Abstract
Chronic obstructive pulmonary disease (COPD) is a heterogeneous disease and responses to therapies are highly variable. The aim of this study was to identify the predictors of pulmonary function response to 3 months of treatment with salmeterol/fluticasone in patients with COPD. A total of 127 patients with stable COPD from the Korean Obstructive Lung Disease (KOLD) Cohort, which were prospectively recruited from June 2005 to September 2009, were analyzed retrospectively. The prediction models for the FEV1, FVC and IC/TLC changes after 3 months of treatment with salmeterol/fluticasone were constructed by using multiple, stepwise, linear regression analysis. The prediction model for the FEV1 change after 3 months of treatment included wheezing history, pre-bronchodilator FEV1, post-bronchodilator FEV1 change and emphysema extent on CT (R = 0.578). The prediction models for the FVC change after 3 months of treatment included pre-bronchodilator FVC, post-bronchodilator FVC change (R = 0.533), and those of IC/ TLC change after 3 months of treatment did pre-bronchodilator IC/TLC and post-bronchodilator FEV1 change (R = 0.401). Wheezing history, pre-bronchodilator pulmonary function, bronchodilator responsiveness, and emphysema extent may be used for predicting the pulmonary function response to 3 months of treatment with salmeterol/fluticasone in patients with COPD.
Keywords: Pulmonary Disease, Chronic Obstructive; Emphysema; Corticosteroids; Adrenergic beta-Agonists; Respiratory Function Tests
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is usually progressive and is associated with an abnormal inflammatory response of the lung to noxious particles or gases (1). Previous studies have shown that regular treatment of COPD with an inhaled corticosteroid (ICS) improve pulmonary function and reduces the frequency of exacerbations, even though it does not modify the long-term decline of forced expiratory volume in 1 sec (FEV1) (2, 3). Combination therapy with an ICS and a long acting β2-agonist (LABA) is better in improving lung function and health status, and reducing daily symptoms and exacerbations than single therapy (4, 5).
COPD is a heterogeneous disease in terms of clinical, physiological, and pathological presentation. The chronic airflow limitation associated with COPD is caused by a variable contribution of small airway disease (obstructive bronchiolitis) and parenchymal destruction (emphysema). Thus, the therapeutic response to combination treatment with an ICS and a LABA is also variable. Previous COPD guidelines recommended the use of short-term (two weeks) oral corticosteroid therapy to identify COPD patients who might benefit from long-term treatment with an ICS (6). However, it was recently shown that the response to a short-term oral corticosteroid is a poor predictor of the longterm response to an ICS (7). Currently, there are no known good predictors of the responsiveness of COPD patients to treatment with an ICS and a LABA.
The aim of this study was to identify predictors of pulmonary function response to 3 months of treatment with salmeterol/fluticasone in patients with COPD.
MATERIALS AND METHODS
Patients
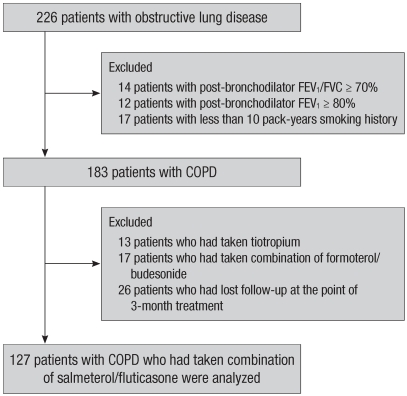
A total of 127 stable COPD patients who had been treated with salmeterol/fluticasone for 3 months were analyzed retrospectively. All patients were selected from the Korean Obstructive Lung Disease (KOLD) Cohort, which had 226 stable patients with obstructive lung disease (OLD) were prospectively recruited from the pulmonary clinics of 11 hospitals in Korea from June 2005 to September 2009 (Fig. 1). The inclusion criteria for the KOLD cohort have been described elsewhere (8). COPD was diagnosed based on smoking history (more than 10 pack-years) and the presence of airflow limitation that was not fully reversible (post-bronchodilator FEV1/forced vital capacity [FVC] < 70% and post-bronchodilator FEV1 < 80% predicted). We included COPD patients who had wheezing history or who showed partial reversibility of airflow limitation after inhalation of salbutamol.
