Abstract
Binge eating disorder (BED) presents with substantial psychiatric comorbidity. This latent structure analysis sought to delineate boundaries of BED given its comorbidity with affective and anxiety disorders. A population-based sample of 151 women with BED, 102 women with affective or anxiety disorders, and 259 women without psychiatric disorders was assessed with clinical interviews and self-report questionnaires. Taxometric analyses were conducted using DSM-IV criteria of BED and of affective and anxiety disorders. The results showed a taxonic structure of BED and of affective and anxiety disorders. Both taxa co-occurred at an above-chance level, but also presented independently with twice-as-large probabilities. Within the BED taxon, diagnostic co-occurrence indicated greater general psychopathology, lower social adaptation, and greater premorbid exposure to parental mood and substance disorder, but not greater eating disorder psychopathology. Eating disorder psychopathology discriminated individuals in the BED taxon from individuals in the affective and anxiety disorders taxon. Diagnostic criteria of BED were more indicative of the BED taxon than were criteria of affective and anxiety disorders. The results show that at the latent level, BED was co-occurring with, yet distinct from, affective and anxiety disorders and was not characterized by an underlying affective or anxiety disorder.
Keywords: classification, psychiatric taxonomies, comorbidity, binge eating, eating disorders
Introduction
Classification of eating disorders is an enduring focus of debate. It relates to our understanding of the nature of pathology and its boundaries with other disorders, especially the preliminarily defined binge eating disorder (BED). Given BED’s substantial comorbidity with affective and anxiety disorders (Grilo, White, & Masheb, 2009; Javaras, Pope, Lalonde et al., 2008; Wilfley, Friedman, Dounchis et al., 2000), the current study sought to elucidate at the latent level whether BED represents an associated feature of affective and anxiety disorders, or a separate mental disorder.
Included in the Diagnostic and Statistical Manual of Mental Disorders fourth edition (DSM-IV) as a provisional diagnosis in need of further study, BED is characterized by recurrent binge eating that occurs in the absence of regular compensatory behaviors (American Psychiatric Association, 1994, 2000). Ample evidence has accumulated that BED is a clinically significant disorder, associated with overweight and obesity, impaired quality of life, and increased general psychopathology and psychiatric comorbidity, especially affective and anxiety disorders (Latner & Clyne, 2008; Striegel-Moore & Franko, 2008; Wilfley, Wilson, & Agras, 2003; Wonderlich, Gordon, Mitchell, Crosby, & Engel, 2009). In anticipation of DSM-V, researchers have begun to empirically examine the boundaries of BED within the eating and weight disorders spectrum, using specific analytical procedures to examine their latent structure, such as taxometric or latent class analysis (Bulik, Sullivan, & Kendler, 2000; Eddy, Crosby, Keel et al., 2009; Mitchell, Crosby, Wonderlich et al., 2007; Striegel-Moore, Franko, Thompson et al., 2005; Wade, Crosby, & Martin, 2006; Williamson, Womble, Smeets et al., 2002). In contrast, the nature of the relationship between BED and other co-occurring psychiatric disorders has received little attention (see Wonderlich, Joiner, Keel, Williamson, & Crosby, 2007).
Psychiatric comorbidity in BED is important to our understanding of this disorder. Some researchers have proposed that BED is a marker of psychopathology within obese individuals rather than a separate mental disorder, due to its fluctuating course and non-specific response to pharmacological and psychological treatment (Stunkard & Allison, 2003). Although the validity of this position has been increasingly challenged by evidence documenting BED’s stability (Fichter, Quadflieg, & Hedlund, 2008; Hudson, Hiripi, Pope, & Kessler, 2007), normative placebo-response (Jacobs-Pilipski, Wilfley, Crow et al., 2007), and specific responsiveness to psychological treatment (Grilo, Masheb, & Wilson, 2006; Masheb & Grilo, 2007; Wilson, Wilfley, Agras, & Bryson, 2010), it remains unknown how strongly BED and major comorbid conditions such as affective and anxiety disorders are related at the latent level. If BED is an associated feature of affective or anxiety disorders, it should be more likely to co-occur with these conditions than to present without them. In addition, the question has been raised as to whether BED is characterized by an underlying affective (Devlin, Goldfein, & Dobrow, 2003) or anxiety disorder. If this was the case, diagnostic indicators of affective or anxiety disorders should at the latent level be more characteristic of BED than its own diagnostic criteria. These are questions that await examination.
In this context, the goal of the present study was to examine the latent structure of BED in relation to that of comorbid psychiatric disorders in order to elucidate (1) whether BED is an associated feature of affective and anxiety disorders and (2) whether it is characterized by an underlying affective or anxiety disorder. For external validation, associations of latent structures were examined with clinically relevant parameters of eating disorder and general psychopathology, health care use, social adaptation, and etiological factors.
Method
Design and Recruitment
Under the auspices of the New England Women’s Health Project, BED cases, psychiatric controls, and non-psychiatric controls were recruited using two recruitment avenues: The first avenue involved telephone recruitment utilizing a consumer information database of 10,000 women; the second avenue consisted of an advertising campaign using posters, newspaper advertisements, community referrals, and public service announcements.
After completion of a telephone screening interview, eligible individuals were invited to participate in the study that included diagnostic interviews, a risk factor interview, and several self-report instruments. Body weight and height were measured. The institutional review boards at Wesleyan and Columbia Universities approved this study. (For further methodological detail, see Pike, Hilbert, Wilfley et al., 2008; Striegel-Moore et al., 2005).
Participants
Participants in this study were 151 women with BED as their primary diagnosis, 102 women with non-eating disorder DSM-IV psychiatric diagnoses (PC group), and 259 women with no psychiatric diagnosis (NC group). Exclusion criteria for all groups were physical conditions known to influence eating or weight, current pregnancy, or presence of a psychotic disorder. For the BED group, inclusion required presence of all DSM-IV criteria for BED. Diagnosis of current BED was ascertained through the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993), a semi-structured, investigator-based interview, considered to be the gold standard in eating disorder diagnosis. For the PC group, inclusion required the presence of a lifetime DSM-IV axis I affective or anxiety disorder, but no history of clinically significant eating disorder symptoms. Psychiatric diagnoses other than eating disorders were made using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 1997), a well-established, semi-structured diagnostic interview. For the NC group, inclusion required absence of past or current clinically significant eating disorder symptoms and absence of a current psychiatric disorder. Both diagnostic interviews were conducted by trained assessors (bachelor level or higher) who received ongoing supervision to ensure standardized administration.
Sociodemographic and clinical characteristics are presented in Table 1. The BED group had a higher BMI than the other study groups and was more racially diverse than the PC group (p < .001; see Hudson et al., 2007; Striegel-Moore et al., 2005). Both clinical groups had higher rates of lifetime and current affective and anxiety disorders than the NC group, and the PC group had higher rates of lifetime and current anxiety disorders than the BED group (all p < .001). A total of N = 140 probands had a current affective or anxiety disorder.
