Abstract
Itch is the most common symptom among patients presenting to the dermatology clinic. Scratching can cause mechanical trauma to the skin, further damaging the epidermal barrier and its function. This damage can facilitate the introduction of microbes that complicate the presenting disease and its management. Pruritus has a negative influence on quality of life. Initiation of treatment that can safely and effectively manage pruritus may provide immediate benefits to the patient. A novel topical formulation of hydrocortisone acetate 2.5% and pramoxine hydrochloride 1% in a hydrophilic lotion base is indicated for the management of pruritus. However, the rate of onset of antipruritic effects has not been well studied. This single-center, open-label, pilot study involved 11 subjects age 18 and older. All subjects applied hydrocortisone acetate 2.5% and pramoxine hydrochloride 1% lotion four times daily for one day. Severity of itch as measured by the visual analog scale decreased significantly following one day of medication use. The change in mean visual analog scale from baseline was -2.16±2.78 (P=0.0275), representing a mean percentage reduction of 31.74±42.11 (P=0.0315). Topical application of hydrocortisone acetate 2.5% and pramoxine hydrochloride 1% lotion provides a significant reduction in pruritus as rated by patients using the visual analog scale with a single day of use. Early onset of action to decrease itch is expected to improve the patient's treatment experience and increase the level of long-term adherence.
Itch is the most common symptom among patients presenting to the dermatology clinic.1,2 The incidence of pruritus in the community setting has been reported to be as high as 27 percent. It is generally associated with increased stress and possibly associated with negative psychological factors.3 Itch is recognized as a consequence of impaired epidermal barrier.4 As such, it is considered an associated symptom of atopic dermatitis (AD), contact dermatitis (CD), and allergic contact dermatitis (ACD), such as poison ivy and psoriasis. Itch provokes scratching, which in turn intensifies pruritus. This phenomenon, known as the “itch-scratch cycle,” is of particular concern in chronic dermatoses, such as AD.
Scratching can cause mechanical trauma to the skin, further damaging the epidermal barrier and its function, and can potentially facilitate the introduction of microbes5 that can complicate the presenting disease and its management. Furthermore, the experience of itch has been shown to disrupt sleep and negatively influence concentration, academic and work performance, and quality of life.6 Therefore, initiation of treatment that can safely and effectively manage pruritus may provide immediate benefits to the patient's quality of life and could provide long-term benefit by interrupting the itch-scratch cycle that prolongs the disease course.
A novel topical formulation of hydrocortisone acetate 2.5% and pramoxine hydrochloride 1% in a hydrophilic lotion base is indicated for the management of pruritus. However, the rate of onset of antipruritic effects has not been well studied. Data from a pilot study, reported here, suggest a rapid onset of effect, evident within 24 hours of therapy initiation.
Background
Pruritus is characteristic of several dermatoses and is considered a symptom of barrier dysfunction. Reported rates of pruritus among adult patients with AD are as high as 83 percent.7 In murine models of AD, prolonged scratching was noted in response to decreased epidermal barrier function and was found to be independent of the effects of histamine and serotonin. Furthermore, application of petrolatum provided temporary improvement of barrier function and produced a decrease in scratching.8
In in-vivo studies of human atopic subjects, affected individuals exhibited an overactive sympathetic response to itch and scratching. Furthermore, parasympathetic tone was persistently and rigidly elevated, which was considered an indication of lack of adaptability in response to stress.9 Some evidence exists supporting the supposition that patients with AD experience pruritus via a different physiological pathway from that in patients without AD.9 Histamine has historically been identified as a primary mediator of itch development. Emerging evidence has shown that several other mediators are associated with itch in AD, including serine proteases, interleukin 31, and nerve growth factor.10
Among adult patients with AD, 83.1 percent of individuals in one study7 reported prutitus most frequently in the evening (52.8 percent) and at night (38.2 percent).7 Severity of pruritus correlated with severity of AD. A significant proportion (81 percent) of patients who reported itch said it caused difficulty in falling asleep. Dryness, sweat, physical effort, food, and hot baths were reported by subjects to exacerbate itch. Patients variably reported use of topical emollients and oral antihistamines with limited long-term benefit. Patients with more severe disease reported more intense pruritus.
Study Design and Methods
This was a single-center, open-label, pilot study involving 11 subjects age 18 and older (mean age=40.8±11.4). Four subjects were Caucasian (36.4%), and seven subjects were African American (63.6%) (Table 1).
Table 1.
Subject demographics (n=11)
| GENDER | ||
| Male | 3 (27.3%) | |
| Female | 8 (72.7%) | |
| AGE (YEARS) | ||
| Mean±SD | 40.8±11.4 | |
| Median (P25, P75) | 40 (33, 50) | |
| Min, Max | 20, 56 | |
| RACE | ||
| Caucasian | 4 (36.4%) | |
| African American | 7 (63.6%) | |
All subjects applied hydrocortisone acetate 2.5% and pramoxine hydrochloride 1% lotion four times daily for one day. The study consisted of two study visits: Baseline and Day 1. Therapy was administered on Day 0 and final assessments were made on Day 1. Visual analog scale (VAS) scores were recorded at Baseline and Day 1.
Prior to Day 0, patients were not permitted to apply topical prescription steroids for one day; oral antihistamines and over-the-counter cough/cold products that contain antihistamines for one week; and systemic immunosuppressants or investigational drugs, oral steroids, or immunomodulators for four weeks.
Statistical analysis was completed with paired t-test/Wilcoxon signed-rank test.
