Abstract
Objective: To evaluate the efficacy and tolerance of a facial hydrating serum when added to a moisturizer regimen compared to a moisturizer regimen alone. Design: Evaluator-blinded, single-center, clinical study with investigator assessments at Baseline and Week 2. Treatment: After washing with a facial cleanser in the morning and evening, subjects either applied the hydrating serum to their face followed by application of the moisturizer or applied only a moisturizer. Participants: Thirty-two women, aged 25 to 55 years with Fitzpatrick skin types I to V and normal or self-perceived dry skin completed the study. Seventeen subjects (Group 1) aged 25 to 51 years were randomly assigned to receive the facial hydrating serum in addition to a moisturizer regimen, whereas 15 subjects (Group 2) aged 34 to 55 years, were randomized to receive the moisturizer regimen alone. Measurements: Visual grading of the condition of the facial skin with regard to dryness, tactile roughness and softness, rating of irritation (subjective and objective), and digital photography. A self-assessment questionnaire was also employed to assess patient satisfaction. Results: Clinical assessments by the investigator showed statistically significant improvements (P<0.02) in facial skin parameters (reduction in dryness and increased skin softness) after two weeks of combined use of the hydrating serum and moisturizer compared to the group who used moisturizer alone. No adverse events were reported during the course of the study. Conclusion: The results from a two-week clinical study demonstrate that this facial hydrating serum was well tolerated and effective in improving facial dry skin parameters beyond that obtained with a moisturizer alone.
The skin is the largest organ of the body and serves to protect the body against physical and chemical injury, control evaporative loss of body water, assist in thermoregulatory homeostasis, provide defense against infectious organisms, and act as a signaling source for general health, reproduction, communication, age, and gender. Exposing the skin to various stressors, including environmental and workplace chemicals, pollutants, smoke, microorganisms, aggressive and potentially irritating cleansing and anti-aging regimens, and extreme environmental temperatures (especially with low humidity), may cause dry skin and skin barrier abnormalities. These untoward changes can result in a degraded and unhealthy appearance of the skin and, if severe enough, may compromise skin functions.
Chronologically aged skin appears dry, thin, and flattened with loss of elasticity and architectural regularity.1,2 Although the skin contains a high percentage of water, which is essential for normal functioning, the moisture content of the skin decreases with increasing age.3 Dehydration of the skin can lead to the development of scaly, taut skin, superficial lines, premature aging, and wrinkles. Studies have shown a significant age-related decline in natural moisturizing factor (NMF). NMF contains hygroscopic components found in the stratum corneum (SC) that act as efficient humectants.4 It is likely that the loss of NMF is exacerbated by an age-related decline in barrier function, which can further accelerate transepidermal water loss (TEWL) from the skin.5 The ability of the skin to retain water is primarily a function of the outermost, nonviable layer of the epidermis, SC, which also acts as a protective barrier for the body. Over the past few decades, the constituents of skin have been better characterized and it is now known that the extracellular matrix (ECM) provides the skin with its major hydration properties. The ECM is comprised of an organized structure of glycosaminoglycans, proteoglycans, glycoproteins, growth factors, and structural proteins, such as collagen and elastin. A major component of the ECM is hyaluronic acid (HA) or hyaluronan.6 HA is a naturally occurring anionic polysaccharide most abundantly present in mammalian skin where it is localized not only in the dermis (≈0.5mg/g wet tissue), but also in the epidermis (≈0.1mg/g wet tissue).7,8 HA, which is produced mainly by fibroblasts and keratinocytes in the skin, binds to the extracellular space via the receptor CD44 and may play an important role in epidermal barrier function and SC hydration.8,9 In general, polysaccharides are regarded as moisture-controlling substances—the rationale for their inclusion in many topical cosmetic agents.10 Due to its considerable capacity to bind water, HA has greater skin hydration properties than other polysaccharides.11 Topical application of HA increases hydration of the SC largely through a humectant effect.12
The facial hydrating serum was formulated to repair and replenish normal-to-mature skin with critical hydration. The serum contains vitamin B5 analogs, HA (high- and low-molecular weight), an amino acid derivative of glycine, a complex of xylitol-based sugars, and a natural matrix metalloproteinase inhibitor (MMP).
The purpose of this two-week, investigator-blinded, single-center study was to evaluate the efficacy and tolerance of a novel facial hydrating serum to enhance moisturization beyond that achieved from using a moisturizer alone. The study was conducted in January 2009 in an alpine desert climate that is stressful to the skin (i.e., 6000-foot elevation with average temperature range of 14–42·F and low humidity).
Methods
Study population. The criteria for study participation included healthy women aged 25 to 55 years with Fitzpatrick skin types I to V and normal or self-perceived dry skin. Subjects were randomly assigned to one of two groups. Group 1 participants were put on a regimen of facial hydrating serum and moisturizer. Group 2 participants were put on a regimen of moisturizer alone.