Table 1.
Sociodemographic and Clinical Characteristics.
| BED | PC | NC | Univariate tests | Post-hoc tests (p < .01) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N = 151 | N = 102 | N = 259 | ||||||||
| M | SD | M | SD | M | SD | F | df | p | ||
| Age, Years | 31.12 | 5.81 | 29.61 | 6.85 | 30.07 | 5.44 | 2.40 | 2, 509 | .092 | |
| Body Mass Index, kg/m2 | 34.45 | 9.54 | 26.04 | 6.94 | 25.50 | 6.23 | 73.59 | 2, 509 | < .001 | BED > PC, NC |
| n | % | n | % | n | % | χ2 | df | p | ||
| Race | 9.91 | 2 | .007 | BED > PC | ||||||
| Black | 56 | 37.1 | 19 | 18.6 | 78 | 30.1 | ||||
| White | 95 | 62.9 | 83 | 81.4 | 181 | 69.9 | ||||
| Education | 1.97 | 4 | .741 | |||||||
| High School or Less | 30 | 19.9 | 21 | 20.6 | 41 | 15.8 | ||||
| Some College | 76 | 50.3 | 48 | 47.1 | 131 | 50.6 | ||||
| College Grad or Higher | 45 | 29.8 | 33 | 32.4 | 87 | 33.6 | ||||
| Lifetime Psychiatric Comorbidity | ||||||||||
| Affective Disorder | 102 | 67.5 | 69 | 67.6 | 12 | 4.6 | 220.86 | 2 | < .001 | BED, PC > NC |
| Anxiety Disorder | 61 | 40.4 | 69 | 67.6 | 14 | 5.4 | 79.49 | 2 | < .001 | PC > BED > NC |
| Affective or Anxiety Disorder | 119 | 78.8 | 102 | 100.0 | 24 | 9.3 | 323.67 | 2 | < .001 | PC > BED > NC |
| Current Psychiatric Comorbidity | ||||||||||
| Affective Disorder | 38 | 25.2 | 29 | 28.4 | 0 | 0.0 | 156.20 | 2 | < .001 | BED, PC > NC |
| Anxiety Disorder | 38 | 25.2 | 57 | 55.9 | 0 | 0.0 | 157.42 | 2 | < .001 | PC > BED > NC |
| Affective or Anxiety Disorder | 62 | 41.1 | 78 | 76.5 | 0 | 0.0 | 235.68 | 2 | < .001 | PC > BED > NC |
Note. BED indicates binge eating disorder; PC, psychiatric control group; NC, non-psychiatric control group.
Assessment
Diagnostic indicators of BED were derived from the Eating Disorder Examination-Questionnaire (EDE-Q; Fairburn & Beglin, 1994), the self-report questionnaire version of the EDE, that was administered to the total sample. The diagnostic indicators of the EDE-Q included frequencies of Objective Bulimic Episodes (OBEs), Subjective Bulimic Episodes (SBEs), and episodes of Compensatory Behaviors over the past 28 days (i.e. total episodes of self-induced vomiting, laxative or diuretic misuse, or excessive exercising), and the degree of Overvaluation of Shape or Weight (composite item, ranging from 0 to 6, with higher scores indicating more severe overvaluation), a criterion that has been recommended as a diagnostic criterion or specifier in the forthcoming revision of the DSM (Latner & Clyne, 2008; Wilfley, Bishop, Wilson, & Agras, 2007; Wonderlich et al., 2009). In previous studies, stability and convergent validity were adequate for OBEs and Overvaluation of Shape or Weight, while validity was more variable for Compensatory Behaviors and SBEs (Hilbert, Tuschen-Caffier, & Ohms, 2004; Mond, Hay, Rodgers, Owen, & Beumont, 2004; Reas, Grilo, & Masheb, 2006). In the current study, convergent validity of the EDE-Q-derived diagnostic indicators was determined through concordance with the EDE that had been used for ascertaining BED diagnosis in the eating disorder group only. Effect sizes were moderate for the number of OBEs (Kendall’s τb = .36, p < .001) and large for Overvaluation of Shape or Weight (Pearson’s r = .61, p < .001; evaluation according to Cohen, 1988).
Diagnostic indicators of current mood and anxiety disorders were derived from the SCID-I (First et al., 1997). In order to form quantitative scales, leading diagnostic items were summed after being coded as present or absent for all main affective and anxiety disorders or syndromes (i.e., initial codes 3 = threshold were recoded as 1, while initial codes 1 = absent and 2 = subthreshold were recoded as 0). For example, for current Major Depressive Episode, the SCID-I items of depressed mood (A1), lack of interest (A2), change of weight (A3), insomnia/hypersomnia (A6), psychomotor agitation/retardation (A9), lack of energy (A12), feelings of worthlessness (A13), poor concentration (A16), and suicidal tendencies (A19) were summed, creating a scale ranging from 0 to 9. Likewise, leading symptoms for other main mood and anxiety disorders or syndromes were summed: Manic Episode (8 items), Dysthymic Episode (7 Items), Panic Attack (4 items), Agoraphobia (2 items), Social Phobia (4 items), Specific Phobia (4 items), Obessive-Compulsiveness (6 items), Posttraumatic Stress (5 items), and Generalized Anxiety (3 items). (A detailed list of items is available upon request).
Validators
As a measure of eating disorder psychopathology, the EDE-Q subscale composites of Restraint and Eating Concern were used (5 items each, ranging from 0 to 6, with higher scores indicating more psychopathology). Both subscales have demonstrated adequate internal consistency, stability, and convergent validity (Peterson et al., 2007; Reas et al., 2006). For the current study sample, internal consistencies as measured by Cronbach a were .78 for Restraint and .86 for Eating Concern.
General psychopathology was assessed through the index of global severity (GSI) from the Brief Symptom Inventory (BSI; Derogatis, 1977). Scores range from 0 to 100, with higher scores indicating more severe psychiatric symptoms, and were T-standardized. The GSI-BSI has good internal consistency and is highly correlated with the GSI of the lengthier, well-established Symptom-Checklist-90-R. Internal consistency of the GSI in the current study sample was Cronbach α = .97.
Health Services Use was determined by whether participants reported any medical or psychotherapeutic consultations, emergency room visits, or partial or full hospitalizations in the year prior to assessment (total score ranging from 0 to 5; Striegel-Moore, Dohm, Wilfley et al., 2004).
The Social Adjustment Scale (SAS; Weissman & Bothwell, 1976) was used as a general measure of social functioning in a broad range of domains (e.g., role performance, interpersonal relationships, social and leisure activities). Scores range from 0 to 5, with higher scores indicating poorer social functioning. The SAS has good reliability and validity (Goldman, Skodol, & Lave, 1992; Weissman, Prusoff, Thompson, Harding, & Myers, 1978), and in the current study, mean Cronbach α for the SAS subscales was .78.