Fig. 1.
Patients selection.
Study protocol
Baseline clinical data were obtained after cessation of the following respiratory medications: an ICS for 2 weeks, an inhaled LABA for 2 days, an inhaled short-acting β2-agonist or inhaled short-acting anti-cholinergic for 12 hr. The baseline clinical data included demographic data, smoking history, chronic bronchitis history, wheezing history, pulmonary function tests, chest radiography and volumetric computed tomography (CT). Chronic bronchitis was defined as cough and sputum production on most days for a minimum of 3 months per year for at least 2 yr (9). Wheezing history was obtained through the following question: "Have you had wheezing or whistling in your chest at any time in the last year?" (10) Atopic status was assessed by a skin prick test to 11 common allergens, with a 10% histamine and saline control. Patients were considered to be atopic if they reacted with a wheal of larger than the histamine control for more than one of the allergens. After obtaining baseline data, patients were treated with a salmeterol/fluticasone propionate 50/500 µg dry powder inhaler twice per day for 3 months, and then spirometry and lung volume measurement were performed again after the morning medication. During the 3-month treatment period, only salbutamol was allowed as needed. Adherence to the treatment medication monitored and recorded by research coordinators.
Pulmonary function tests
Spirometry was performed using a Vmax 22 instrument (Sensor-Medics; Yorba Linda, CA, USA) or a PFDX machine (MedGraphics, St. Paul, MN, USA). To assess the post-bronchodilator change, spirometry was performed pre-bronchodilator and 15 min after inhalation of salbutamol (400 µg) through a metered-dose inhaler (MDI) with a spacer. Lung volumes were measured by body plethysmography (V6200; SensorMedics, or PFDX). Diffusing capacity for carbon monoxide (DLco) was measured by the single-breath method using a Vmax229D (Sensor-Medics) or a Masterlab Body (Jaeger AB, Würtsburg, Germany). The predicted values of FEV1, forced vital capacity (FVC), FEV1/FVC and DLco were calculated from Korean equations formulated using data from a healthy non-smoking population (11, 12). The predicted values of lung volumes were calculated from ECSC equations (13). All pulmonary function tests were performed as recommended by the American Thoracic Society/European Respiratory Society (ATS/ERS).
Computed tomography
Volumetric CT scans were performed using 16-slice multi-detector CT (MDCT) scanners, according to previous described scanning protocols (14). Image data were stored in the Digital Imaging and Communications in Medicine (DICOM) format. Using in-house software, images of the whole lung were extracted automatically and the attenuation coefficient of each pixel was measured and calculated. The cutoff level between normal lung density and a low-attenuation area (LAA) was defined as -950 HU (15). From the CT data, the volume fraction of the lung below -950 HU (V950) was calculated automatically. The airway dimensions, wall area (WA), lumen area (LA) and wall area percent (WA%, defined as WA/[WA + LA] × 100), were measured near the origin of two segmental bronchi (right apical and left apico-posterior) selected by a consensus reading of two radiologists. The software automatically detects the airway lumen and the inner and outer boundaries of the airway wall by use of a full-width-half-maximum (FWHM) method (16). The mean value of each segmental bronchus was used for analysis.
