Poor adherence to antihypertensive medications remains a significant challenge in the management of patients with hypertension. 1 , 2 , 3 , 4 Physicians and other health care providers are well aware that the benefits of prescribed medications are only available to those patients who take them; yet, medication adherence is seldom adequately addressed in the outpatient clinical setting. In fact, clinicians often do not ask patients about their medication‐taking behavior; and this may be for a variety of reasons. 5 , 6
For years, there has been discussion regarding adherence to the therapeutic alliance as a key factor in the management of hypertension. Initially termed “compliance,” 7 the problem was unfairly placed on the patient’s subservience to the dictates of the provider. Dr Harriet Dustan and one of the authors (EDF) brought this issue to the attention of the National High Blood Pressure Education Program suggesting that a more reasonable term might be a mutual “adherence” to the doctor–patient relationship. A special adherence program followed. Nevertheless, the terms “adherence” and “compliance” are often used interchangeably, although the term “adherence” seems to more accurately recognize the mutual responsibility of patients and caregivers to their joint involvement in medical care. 1 , 8
Regardless of the term, the fact remains that many adults with hypertension do not take their medications as prescribed, and poor adherence results in up to 50% of treatment failures. 9 Even for patients who partially adhere to prescribed therapies and may intermittently achieve blood pressure control, there is growing evidence that partial adherence may not provide adequate protection from target organ damage. 10 The multifactorial nature of poor adherence to prescribed antihypertensive medications has been well documented. 1 , 2 This includes factors which may be ascribed to the patient, the patients’ medical condition(s) and prognosis, the health care provider, the health care system, the prescribed treatment, socioeconomic variables, self‐management, and, clearly, other intangible factors (Table).
Table.
| Patient Characteristics | Clinical Factors | Health Care Systems Factors | Treatment Factors | Self‐Management/Behavioral Factors |
|---|---|---|---|---|
| Sociodemographics Inadequate social support Lack of hypertension knowledge Low self‐efficacy Poor quality of life Forgetfulness Low coping skills | Asymptomatic nature of hypertension Duration of hypertension Severity of hypertension Body mass index Depressive symptoms Other comorbid diseases | Health care provider characteristics/perceptions Dissatisfaction with health care Low access to health care Insurance status Pharmacy benefit | Number of medications Complexity of medication regimen Side effects of medications Costs of medications Ineffective or inappropriate choice of medication | Complementary and alternative medicine use Poor adherence to lifestyle modifications |
This discussion relates to one of these factors, the existence of one comorbid condition that complicates the clinical management of hypertension—endogenous depression. Although the association between depressive symptoms and poor adherence to medications has been recognized by investigators, it is critical that clinicians realize that this association is more than an “epidemiological finding” and that all of us take action in clinical settings to address the heretofore clinically underrecognized issue. We suggest herein that the ability for patients to cope with their problem of depressive symptoms and the need for the clinician to recognize that this comorbid condition is a barrier to hypertension management, if not in the management of the patient’s depression, should be addressed. These are important challenges that confront both parties of the doctor–patient relationship and contribute to the issue of therapeutic adherence.
Poor Antihypertensive Medication Adherence and Depression: Clinical Challenges
The National Council on Patient Information and Education has characterized low medication adherence as “America’s other drug problem” 11 which hinders the health care providers’ assessment of effectiveness of prescribed therapies. 12 , 13 Hypertension is one of the most important risk factors for stroke, coronary heart disease, heart failure, and endstage renal disease. Even though progress has been made in prevention, detection, and treatment of hypertension, it still remains a major public health burden affecting approximately 1 billion persons worldwide and 70 million people in the United States. 14 , 15 At present, blood pressure control is not optimal and over 36% of US adults treated for hypertension have uncontrolled blood pressure. 15 Poor adherence to antihypertensive medications is a major modifiable barrier to controlled blood pressure.
