Abstract
Purpose
We used principles of community-based participatory research (CBPR) to develop and pilot test a 5-week intervention for middle school students, Students for Nutrition and eXercise (SNaX). SNaX aimed to translate school obesity-prevention policies into practice with peer advocacy of healthy eating and school cafeteria changes.
Methods
425 7th graders in the intervention school (63% of all 7th graders) were surveyed at baseline regarding cafeteria attitudes and sugar-sweetened beverage (SSB) consumption; of the 425 students, 399 (94%) were surveyed again at one-month post-intervention. School cafeteria records were obtained from the intervention school and a non-randomly selected comparison school with similar student socio-demographic characteristics.
Results
140 intervention school students were trained as peer advocates. In the intervention school, cafeteria attitudes among peer advocates significantly improved over time (~one-third of a standard deviation), whereas non-peer advocates’ cafeteria attitudes remained stable; the improvement among peer advocates was significantly greater than the pre-post change for non-peer advocates (b = 0.71, p <.001). Peer advocates significantly reduced their SSB intake (sports and fruit drinks), from 33% pre-intervention to 21% post-intervention (p = .03). Cafeteria records indicated that servings of fruit and healthier entrees (salads, sandwiches, yogurt parfaits) significantly decreased in the comparison school and significantly increased in the intervention school; the magnitude of changes differed significantly between schools (p <.001).
Conclusions
Peer advocates appeared to benefit from the intervention more than did non-peer advocates. Future research should consider engaging parents, students, and other key community stakeholders to determine acceptable and sustainable cafeteria changes.
Keywords: Community-Based Participatory Research (CBPR), Nutrition, Obesity, School
Introduction
Current policy targets schools as key settings in which to address child obesity [1–3]. Schools can promote healthy eating (e.g., by establishing nutritional guidelines for foods served and sold in schools) and physical activity in physical education (PE) classes (e.g., through PE provision requirements) [4]. Although most obesity prevention policies focus on school food changes, almost none mandate improved marketing of school food in tandem with nutritional improvements. Marketing may be necessary to obtain acceptance of school food changes from students, parents, and school staff, and to increase awareness about new healthy food options.
Few randomized controlled trials of middle school obesity prevention interventions have examined effects of school food improvements paired with marketing. Teens Eating for Energy and Nutrition in Schools (TEENS) consisted of increased availability and marketing of fruits and vegetables in the cafeteria, class-based nutritional education, student-led in-class discussions on nutrition, and family assignments [5, 6]; intervention-control differences in students’ dietary behaviors were non-significant two-years post-baseline. Trying Alternative Cafeteria Options (TACOS) paired increased availability with student-led promotions of lower-fat cafeteria options [7]; after two-years, intervention schools offered and sold more lower-fat foods than did control schools, but students did not report healthier eating. MSPAN (Middle School Physical Activity and Nutrition) provided and marketed lower-fat food at school and involved a small number of student advocates to promote healthy eating; it did not significantly reduce fat intake [8]. Thompson et al[9] found that increased fruit and vegetable availability plus educational posters significantly increased fruit, fruit juice, and fried (but not raw) vegetable intake.
We developed and piloted an intervention for middle school students, Students for Nutrition and eXercise (SNaX), which aimed to translate one school district’s obesity-prevention policy into practice through peer leader advocacy of healthy eating and school cafeteria changes, including improved signage, point-of-sale nutritional information postings, and introduction of a new food option (sliced fruit). SNaX was developed using principles of community-based participatory research (CBPR) [10, 11], by academic researchers and community stakeholders (e.g., students, parents, teachers, administrators) of the Los Angeles Unified School District (LAUSD).[12] SNaX’s peer leader component, which engaged a substantial proportion of the seventh grade class in peer advocacy, was more intensive and involved a greater number of students as peer leaders than other published school-based obesity-prevention interventions. Because peer influence increases substantially during middle school [13], middle school peer advocates can bee effective change agents [14–17].
SNaX’s theoretical basis combines social-cognitive health behavior change constructs and ecological influences that may limit and control opportunities for healthy behaviors [18]. Social-cognitive factors (e.g., self-efficacy, attitudes, norms) contribute to youths’ dietary and exercise behaviors [19–22]. To change school-wide attitudes and behaviors, peer leaders modeled and promoted healthy behaviors, and imparted knowledge to other students about ways to change behavior through face-to-face discussions and handouts; cafeteria changes provided access to healthy foods. Consistent with prior research [5, 23], we expected stronger effects among peer leaders, who received the most direct exposure to the intervention.
