Abstract
Purpose
Infection with human immunodeficiency virus (HIV) remains a major global threat, and although the prevalence is comparatively still very low, the number of HIV-positive Koreans is increasing. However, there are no official guidelines as to how to treat people living with HIV/acquired immunodeficiency syndrome (AIDS) (PLWHA) or how to screen for potentially infectious people. This study assessed the level of knowledge and attitudes of dentists in Korea toward PLWHA, and their attitudes to screening patients for HIV infections.
Methods
A cross-sectional prospective survey targeting dentists working in Korea was conducted using a self-administered questionnaire.
Results
A satisfactory level of knowledge about HIV/AIDS and a relatively positive attitude toward PLWHA was found. Most of the respondents preferred rapid HIV testing using oral fluid as a specimen. The general attitude of dentists toward HIV/AIDS is sufficiently positive to enable provision of the best treatment to the patients in need.
Conclusions
Most of the dentists require HIV testing in dental clinics. In spite of their needs, there are several obstacles. It is hoped that financial considerations and official legal requirements related to HIV testing strategies will be considered.
Keywords: Acquired immunodeficiency syndrome, AIDS-related opportunistic infections, Data collection, HIV long-term survivors, HIV
INTRODUCTION
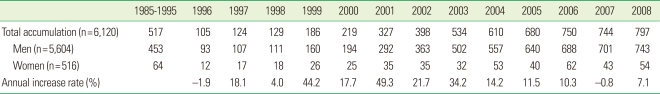
Since important progress has been made in preventing new human immunodeficiency virus (HIV) infections, the annual number of acquired immunodeficiency syndrome (AIDS)-related deaths has been decreased, and the number of people living with HIV continues to increase. Worldwide, more than 6,800 people become infected with HIV every day and more than 5,700 individuals die from AIDS [1]. Since the first case report of HIV infection in 1985 [2], the number of accumulated infected patients in the Republic of Korea is 6,120 as of December 2008 [3], of which 1,084 of the patients have died. Compared to western countries and sub-Saharan Africa, HIV prevalence is comparatively low, but the epidemic is steadily expanding from specific populations such as injecting drug users, sex workers, and homosexual men into lower risk populations by transmission to the sexual partners of those most at risk [4]. The important issue is that the number of newly reported HIV infection cases are increasing every year with a changing epidemic pattern (Table 1), but dental care workers are unprepared to treat this increasing number of people living with HIV/AIDS (PLWHA) [5].
Table 1.
Reported number of people newly infected with human immunodeficiency virus.
In Korea, as in many other countries, people with HIV frequently encounter discrimination in everyday life as well as when seeking and receiving health care services. Forty percent of the general public reported that "They would not sit together at the same table" and 48.5% reported that "PLWHA should be isolated from non-infected people" [6,7]. Even 78.9% of healthcare workers answered "PLWHA have lifestyles that are morally wrong" and 67.7% answered that "PLWHA should be isolated" [8,9]. The knowledge and attitudes of healthcare workers in relation to HIV infection is an important factor influencing the willingness and ability of people with HIV to access medical care and the quality of the care they receive. There have been several studies conducted evaluating dental workers' knowledge about AIDS and their attitudes towards HIV-infected patients [10-17].
The Centers for Disease Control in the United States introduced the concept of universal precautions for dental infection control protocols to decrease fears and remove barriers to care in 1993 [18]. In Japan, the 1996 protocol for education on infection control for HIV-related patients recommends that dental care workers assume that all patients are potentially infectious [19]. However, there have been no official guidelines regarding how to care for PLWHA in the dental clinic and, surprisingly, research on HIV or AIDS from the dentistry perspective is almost nonexistent in Korea.
The subject of this study is the evaluation of the knowledge and attitudes of Korean dentists towards HIV and the compilation of their opinions on HIV/AIDS policy.