Depression is common in patients with chronic diseases including hypertension and is also associated with adverse health outcomes, poor quality of life, and excessive use of health care resources. 16 , 17 Although depression may be an independent diagnosis, it is also possible that depressive symptoms are secondary to chronic illnesses and their associated complex medication regimens. Regardless of the diagnosis being primary or secondary, prior reports have demonstrated that depressive symptoms are associated with inadequate blood pressure control and complications of hypertension. 18 More recently, investigators have reported associations between depressive symptoms and low antihypertensive medication adherence, 19 , 20 , 21 , 22 which may be mediated by self‐efficacy. 21 In one metaanalysis, investigators found that depressed persons with chronic medical conditions were 3 times more likely than those not depressed to be nonadherent to their prescribed treatment. 23 Despite the high prevalence of depression and anxiety disorders in clinical practice, previous studies have demonstrated that many patients with depression or anxiety seen in primary care settings did not receive appropriate treatment. 24
Comanagement of Hypertension and Depression: Making the Case
Physicians and other health care providers play a critical role in facilitating patients’ adherence to all medical treatments including antihypertensive medications. 12 , 25 In evaluating patients prescribed antihypertensive medications with uncontrolled blood pressure, providers should assess adherence to antihypertensive medications as well as to treatment recommendations for comorbid diseases. There are many approaches to assessing medication adherence in outpatient settings including self‐report surveys, pharmacy fill rates, pill counts, electronic monitoring, and bioassays; however, validated self‐report tools and pharmacy fill measures are emerging as the more practical tools for use in clinical settings. 6 , 26 , 27 With these tools becoming available, the assessment of adherence should be integral to the history‐taking for all patient visits. In those patients identified as poor adherers to prescribed medications who may be at risk for depression, clinicians should think about screening for and treating depression. If the screening is positive, then clinicians should confirm the diagnosis, consider management of depressive symptoms, and follow‐up to assess response to therapy (Figure). Screening for depression (using a short survey tool) in patients with coronary artery disease has been recommended recently by the American Heart Association. 28 Furthermore, in those patients with depression, physicians must also factor in management of comorbidities, especially cardiovascular diseases. 16
Figure.
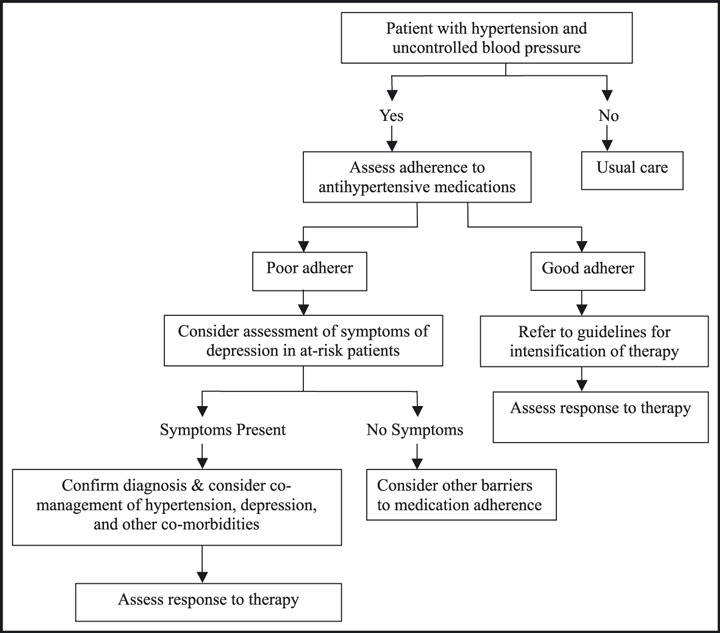
Flowchart for assessing blood pressure control, medication adherence, and depressive symptoms for patients with hypertension.