Methods
Human Subjects Protection
This research was approved by the RAND Human Subjects Protection Committee and the LAUSD Committee for External Research Review. Parents provided informed consent for children; children provided assent. Parent consent forms were distributed in-class for children to give to parents.
Intervention Setting
LAUSD is at the forefront of efforts to improve school food and increase physical activity, enacting policies [24–26] to ban the sale of unhealthy beverages; mandate collaboration with researchers, parents, and students to increase participation in the US Department of Agriculture’s (USDA’s) National School Lunch Program (NSLP; provides ~1/3 of a child’s daily caloric intake and Recommended Dietary Allowance of protein, calcium, iron, and vitamins A and C, for students eligible by income for free or reduced-price meals); improve NSLP food nutritional content and marketing; and post point-of-sale nutritional information. Consistent with research showing seasonal decreases in nutritional intake [27–30], Food Services Branch records generally show seasonal decreases in NSLP participation over the spring semester (when SNaX was conducted).
School district administrators were equal partners with academic researchers. The team partnered with three community advisory boards, one of community stakeholders where the intervention was pilot-tested, one of individuals invested in youth obesity issues, and one of high school students. Formative research [12, 31, 32] involved community partners in identifying community needs and priorities.
Intervention Protocol
Peer advocacy
Peer leaders attended a club in which they learned how to distribute healthy samples (cafeteria food, water) and bookmarks with educational messages to other students during lunchtime. Each peer leader participated for one week during the five-week club. Based on diffusion of innovation theory [33], for optimal diffusion of key messages across a population, ≥15% of a target group should be trained as advocates [16, 34]. Thus, we recruited a new group of peer leaders from the seventh grade class each week, and asked each one to recruit a partner for advocacy activities, in order to reach a ‘critical mass’ of advocates for behavior change. A total of 673 seventh graders were enrolled in the intervention school; 90 peer leaders (~18 per week) and 66 partners participated (16 of the 66 partners were also peer leaders). Thus, 140 peer leaders and partners (21% of the seventh-grade population) were peer advocates. They were given $20 gift cards for participation.
In the club, adult facilitators focused on a different topic each week (healthy and unhealthy beverages, including water and sugar-sweetened beverages or SSBs; fruits; vegetables; two sessions on school cafeteria food benefits). Physical activity was discussed in each session (i.e., balancing intake with exercise). Peer leaders played a quiz game on each topic. To elicit behavior change, facilitators discussed healthy eating and physical activity using a motivational interviewing (MI) style (open-ended questions; reflective listening; exploration of ambivalence about healthy behaviors and reasons for healthy and less healthy behaviors) [35]; students were trained in role-plays to use an MI style to discuss healthy eating and physical activity with their peers at lunchtime
Two raters observed whether key MI elements (i.e., elicitation of student responses, positive feedback, respect for students, role plays) were covered in each session (1, not at all, to 7, all or nearly all the time). For the first three elements, ratings were uniformly 7; for role plays, the average rating was 6.2 (SD = 1.4). Raters had perfect agreement that all lessons were taught as intended.
School food changes
In our formative research, students said they preferred sliced (vs. whole) fruit [32, 36]. Cafeteria signage was small, often handwritten, and difficult to read, and nutritional information was not posted. We worked with LAUSD’s FSB to introduce sliced fruit to the cafeteria menu during every lunch period during the intervention, and to post point-of-sale cafeteria signage with nutritional information, posters with nutritional information, and posters explaining how to read nutritional information. Teachers disseminated handouts to all seventh graders (i.e., smaller versions of the two nutritional information posters). SNaX-related cafeteria changes and messages were publicized in a full-class period assembly for all seventh graders on the first day of the intervention.
Survey evaluation
Although all students in the school were exposed to cafeteria changes, seventh graders were targeted for intensive intervention activities and were therefore the focus of the survey evaluation. A total of 425 seventh graders in the intervention school (63% of 7th graders) were surveyed at baseline; of these, 399 (94%) were surveyed again one-month post-intervention. Intervention students who completed the baseline but not the follow-up survey (n=26, 6%) were not significantly different (p >.05) from those who completed both waves on the main outcomes (cafeteria attitudes; soda and sports/fruit drink consumption).