Early life experiences were assessed retrospectively using the Oxford Risk Factor Interview (RFI; Fairburn, Doll, Welch et al., 1998). The RFI assesses biological, psychological, and social factors believed to increase risk for the development of an eating disorder. Assessment focuses on the period before the “index age,” that is, the age at which significant and persistent eating disorder symptoms first appeared. Individuals in the PC and in the NC group were assigned the index age of the BED case for which they had served as a comparison subject. Scores of the risk factor items range from 0 to 4, with higher scores indicating more severe or frequent exposure. In order to reduce the likelihood of false positives, data were recoded into 1 = definite exposure (initially coded 3 or 4) versus 0 = no definite exposure (initially coded 0, 1, or 2). Based on factor analytic procedures (see Striegel-Moore et al., 2005), seven composite risk factor domains were derived from the individual risk factor items and considered in the current report: Participant’s Mental Health, Participant’s Physical Health, Other Environmental Experiences, Family Weight and Eating Concerns, Quality of Parenting, Parental Psychopathology, and Childhood Abuse.
Data Analysis
The taxometric method is a family of statistical procedures designed to determine latent structures of phenomena and is well-suited for research on the classification of disorders in relation to co-occurring conditions (for methodological detail see Beauchaine, 2007; Ruscio et al., 2004, 2006). Taxometric procedures explore the associations among manifest indicator variables to determine whether the underlying structure is dimensional and consists of a single latent continuum, or taxonic and consists of two latent classes (i.e. a taxon and its complement).
Indicator selection
The taxometric method requires that variables used as indicators of the target construct distinguish the putative taxon and its complement with sufficient validity (usually d ≥ 1.25) and be substantially less correlated within these classes than in the full sample (nuisance covariance; Meehl, 1995; Ruscio et al., 2006). To address these requirements, validity was estimated by examining the separation of the putative taxa and complements on each indicator variable, and by examining the correlation between them within the putative taxa and complements in a preparatory step. All variables were z-standardized prior to analyses.
Taxometric analyses
The taxometric analyses pursued the following steps: In order to determine (1) whether BED is an associated feature of affective and anxiety disorders, the taxonicity or continuity of BED was established using the diagnostic indicators for BED; the taxonicity or continuity of current affective and anxiety disorders was determined using the diagnostic indicators of affective and anxiety disorders; and the association between the latent structures of the identified taxa or continua of BED and affective/anxiety disorders was examined (Ruscio & Ruscio, 2004). For each individual, the taxon membership or location on a continuum was estimated using the base-rate technique (Ruscio, 2009). Individuals’ estimated class membership or dimensional scores were then used to estimate the degree of association between the two latent constructs as a test of diagnostic co-occurrence. In order to address (2) whether there is an underlying affective or anxiety disorder in BED, the strength of association of diagnostic indicators of both BED and affective and anxiety disorders with membership to the BED taxon was examined, clarifying whether the diagnostic indicators of BED were more characteristic of that latent structure than the diagnostic indicators of affective and anxiety disorders.
Data were submitted to the taxometric procedure MAMBAC (mean above minus below a cut; Meehl & Yonce, 1994), programmed in R. The SD of the base rate estimate was evaluated. For bootstrapping, the averaged empirical curves were compared to those derived on the basis of simulated taxonic and dimensional comparison data (Ruscio & Marcus, 2007). The curves yielded by these procedures were then inspected for evidence of taxonic or dimensional structure by n = 24 independent raters, blind to study design and hypotheses (−1 = taxonic, 0 = neither/nor, 1 = dimensional). A comparison curve fit index (CCFI) was calculated to quantify the match between the results for research data and those of taxonic and dimensional comparison data. CCFI values can range from 0 = dimensional to 1 = taxonic, with values < .40 indicating a dimensional structure, and values > .60 indicating a taxonic structure.
Consistency check
As a consistency check, the taxometric procedure MAXSLOPE (maximum slope) (Grove, 2004, 2005), programmed in R, and latent profile analysis (LPA; Latent Gold 4.5) were conducted using the same quantitative indicators as in the MAMBAC analyses. For MAXSLOPE, the SD of the base rate estimate and the goodness of fit index (GFI; Waller & Meehl, 1998) were considered for evaluation of latent structure. The curves yielded by MAXSLOPE were inspected for evidence of taxonic or dimensional structure by n = 24 independent raters, blind to study design and hypotheses (−1 = non-linear increase or decrease [i.e. taxonic], 0 = neither/nor, 1 = no non-linear increase or decrease [i.e. dimensional]). In the taxonic case, consistency of individuals’ assignment to latent structures by MAMBAC and by MAXSLOPE was evaluated using the tetrachoric correlation coefficient.
In addition, LPA was used as a consistency check (as recommended by R. Crosby, personal communication, 01.09.2009). LPA models varying the number of LPs from 1 to 4 were evaluated, using parameters estimated by maximum likelihood. The number of clusters was determined through minimization of the sample-size adjusted Bayesian information criteria parsimony index (Sclove, 1987) and of the consistent Akaike information criterion (Bozdogan, 1987). Assignment of cluster membership was based on Bayesian probabilities. In cases in which taxometric analysis revealed a latent taxon/complement, LPA was expected to produce at least two latent profiles. If taxometric analyses were suggestive of a latent dimension, LPA was expected to identify one single latent profile. In order to detect spurious classes (Uebersax, 1999), plots of classes across indicators were visually inspected for parallel lines. In the taxonic case, consistency of individuals’ assignment to latent structures by taxometric analyses and by LPA was evaluated using the tetrachoric correlation coefficient.
Analysis of diagnostic co-occurrence
The strength of association between the latent structure of BED and diagnostic indicators of BED, and of affective and anxiety disorders, was examined using biserial correlation coefficients, interpreted according to Cohen (1988; small: r ≥ 0.10, medium: r ≥ 0.30, large: r ≥ 0.50) and compared using z tests for correlation coefficients.
Validation analyses
For validation analyses, comparisons of health services use, social adaptation, risk factors, eating disorder psychopathology, and general psychopathology by individuals’ estimated class membership or dimensional scores were conducted. These were based on GLM and post hoc Tukey tests for continuous variables, χ2 tests for categorical variables, or correlation analyses (product-moment, Kendall’s τb, or point-biserial correlation coefficients; analyses conducted using SPSS 17.0). Significance level for all statistical analyses was set at a two-tailed α < .05 (for post hoc analyses, α < .01).