Results
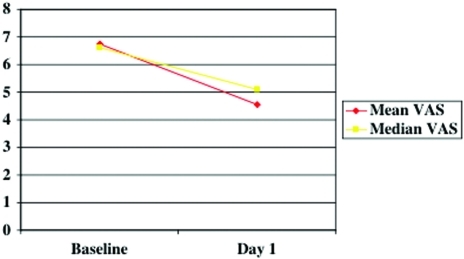
Severity of itch as measured by the VAS (Figure 1) decreased significantly following one day of medication use. Mean VAS score at baseline was 6.72±0.97; median VAS score at baseline was 6.60. On Day 1, mean VAS score was 4.56±2.81; median VAS score was 5.10. Baseline and Day 1 VAS scores are shown in Figure 2.
Figure 1.
Visual analog scale
Figure 2.
Mean and median visual analog scale scores
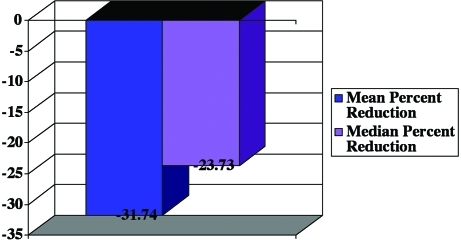
The change in mean VAS score from baseline was -2.16±2.78 (P=0.0275), representing a mean percentage reduction of 31.74±42.11 (P=0.0315) (Figure 3). Treatment was well tolerated with no significant adverse events reported.
Figure 3.
Percentage reduction in visual analog scale score
Conclusion and Discussion
Pruritus is common in AD and other inflammatory dermatoses. Itch-associated negative sequelae, including interrupted/delayed sleep and decreased quality of life, are prevalent.11 Many patients report that common interventions recommended to manage itch, including regular use of emollients and oral antihistamines, fail to provide long-term benefit. Therefore, there is a need for an effective intervention that is convenient, rapidly effective, and safe.
Data from this pilot study indicate that hydrocortisone acetate 2.5% and pramoxine hydrochloride 1% lotion is a rapidly effective and well-tolerated treatment option. Pramoxine is a mild local anesthetic with a history of use for management of pruritus. It is not a member of the class of “caine” anesthetics. Pramoxine appears to confer its antipruritic effects by stabilizing neuronal membranes of nerve endings.
The oil-in-water lotion base investigated in this trial was well tolerated with no reports of significant adverse events. The formulation contains a reverse emulsion of 70 percent lipids dispersed in 30 percent water. The unique hydrolipid emollient vehicle is expected to improve transepidermal water loss and contribute to improved barrier function, providing further benefit in the management of itch in AD.
Topical application of hydrocortisone acetate 2.5% and pramoxine hydrochloride 1% lotion provides a significant reduction in pruritus as rated by patients using the VAS with a single day of use. Early onset of action to decrease itch is expected to improve the patient's treatment experience and increase the level of long-term adherence.
References
- 1. Weisshaar E, Dalgard F. Epidemiology of itch: adding to the burden of skin morbidity. Acta Derm Venereol. 2009;89(4):339–350. doi: 10.2340/00015555-0662. [DOI] [PubMed] [Google Scholar]
- 2. Matterne U, Strassner T, Apfelbacher CJ, Diepgen TL, Weisshaar E. Measuring the prevalence of chronic itch in the general population: development and validation of a questionnaire for use in large-scale studies. Acta Derm Venereol. 2009;89(3):250–256. doi: 10.2340/00015555-0641. [DOI] [PubMed] [Google Scholar]
- 3. Dalgard F, Lien L, Dalen I. Itch in the community: associations with psychosocial factors among adults. J Eur Acad Dermatol Venereol. 2007;21(9):1215–1219. doi: 10.1111/j.1468-3083.2007.02234.x. [DOI] [PubMed] [Google Scholar]
- 4. Meyer-Hoffert U. Reddish, scaly, and itchy: how proteases and their inhibitors contribute to inflammatory skin diseases. Arch Immunol Ther Exp (Warsz) 2009;57(5):345–354. doi: 10.1007/s00005-009-0045-6. Epub 2009 Aug 18. [DOI] [PubMed] [Google Scholar]
- 5. Arnold LM, Starck LO, McElroy SL. Treatment of psychogenic excoriation in the elderly patient. Clin Geriatrics. 2002;10:36–46. [Google Scholar]
- 6. Kelsay K, Klinnert M, Bender B. Addressing psychosocial aspects of atopic dermatitis. Immunol Allergy Clin North Am. 2010;30(3):385–396. doi: 10.1016/j.iac.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 7. Chrostowska-Plak D, Salomon J, Reich A, Szepietowski JC. Clinical aspects of itch in adult atopic dermatitis patients. Acta Derm Venereol. 2009;89(4):379–383. doi: 10.2340/00015555-0676. [DOI] [PubMed] [Google Scholar]
- 8. Fujii M, Nabe T, Tomozawa J, Kohno S. Involvement of skin barrier dysfunction in itch-related scratching in special diet-fed hairless mice. Eur J Pharmacol. 2006;530(1-2):152–156. doi: 10.1016/j.ejphar.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 9. Tran BW, Papoiu AD, Russoniello CV, et al. Effect of itch, scratching and mental stress on autonomic nervous system function in atopic dermatitis. Acta Derm Venereol. 2010;90(4):354–361. doi: 10.2340/00015555-0890. [DOI] [PubMed] [Google Scholar]
- 10. Yosipovitch G, Papoiu AD. What causes itch in atopic dermatitis? Curr Allergy Asthma Rep. 2008;8(4):306–311. doi: 10.1007/s11882-008-0049-z. [DOI] [PubMed] [Google Scholar]
- 11. Bender BG, Ballard R, Canono B, Murphy JR, Leung DY. Disease severity, scratching, and sleep quality in patients with atopic dermatitis. J Am Acad Dermatol. 2008;58(3):415–420. doi: 10.1016/j.jaad.2007.10.010. [DOI] [PubMed] [Google Scholar]