MATERIALS AND METHODS
Data collection was done with the use of a standardized self-administered questionnaire, which covered demography, knowledge of HIV transmission, occupational vulnerability, infection control, and opinions on HIV/AIDS policy. Five hundred survey questionnaires were sent out at around the same time to limit a bias due to changes over time and mailed only to dentists belonging to the Korean Dental Association. In total, 475 replies were received and the data were analyzed anonymously.
RESULTS
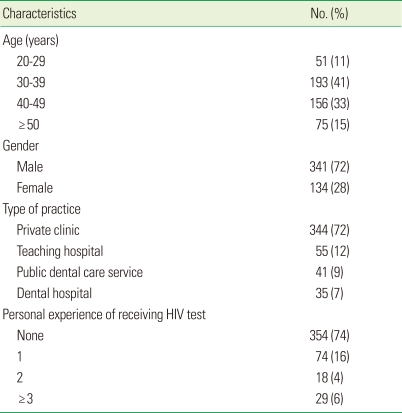
As shown in Table 2, a total of 475 Korean dentists took part in the study, and 74% of respondents were between the ages of 30 and 50 years. The study population consisted of 341 males (72%) and 134 females (28%). As for the type of practice, a majority of the dentists (72%) were running private clinics, followed by teaching hospitals (12%).
Table 2.
Demographic characteristics of the respondents (n=475).
HIV: human immunodeficiency virus.
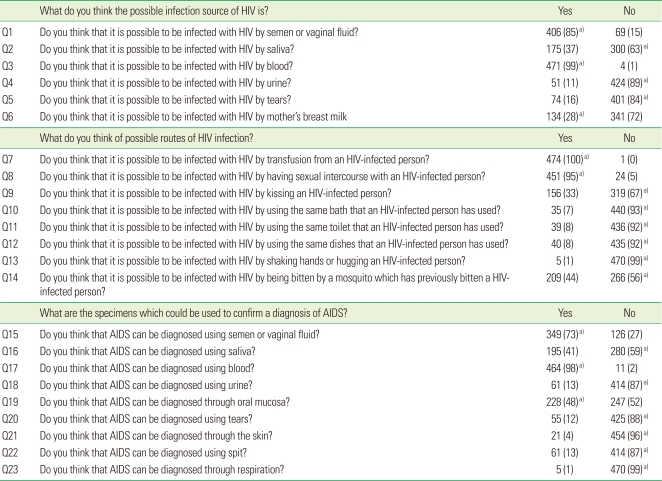
Knowledge of HIV transmission
The dentists were asked to answer true or false to 23 statements regarding possible routes of HIV transmission (Table 3). Correct responses were scored as one and incorrect responses as zero. An overall knowledge score was calculated by summing the scores for each statement, and the highest possible score was 23. The average was 18.78±2.46. Many dentists mistakenly believed that HIV could not be transmitted by mother's breast milk and was not aware of the fact that HIV detection was possible from oral mucosa.
Table 3.
Response scores to questions concerning HIV/AIDS (n=475).
Values are presented as number (%).
HIV: human immunodeficiency virus, AIDS: acquired immunodeficiency syndrome.
a)Correct answers.