Statistical analysis
To investigate factors associated with the initial maximal positive pulmonary function response to 3 months of treatment with salmeterol/fluticasone, changes in pre-bronchodilator FEV1, FVC and inspiratory capacity (IC)/total lung capacity (TLC) before and after 3 months were used as the dependent variable in univariate and multivariate analyses. The FEV1 and FVC changes were expressed as % of predicted normal values (% predicted) to avoid the potential problem that baseline FEV1 and FVC appear to influence on FEV1 and FVC changes if expressed as % of baseline (17). Selected independent variables were sex, age, body mass index (BMI), chronic bronchitis history, wheezing history, smoking status (current or ex-smokers, smoking pack-years), pulmonary function parameters and CT parameters. For data had a normal distribution, we used Student's t-test or a oneway analysis of variance (ANOVA) for categorical variables. For data that had a non-normal distribution, we used Mann-Whitney U test or the Kruskall-Wallis test for categorical variables. Relationships between two continuous variables were examined by Pearson's correlation analysis. The prediction models for pulmonary function response to 3 months of treatment with salmeterol/fluticasone were constructed from multiple, stepwise, linear regression models. All statistical analyses were performed with the SPSS statistical package (version 12.0, SPSS Inc, Chicago, IL, USA), and P values less than 0.05 were considered significant.
Ethics statement
This study was approved by the Asan Medical Center institutional review board (Approval No. 2005-0345) and institution review boards of other10 hospitals. Written informed consent was obtained from all patients.
RESULTS
Patient characteristics
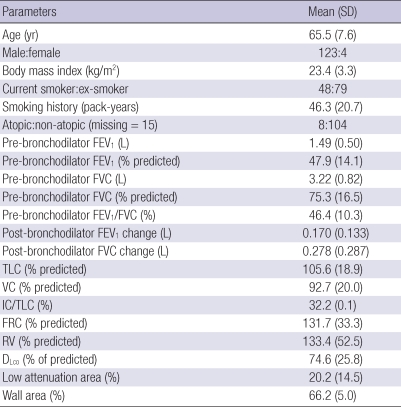
Table 1 lists the baseline characteristics of the 127 COPD patients. Of the enrolled patients, 123 (97%) were male. Mean age was 65.5 (SD: 7.6) yr, and mean smoking history was 46.3 (20.7) pack years. A total of 74 patients were classified as GOLD II (moderate COPD), 46 as GOLD III (severe COPD), and 7 as GOLD IV (very severe COPD). Ninety-one percent of subjects indicated that they had taken over 80% of the recommended medication dose.
Table 1.
Baseline characteristics of patients (N = 127)
FEV1, forced expiratory volume in 1 sec; FVC, forced vital capacity; TLC, total lung capacity; VC, vital capacity; IC, inspiratory capacity; FRC, functional residual capacity; RV, residual volume; DLco, diffusing capacity for carbon monoxide; Low attenuation area, volume fraction of the lung below -950 HU at full inspiration computed tomography; Wall area, wall area/(wall area + lumen area) on computed tomography.
Univariate analysis of baseline clinical variables and pulmonary function response to 3 months of treatment with salmeterol/fluticasone
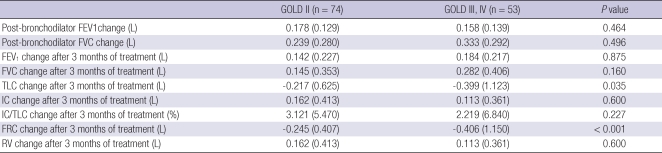
The FEV1, FVC and IC/TLC changes after 3 months of treatment were normally distributed without evidence of a separate responder group. The mean FEV1, FVC and IC/TLC changes after 3 months of the treatment were 0.160 (0.223) L, 5.1 (7.3)% predicted and 0.202 (0.380) L, 4.8 (9.0)% predicted, and 2.7 (6.1)%, respectively. There were no significant differences in the mean postbronchodilator FEV1 and FVC changes according to baseline GOLD severity stage. Patients with GOLD stage III or IV showed significantly larger TLC and functional residual capacity (FRC) reduction after the 3 months of treatment with salmeterol/fluticasone than patients with GOLD stage II. However, there were no significant differences in the mean FEV1, FVC and IC/TLC changes after 3 months of the treatment (Table 2).
Table 2.
Pulmonary function response to short-acting bronchodilator and 3 months of treatment with salmeterol/fluticasone according to baseline GOLD severity stage
Data are expressed as means with standard deviations. FEV1, forced expiratory volume in 1 sec; FVC, forced vital capacity; TLC, total lung capacity; IC, inspiratory capacity; FRC, functional residual capacity; RV, residual volume.