Written, informed consent conforming to 21 CFR 50.25 was obtained from each subject prior to enrollment in the study. The study was conducted during the month of January 2009 in Colorado Springs, Colorado.
Study design. During the two-week, investigator-blinded study, clinical evaluations were conducted at Baseline and Week 2.
Study endpoints. Efficacy. The investigator graded each subject globally on the face for dryness, tactile roughness, and softness at Baseline and Week 2. Dryness was graded using a 10-point scale where 0=none, 0.5 to 3.5=mild, 4.0 to 6.5=moderate, and 7 to 9=severe. Tactile roughness was graded using a 10-point scale where 0=very smooth, 0.5 to 2.5=smooth with very occasional rough areas, 3 to 4.5=mild roughness, 5 to 7=moderate roughness, and 7.5 to 9=severe roughness. Softness was graded using a 10-point scale where 0=very soft, 0.5 to 3.5=slightly more resistance to pressure, 4 to 7.5=moderate resistance to pressure and 8 to 9=very hard like a callous.
Tolerance was assessed by the investigator for objective and subjective irritation parameters and from the reporting of adverse events. Objective irritation (e.g., erythema, scaling) and subjective irritation (e.g., burning, stinging, itching, and tingling) were graded on a scale of 0 to 3 (with half points allowed) at Baseline and Week 2.
Subject self-assessment. Subjects completed a self-assessment questionnaire at Week 2 related to statements about their experience using the facial hydrating serum “immediately after applying” and “with continued use.” Subjects answered questions with “strongly agree,” “agree,” “disagree,” and “strongly disagree.” Self-assessment questionnaire responses were tabulated and a top-box analysis was performed.
Statistical Analysis
Comparisons, based on the average change from baseline, were conducted using analysis of variance (ANOVA) with paired t-tests to determine significant differences between Group 1 and Group 2 at the p≤0.05 level.
Results
Demographics. Thirty-two women aged 25 to 55 years with Fitzpatrick skin types I to V and normal or self-perceived dry skin, entered and completed the study. Seventeen subjects (Group 1) aged 25 to 51 years (median=44 years) were randomly assigned to receive the facial hydrating serum in addition to a moisturizer regimen, whereas 15 subjects (Group 2) aged 34 to 55 years (median=44 years) were randomly assigned to receive the moisturizer regimen alone. The demographics of the two groups are presented in Table 1. Subjects in both groups were of similar age and the majority of subjects were of Caucasian ethnicity.
Table 1.
Subject demographics
| FACIAL HYDRATING SERUM PLUS MOISTURIZER | ETHNICITY | AGE | FITZPATRICK SKIN TYPE |
|---|---|---|---|
| 1 | Hispanic | 48 | III |
| 2 | Caucasian | 26 | III |
| 3 | Caucasian | 29 | II |
| 4 | Caucasian | 34 | III |
| 5 | Caucasian | 44 | III |
| 6 | Caucasian | 46 | II |
| 7 | Caucasian | 51 | III |
| 8 | Caucasian | 42 | III |
| 9 | Caucasian | 54 | IV |
| 10 | Caucasian | 25 | II |
| 11 | Caucasian | 25 | II |
| 12 | African American | 38 | V |
| 13 | Asian | 51 | III |
| 14 | Caucasian | 51 | I |
| 15 | Caucasian | 49 | II |
| 16 | Caucasian | 49 | I |
| 17 | Caucasian | 25 | I |