Preliminary Analysis: Indicator Selection
Latent structure of BED
Within the diagnostic indicators of BED (OBEs, SBEs, Overvaluation of Shape or Weight, Compensatory Behaviors), SBEs and Compensatory Behaviors did not sufficiently discriminate between the putative taxon of BED versus the putative complement of PC and NC (d < 1.25). In addition, the nuisance covariation criterion was violated for SBEs that showed similar correlations with Overvaluation of Shape or Weight and Compensatory Behaviors in the full sample as in the putative taxon and/or complement (full sample r = .41 vs. taxon r = .12, complement r = .39; full sample r = .31 vs. taxon r = .24, complement r = .26). Formation of a composite from OBEs and SBEs did not lead to a better nuisance covariation. Therefore, the indicator variables of OBEs and Overvaluation of Shape or Weight were selected for taxometric analysis. Summary statistics for all selected indicators are presented in Table 2.
Table 2.
Correlations and Validity Estimates for Indicators in Taxometric Analyses (N = 512).
| (a) Criteria of BED in a BED Taxon (n = 151) and Complement (n = 361) | ||
|---|---|---|
| OBEs | Overvaluation of Shape or Weight | |
|
Correlations |
||
| Overvaluation Shape or Weight | .53 (.22/.33) | |
|
Validity
Estimates |
||
| Taxon M (SD) | 0.91 (1.17) | −0.53 (0.12) |
| Complement M (SD) | 0.89 (0.91) | −0.52 (0.60) |
| Validity (d) | 2.23 | 2.01 |
| Skew | 2.65 | 0.58 |
| (b) Criteria of Affective and Anxiety Disorders in a Taxon of Current Affective and Anxiety Disorders (n = 140) and Complement (n = 372) | ||
|
Correlations |
||
| Affective Disorder | Anxiety Disorder | |
| Anxiety Disorder | .28 (.13/−.12) | |
|
Validity
Estimates |
||
| Taxon M (SD) | 1.56 (1.63) | 1.31 (1.34) |
| Complement M (SD) | −0.23 (0.45) | −0.23 (0.71) |
| Validity (d) | 1.97 | 1.67 |
| Skew | 2.79 | 1.97 |
Note. OBEs indicate objective bulimic episodes. Correlation coefficients are displayed as full sample (taxon/complement).
Latent structure of affective and anxiety disorders
The SCID-I items for current affective and anxiety disorders had low validity to discriminate between the putative taxon of current affective and anxiety disorders and the putative complement. Only Major Depressive Episode yielded a d ≥ 1.25. As the correlation matrix did not display clear indication to group items, composite diagnostic indicators (i.e. total number of symptoms) of affective disorders and anxiety disorders were formed. These composite indicators displayed sufficient validity (d = 1.97, 1.67) and satisfied the nuisance covariance criterion (see Table 2).
Results
(1) Is BED an Associated Feature of Affective and Anxiety Disorders?
Latent structure of BED
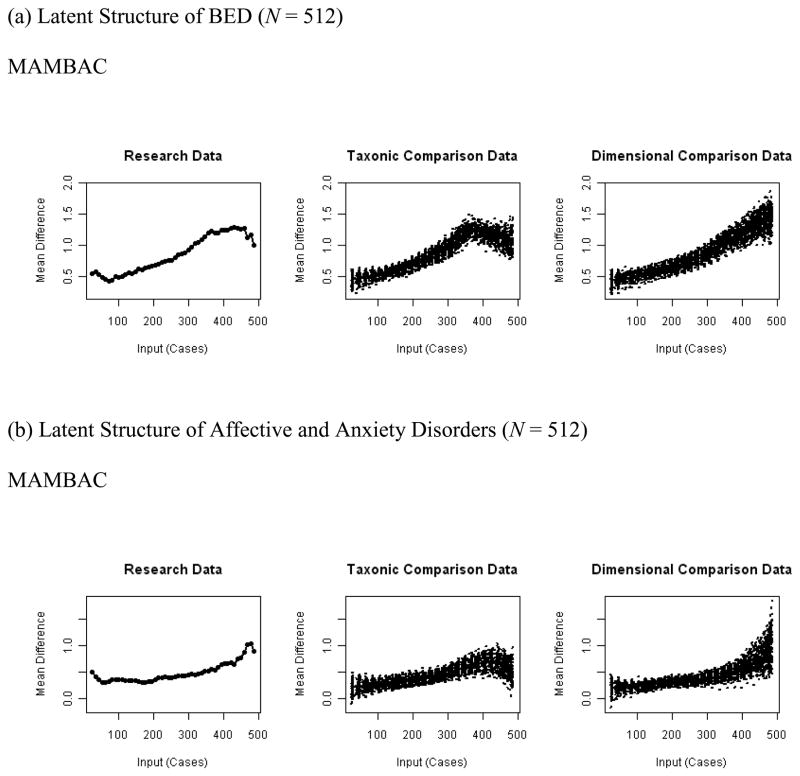
In the MAMBAC analysis of the latent structure of BED, both curves contained peaked shapes consistent with taxonic structure. The averaged curve, shown in Figure 1, was more similar to that for taxonic than dimensional comparison data; in fact, all independent, blind raters indicated a taxonic structure (24/24, 100.0%). The CCFI > .60 and small SD of base rate estimates (Table 3) provided further evidence of taxonic structure.
Figure 1.
Empirical and Simulated Averaged Curves From Taxometric Analyses.
Note. MAMBAC indicates mean above minus below a cut.
Table 3.
Estimated Base Rate and Comparison Curve Fit Index (CCFI) for Taxometric Analyses (N = 512).
| Taxon Base Rate Estimate | CCFI | |
|---|---|---|
| M (SD) | ||
| Latent Structure of BED | ||
| MAMBAC | .36 (.05) | .62 |
| Latent Structure of Affective and Anxiety Disorders | ||
| MAMBAC | .36 (.01) | .41 |
Note. CCFI ranges from 0 = dimensional to 1 = taxonic. CCFI > .50 is interpreted as evidence in support of taxonic structure. MAMBAC indicates mean above minus below a cut.
Consistently, the MAXSLOPE analysis yielded curves with a non-linear increase. All independent, blind raters indicated a taxonic structure (24/24, 100.0%). The large GFI (0.97) and small SD of base rate estimates (0.00) provided further evidence of taxonic structure. Consistency with the MAMBAC solution was high (tetrachoric rtetr = .94, p < .001). Further, the LPA produced a 2-profile solution (χ2(69, N = 512) = 59.29, p = .79), demonstrating high consistency with the MAMBAC solution (rtetr = .98, p < .001).
Overall, the evidence was in support of a taxonic structure. The taxon as derived from the MAMBAC analysis included 158 individuals (30.9% out of 512): 124 individuals with BED (78.5% out of 158), 12 individuals from the NC group (7.6%), and 22 individuals from the PC group (13.9%) (χ2(2, N = 512) = 273.58, p < .001). As indicated by large effect sizes, the individuals assigned to the taxon had greater values for OBEs and Overvaluation of Shape or Weight than individuals assigned to the complement (d = 1.67, 3.21).