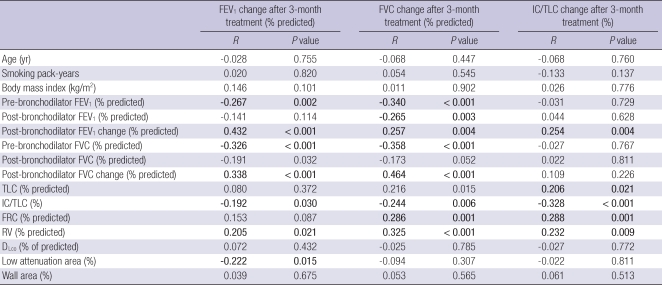
Among categorical variables, COPD patients with wheezing history had significantly greater FEV1 and FVC changes after 3 months of treatment than those without wheezing history (7.8% vs 2.7% predicted for FEV1, P < 0.001; 7.3% vs 2.3% predicted for FVC, P = 0.002). Simple correlation analysis indicated that pre-bronchodilator FEV1 and FVC had a weak negative correlation with the FEV1 and FVC changes after 3 months of the treatment but that post-bronchodilator FEV1 and FVC had no significant correlation with FEV1 and FVC changes after 3 months of the treatment. The post-bronchodilator FEV1 and FVC changes had a positive correlation with the FEV1 and FVC changes after 3 months of the treatment. LAA had a weak negative correlation with the FEV1 change after 3 months of the treatment, but mean WA was not correlated with the FEV1, FVC and IC/TLC changes after 3 months of the treatment (Table 3).
Table 3.
Correlation between baseline clinical variables and pulmonary function response to 3 months of treatment with salmeterol/fluticasone
R, correlation coefficient; FEV1, forced expiratory volume in 1 sec; FVC, forced vital capacity; TLC, total lung capacity; VC, vital capacity; IC, inspiratory capacity; FRC, functional residual capacity; RV, residual volume; DLco, diffusing capacity for carbon monoxide; Low attenuation area, volume fraction of the lung below -950 HU at full inspiration computed tomography; Wall area, wall area/(wall area + lumen area) × 100 on computed tomography.
Prediction models for pulmonary function response to 3 months of treatment with salmeterol/fluticasone
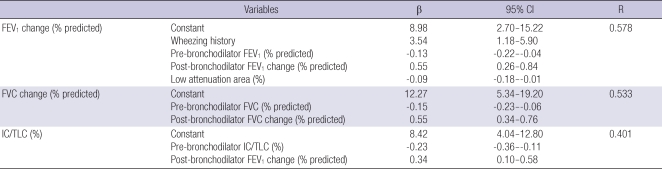
Multiple, stepwise, linear regression analysis showed that four variables, wheezing history, pre-bronchodilator FEV1, post-bronchodilator FEV1 change, and LAA were independently associated with the FEV1 change after 3 months of the treatment (R = 0.578). Multiple, stepwise, linear regression analysis also showed that two variables, pre-bronchodilator FVC and post-bronchodilator FVC change were independently associated with FVC change after the 3-month treatment (R = 0.533), and pre-bronchodilator IC/TLC and post-bronchodilator FEV1 change were independently associated with IC/TLC change after 3 months of the treatment (R = 0.401, Table 4).
Table 4.
Multiple linear regression models for pulmonary function response to 3 months of treatment with salmeterol/fluticasone
FEV1, forced expiratory volume in 1 sec; FVC, forced vital capacity; IC/TLC, inspiratory capacity/total lung capacity; Low attenuation area, volume fraction of the lung below -950 HU at full inspiration computed tomography; β, unconditioned coefficient; CI, confidence interval.
DISCUSSION
Our results show that wheezing history, baseline pulmonary function, bronchodilator responsiveness, and emphysema extent on CT could be used for predicting the pulmonary function response to 3 months of treatment with salmeterol/fluticasone in patients with COPD. This allowed us to make a significant prediction model for FEV1, FVC and IC/TLC changes after 3 months of treatment.