| MOISTURIZER ALONE | ETHNICITY | AGE | FITZPATRICK SKIN TYPE |
|---|---|---|---|
| 1 | Caucasian | 34 | II |
| 2 | Caucasian | 55 | III |
| 3 | Caucasian | 44 | III |
| 4 | Caucasian | 35 | II |
| 5 | African American | 48 | IV |
| 6 | Caucasian | 48 | IV |
| 7 | Hispanic | 44 | III |
| 8 | Hispanic | 41 | IV |
| 9 | Hispanic | 34 | IV |
| 10 | Caucasian | 39 | I |
| 11 | Caucasian | 38 | III |
| 12 | Caucasian | 34 | II |
| 13 | Caucasian | 50 | I |
| 14 | Caucasian | 49 | IV |
| 15 | Asian | 50 | II |
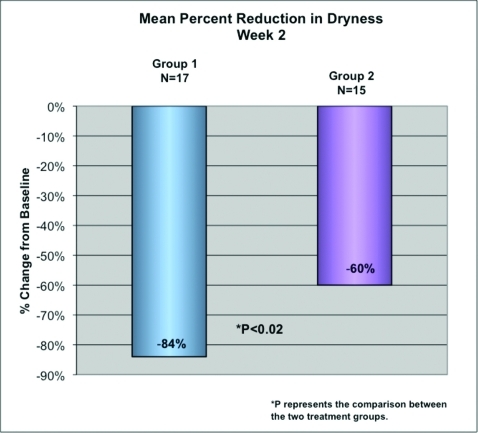
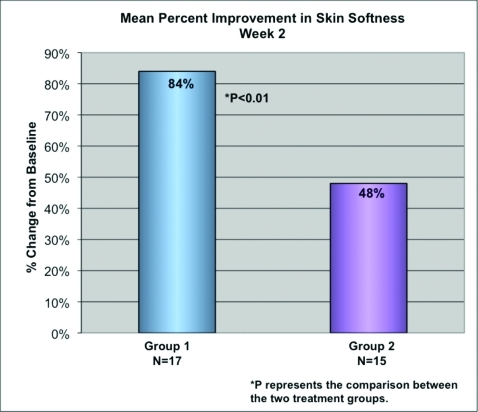
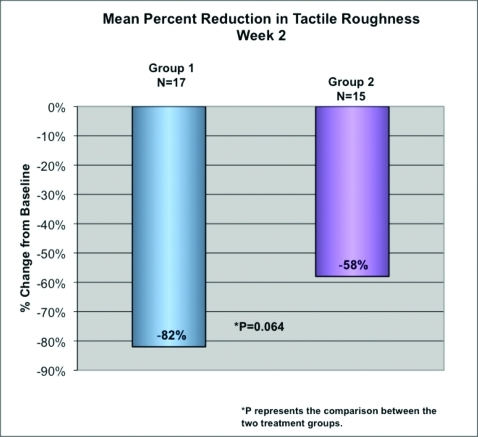
Efficacy. Clinical assessments by the investigator showed that both Group 1 and Group 2 demonstrated significant reductions in dryness and tactile roughness and improvements in softness at Week 2 compared to Baseline (all p<0.0001). Clinical assessments by the investigator also showed statistically significant improvements (P<0.02) in facial skin parameters (reduction in dryness and increased skin softness) after two weeks of use in Group 1 compared to Group 2 (Figures 1 and 2). Tactile roughness also showed a trend toward statistical significance (p=0.064) (Figure 3). Results of the top-box analysis of the self-assessment questionnaires are shown in Table 2. Overall, 94 percent of subjects felt the hydrating serum increased moisturization of the skin and 94 percent were interested in continuing the use of this facial hydrating serum at the conclusion of the study. A photograph of a Group 1 subject at baseline and after two weeks of treatment showed enhanced moisturization (Figure 4).
Figure 1.
Mean reductions in investigator-graded dryness
Figure 2.
Mean improvement in investigator-graded skin softness
Figure 3.
Mean reduction in investigator-graded tactile roughness
Table 2.
Subject self-assessment of facial hydrating serum attributes after two weeks treatment
| PRODUCT ATTRIBUTES AT WEEK 2 | PERCENTAGE OF PATIENTS AGREE OR STRONGLY AGREE |
|---|---|
| Overall satisfaction (excellent or good) | 82% |
| Improves smoothness of skin | 94% |
| Increases moisturization of skin | 94% |
| Improves texture of skin | 88% |
| Increases radiance or glow of skin | 88% |
| Provides a moisturizing base for makeup | 92% |
| Makes skin look healthier and more youthful | 82% |
| Makes skin feel softer and more supple | 100% |
| Increases hydration of skin | 88% |
| Convenient to use as part of daily skin-care regimen | 94% |
| Improves softness of skin | 94% |
| Improves overall appearance of skin | 82% |
Figure 4.


Photograph of Group 1 subject at baseline (left) and after two weeks of treatment (right)
Safety. The facial hydrating serum was very well tolerated and there were no adverse events related to the serum during the course of the study.
Discussion
Despite expected changes associated with the normal aging process, society continues to strive for a healthy youthful appearance. The appearance and feel of skin are central to the perception of personal skin health, beauty, and attraction. It is well accepted that cleansing and moisturizing are two basic means of maintaining good skin health. Adequate skin hydration is absolutely critical for the maintenance of healthy skin.