Latent structure of affective and anxiety disorders
In the MAMBAC analysis of the latent structure of affective and anxiety disorders, both curves contained peaks, but these peaks appeared at the very right hand of the distribution and were not clearly marked. The averaged curve, depicted in Figure 1, provided some evidence of a taxonic structure, albeit not unambiguously; visual inspection through independent, blind raters yielded in 66.7% (16/24) of raters evidence of a taxonic structure. The low SD of base rate estimates provided evidence for a taxonic structure, and the CCFI score was neither clearly in favor nor against a taxonic structure, as CCFI scores between .40 and .60 should be interpreted with caution.
The MAXSLOPE analysis yielded one curve with a non-linear increase (affective disorders, anxiety disorders) and one with a rather linear increase (anxiety disorders, affective disorders): For the first curve, 75.0% of independent, blind raters raters (18/24) indicated a non-linear increase, while for the second curve, 41.7% indicated a non-linear increase (10/24) Overall, the large GFI (1.00) and small SD of base rate estimates (0.00) provided evidence of taxonic structure. Consistency with the MAMBAC solution was high (rtetr = .88, p < .001). The LPA produced a 2-profile solution (χ2(270, N = 512) = 199.00, p > .99) that was highly consistent with the taxonic structure identified in the MAMBAC analysis (rtetr = 1.00, p < .001).
Overall, most of the evidence was in support of a taxonic structure for affective and anxiety disorders, but not unambiguously. Further analysis therefore used a taxon, comprised by 92 individuals (18.0% out of 512): 54 individuals with BED (35.8% out of 92), 1 individual from the NC group (0.4%), and 37 individuals from the PC group (36.3%) (χ2(2, N = 512) = 109.94, p < .001). Demonstrated by large effect sizes, the taxon was characterized by greater values for affective and anxiety disorders than the complement (d = 1.25, 2.24).
Diagnostic co-occurrence
For the analysis of diagnostic co-occurrence, the product of the base rates of both diagnoses at the manifest level (BED diagnosis: 151/512 = 0.29; diagnosis of affective or anxiety disorder: 0.27 = 140/512; product of base rates: 0.29 × 0.27 = 0.08) was compared with the co-occurrence of the taxa of BED and of affective and anxiety disorders at the latent level (55/512 = 0.11; see Table 4), following the analytic approach described by Ruscio and Ruscio (2004). The co-occurrence at the latent level exceeded that of the manifest level (0.11 > 0.08, z test, p = .017), suggesting that the two conditions co-occurred at greater-than-chance level. The latent taxa were statistically independent (χ2(1, N = 512) = 43.97, p < .001). The BED taxon was approximately twice as likely to occur without the taxon of affective or anxiety disorders (0.65, 103/158) than to co-occur with this taxon (0.35, 55/158) (χ2(1, N = 158) = 14.58, p < .01).
Table 4.
Co-Occurrence of the Latent Taxa of BED and Affective/Anxiety Disorders (N = 512).
| BED Taxon | |||
|---|---|---|---|
| Absent | Present | ||
| Affective/Anxiety | Absent | 317 (61.9%) | 103 (20.1%) |
| Disorder Taxon | Present | 37 (7.2%) | 55 (10.7%) |
Validation analyses
As shown in Table 5, individuals in the BED taxon with and without co-occurring affective or anxiety disorders had similar eating disorder psychopathology, health services use, and early childhood experiences (p > .01). Diagnostic co-occurrence within the BED taxon indicated greater general psychopathology, lower social adaptation, and greater premorbid exposure to parental mood and substance disorder (p < .01). Individuals from the BED taxon with and without co-occurring affective or anxiety disorders were significantly different from individuals from the affective or anxiety disorders taxon without co-occurring BED on eating disorder psychopathology (p < .01), but not on general psychopathology, health services use, social adaptation, or early life experiences (p > .01). Both taxa with and without diagnostic co-occurrence differed significantly on nearly all validators from the complement (p < .01). There were no group differences on sociodemographic characteristics including BMI (p > .05).
Table 5.
Validation of Taxa of BED and of Affective and Anxiety Disorders With or Without Diagnostic Co-occurrence (N = 512).
| BED Taxon without Co-occurrence | Affective and Anxiety Disorders Taxon without Co-occurrence | Co-occurrence | Complement | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 103 | N = 37 | N = 55 | N = 317 | ||||||||
| M | SD | M | SD | M | SD | M | SD | F | df | p | |
| Psychopathology | |||||||||||
| Restraint (EDE-Q) | 2.34a | 1.39 | 1.01b | 1.21 | 2.17a | 1.36 | 0.90b | 1.10 | 47.46 | 3, 508 | <.001 |
| Eating Concern (EDE-Q) | 2.60a | 1.36 | 0.65b | 0.94 | 2.86a | 1.03 | 0.45b | 0.72 | 206.93 | 3, 507 | <.001 |
| General Psychopathology (BSI GSI) | 66.44a | 20.89 | 72.48ab | 26.27 | 78.26b | 21.28 | 49.73c | 11.63 | 70.64 | 3, 492 | <.001 |
| Health Services Use | 1.61a | 0.92 | 1.86a | 0.83 | 1.90a | 1.00 | 1.30b | 0.72 | 13.58 | 3, 481 | <.001 |
| Social Adaptation (SAS) | 1.99a | 0.48 | 1.93ab | 0.39 | 2.18b | 0.52 | 1.55c | 0.35 | 50.87 | 3, 420 | <.001 |
| Early Childhood Experiences (RFI) | |||||||||||
| Participant’s Mental Health | 0.33a | 1.38 | 0.64a | 1.64 | 0.71a | 1.36 | −0.56b | 0.67 | 45.36 | 3, 508 | <.001 |
| Participant’s Physical Health | 0.43a | 1.96 | −0.26ab | 1.58 | 0.69a | 2.35 | −0.27a | 1.18 | 9.74 | 3, 508 | <.001 |
| Sexual and Physical Abuse | 0.48a | 2.48 | 0.63a | 2.16 | 1.26a | 2.61 | −0.56b | 1.86 | 16.41 | 3, 508 | <.001 |
| Other Environmental Experiences | 0.19a | 1.61 | −0.17ab | 1.26 | 0.75a | 1.78 | −0.33b | 1.40 | 10.00 | 3, 508 | <.001 |
| Family Weight and Eating Concerns | 0.14a | 0.65 | −0.31ab | 0.61 | 0.00a | 0.81 | −0.44b | −0.25 | 17.02 | 3, 508 | <.001 |
| Quality of Parenting | 0.49a | 1.13 | 0.56a | 0.99 | 0.87a | 1.34 | −0.56b | 1.05 | 47.81 | 3, 508 | <.001 |
| Parental Mood and Substance Disorder | 0.28a | 2.14 | 0.67ab | 2.13 | 1.19b | 2.57 | −0.47b | 1.64 | 15.79 | 3, 508 | <.001 |
Note. EDE-Q, Eating Disorder Examination-Questionnaire (range: 0–6*; scores indicating less favorable conditions are asterisked); BSI, Brief Symptom Inventory, GSI, Global Severity Index (T scores); SAS, Social Adjustment Scale (1–5*); RFI, Oxford Risk Factor Interview (average of standardized risk factor scores by risk factor domain; they can be interpreted as deviations from the mean, with higher scores indicating greater exposure).