The response of pulmonary function to an ICS and a LABA in COPD patients has been well established in previous studies (4, 5). Current guidelines recommend combination of an ICS and a LABA for symptomatic COPD patients with post-bronchodilator FEV1 < 50% predicted and repeated exacerbation (1). However, clinical benefits from combination pharmacotherapy are not restricted to patients of severe stage of disease (18, 19). It has been difficult to predict which patients will show better responses to an ICS and a LABA. In this study, COPD patients with wheezing history, lower baseline lung function, larger bronchodilator responsiveness and lower LAA on CT responded better to the treatment with salmeterol and fluticasone. This combination would be expected to be more effective in improving the small airway component (chronic obstructive bronchiolitis) of COPD.
Wheezing is the most common symptom reported by asthmatic patients, but is also commonly reported by COPD patients (20). Marini et al. (21) reported that wheezing patients with chronic airflow obstruction differed from non-wheezing patients with chronic airflow obstruction by their bronchodilator response. Our results showed the COPD patients with a wheezing history had a significantly higher mean FEV1 and FVC changes after bronchodilator and 3 months of treatment than those without such a history. Our study also showed a positive correlation between bronchodilator responsiveness (post-bronchodilator FEV1 and FVC changes) and the FEV1 and FVC changes after 3 months of treatment. Previous studies showed that corticosteroid reversibility in COPD patients was related to features of asthma (22). Recently, Kitaguchi et al. (23) also reported that wheezing and bronchodilator responsiveness were significant determinant for the reversibility in response to an ICS.
This study also showed that COPD patients with lower pre-bronchodilator FEV1 and FVC have better responses to our combination treatment. On the contrary, there was no significant effect of post-bronchodilator FEV1 on the response to combination treatment. A post-hoc analysis in the TORCH study showed similar results in that the severity of COPD which was assessed by post-bronchodilator FEV1 was not related to the FEV1 improvements after a combination treatment (19). This result might be explained as follows. The lack of a relation between COPDseverity and treatment responsiveness may be caused by the fact that pre-bronchodilator FEV1 and post-bronchodilator FEV1 change relate to treatment responsiveness. The post-bronchodilator FEV1 and FVC (which is unrelated to responsiveness) are the sum of the value of pre-bronchodilator FEV1 and FVC (which is related to responsiveness) and the post-bronchodilator FEV1 and FVC changes (which is related to responsiveness).
CT provided an objective method for measuring the extent and severity of emphysema (15, 24). Several recent studies indicated that it is possible to separate COPD patients into emphysema-dominant and airway-dominant phenotypes by use of high resolution CT (HRCT) (23, 25, 26). Kitaguchi et al. (23) reported that lower total LAA score and the grade of bronchial wall thickening were significant determinants for bronchodilator responsiveness and for the responsiveness to the treatment with an ICS. However, other two studies found no significant differences in bronchodilator responsiveness among groups classified according to severity of emphysema (25, 26). Previously, our study group has shown that emphysema dominant COPD patients (LAA ≥ 20% and pre-bronchodilator FEV1 ≥ 45% predicted) responded poorly to the 3 months of combination treatment (27). In this study, LAA had a week negative correlation with the FEV1 change after 3 months of the treatment. This result might be explained as follows. For COPD patients, the major determinants of FEV1 are small airway disease and emphysema. If a COPD patient has a more significant emphysema component than that of small airway disease, he or she would be expected to have a poorer response to pharmacologic treatments that predominantly target small airway disease. In this study, mean WA was not correlated with the FEV1 and FVC change after 3 months of the treatment. A previous report showed that large airway dimension serve as a useful surrogate for small airway remodeling (28). Nonetheless, it is possible that the lack of a significant relationship between WA and treatment response may be due to the relatively imprecise and indirect estimate of small airway wall area. There are two factors that could have potentially confounded our volumetric CT result. First, we used three different MDCT scanners, and different scanners may have graded the emphysema index differently. A method that corrects for differences between different CT scanners has not yet been established. Second, we used only two large airways to evaluate airway dimension.