One-third (33%; n = 222) of intervention school parents refused to let their child participate. Because of the high refusal rate, we contacted 124 (56%) of these parents to determine reasons for refusal. We made parents aware that their child could have participated in some, none, or all SNaX activities, and that they could have for some components of the study but not others (e.g., for survey but not club participation). Choosing among response options, 47 parents (37%) reported that they had refused because their child had another activity during the club time, 17 (14%) that their child was not interested, and 2 that their child was not overweight/did not need the program; 1 had privacy concerns. Sixty said they would have provided consent for some components of the study, had they known about this option.
Survey content
Socio-demographic characteristics included student gender, age, race/ethnicity, and primary language spoken at home. Participants were asked to check all that apply using the categories: African American, Native American, Asian/Pacific Islander (i.e., Asian Indian, Chinese, Filipino, Japanese, Korean, Pacific Islander, Vietnamese, other Asian, other Pacific Islander), Latino/Hispanic (i.e., Mexican, Salvadoran, Guatemalan, other Latino), White, and other. Using a hierarchical algorithm, we assigned each participant to one category, prioritized as: Latino/Hispanic, African American, Native American, Asian/Pacific Islander, White, and all others; White, Native American, and “other” were collapsed [37]. Primary language was categorized as English vs. not English (assessed as Spanish, Tagalog, Vietnamese and other).
Cafeteria attitudes were measured with the stem, “I believe eating in the cafeteria is…” and three 7-point semantic differential scales (unsatisfying/satisfying; bad/good; unhealthy/healthy; midpoint = neither). Scale responses were averaged (α=.87).
Beverage consumption was measured with the stem, “Yesterday, which of the following did you drink?” and checkboxes for “soda” and “sports drinks or non-carbonated fruit drinks.” The day before the survey was always a school day (the survey was not given on Mondays or immediately after school holidays).
Peer advocacy was assessed by asking peer advocates to whom they spoke about healthy eating and SNaX, with response options friends, other students, parents, other family members, and teachers, and other. Non-peer advocates reported if a peer leader talked with them.
Cafeteria records
School cafeteria records were obtained from the intervention school and a comparison school with similar socio-demographic distributions (i.e., on race/ethnicity, English learners, physical fitness, and NSLP eligibility) located in the same geographic region of LAUSD. In both schools, 77% of students were NSLP-eligible. We obtained daily cafeteria records for the entire semester in which we conducted the intervention, allowing us to examine pre-intervention, intervention, and post-intervention cafeteria patterns for all students in the intervention and comparison schools. The records contain daily percentages of total students, NSLP-eligible students, and full-price students who obtained food, and per-item ordering and sales information. We created two summary measures of number of fruits and “healthier entrées” (i.e., NSLP entrees designed to be healthier with respect to calorie and fat content; included deli sandwiches, salads, and yogurt fruit parfaits) that were selected by students daily (measured per student eating in the cafeteria each day). We examined fruit because the introduction of sliced fruit was a major SNaX component. We examined healthier entrées because our formative work revealed that they were available in both schools but not listed on cafeteria menus or signs prior to the intervention, and students were generally unaware that they were available. Because we tested SNaX in one intervention and one comparison school and did not randomly assign schools to condition, we cannot examine causality in this pilot investigation. However, we were able to obtain preliminary data on within-school changes from baseline, as well as to compare these changes between the schools.
Statistical Analysis
Survey data
Analyses were restricted to the 399 students who responded to baseline and follow-up surveys. We expected that the weaker intervention dose given to non-advocates (versus peer advocates) would translate into weaker effects, and any seasonal trends in eating behaviors over the course of the semester would be more apparent among non-advocates. Thus, we conducted separate, parallel analyses for peer advocates and non-peer advocates, using paired t-tests to examine pre-post differences in the linear outcome (cafeteria attitudes), and exact McNemar tests to examine dichotomous beverage outcomes (i.e., whether students’ drinking of soda and sports/fruit drinks changed from baseline to follow-up). We conducted multivariate regressions to compare pre-to-post changes among peer advocates to parallel changes among non-peer advocates (a “difference-of-differences” test). These regressions predicted each outcome at follow-up using baseline outcome value, an indicator for whether the student was an advocate, and student socio-demographic characteristics. Linear regression was used for cafeteria attitudes, and logistic regression for beverage outcomes.