Attitudes towards HIV/AIDS
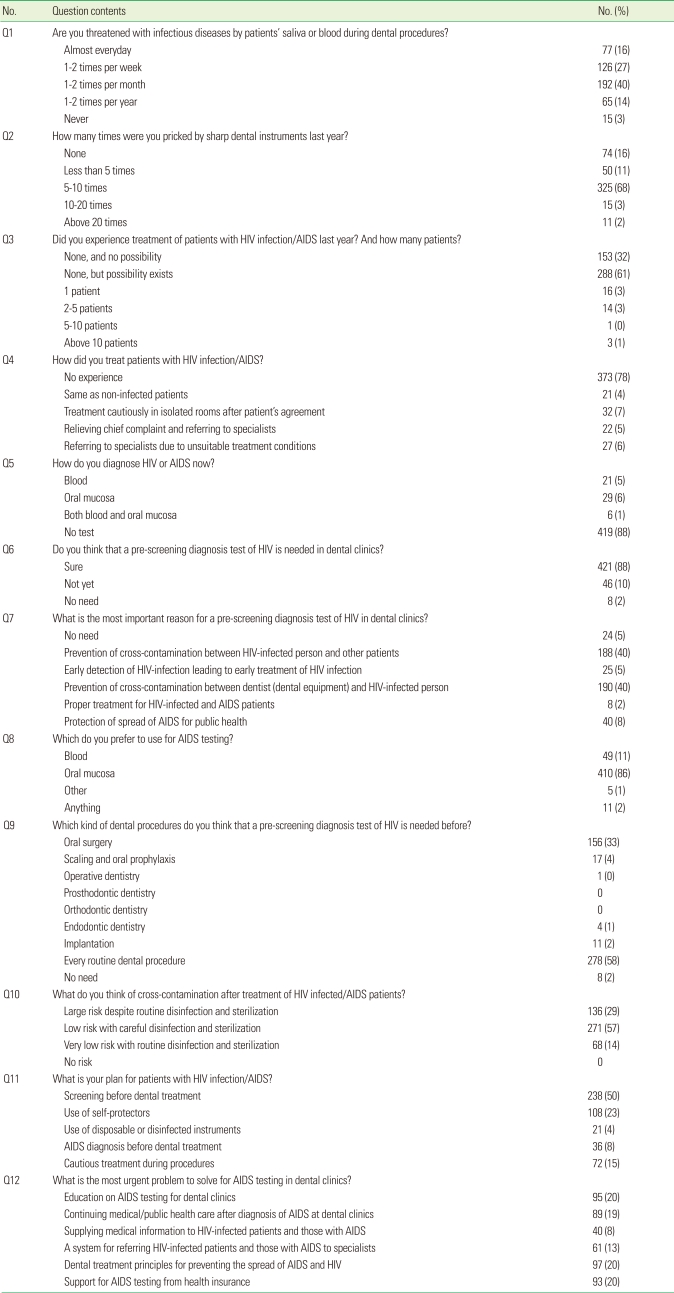
As shown in Table 4, a majority of respondents (93%) answered that they had not treated an HIV-infected person within the past year, but 61% were not sure about the infection state of the patients. Of the dentists who have experienced treating an HIV-infected person, treatment plans were equally distributed over various options, such as referring to specialists, relieving only chief complaints, and treating just like a non-infected person.
Table 4.
Fear and attitudes towards HIV/AIDS (n=475).
HIV: human immunodeficiency virus, AIDS: acquired immunodeficiency syndrome.
While 88% answered they do not test their patients for HIV infection, 89% of respondents thought HIV testing was necessary in the dental clinic and 80% stated that the reason for needing HIV testing in the dental clinic was to prevent cross contamination among patients and between patients and dental care workers. Pricking with sharp instruments after usage with HIV-infected and AIDS patients is one of the sources of HIV infection [8]. Eighty-four percent of respondents answered they were pricked by sharp instruments at least once a year. As for the type of HIV test, 86% preferred non-invasive tests using oral fluid specimens collected by swabbing the outer surface of the upper and lower gums. Slightly more than half of the dentists (59%) answered that HIV testing should be performed before every routine dental procedure and 33% answered that only oral surgeries required HIV testing before operation.
DISCUSSION
HIV and AIDS are widely spread infectious diseases and the number of people living with HIV worldwide has continued to increase, reaching an estimated 33.4 million. Compared to 1990, the total number of people living with the virus in 2008 was approximately threefold higher [4]. Due to the advancement of medical treatment, acute and fatal HIV infection has been transformed into a chronic disease which requires management and monitoring. Consequently, there are more chances for dental care workers to meet PLWHA in clinics, and the workers should be prepared with knowledge and the appropriate attitude.