In this study, 19.7% of included patients had overlapping diagnoses of COPD and asthma (overlap syndrome). Those patients with overlap syndrome could affect our study results. However, subgroup analysis after excluding patients with overlap syndrome showed the similar results. Our study has two limitations. First, we did not consider airway inflammatory markers. Previous studies showed an increased number of eosinophils in bronchoalveolar lavage fluid in a subset of patients with COPD who responded to short-term administration of oral corticosteroids (29) and sputum eosinophil counts were significantly correlated with reversibility in response to ICS treatment (23). If we had included airway inflammatory markers, we might have been able to develop more powerful prediction models. Second, 97% of our patients were male. Gender may have a substantial influence on treatment response in COPD patients (30), so we cannot generalize our results to females.
In conclusion, wheezing history, baseline pulmonary function, bronchodilator responsiveness, and emphysema extent in COPD patients may be used for predicting the pulmonary function response to 3 months of treatment with salmeterol/fluticasone.
Footnotes
J. S. Lee, S.W. Ra, E. J. Chae, J-H Lee, E-K Kim, Y. K. Lee, T-H Kim, J. W. Huh, W. J. Kim, J. H. Lee, S-M Lee, S. Y. Lee, S. Y. Lim, T. R. Shin, H. I. Yoon and S. S. Sheen have no conflicts of interest to disclose. J. B. Seo has been an investigator in a government-sponsored study (2006-2008 Korea Science and Engineering Foundation).
Y-M. Oh has been an investigator in university-sponsored studies (Asan Institute for Life Science, University of Ulsan College of Medicine) and an industry-sponsored study (MSD Korea, and AstraZeneca Korea), and has participated as a speaker at scientific meetings organized and financed by various pharmaceutical companies (Handok, GlaxoSmithKline, AstraZeneca Korea, MSD Korea, and Boehringer Ingelheim) and a magazine company (Korea Doctors' Weekly). S-D. Lee serves as a consultant to GlaxoSmithKline, and has participated as a speaker at scientific meetings organized and financed by various pharmaceutical companies (GlaxoSmithKline, AstraZeneca Korea, and Boehringer Ingelheim).
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A040153) and by the Asan Institute for Life Science (07-306).
AUTHOR SUMMARY
Predictors of Pulmonary Function Response to Treatment with Salmeterol/fluticasone in Patients with Chronic Obstructive Pulmonary Disease
Jae Seung Lee, Jin Won Huh, Eun Jin Chae, Joon Beom Seo, Seung Won Ra, Ji-Hyun Lee, Eun-Kyung Kim, Young Kyung Lee, Tae-Hyung Kim, Woo Jin Kim, Jin Hwa Lee, Sang-Min Lee, Sangyeub Lee, Seong Yong Lim, Tae Rim Shin, Ho Il Yoon, Seung Soo Sheen, Yeon-Mok Oh, and Sang-Do Lee
Chronic obstructive pulmonary disease (COPD) is a heterogeneous disease and their responses to combination therapy (inhaled corticosteroid [ICS] + long acting β2-agonist [LABA]) are variable. Currently, reliable predictors for the responsiveness of COPD patients to the combination therapy are lacking. Here we investigated the parameters of pulmonary function test and radiological findings in the COPD patients treated for 3 months with salmeterol and fluticasone. The results show that wheezing history, pre-bronchodilator pulmonary function, bronchodilator responsiveness, and emphysema extent may be used for predicting the pulmonary function response to 3 months of treatment with the combination therapy.