Follow-up survey values were substituted for missing baseline values of gender (2%), primary language (5%), and birth-date (2%). Mean values were used in four cases when values were missing at both baseline and follow-up.
Cafeteria data
We obtained cafeteria records containing the number of students visiting the cafeteria each day, and the number who selected fruit and healthier entrées before, during, and after the intervention in the intervention and comparison schools. Assuming a maximum of one serving per student per day (as suggested by Food Services Branch staff), we used multivariate logistic regression to predict whether a student selected fruit, among students who attended the cafeteria on that day, using an intervention school indicator, two intervention period indicators (during and after, versus before), and intervention school by period interactions. Among students visiting the cafeteria, this model tested whether intervention school students were more likely to select fruit each day during and after the intervention period absolutely, and relative to corresponding changes among comparison school students (i.e., the difference between pre-to-post change within the intervention school and pre-to-post change within the comparison school). Parallel multivariate models were conducted for cafeteria data for healthier entrées among students visiting the cafeteria.
Results
Student Socio-Demographics
Of the 399 seventh graders who completed baseline and follow-up surveys, half were female; the average age was 13 years (SD = 0.5). The majority (68%) were Latino; 17% were Asian/Pacific Islander, 11% were Black/African American, 2% were White, 1% was Native American, and 1% was “other”; 65% primarily spoke English at home.
Peer Advocacy Activities
Nearly all peer advocates (96%) talked to at least one other person about SNaX and healthy eating. Half talked to at least 3 different categories of people: most (85%) talked to friends, 70% to other students, 66% to parents, 48% to other family members, 25% to teachers, and 15% to another type of individual. Nearly half (48%) of non-peer advocates reported speaking with a SNaX peer leader.
Self-reported Cafeteria Attitudes and Behavior
As shown in Table 1, significant effects emerged for cafeteria attitudes and sports/fruit drink consumption. Cafeteria attitudes significantly improved over time among peer advocates (pre: M = 3.52, SD = 1.78; post: M = 4.07, SD = 1.68, p = .003) but remained stable for non-peer advocates (pre: M = 3.45, SD = 1.60; post: M = 3.37, SD = 1.60, p = .34). The difference-of-differences test indicated that the improvement in cafeteria attitudes among peer advocates (~one-third of a standard deviation) was significantly greater than the pre-post change for non-peer advocates, b = 0.71, p <.001.
Table 1.
Bivariate and Multivariate Tests Examining Pre-Post Differences in Average Cafeteria Attitudes, and Percentage who Drank Soda and Sports/Fruit Drinks the Day before the Survey, among Peer Advocates and Non-Peer Advocates.
| Peer Advocates | Non-Peer Advocates | Peer advocate change minus non-peer advocate change 3 | |||||
|---|---|---|---|---|---|---|---|
| Pre- Intervention | Post- Intervention | n | Pre- Intervention | Post- Intervention | n | b | |
| Cafeteria Attitudes, M(SD)1 | 3.52 (1.78) | 4.07 (1.68)** | 107 | 3.45 (1.60) | 3.37 (1.60) | 283 | 0.71*** |
| Soda, %2 | 36.1 | 35.2 | 108 | 37.2 | 43.9† | 285 | −0.38 |
| Sports/Fruit Drinks, %2 | 33.3 | 21.3* | 108 | 32.6 | 26.0† | 285 | −0.19 |
p <.10
p<.05
p<.01
p<.001
Note: All tests restrict to students with non-missing values for the response at both waves.
For continuous outcomes (cafeteria attitudes), paired t-tests were used to test for within-group change, and multivariate linear regressions were used to test for different magnitudes of within-group change across groups.
For dichotomous outcomes (drank soda, sports/fruit drinks), McNemar’s tests were used to test for within-group change, and multivariate logistic regressions were used to test for different magnitudes of within-group change across groups.
Multivariate regressions controlled for baseline outcome, gender, age, race/ethnicity, and primary language spoken at home.
Intervention school students reduced their intake of two types of SSBs, sports and fruit drinks. Before the intervention, a third of students in both groups (i.e., advocates and non-advocates) consumed sports and fruit drinks; after the intervention, 21% of peer advocates, and 26% of non-advocates, drank those SSBs. This decrease was significant for peer advocates (p = .03) and nearly significant for non-peer advocates (p = .06). The difference-of-differences test did not show significant differences between the groups (p = .50).