In a pilot randomized controlled trial of adults ages 50–80 years, combining depression and antihypertensive treatment in primary care practice resulted in a significant decline in depressive symptoms (Center for Epidemiologic Studies Depression Scale mean scores: 9.9 intervention group vs 19.3 usual care group; P<.01) and improved blood pressure control (mean systolic blood pressure 127.3 mm Hg intervention group vs 141.3 mm Hg control group; P<.01). Moreover, increased rates of medication adherence of both antihypertensive (78.1% intervention group vs 31.3% usual care; P<.01) as well as antidepressant (71.9% intervention group vs 31.3% usual care; P<.01) medication were observed. 29 Although benefits of comanagement of hypertension and depression were evident in this previous trial, health care providers are well aware of the clinical challenges regarding delayed onset of efficacy of antidepressant medications and the high proportion of depressed patients being poor responders and poor adherers to antidepressant medication. 30 It is necessary to follow patients comprehensively in order to assess their response to antidepressant and other therapies. Physicians and other health care providers should be cognizant of the effects of antidepressant medications on blood pressure 31 , 32 and extra care should be taken when treating depression in hypertensive older patients to minimize the side effects on blood pressure of antidepressant medication. 18 A recent systematic review has revealed the effectiveness of collaborative care interventions (ie, treatment provided through a combination of mental health and primary care providers within a target health care system) for the management of depression. 33 This collaborative approach may be important in providing high quality medical care in primary care practices given the limited resources available in most of these practices for managing mental health conditions. Given the profound impact of depression, the availability of proven pharmacologic and nonpharmacologic treatment for depression, and its poor recognition in clinical practice, systematic screening for depression in at‐risk patients should be considered. Health care organizations should move to comprehensive management programs that facilitate treatment of depressive symptoms along with the medical care for cardiovascular diseases and other comorbidities.
Other Clinical Implications
Clinicians must first recognize and then consider depression as a modifiable cofactor when uncontrolled blood pressure and poor adherence to antihypertensive medication are identified. Detection of patients suffering from depression would facilitate tailoring of clinical interventions for closer management of depression and hypertension to improve medication adherence, depressive symptoms, and blood pressure control in those patients with both chronic illnesses. Providers must also realize that there are factors other than depressive symptoms which may be associated with poor medication adherence and uncontrolled blood pressure; thus, providers should avoid targeting depression alone. 12 , 34 Other comorbidities in association with hypertension further increase the risk of cardiovascular events, and clinicians must also address the coexistence of diabetes mellitus, hyperlipidemia, atherosclerotic disease, heart failure, chronic renal disease, and obesity when indicated.
Future Directions
Although there is mounting evidence regarding the association between poor medication adherence, depressive symptoms, and uncontrolled blood pressure, assessment of patient adherence to prescribed medications, screening for depressive symptoms, and use of tailored interventions to improve adherence are rarely done in routine clinical practice. 35 This may be due, in part, to health care providers’ uncertainty about the role that adherence plays in blood pressure management for individual patients (eg, lack of a patient‐specific risk assessment tool). Furthermore, lack of access to validated and simple means to practically assess adherence, time management pressures in outpatient clinics, and the lack of effective interventions that can be feasibly applied in outpatient clinical settings hinder assessment of adherence in medical practice. 5 , 6 Earlier reports have called for an objective risk assessment model to be created through independent observations of patient characteristics, other factors associated with medication adherence, and validated assessment of medication adherence (ie, pharmacy fill and validated self‐report measures). 12 A risk assessment tool that can be realistically incorporated into clinical practice would help clinicians identify patients who are poor medication adherers along with their key barriers to adherence and facilitate triaging of these patients for tailored interventions. 25