The results of this study showed that the average level of knowledge was high, reflecting a correct understanding of the mechanisms of HIV infection. However, some of the respondents did not know that saliva cannot transmit the virus. Dental care workers who deal daily with patients' saliva tend to be unwilling to treat PLWHA when they do not know that the viral load in saliva is so low that it cannot transmit the HIV virus. Therefore, it is important for dental care workers to be well equipped with up-to-date information, treatment strategies, and knowledge of resources available.
It is generally accepted that attitudes are affected by the level of knowledge. Most of the studies on HIV/AIDS have investigated attitudes in combination with the level of knowledge, and have concluded that more and continuous education is required to change negative attitudes towards PLWHA. However, Mitchell [20] reported that knowledge alone does not seem to change the attitude of most health care professionals, as some of them still experienced difficulty in establishing good relationship with AIDS patients. The study also showed that the level of knowledge was high enough for the dentists to continue proper infection control and care for PLWHA. However, the respondents answered that they avoid active treatment or seek referrals as much as they treat like healthy people. The motivation to care for the possibly infected person does not seem to come from a high level of knowledge, and solutions should seek to change the attitude of dentists and to encourage the proper and the best treatment for PLWHA.
HIV testing prior to dental treatment and knowledge about patients' infection state can reassure dentists and allow them to confidently do their jobs. Up to now, several types of HIV testing have been developed that use whole blood or an oral fluid specimen. One of the latest types of testing is OraQuick Advance, which detects antibodies to HIV-1 and HIV-2 in oral fluid. The manufacturer indicates a specificity of 99.8% with oral fluid and 100% with whole blood. In this report, 86% of respondents answered they preferred using this product for its non-invasive method of application. Also, 89% of respondents said they believe that HIV testing is necessary in the dental clinic, even though 88% were not currently testing their patients for HIV infection. This reveals a major contradiction between the ideal and reality, and it seems that there are certain obstacles to initiating patient HIV infection testing in dental clinics.
First, it should be determined that who will pay for the test. The HIV and AIDS prevalence is low in Korea relative to other countries and public attention regarding infection has not been widely aroused. Therefore, a prudent policy should be developed regarding costs in order to prevent a misunderstanding that dentists benefit much more than patients from this test, since the possibility of the cross infection from patient to dentist is greater than the possibility of the cross infection from patient to patient. Covering the costs of testing using national insurance would ensure that dentists could routinely test their patients and detect undiagnosed HIV-infected people. Second, getting consent from patients to test for HIV infection before dental treatment can cause unexpected problems in clinics. Negative perception of HIV/AIDS is dominant among Korean people and asking for consent for HIV testing can be taken as a humiliating question. Also, most people do not understand why HIV testing is performed at dental clinics. The perceived value of HIV testing by patients appears to be quite low due to the belief that HIV infection is rare. Therefore, general education for the public should be combined with systematic support to provide HIV testing in dental clinics.
Recent advances in HIV medical management have transformed HIV infection from a fatal and terminal disease into a chronic illness requiring continued management and careful monitoring. However, dentists and dental care workers' general perception is still negative despite a high level of knowledge. Routine HIV testing in dental clinics would help dentists to change negative attitudes towards PLWHA and provide the best treatment when financial and systematic support is provided from the government.