Changes in Students’ Selection of Cafeteria Foods
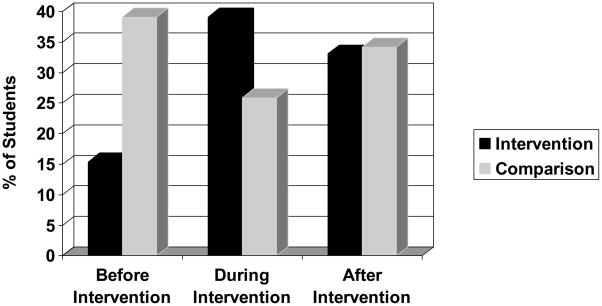
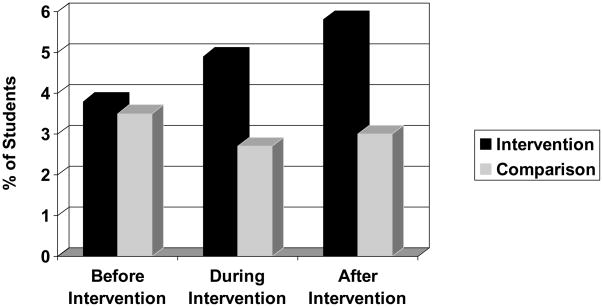
Figures 1 and 2 show percentages of fruits and healthier entrées selected per student visiting the cafeteria each day before, during, and after the intervention period, among students in attendance. Table 2 shows the results of logistic regressions that tested changes within the intervention and comparison schools, and differences between schools in the change in percentages of students who selected fruit or healthier entrées pre-intervention, to during or after the intervention period.
Figure 1.
Percentages of Students Who Selected Fruit in Cafeteria. Data represent servings per student per day, among those visiting the cafeteria.
Figure 2.
Percentages of Students Who Selected Healthy Entrées in Cafeteria. Data represent servings per student per day, among those visiting the cafeteria.
Table 2.
Changes in Percentages of Students Served Fruits and Healthy Entrées (i.e., salads, sandwiches, yogurt parfaits) in Cafeteria.
| Before Intervention (%) | Change During Intervention1 (%) | Change After Intervention1 (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Cafeteria Servings2 | Intervention | Comparison3 | Intervention | Comparison | Intervention- Comparison Difference | Intervention | Comparison | Intervention- Comparison Difference |
| (40 days) | (48 days) | (26 days) | (26 days) | (30 days) | (26 days) | |||
| Fruits | 15.4 | 39.1 | 23.7*** | −13.2*** | 36.9*** | 17.6*** | −4.9*** | 22.5*** |
| Healthy Entrées | 3.8 | 3.5 | 1.1*** | −0.8** | 1.9*** | 1.9*** | −0.5 | 2.4*** |
p <.01
p <.001
Relative to before intervention
Servings per student per day, among those visiting the cafeteria, i.e., percentage of students who took fruit or healthy entrées, among number of students visiting cafeteria each day (Interpretation of percentages are based on the assumption that students can only obtain one fruit serving and one healthy entrée item per day.)
Due to differences in the intervention and comparison school spring semester calendars, pre-intervention time periods varied between schools.
Difference scores indicated significant intervention condition by period interactions (i.e., the intervention school change differed significantly from the comparison school change). Fruit servings significantly decreased in the comparison school and significantly increased in the intervention school. The magnitude of the intervention school’s changes significantly differed from the comparison school’s parallel changes from baseline to during the intervention (p <.001), and from baseline to post-intervention (p <.001). In the comparison school, 39% of students visiting the cafeteria took fruit before the intervention period, 26% took fruit during the intervention period, and 34% took fruit after the intervention period. In the intervention school, 15% of students took fruit before the intervention period, 39% took fruit during the intervention period, and 33% took fruit after the intervention period (for both comparison and intervention schools, p <.001 for within-school changes from baseline to during the intervention, and baseline to post-intervention). Thus, baseline values of fruit selections were much higher in the comparison school than the intervention school; both schools showed similar post-intervention percentages.
