. [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinson EB, Rooke SE, Schutte, Nicola S. Alcohol involvement and the five-factor model of personality: A meta-analysis. Journal of Drug Education. 2007;37(3):277–294. doi: 10.2190/DE.37.3.d. [DOI] [PubMed] [Google Scholar]
- Midlarsky E, Kahana E. Altruism in later life. Thousand Oaks, CA: Sage Publications, Inc; 1994. [Google Scholar]
- Moen P, Dempster-McClain D, Williams RM., Jr Social integration and longevity: an event history analysis of women’s roles and resilience. American Sociological Review. 1989;54(4):635–647. [Google Scholar]
- Monroe KR. Explicating Altruism. In: Post S, Underwood L, Schloss J, editors. Altruism & Altruistic Love: Science, Philosophy, & Religion in Dialogue. New York: Oxford University Press; 2002. pp. 106–122. [Google Scholar]
- Pagano ME, Cassidy LJ, Little M, Murphy JM, Jillinek MS. Identifying psychosocial dysfunction in school age children: The pediatric symptom checklist as a self-report measure. Psychology in the Schools. 2000;37(2):91–106. doi: 10.1002/(SICI)1520-6807(200003)37:2<91::AID-PITS1>3.0.CO;2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Friend KB, Tonigan JS, Stout RL. Helping other alcoholics in Alcoholics Anonymous and drinking outcomes: findings from Project Match. Journal of Studies on Alcohol. 2004;65(6):766–773. doi: 10.15288/jsa.2004.65.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Phillips KA, Stout RL, Menard W, Piliavin JA. Impact of helping behaviors on the course of substance-use disorders in individuals with body dysmorphic disorder. Journal of Studies on Alcohol. 2007;68(2):291–295. doi: 10.15288/jsad.2007.68.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Zeltner B, Post S, Jaber J, Zywiak WH, Stout RL. Who should I help to stay sober?: Helping behaviors among alcoholics who maintain long-term sobriety. Alcohol Treatment Quarterly. 2009a;27(1):38–50. doi: 10.1080/07347320802586726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME, Zemore SE, Onder CC, Stout RL. Predictors of initial AA-related helping: Findings from Project MATCH. Journal of Studies on Alcohol and Drugs. 2009b;10:117–125. doi: 10.15288/jsad.2009.70.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano ME. Service to Others in Sobriety (S0S) Research Plan, Phase I. Cleveland OH: Case Western Reserve University; 2005. Unpublished data. [Google Scholar]
- Penner LA, Finkelstein MA. Dispositional and structural determinants of volunteerism. Journal of Personality and Social Psychology. 1998;74(2):525–537. [Google Scholar]
- Penner LA, Fritzche BA, Craiger JP, Freifeld TS. Measuring the prosocial personality. In: Butcher JN, Spielberger CD, editors. Advances in personality assessment. Vol. 12. Hillsdale, NJ: Erlbaum; 1995. [Google Scholar]
- Post SG. Altruism and Health: Perspectives from Empirical Research. New York: Oxford University Press; 2007. [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Rietschlin J. Voluntary association membership and psychological distress. Journal of Health & Social Behavior. 1998;39(4):348–355. [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT User’s Guide, Version 9.1. Cary, NC: SAS Institute Inc; 2004. [Google Scholar]
- Schwartz C, Meisenhelder JB, Ma Y, Reed G. Altruistic social interest behaviors are associated with better mental health. Psychosomatic Medicine. 2003;65:778–785. doi: 10.1097/01.psy.0000079378.39062.d4. [DOI] [PubMed] [Google Scholar]
- Sheeren M. The relationship between relapse and involvement in Alcoholics Anonymous. Journal of Studies on Alcohol. 1988;49(1):104–106. doi: 10.15288/jsa.1988.49.104. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E. The reliability of the timeline method for assessing normal drinker college students’ recent drinking history: Utility for alcohol research. Addictive Behaviors. 1986;11:149–161. doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- Stout RL, Rubin A, Zwick W, Zywiak W, Bellino L. Optimizing the cost-effectiveness of alcohol treatment: A rationale for extended case monitoring. Addictive Behaviors. 1999;24:17–35. doi: 10.1016/s0306-4603(98)00029-x. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz P, Carbonari JP, Del Boca F. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;12(S):70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Connors GJ, Miller WR. Participation and involvement in Alcoholics Anonymous. In: Babor TF, Del Boca FK, editors. Treatment matching in alcoholism. New York: Cambridge University Press; 2003. pp. 184–204. [Google Scholar]
- Tonigan JS, Connors G, Miller WR. The Alcoholic Anonymous Involvement Scale (AAI): Reliability and Norms. Psychology of Addictive Behavior. 1996;10:75–80. [Google Scholar]
- Uggen C, Janikula J. Volunteerism and arrest in the transition to adulthood. Social Forces. 1999;78(1):331–362. [Google Scholar]
- Webb GR, Redman S, Hennrikus D, Rostas JA, Sanson-Fisher RW. The prevalence and sociodemographic correlates of high-risk and problem drinking at an industrial worksite. British Journal of Addiction. 1990;85:495–507. doi: 10.1111/j.1360-0443.1990.tb01670.x. [DOI] [PubMed] [Google Scholar]
- Wink P. Two faces of narcissism. Journal of Personality & Social Psychology. 1991;61(4):590–587. doi: 10.1037//0022-3514.61.4.590. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Pagano ME. Kickbacks from Helping Others: Health and Recovery. In: Galanter M, Kaskustas LA, editors. Recent Developments in Alcoholism. Research on Alcoholics Anonymous and Spirituality in Addiction Recovery. Vol. 18. New York: Springer; 2009. pp. 141–166. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Kaskutas LA. Helping, spirituality, and Alcoholics Anonymous in recovery. Journal of Studies on Alcohol. 2004;65(3):383–391. doi: 10.15288/jsa.2004.65.383. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Kaskutas LA, Ammon LN. In 12-step groups, helping helps the helper. Addiction. 2004;99:1015–1023. doi: 10.1111/j.1360-0443.2004.00782.x. [DOI] [PubMed] [Google Scholar]
- Zweben A, Rose SJ, Stout RL, Zywiak WH. Case monitoring and motivational style brief interventions. In: Hester RK, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. 3rd Edition. Boston: Allyn & Bacon; 2003. pp. 113–130. [Google Scholar]