ACKNOWLEDGEMENTS
This study was supported by a grant for Health Promotion against HIV/AIDS & STD (4800-4842-302-260) from the Korea Centers for Disease Control and Prevention.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.UNAIDS; World Health Organization. AIDS epidemic update: December 2007. Geneva: UNAIDS; 2007. [Google Scholar]
- 2.Lee SY. The change of route of HIV transmission for the past 11 years in Korea and the projection of the HIV/AIDS cases to the year 2000. Korean J Prev Med. 1996;29:331–346. [Google Scholar]
- 3.Korea Centers for Disease Control and Prevention. Report on the Korean HIV/AIDS epidemic 2008. Seoul: Korea Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 4.UNAIDS. UNAIDS report on the global HIV/AIDS epidemic 2009. Geneva: UNAIDS; 2009. [Google Scholar]
- 5.Bishop GD, Oh HM, Swee HY. Attitudes and beliefs of Singapore health care professionals concerning HIV/AIDS. Singapore Med J. 2000;41:55–63. [PubMed] [Google Scholar]
- 6.Kwoen KW, Lee KM, Byeon JO. A study on discrimination of people living with HIV/AIDS (PLWHAs) in Korea. Health Soc Sci. 2002;12:199–218. [Google Scholar]
- 7.Park SH, Lim DO, Lee BK, Han JH. Study on the attitudes toward condoms and STDs/AIDS in male college students. J Reprod Med Popul. 2002;15:46–55. [Google Scholar]
- 8.Han YR, Lee KO. A Study on knowledge and attitude of college nursing students to patient with HIV/AIDS. J Korea Community Health Nurs Acad Soc. 1998;12:201–220. [Google Scholar]
- 9.Park IH, Lee SJ, Lee JH. A study of assessing educational needs on program planning for AIDS (acquired immunodeficiency syndrome) inservice education for clinical nurses. J Korean Acad Nurs. 1999;29:371–382. [Google Scholar]
- 10.Dove SB, Cottone JA. Knowledge and attitudes of Texas dentists concerning AIDS. Am J Dent. 1990;3:5–8. [PubMed] [Google Scholar]
- 11.Gerbert B. AIDS and infection control in dental practice: dentists' attitudes, knowledge, and behavior. J Am Dent Assoc. 1987;114:311–314. doi: 10.14219/jada.archive.1987.0078. [DOI] [PubMed] [Google Scholar]
- 12.Kunzel C, Sadowsky D. Comparing dentists' attitudes and knowledge concerning AIDS: differences and similarities by locale. J Am Dent Assoc. 1991;122:55–61. doi: 10.14219/jada.archive.1991.0091. [DOI] [PubMed] [Google Scholar]
- 13.McCartan BE, Samaranayake LP. Oral care of HIV infected patients: the knowledge and attitudes of Irish dentists. J Ir Dent Assoc. 1991;37:41–43. [PubMed] [Google Scholar]
- 14.Rankin KV, Jones DL, Rees TD. Attitudes of dental practitioners and dental students towards AIDS patients and infection control. Am J Dent. 1993;6:22–26. [PubMed] [Google Scholar]
- 15.Scheutz F. Dental care of HIV-infected patients: attitudes and behavior among Danish dentists. Community Dent Oral Epidemiol. 1989;17:117–119. doi: 10.1111/j.1600-0528.1989.tb00002.x. [DOI] [PubMed] [Google Scholar]
- 16.Verrusio AC, Neidle EA, Nash KD, Silverman S, Jr, Horowitz AM, Wagner KS. The dentist and infectious diseases: a national survey of attitudes and behavior. J Am Dent Assoc. 1989;118:553–562. doi: 10.14219/jada.archive.1989.0082. [DOI] [PubMed] [Google Scholar]
- 17.Wisborg T, Brattebö G. Norwegian dentists' knowledge, attitudes, and behavior concerning the HIV. Scand J Dent Res. 1989;97:446–450. doi: 10.1111/j.1600-0722.1989.tb01459.x. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Recommended infection-control practices for dentistry, 1993. MMWR Recomm Rep. 1993;42(RR-8):1–12. [PubMed] [Google Scholar]
- 19.Aizawa F, Yonemitsu M, Aizawa Y, Hanada N, Akada H. A survey on infection control practices, knowledge and attitudes toward AIDS/HIV among dental practitioners. Nippon Koshu Eisei Zasshi. 1996;43:364–373. [PubMed] [Google Scholar]
- 20.Mitchell B. Attitudes of nurses towards AIDS patients. [cited 2010 Sep 20];Aust Electron J Nurs Educ [Internet] 1999 Mar;4(2) Available from: http://www.scu.edu.au/schools/nhcp/aejne/archive/vol4-2/studentmitchvol4_2.htm. [Google Scholar]