The Cohort Study of Medication Adherence Among Older Adults (CoSMO) is a National Institutes of Health–funded prospective study with over 2000 older adults with essential hypertension enrolled in a single managed care organization. 2 It is being conducted to investigate determinants of and barriers to antihypertensive medication adherence and shed light on statistical models predicting low medication adherence (using validated tools) based on sociodemographic characteristics, treatment variables, health care system factors, clinical variables including depressive symptoms, and quality of life. Baseline results from CoSMO revealed that nearly 50% of older insured adult participants have low or medium adherence to prescribed antihypertensive medications by self‐report. Participants who were 65–74 years of age (vs 75 years or older), black (vs white), and had a higher body mass index (vs lower body mass index) were more likely to be low adherers. The 8‐item self‐report measure of medication adherence performed well with respect to pharmacy fill adherence and blood pressure control in older insured adults. 2 Participants with depressive symptoms were more likely to have low medication adherence by self‐report as those participants without depressive symptoms. 36 Long‐term data collection and multivariable analyses are underway and information is forthcoming regarding the association of depressive symptoms and other barriers to adherence on medication adherence, blood pressure control, and cardiovascular events. The results from this study should lay the groundwork for the development of interventions tailored to overcome patient‐specific barriers to adherence in outpatient settings in order to improve blood pressure control and reduce cardiovascular events. If future research on medication adherence is to move the field forward in a clinically meaningful way, then physicians and other health care providers must respond by developing and evaluating these interventions to improve medication adherence in their patients with chronic diseases. In addition, patients, clinicians, and health care organizations must work together to incorporate assessment of adherence and management of barriers (such as depressive symptoms) to taking antihypertensive medications into clinical practice if we are to increase the proportion of adults with hypertension whose blood pressure is under control. If we fail to follow through in this fashion, we are likely doomed to another 5 decades of bemoaning the lack of adherence to treatment by patients with comorbid chronic illnesses.
Disclosure: The project described was supported by Grant Number R01 AG022536 from the National Institute on Aging (Dr Krousel‐Wood, principal investigator). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health.
References
- 1. Krousel‐Wood M, Thomas S, Muntner P, et al. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19:357–362. [DOI] [PubMed] [Google Scholar]
- 2. Krousel‐Wood MA, Muntner P, Islam T, et al. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am. 2009;93:753–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hyre A, Krousel‐Wood MA, Muntner P, et al. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich). 2007;9:179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Krousel‐Wood M, Muntner P, Jannu A, et al. Reliability of a medication adherence measure in an outpatient setting. Am J Med Sci. 2005;330:128–133. [DOI] [PubMed] [Google Scholar]
- 5. Bokhour BG, Belowitz DR, Long JA, et al. How do providers assess antihypertensive medication adherence in medical encounters? J Gen Intern Med. 2006;21:577–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Krousel‐Wood MA, Islam T, Webber LS, et al. New medication adherence scale versus pharmacy fill rates in hypertensive seniors. Am J Manag Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]
- 7. Sackett DL. Introduction. In: Sackett DL, Haynes RB, eds. Compliance With Therapeutic Regimens. Baltimore, MD: Johns Hopkins University Press; 1976:1–6. [Google Scholar]
- 8. Elliott WJ. Compliance–and improving it–in hypertension. Manag Care. 2003;12:56–61. [PubMed] [Google Scholar]
- 9. Stephenson J. Noncompliance may cause half of antihypertensive drug “failures”. JAMA. 1999;282:313–314. [DOI] [PubMed] [Google Scholar]
- 10. Susic D, Krousel‐Wood M, Zhou X, et al. Partial adherence to antihypertensive therapy fails to achieve full cardiovascular benefits in hypertensive rats. Am J Med Sci. 2008;335:420–425. [DOI] [PubMed] [Google Scholar]