Different superscripts indicate significant post hoc Tukey tests (p < .01) following significant univariate GLM analyses (p < .05).
(2) Is BED Characterized by an Underlying Affective Disorder or Anxiety Disorder?
When examining the strength of association between the membership to the BED taxon and single diagnostic indicators, large biserial correlations for OBEs and Overvaluation of Shape or Weight (rbis = .88, 1.00) and medium correlations for affective disorder and anxiety disorder (rbis = .36, = .33; all p < .001) were revealed. The strength of association between the diagnostic indicators of BED and membership of the BED taxon was significantly greater than that between the diagnostic indicators of affective and anxiety disorders and membership of the BED taxon (z tests of correlation coefficients; all p < .001).
Discussion
Comorbid psychopathology continues to complicate the assessment, diagnosis, and treatment of eating disorders, including BED. This raises the question as to whether and how shared characteristics of mental disorders should be considered in classification. An important criterion for recognizing a clinical syndrome as appropriate for inclusion in the DSM as a distinct disorder is whether it can be distinguished from other mental disorders already represented in the DSM (Blashfield, Sprock, & Fuller, 1990).
(1) Is BED an Associated Feature of Affective and Anxiety Disorders?
The current study elaborated on the boundaries between BED and other mental disorders that are frequently comorbid with BED. Previous studies examining the boundaries between BED and other eating disorders or normality provided initial support for a latent entity of BED (e.g., Bulik et al., 2000; Eddy et al., 2009; Mitchell et al., 2007; Striegel-Moore et al., 2005; Wade et al., 2006; Williamson et al., 2002), but this support was not consistent (Hay, Fairburn, & Doll, 1996). Our latent structure analysis showed that at the latent level BED was co-occurring with, yet distinct from, affective and anxiety disorders. Diagnostic co-occurrence was demonstrated at an above-chance level, suggesting that individuals with both BED and affective disorders have shared characteristics that may be maintained by the association between negative mood or anxiety, and binge eating behavior (Binford, Pederson Mussell, Peterson, Crow, & Mitchell, 2004; Hilbert & Tuschen-Caffier, 2007; Stein et al., 2007) or weight and shape concern (Hilbert, Tuschen-Caffier, & Vögele, 2002; Masheb & Grilo, 2003; Svaldi, Caffier, Blechert, & Tuschen-Caffier, 2009). Shared characteristics could stem from exposure to similar risk factors such as impairments in mental or physical health, abusive and disruptive experiences, and familial problems, as suggested by retrospective risk correlates (see also Fairburn et al., 1998). Alternatively, comorbid mental disorders could also represent a consequence of the eating disorder (Mussell, Mitchell, Weller et al., 1995). Longitudinal research is needed to examine the association of BED and co-occurring conditions over time.
Despite diagnostic co-occurrence of BED and affective and anxiety disorders, the probability for BED to occur without an affective or anxiety disorder was twice as large as to co-occur with these conditions at the latent level. Diagnostic co-occurrence within the BED taxon indicated greater general psychopathology, lower social adaptation, and greater premorbid exposure to parental mood and substance use disorder, but not greater eating disorder psychopathology. Previous research has at the manifest level consistently documented associations between psychiatric comorbidity and general psychopathology in clinical samples of BED (Grilo et al., 2009; Peterson, Miller, Crow, Thuras, & Mitchell, 2005). In contrast to the current and another clinical study’s results (Wilfley et al., 2000), these studies also found significantly greater eating disorder psychopathology in patients with BED with psychiatric comorbidity than in patients with BED without psychiatric comorbidity. Methodological differences in sampling, operationalization, and level of analysis may account for these inconsistencies. However, it is also noted that the differences in eating disorder psychopathology by psychiatric comorbidity that have been found in previous studies were mostly small.
Eating disorder psychopathology discriminated individuals in the BED taxon from individuals in the affective and anxiety disorders taxon. These results from the current study suggest that the specific eating disorder psychopathology can be captured with eating-disorder-specific diagnostic indicators, but would largely not be captured when using only indicators of affective or anxiety disorders. In addition, this study found that women in the BED taxon with or without co-occurrence differed from the complement in nearly all validators. The latent taxon of BED was composed of more than two-thirds of individuals with a manifest diagnosis of BED; thus, this diagnostic entity was mostly reproduced, although for this taxometric analysis only a subset of self-reported diagnostic indicators was available. Delineation of the boundary between BED and obesity was not the focus of the current study; the non-eating disordered control sample was not matched to the BED sample on BMI. Nevertheless, these results underscore that BED is not an associated feature of comorbid psychopathology but should be conceptualized as an eating disorder with substantial comorbid psychopathology (see Devlin et al., 2003).
(2) Is BED Characterized by an Underlying Affective Disorder or Anxiety Disorder?
The diagnostic indicators of BED were more characteristic of the latent taxon of BED than indicators of affective or anxiety disorders, suggesting that BED is not an associated feature of an underlying affective or anxiety disorder. It is noteworthy that these results refer to BED as a whole. Based on the evidence from suptyping by negative mood at the manifest level (Chen, McCloskey, & Keenan, 2009; Jansen, Havermans, Nederkoorn, & Roefs, 2008; Masheb & Grilo, 2008; Stice, Davis, Miller, & Marti, 2008) it is possible that for a subset of individuals with BED (e.g., those from the high negative affect subtype), the indicators of affective or anxiety disorders or of a specific affective or anxiety disorder are more characteristic than the indicators of BED. Future research can address these questions in latent structure analyses with adequate sampling of individuals from the high versus low negative affect subtype and of specific major affective and anxiety disorders. Although the results are overall not suggestive of an underlying affective or anxiety disorder in BED, the medium-size associations between indicators of affective and anxiety disorders and membership in the BED taxon suggest, in accordance with previous research, that general psychopathology is a characteristic of this disorder for a subset of individuals.