The mechanisms for maintaining skin hydration are complex, but understanding has greatly improved over recent years. It has now been shown that glycerol exists in the SC as a natural endogenous humectant and HA, previously regarded primarily as a dermal component, is also found in the epidermis and is critical for the maintenance of normal SC structure, hydration, and function of the epidermal barrier.12 While increasing age does not decrease hyaluronan concentrations in the skin, there is increased binding with tissue structures that result in a diminished ability of HA to absorb water of hydration with subsequent loss in skin moisture.13 Animal and human studies have shown that topically applied HA gel disseminates through all layers of intact skin and passes rapidly into the dermis before its eventual metabolic degradation. HA absorption through the skin is not restricted to smaller polymers as demonstrated by the recovery of high molecular weight polymers (360–400kDa).14 The addition of HA to topical formulations also provides a smooth and viscous feel. After application to the skin, a hydrated film is formed that holds water for an extended period and confers the properties of a moisturizer.6
Moisturizing or hydrating agents are important components in a basic skin care regimen. They protect the skin from daily insults of the environment and assist in preventing premature skin aging. The combination of novel ingredients in the facial hydrating serum was designed to provide rapid and long-lasting benefit in maintaining skin hydration. This data demonstrate the additive skin hydration and softening benefits from using the hydrating serum with a standard moisturizer compared to using the moisturizer alone.
References
- 1. Loden M. Role of topical emollients and moisturizers in the treatment of dry skin barrier disorders. Am J Clin Dermatol. 2003;4:771–788. doi: 10.2165/00128071-200304110-00005. [DOI] [PubMed] [Google Scholar]
- 2. Callaghan TM, Wilhelm K-P. A review of aging and an examination of clinical methods in the assessment of aging skin. Part 1: cellular and molecular perspectives of skin aging. Inter J Cosmet Sci. 2008;30:313–322. doi: 10.1111/j.1468-2494.2008.00454.x. [DOI] [PubMed] [Google Scholar]
- 3. Potts RO, Buras EM, Chrisman DA. Changes with age in moisture content of human skin. J Invest Dermatol. 1984;82:97–100. doi: 10.1111/1523-1747.ep12259203. [DOI] [PubMed] [Google Scholar]
- 4. Rawlings AV, Harding CR. Moisturization and skin barrier function. Dermatol Ther. 2004;17:43–48. doi: 10.1111/j.1396-0296.2004.04s1005.x. [DOI] [PubMed] [Google Scholar]
- 5. Ghadially R, Brown BE, Sequeira-Martin SM, et al. The aged epidermal permeability barrier-structural, functional and lipid biochemical abnormalities in humans and a senescent murine model. J Clin Invest. 1995;95:2281–2290. doi: 10.1172/JCI117919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neudecker BA, Csoka AB, Mio K, et al. Hyaluronan: the natural skin moisturizer. In: Elsner P, Maibach HI, editors. Cosmeceuticals: Drugs vs. Cosmetics. New York, NY: Marcel Dekker; 2000. pp. 319–352. [Google Scholar]
- 7. Brown MB, Jones SA. Hyaluronic acid: a unique topical vehicle for localized delivery of drugs to the skin. J Eur Acad Dermatol Venereol. 2005;19:308–318. doi: 10.1111/j.1468-3083.2004.01180.x. [DOI] [PubMed] [Google Scholar]
- 8. Tammi R, Ripellino JA, Margolis RU, Tammi M. Localization of epidermal hyaluronic acid using the hyaluronate binding region of cartilage proteoglycan as a specific probe. J Invest Dermatol. 1998;90:412–414. doi: 10.1111/1523-1747.ep12456530. [DOI] [PubMed] [Google Scholar]
- 9. Sakai S, Yasuda R, Sayo T, et al. Hyaluronan exists in the normal stratum corneum. J Invest Dermatol. 2000;114:1184-1187. doi: 10.1046/j.1523-1747.2000.00992.x. [DOI] [PubMed] [Google Scholar]
- 10.Whistler RL. Introduction to industrial gums. In: Whistler RL, BeMiller JN, editors. Industrial Gums: Polysaccharides and Their Derivatives. San Diego: Academic Press; 1993. pp. 1–3. [Google Scholar]
- 11.Cowman MK, Liu J, Hittner DM, Kim JS. Hyaluronan interactions: salt, water, ions. In: Laurent TC, editor. The Chemistry, Biology and Medical Applications of Hyaluronan and its Derivatives. London: Portland Press; 1998. pp. 17–25. [Google Scholar]
- 12. Verdier-Sevrain S, Bonte F. Skin hydration: a review on its molecular mechanisms. J Cosmet Dermatol. 2007;6:75–82. doi: 10.1111/j.1473-2165.2007.00300.x. [DOI] [PubMed] [Google Scholar]
- 13. Meyer LJ, Stern R. Age-dependent changes of hyaluronan in human skin. J Invest Dermatol. 1994;102:385–389. doi: 10.1111/1523-1747.ep12371800. [DOI] [PubMed] [Google Scholar]
- 14. Brown TJ, Alcorn D, Fraser JRE. Absorption of hyaluronan applied to the surface of intact skin. J Invest Dermatol. 1999;113:740–746. doi: 10.1046/j.1523-1747.1999.00745.x. [DOI] [PubMed] [Google Scholar]