For healthier entrées, the magnitude of changes over time for the intervention school differed significantly from changes for the comparison school from baseline to during the intervention, and from baseline to post-intervention (p <.001 for each period). In the comparison school, 4% of students visiting the cafeteria were served a healthy entrée before the intervention period, versus 3% both during and after the intervention period (p = .003 and p = .08 vs. pre-intervention, respectively). In the intervention school, 4% of students visiting the cafeteria school were served a healthy entrée before the intervention period, versus 5% during the intervention period and 6% after the intervention period (p <.001 for each period vs. pre-intervention).
Discussion
In a pilot school-based obesity-prevention intervention designed through a community-academic partnership, seventh graders receiving a higher dose of the intervention (as peer advocates) had positive changes in attitudes regarding the cafeteria and lower rates of SSB consumption post-intervention. Seventh graders who were not peer advocates showed slight decreases in positive attitudes and trends for more soda consumption at follow-up. Although we cannot make conclusions about causality from this small non-randomized pilot, results suggest that interventions should actively involve all students in advocacy, even for brief periods: Partners of peer leaders participated for less than half an hour (during lunch), and each peer leader participated in only one club and one lunchtime session (~2 hours total).
Although the intervention was most intensively delivered to seventh graders, school-wide cafeteria records showed significant changes in fruit and healthier entrée selections in the intervention school. Intervention school changes were larger than likely explained by changes only in the 21% of seventh graders who were peer advocates (7% of all students in cafeteria data). Cafeteria changes persisted after the intervention (for an additional month), indicating that cafeteria staff continued to prepare (and students continued to take) additional selections, even though they were no longer being supported by SNaX resources. When conducting follow-up school visits, we found that cafeteria staff sustained the sliced fruit and signage during the next school year. These findings are consistent with research showing increased fruit and vegetable consumption after improved marketing and/or greater availability of fruits and vegetables at school [38, 39], and increased cafeteria servings of healthier options following student-led promotions [9, 40].
Results suggest that schools should not only work to improve the quality and nutritional value of foods offered as part of the NSLP, but also to use marketing to increase the foods’ appeal. Since the described intervention test was completed, LAUSD has taken steps to improve marketing by gathering data on student preferences, conducting taste tests, and advertising new entrées. Starting in the 2008–2009 school year, in part due to our results, LAUSD cafeterias offered sliced fruits and vegetables.
We cannot draw conclusions about intervention effects because we did not randomly select a control school in which to measure survey outcomes; nor did we randomly choose the comparison school. Further, cafeteria data showed large differences between the intervention and comparison schools at baseline and thus any differences in cafeteria outcomes may be attributable to variability between the schools rather than the intervention. The mismatch in baseline values may be partially attributable to differences in cafeteria staffing. Prior to the intervention, the intervention school cafeteria lost several staff members and was under-staffed, leading to long student waiting times, lower food quality, and consequent lower participation in the school meal program. In contrast, the comparison school had more adequate staffing. Other limitations include the general lack of diversity in the sample (which was largely Latino); the lack of validity information for the survey measures, which were created for this pilot; and the inability to link student survey data with aggregate cafeteria data, which would have allowed us to examine cafeteria effects by peer advocate involvement and NSLP eligibility.
In terms of community relationships and capacity-building, our research went beyond our seventh grade participants to include other students at the school and throughout the district. Seventh graders gained leadership skills for educating peers, cafeteria staff continued to post signage and slice fruit, and LAUSD adopted a policy of offering sliced fruit. Our research experiences demonstrate how CBPR can help to develop programs that are based on community needs and priorities identified by community members.