- 11. Bond WS, Hussar DA. Detection methods and strategies for improving medication compliance. Am J Hosp Pharm. 1991;38:1978–1988. [PubMed] [Google Scholar]
- 12. Harmon G, Lefante J, Krousel‐Wood MA. The role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21:310–315. [DOI] [PubMed] [Google Scholar]
- 13. Heisler M, Hogan MM, Hofer TP, et al. When more is not better: treatment intensification among hypertensive patients with poor medication adherence. Circulation. 2008;117:2884–2892. [DOI] [PubMed] [Google Scholar]
- 14. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 15. Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. [DOI] [PubMed] [Google Scholar]
- 16. Bogner HR, Cary MS, Bruce ML, et al. The role of medical comorbidity in outcome of major depression in primary care: the PROSPECT study. Am J Geriatr Psychiatry. 2005;13:861–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–3285. [DOI] [PubMed] [Google Scholar]
- 18. Scalco AZ, Scalco MZ, Azul JB, et al. Hypertension and depression. Clinics. 2005;60:241–250. [DOI] [PubMed] [Google Scholar]
- 19. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta‐analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. [DOI] [PubMed] [Google Scholar]
- 20. Kim MT, HanHR, HillMN, et al. Depression, substance use, adherence behaviors, and blood pressure in urban hypertensive black men. Ann Behav Med. 2003;26:24–31. [DOI] [PubMed] [Google Scholar]
- 21. Schoenthaler A, Ogedegbe G, Allegrante JP. Self‐efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive African Americans. Health Educ Behav. 2009;36:127–137. [DOI] [PubMed] [Google Scholar]
- 22. Wang PS, Bohn RL, Knight E, et al. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wing RR, Phelan S, Tate D. The role of adherence in mediating the relationship between depression and health outcomes. J Psychosom Res. 2002;53:877–881. [DOI] [PubMed] [Google Scholar]
- 24. Young AS, Klap R, Sherbourne CD, et al. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58:55–61. [DOI] [PubMed] [Google Scholar]
- 25. Krousel‐Wood M, Hyre A, Muntner P, et al. Methods to improve medication adherence in patients with hypertension: current status and future directions. Curr Opin Cardiol. 2005;20:296–300. [DOI] [PubMed] [Google Scholar]
- 26. Hawkshead J, Krousel‐Wood MA. Techniques of measuring medication adherence in hypertensive patients in outpatient settings: advantages and limitations. Dis Manage Health Outcomes. 2007;15:109–118. [Google Scholar]
- 27. Morisky DE, Ang A, Krousel‐Wood MA, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10:348–354. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 28. Lichtman JH, Bigger JT Jr, Blumenthal JA, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. [DOI] [PubMed] [Google Scholar]
- 29. Bogner HR, De Vries HF. Integration of depression and hypertension treatment: a pilot, randomized controlled trial. Ann Fam Med. 2008;6:295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Henkel V, Seemuller F, Obermeier M, et al. Does early improvement triggered by antidepressants predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord. 2009;115:439–449. Epub 2008 Nov 22. [DOI] [PubMed] [Google Scholar]
- 31. Amsterdam JD, Garcia‐Espana F, Fawcett J, et al. Blood pressure changes during short‐term fluoxetine treatment. J Clin Psychopharmacol. 1999;19:9–14. [DOI] [PubMed] [Google Scholar]
- 32. Scalco MZ, De Almeida OP, Hachul DT, et al. Comparison of risk of orthostatic hypotension in elderly depressed hypertensive women treated with nortriptyline and thiazides versus elderly depressed normotensive women treated with nortriptyline. Am J Cardiol. 2000;85:1156–1158. [DOI] [PubMed] [Google Scholar]
- 33. Chang‐Quan H, Bi‐Rong D, Zhen‐Chan L, et al. Collaborative care interventions for depression in the elderly: a systematic review of randomized controlled trials. J Investig Med. 2009;57:446–455. [DOI] [PubMed] [Google Scholar]
- 34. Rose LE, Kim MT, Dennison CR, et al. The contexts of adherence for African Americans with high blood pressure. J Adv Nurs. 2000;32:587–594. [DOI] [PubMed] [Google Scholar]
- 35. Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. [DOI] [PubMed] [Google Scholar]
- 36. Krouselwood MA, Islam T, Muntner P, et al. Depression and older adults: impact of depressive symptoms on medication adherence. Perspective from COSMO. American Heart Association 50th Cardiovascular Disease Epidemiology and Prevention Conference. March 4, 2010. San Francisco, CA: Abstract P237 in session “Aging.” [Google Scholar]