References
- 1.Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 2.Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000;320:1297–1303. doi: 10.1136/bmj.320.7245.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lung Health Study Research Group. Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. N Engl J Med. 2000;343:1902–1909. doi: 10.1056/NEJM200012283432601. [DOI] [PubMed] [Google Scholar]
- 4.Mahler DA, Wire P, Horstman D, Chang CN, Yates J, Fischer T, Shah T. Effectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166:1084–1091. doi: 10.1164/rccm.2112055. [DOI] [PubMed] [Google Scholar]
- 5.Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, Yates JC, Vestbo J TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356:775–789. doi: 10.1056/NEJMoa063070. [DOI] [PubMed] [Google Scholar]
- 6.The COPD guidelines group of the standards of care committee of the BTS. BTS guidelines for the management of chronic obstructive pulmonary disease. Thorax. 1997;52(Suppl 5):S1–S28. [PMC free article] [PubMed] [Google Scholar]
- 7.Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA. Prednisolone response in patients with chronic obstructive pulmonary disease: results from the ISOLDE study. Thorax. 2003;58:654–658. doi: 10.1136/thorax.58.8.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim WJ, Oh YM, Sung J, Kim TH, Huh JW, Jung H, Lee JH, Kim EK, Lee JH, Lee SM, Lee S, Lim SY, Shin TR, Yoon HI, Kwon SY, Lee SD. Lung function response to 12-week treatment with combined inhalation of long-acting beta2 agonist and glucocorticoid according to ADRB2 polymorphism in patients with chronic obstructive pulmonary disease. Lung. 2008;186:381–386. doi: 10.1007/s00408-008-9103-9. [DOI] [PubMed] [Google Scholar]
- 9.Terminology, definitions, and classification of chronic pulmonary emphysema and related conditions: a report of the conclusions of a Ciba guest symposium. Thorax. 1959;14:286–299. [Google Scholar]
- 10.Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, Strachan D, Weiland SK, Williams HC. International study of asthma and allergies in childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8:483–491. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- 11.Park JO, Choi IS, Park KO. Normal predicted standards of single breath carbon monoxide diffusing capacity of lung in healthy nonsmoking adults. Korean J Intern Med. 1985;28:176–183. doi: 10.3904/kjim.1986.1.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi JK, Paek D, Lee JO. Normal predicted values of spirometry in Korean population. Tuberc Respir Dis. 2005;58:230–242. [Google Scholar]
- 13.Quanjer P, Dalhuijsen A, Van Zoramen B. Standardized lung function testing. Report of the working party for the European Community for Coal and Steel. Bull Eur Physiopathol Respir. 1983;19(Suppl 5):1–95. [PubMed] [Google Scholar]
- 14.Lee YK, Oh YM, Lee JH, Kim EK, Lee JH, Kim N, Seo JB, Lee SD KOLD Study Group. Quantitative assessment of emphysema, air trapping, and airway thickening on computed tomography. Lung. 2008;186:157–165. doi: 10.1007/s00408-008-9071-0. [DOI] [PubMed] [Google Scholar]
- 15.Gevenois PA, de Maertelaer V, De Vuyst P, Zanen J, Yernault JC. Comparison of computed density and macroscopic morphometry in pulmonary emphysema. Am J Respir Crit Care Med. 1995;152:653–657. doi: 10.1164/ajrccm.152.2.7633722. [DOI] [PubMed] [Google Scholar]
- 16.Wood SA, Zerhouni EA, Hoford JD, Hoffman EA, Mitzner W. Measurement of three-dimensional lung tree structures by using computed tomography. J Appl Physiol. 1995;79:1687–1697. doi: 10.1152/jappl.1995.79.5.1687. [DOI] [PubMed] [Google Scholar]