Acknowledgments
This research was supported by R24 MD001648 from the National Center on Minority Health and Health Disparities (NCMHD) of the National Institutes of Health. We would like to acknowledge the contributions of the following individuals: Burton Cowgill, Elizabeth D’Amico, Ying-Ying Goh, Ritamarie Knizewski, Bessie Ko Sipple-Asher, Josefina Olarita-Dhungana, Andrew Parker, Anisha Patel, and Karen Chan Osilla.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Institute of Medicine. Nutrition standards for foods in schools: leading the way toward healthier youth. Washington, D.C: National Academy of Sciences; 2007. [Google Scholar]
- 2.Institute of Medicine. School meals: building blocks for healthy children. Washington, D.C: National Academy of Sciences; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Schools can play a role in childhood obesity prevention. Washington, D.C: National Academy of Sciences; 2005. [Google Scholar]
- 4.Gordon-Larsen P, McMurray RG, Popkin BM. Determinants of adolescent physical activity and inactivity patterns. Pediatrics. 2000 Jun;105(6):E83. doi: 10.1542/peds.105.6.e83. [DOI] [PubMed] [Google Scholar]
- 5.Birnbaum AS, Lytle LA, Story M, et al. Are differences in exposure to a multicomponent school-based intervention associated with varying dietary outcomes in adolescents? Health Educ Behav. 2002;29(4):427–443. doi: 10.1177/109019810202900404. [DOI] [PubMed] [Google Scholar]
- 6.Lytle LA, Murray DM, Perry CL, et al. School-based approaches to affect adolescents’ diets: results from the TEENS study. Health Educ Behav. 2004 Apr;31(2):270–287. doi: 10.1177/1090198103260635. [DOI] [PubMed] [Google Scholar]
- 7.French SA, Story M, Fulkerson JA, et al. An environmental intervention to promote lower-fat food choices in secondary schools: outcomes of the TACOS Study. Am J Public Health. 2004 Sep;94(9):1507–1512. doi: 10.2105/ajph.94.9.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallis JF, McKenzie TL, Conway TL, et al. Environmental interventions for eating and physical activity: a randomized controlled trial in middle schools. Am J Prev Med. 2003 Apr;24(3):209–217. doi: 10.1016/s0749-3797(02)00646-3. [DOI] [PubMed] [Google Scholar]
- 9.Thompson V, Cullen KW, Watson KB, et al. The increased availability and marketing of fruit, juice, and vegetables to middle school students increases consumption. J Child Nutr Manag. 2007;31(1) [Google Scholar]
- 10.Israel BA, Eng E, Schulz AJ, et al. Methods in community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- 11.Bogart LM, Uyeda K. Community-based participatory research: partnering with communities for effective and sustainable behavioral health interventions. Health Psychol. 2009 Jul;28(4):391–393. doi: 10.1037/a0016387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uyeda KE, Bogart LM, Hawes-Dawson J, et al. Development and implementation of a school-based obesity prevention intervention: Lessons learned from community-based participatory research. Prog Community Health Partnersh. 2009;3(3):249–255. doi: 10.1353/cpr.0.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simons-Morton B, Haynie DL, Crump AD, et al. Peer and parent influences on smoking and drinking among early adolescents. Health Educ Behav. 2001;28(1):95–107. doi: 10.1177/109019810102800109. [DOI] [PubMed] [Google Scholar]
- 14.Mellanby A, Rees J, Tripp J. Peer-led and adult-led school health education: a critical review of available comparative research. Health Educ Res. 2000;15(5):533–545. doi: 10.1093/her/15.5.533. [DOI] [PubMed] [Google Scholar]
- 15.Kinsman S, Romer D, Furstenberg F, et al. Early sexual initiation: the role of peer norms. Pediatrics. 1998;102(5):1185–1192. doi: 10.1542/peds.102.5.1185. [DOI] [PubMed] [Google Scholar]
- 16.Campbell R, Starkey F, Holliday J, et al. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet. 2008;371:1595–1602. doi: 10.1016/S0140-6736(08)60692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valente T, Hoffman B, Ritt-Olson A, et al. Effects of a social-network method for group assignment strategies on peer-led tobacco prevention programs in schools. Am J Public Health. 2003;93(11):1837–1843. doi: 10.2105/ajph.93.11.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fishbein M. A reasoned action approach to health promotion. Med Decis Making. 2008;28(6):834–844. doi: 10.1177/0272989X08326092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cullen KW, Baranowski T, Rittenberry L, et al. Child-reported family and peer influences on fruit, juice and vegetable consumption: reliability and validity of measures. Health Educ Res. 2001;16(2):187–200. doi: 10.1093/her/16.2.187. [DOI] [PubMed] [Google Scholar]
- 20.Kassem NO, Lee JW. Understanding soft drink consumption among male adolescents using the theory of planned behavior. J Behav Med. 2004;27(3):273–296. doi: 10.1023/b:jobm.0000028499.29501.8f. [DOI] [PubMed] [Google Scholar]
- 21.Barr-Anderson DJ, Young DR, Sallis JF, et al. Structured physical activity and psychosocial correlates in middle-school girls. Prev Med. 2007;44(5):404–409. doi: 10.1016/j.ypmed.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 22.Saunders RP, Motl RW, Dowda M, et al. Comparison of social variables for understanding physical activity in adolescent girls. Am J Health Behav. 2004;28(5):426–436. doi: 10.5993/ajhb.28.5.5. [DOI] [PubMed] [Google Scholar]
- 23.Pearlman DN, Dowling E, Bayuk C, et al. From concept to practice: using the School Health Index to create healthy school environments in Rhode Island elementary schools. Prev Chronic Dis. 2005 Nov;2(Spec no:A09) [PMC free article] [PubMed] [Google Scholar]
- 24.Los Angeles Unified School District. Healthy beverage motion. 2004 [cited June 28, 2007]; Available from: http://cafe-la.lausd.k12.ca.us/healthy.htm.