Methodological Considerations
Our findings need to be considered in light of strengths and limitations of the current study. We utilized well-characterized community samples of women with BED, affective and anxiety disorders, and no current psychiatric diagnosis. Although an unselected sample would have been preferable for these analyses, with a low base rate entity such as BED more than 20,000 individuals would have been required to detect a BED taxon. In this case, oversampling of BED is permissible (Ruscio & Ruscio, 2004). However, as the exclusion of eating disorders from both control groups may have increased separation between groups, replication of results in an unselected sample is warranted. The measures used had established reliability and validity. Standardized administration of diagnostic interviews was ensured through training and supervision, but information on interrater reliability was not available. For the latent structure analysis, diagnoses were based on diagnostic items from clinical interview or self-report-questionnaire that had overlap but were not fully congruent with criteria used to form the diagnostic groups. For example, the BED diagnostic indicators used in the taxometric analysis based on self-report did not include behavioral indicators of loss of control or of distress over binge eating; both criteria have been critized for lacking empirical support (Latner & Clyne, 2007). This contributed to a low number of indicators available for the current analysis, and as a consequence, MAMBAC results could only be corroborated with the taxometric method MAXSLOPE that also requires only two indicators, but is less commonly used in latent structure analyses than other procedures. We used LPA analysis to check consistency and overcome this limitation. A further limitation is that the evidence was mostly – but not unambiguously – in support of a taxonic structure of affective and anxiety disorders, which is nevertheless consistent with the literature. Taxometric analyses of major depression have provided evidence for a taxonic structure when assessment of depression was based on interview, but not when based on self-report (Ruscio, Brown, & Ruscio, 2009; Ruscio & Marcus, 2007). For anxiety disorders, there is some evidence of a taxonic structure of severe anxiety symptoms (Kotov, Schmidt, Lerew, Joiner, & Ialongo, 2005) and mixed anxiety and depression in youth (Schmidt et al., 2009), whereas evidence on agoraphobia, social phobic fears, worry, posttraumatic stress, or other fears are mostly suggestive of a dimensional structure (Broman-Fulks, Ruggiero, Green et al., 2006; Forbes, Haslam, Williams, & Creamer, 2005; Haslam, 2003; Kollman, Brown, Liverant, & Hofmann, 2006; Ruscio, Borkovec, & Ruscio, 2001; Slade & Grisham, 2009; Weeks, Norton, & Heimberg, 2009). Collapsing affective and anxiety disorders into one category is supported by structural evidence indicating that affective and anxiety disorders fall within one internalizing spectrum, although there may be depression- and anxiety-related subclasses among them (Watson, 2005). Finally, we were able to use for validation analyses clinically informative correlates such as health services utilization and social adaptation as well as data about early life experiences in order to gain insight into retrospectively gathered etiological patterns.
Implications
The results of the current study have important implications for the understanding of the nature of BED. By demonstrating distinctiveness of BED from affective and anxiety disorders at the latent level, the results contribute to the construct validity of this disorder. Future research will need to determine BED’s association with single affective or anxiety disorders and other comorbid conditions such as substance use disorder (Lilenfeld, Ringham, Kalarchian, & Marcus, 2008), personality disorders (Wonderlich et al., 2007), and obesity (Devlin, Goldfein, Petkova, Liu, & Walsh, 2007; Wonderlich et al., 2009). Our results further show that OBEs and overvaluation of shape or weight are central for the construct and classification of BED (Grilo, Hrabosky, White et al., 2008; Grilo et al., 2009; Hrabosky, Masheb, White, & Grilo, 2007; Mond, Hay, Rodgers, & Owen, 2007; Goldschmidt et al., 2010; Grilo, Masheb, & White, 2010), while characteristics of affective and anxiety disorders do not seem suited to fully capture the specific psychopathology of BED.
Clinically, similar to previous findings on subtyping by current or lifetime depressive disorders (Grilo, Masheb, & Wilson, 2001; Peterson et al., 2005), the results advocate for a thorough assessment of comorbid psychiatric disorders as an indicator of greater general psychopathology and less social adaptation, as psychiatric comorbidity predicts a less favorable long-term outcome (Fichter et al., 2008). Psychiatric comorbidity can be used as an indicator of a need for enhanced treatment (Wilson et al., 2010). Further, because the data suggest shared maintenance factors among BED and affective and anxiety disorders, maintenance models should more explicitly take these maintenance factors into account that apply to some, but not all, patients with BED (see Fairburn, Cooper, & Shafran, 2003). Such models could guide treatment design to integrate standard cognitive-behavioral interventions for BED with those for co-occurring pathology, such as self-monitoring of mood- or anxiety-related symptoms, exposure and response prevention for anxiety, cognitive interventions for negative cognitive schemata related to the affective or anxiety disorder, or emotion regulation interventions for irritable mood. Future research may continue to establish (Fairburn, Cooper, Doll et al., 2009) whether treatment approaches that address co-occurring pathology beyond eating disorder psychopathology can lead to an improved treatment outcome.
Acknowledgments
Funding sources for this study include NIH grants MH52348 (Dr. Striegel-Moore), K24 MH070446 (Dr. Wilfley), and a supplemental grant from the Office for Research on Women’s Health at NIH. Dr. Fairburn is supported by a Principal Research Fellowship from the Wellcome Trust, London (046386).
Role of the Funding Source
Study sponsors do not have any influence on study design; data collection, analysis, and interpretation; on writing of the report; or on the decision to submit the paper for publication.
Footnotes
Disclosure Statement
The authors declare not to have any actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations within three years of beginning the work submitted that could inappropriately influence the work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Anja Hilbert, Email: anja.hilbert@unifr.ch.
Denise E. Wilfley, Email: wilfleyd@psychiatry.wustl.edu.
Faith-Anne Dohm, Email: fdohm@mail.fairfield.edu.
Kathleen M. Pike, Email: kmp2@columbia.edu.
Christopher G. Fairburn, Email: credo@medsci.ox.ac.uk.