- 17.Calverley PM, Burge PS, Spencer S, Anderson JA, Jones PW. Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax. 2003;58:659–664. doi: 10.1136/thorax.58.8.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calverley P, Pauwels RA, Jones PW, Anderson JA, Vestbos J. The severity of airways obstruction as a determinant of treatment response in COPD. Int J Chron Obstruct Pulmon Dis. 2006;1:209–218. doi: 10.2147/copd.2006.1.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jenkins CR, Jones PW, Calverley PM, Celli B, Anderson JA, Ferguson GT, Yates JC, Willits LR, Vestbo J. Efficacy of salmeterol/fluticasone propionate by GOLD stage of chronic obstructive pulmonary disease: analysis from the randomised, placebo-controlled TORCH study. Respir Res. 2009;10:59. doi: 10.1186/1465-9921-10-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meslier N, Charbonneau G, Racineux J. Wheezes. Eur Respir J. 1995;8:1942–1948. doi: 10.1183/09031936.95.08111942. [DOI] [PubMed] [Google Scholar]
- 21.Marini JJ, Pierson DJ, Hudson LD, Lakshminarayan S. The significance of wheezing in chronic airflow obstruction. Am Rev Respir Dis. 1979;120:1069–1072. doi: 10.1164/arrd.1979.120.5.1069. [DOI] [PubMed] [Google Scholar]
- 22.Chanez P, Vignola AM, O'Shaugnessy T, Enander I, Li D, Jeffery PK, Bousquet J. Corticosteroid reversibility in COPD is related to features of asthma. Am J Respir Crit Care Med. 1997;155:1529–1534. doi: 10.1164/ajrccm.155.5.9154853. [DOI] [PubMed] [Google Scholar]
- 23.Kitaguchi Y, Fujimoto K, Kubo K, Honda T. Characteristics of COPD phenotypes classified according to the findings of HRCT. Respir Med. 2006;100:1742–1752. doi: 10.1016/j.rmed.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 24.Nakano Y, Muro S, Sakai H, Hirai T, Chin K, Tsukino M, Nishimura K, Itoh H, Paré PD, Hogg JC, Mishima M. Computed tomographic measurements of airway dimensions and emphysema in smokers. Correlation with lung function. Am J Respir Crit Care Med. 2000;162:1102–1108. doi: 10.1164/ajrccm.162.3.9907120. [DOI] [PubMed] [Google Scholar]
- 25.Boschetto P, Miniati M, Miotto D, Braccioni F, De Rosa E, Bononi I, Papi A, Saetta M, Fabbri LM, Mapp CE. Predominant emphysema phenotype in chronic obstructive pulmonary. Eur Respir J. 2003;21:450–454. doi: 10.1183/09031936.03.00048703. [DOI] [PubMed] [Google Scholar]
- 26.Makita H, Nasuhara Y, Nagai K, Ito Y, Hasegawa M, Betsuyaku T, Onodera Y, Hizawa N, Nishimura M Hokkaido COPD Cohort Study Group. Characterisation of phenotypes based on severity of emphysema in chronic obstructive pulmonary disease. Thorax. 2007;62:932–937. doi: 10.1136/thx.2006.072777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee JH, Lee YK, Kim EK, Kim TH, Huh JW, Kim WJ, Lee JH, Lee SM, Lee S, Lim SY, Shin TR, Yoon HI, Sheen SS, Kim N, Seo JB, Oh YM, Lee SD. Responses to inhaled long-acting beta-agonist and corticosteroid according to COPD subtype. Respir Med. 2010;104:542–549. doi: 10.1016/j.rmed.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 28.Nakano Y, Wong JC, de Jong PA, Buzatu L, Nagao T, Coxson HO, Elliott WM, Hogg JC, Paré PD. The prediction of small airway dimensions using computed tomography. Am J Respir Crit Care Med. 2005;171:142–146. doi: 10.1164/rccm.200407-874OC. [DOI] [PubMed] [Google Scholar]
- 29.Lapperre TS, Snoeck-Stroband JB, Gosman MM, Stolk J, Sont JK, Jansen DF, Kerstjens HA, Postma DS, Sterk PJ Groningen and Leiden Universities Corticosteroids in Obstructive Lung Disease Study Group. Dissociation of lung function and airway inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004;170:499–504. doi: 10.1164/rccm.200401-112OC. [DOI] [PubMed] [Google Scholar]
- 30.Han MK, Postma D, Mannino DM, Giardino ND, Buist S, Curtis JL, Martinez FJ. Gender and chronic obstructive pulmonary disease: why it matters. Am J Respir Crit Care Med. 2007;176:1179–1184. doi: 10.1164/rccm.200704-553CC. [DOI] [PMC free article] [PubMed] [Google Scholar]