- 25.Los Angeles Unified School District. Snack foods and school board obesity prevention motion. 2004 [cited June 28, 2007]; Available from: http://cafe-la.lausd.k12.ca.us/snacks.htm.
- 26.Los Angeles Unified School District. Cafeteria improvement motion. 2005 [cited June 28, 2007]; Available from: http://cafe-la.lausd.k12.ca.us/motion.htm.
- 27.Fowke JH, Schlundt D, Gong Y, et al. Impact of season of food frequency questionnaire administration on dietary reporting. Ann Epidemiol. 2004;14(10):778–785. doi: 10.1016/j.annepidem.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Givens ML, Lu C, Bartell SM, et al. Estimating dietary consumption patterns among children: A comparison between cross-sectional and longitudinal study designs. Environ Res. 2007;103(3):325–330. doi: 10.1016/j.envres.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Shahar DR, Froom P, Harari G, et al. Changes in dietary intake account for seasonal changes in cardiovascular disease risk factors. Eur J Clin Nutr. 1999;53(3):395–400. doi: 10.1038/sj.ejcn.1600761. [DOI] [PubMed] [Google Scholar]
- 30.Shahar DR, Yerushalmi N, Lubin F, et al. Seasonal variations in dietary intake affect the consistency of dietary assessment. Eur J Epidemiol. 2001;17(2):129–133. doi: 10.1023/a:1017542928978. [DOI] [PubMed] [Google Scholar]
- 31.Patel AI, Bogart LM, Uyeda KE, et al. Site visits as a tool for community based participatory research. Am J Prev Med. doi: 10.1016/j.amepre.2009.08.009. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goh YY, Bogart LM, Sipple-Asher BK, et al. Using community-based participatory research to identify potential interventions to overcome barriers to adolescents’ healthy eating and physical activity. J Behav Med. 2009 Oct;32(5):491–502. doi: 10.1007/s10865-009-9220-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rogers EM. Diffusion of Innovations. 5. New York, NY: Free Press; 2003. [Google Scholar]
- 34.Kelly JA, Stevenson LY. Opinion leader HIV prevention training manual. Milwaukee, WI: Center for AIDS Intervention Research, Medical College of Wisconsin; 1995. [Google Scholar]
- 35.Miller WR, Rollnick S. Motivational interviewing: preparing people for change. 2. New York, NY: Guilford Press; 2002. [Google Scholar]
- 36.Patel AI, Bogart LM, Uyeda KE, et al. School site visits for community-based participatory research on healthy eating. Am J Prev Med. 2009;37(6S1):S300–306. doi: 10.1016/j.amepre.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mays VM, Ponce NA, Washington DL, et al. Classification of race and ethnicity: implications for public health. Ann Rev Public Health. 2003;24:83–110. doi: 10.1146/annurev.publhealth.24.100901.140927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baranowski T, Davis M, Resnicow K, et al. Gimme 5 fruit, juice, and vegetables for fun and health: outcome evaluation. Health Educ Behav. 2000;27(1):96–111. doi: 10.1177/109019810002700109. [DOI] [PubMed] [Google Scholar]
- 39.Davis M, Baranowski T, Resnicow K, et al. Gimme 5 fruit and vegetables for fun and health: process evaluation. Health Educ Behav 2000. 2000 April 1;27(2):167–176. doi: 10.1177/109019810002700203. [DOI] [PubMed] [Google Scholar]
- 40.French SA, Story M, Fulkerson JA, et al. An environmental intervention to promote lower-fat food choices in secondary schools: outcomes of the TACOS Study. Am J Public Health. 2004 Sep;94(9):1507–1512. doi: 10.2105/ajph.94.9.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]