Ruth H. Striegel-Moore, Email: ruth.striegelmoore@montana.edu.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. Textrevision. [Google Scholar]
- Beauchaine TP. A brief taxometrics primer. Journal of Clinical Child and Adolescent Psychology. 2007;36:654–676. doi: 10.1080/15374410701662840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binford RB, Pederson Mussell M, Peterson CB, Crow SJ, Mitchell JE. Relation of binge eating age of onset to functional aspects of binge eating in binge eating disorder. International Journal of Eating Disorders. 2004;35:286–292. doi: 10.1002/eat.10272. [DOI] [PubMed] [Google Scholar]
- Blashfield RK, Sprock J, Fuller AK. Suggested guidelines for including or excluding categories in the DSM-IV. Comprehensive Psychiatry. 1990;31:15–19. doi: 10.1016/0010-440x(90)90049-x. [DOI] [PubMed] [Google Scholar]
- Bozdogan H. Model selection and Akaike’s Information Criterion (AIC): The general theory and its analytical extensions. Psychometrika. 1987;52:345–370. [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Kilpatrick DG, Danielson CK, Resnick HS, et al. Taxometric Investigation of PTSD: Data from two nationally representative samples. Behavior Therapy. 2006;37:364–380. doi: 10.1016/j.beth.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Kendler KS. An empirical study of the classification of eating disorders. American Journal of Psychiatry. 2000;157:886–895. doi: 10.1176/appi.ajp.157.6.886. [DOI] [PubMed] [Google Scholar]
- Chen EY, McCloskey MS, Keenan KE. Subtyping dietary restraint and negative affect in a longitudinal community sample of girls. International Journal of Eating Disorders. 2009;42:275–283. doi: 10.1002/eat.20661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. New York: Academic; 1988. [Google Scholar]
- Derogatis LR. SCL-90-R, Administration, Scoring and Procedures Manual-I for the Revised Version. Baltimore: Johns Hopkins School of Medicine; 1977. [Google Scholar]
- Devlin MJ, Goldfein JA, Dobrow I. What is this thing called BED? Current status of binge eating disorder nosology. International Journal of Eating Disorders. 2003;34(Suppl):S2–18. doi: 10.1002/eat.10201. [DOI] [PubMed] [Google Scholar]
- Devlin MJ, Goldfein JA, Petkova E, Liu L, Walsh BT. Cognitive behavioral therapy and fluoxetine for binge eating disorder: two-year follow-up. Obesity. 2007;15:1702–1709. doi: 10.1038/oby.2007.203. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Crosby RD, Keel PK, Wonderlich SA, le Grange D, Hill L, et al. Empirical identification and validation of eating disorder phenotypes in a multisite clinical sample. Journal of Nervous and Mental Disease. 2009;197:41–49. doi: 10.1097/NMD.0b013e3181927389. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment and Treatment. 12. New York: Guilford; 1993. pp. 317–360. [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Bohn K, Hawker DM, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: A two-site trial with 60-week follow-up. American Journal of Psychiatry. 2009;166:311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour Research and Therapy. 2003;41:509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Doll HA, Welch SL, Hay PJ, Davies BA, O’Connor ME. Risk factors for binge eating disorder: A community-based, case-control study. Archives of General Psychiatry. 1998;55:425–432. doi: 10.1001/archpsyc.55.5.425. [DOI] [PubMed] [Google Scholar]
- Fichter MM, Quadflieg N, Hedlund S. Long-term course of binge eating disorder and bulimia nervosa: Relevance for nosology and diagnostic criteria. International Journal of Eating Disorders. 2008;41:577–586. doi: 10.1002/eat.20539. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Non-Patient Edition (SCID-I/NP, version 2.0, 4/97 revisions) New York: Biometrics Research Department; 1997. [Google Scholar]
- Forbes D, Haslam N, Williams BJ, Creamer M. Testing the latent structure of posttraumatic stress disorder: A taxometric study of combat veterans. Journal of Traumatic Stress. 2005;18:647–656. doi: 10.1002/jts.20073. [DOI] [PubMed] [Google Scholar]
- Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: A review of measures of social functioning. American Journal of Psychiatry. 1992;149:1148–1156. doi: 10.1176/ajp.149.9.1148. [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Hilbert A, Manwaring JL, Wilfley DE, Pike KM, Fairburn CG, Striegel-Moore RH. The significance of overvaluation of shape and weight in binge eating disorder. Behaviour Research and Therapy. 2010;48:187–193. doi: 10.1016/j.brat.2009.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Hrabosky JI, White MA, Allison KC, Stunkard AJ, Masheb RM. Overvaluation of shape and weight in binge eating disorder and overweight controls: Refinement of a diagnostic construct. Journal of Abnormal Psychology. 2008;117:414–419. doi: 10.1037/0021-843X.117.2.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, White MA. Significance of overvaluation of shape/weight in binge-eating disorder: Comparative study with overweight and bulimia nervosa. Obesity. 2010;18:499–504. doi: 10.1038/oby.2009.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. Subtyping binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69:1066–1072. doi: 10.1037//0022-006x.69.6.1066. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. Rapid response to treatment for binge eating disorder. Journal of Consulting and Clinical Psychology. 2006;74:602–613. doi: 10.1037/0022-006X.74.3.602. [DOI] [PubMed] [Google Scholar]
- Grilo CM, White MA, Masheb RM. DSM-IV psychiatric disorder comorbidity and its correlates in binge eating disorder. International Journal of Eating Disorders. 2009;42:228–234. doi: 10.1002/eat.20599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grove WM. The maxslope taxometric procedure: Mathematical derivation, parameter estimation, consistency tests. Psychological Reports. 2004;95:517–550. doi: 10.2466/pr0.95.2.517-550. [DOI] [PubMed] [Google Scholar]
- Grove WM. Clinical versus statistical prediction: The contribution of Paul E. Meehl. Journal of Clinical Psychology. 2005;61:1233–1243. doi: 10.1002/jclp.20179. [DOI] [PubMed] [Google Scholar]
- Haslam N. Categorical versus dimensional models of mental disorder: The taxometric evidence. Australian and New Zealand Journal of Psychiatry. 2003;37:696–704. doi: 10.1080/j.1440-1614.2003.01258.x. [DOI] [PubMed] [Google Scholar]
- Hay PJ, Fairburn CG, Doll HA. The classification of bulimic eating disorders: A community-based cluster analysis study. Psychological Medicine. 1996;26:801–812. doi: 10.1017/s003329170003782x. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B. Maintenance of binge eating through negative mood: A naturalistic comparison of binge eating disorder and bulimia nervosa. International Journal of Eating Disorders. 2007;40:521–530. doi: 10.1002/eat.20401. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B, Ohms M. Eating Disorder Examination: Deutschsprachige Version des strukturierten Essstörungsinterviews. Diagnostica. 2004;50:98–106. [Google Scholar]
- Hilbert A, Tuschen-Caffier B, Vögele C. Effects of prolonged and repeated body image exposure in binge-eating disorder. Journal of Psychosomatic Research. 2002;52:137–144. doi: 10.1016/s0022-3999(01)00314-2. [DOI] [PubMed] [Google Scholar]
- Hrabosky JI, Masheb RM, White MA, Grilo CM. Overvaluation of shape and weight in binge eating disorder. Journal of Consulting and Clinical Psychology. 2007;75:175–180. doi: 10.1037/0022-006X.75.1.175. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs-Pilipski MJ, Wilfley DE, Crow SJ, Walsh BT, Lilenfeld LR, West DS, et al. Placebo response in binge eating disorder. International Journal of Eating Disorders. 2007;40:204–211. doi: 10.1002/eat.20287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen A, Havermans R, Nederkoorn C, Roefs A. Jolly fat or sad fat? Subtyping non-eating disordered overweight and obesity along an affect dimension. Appetite. 2008;51:635–640. doi: 10.1016/j.appet.2008.05.055. [DOI] [PubMed] [Google Scholar]
- Javaras KN, Pope HG, Lalonde JK, Roberts JL, Nillni YI, Laird NM, et al. Co-occurrence of binge eating disorder with psychiatric and medical disorders. Journal of Clinical Psychiatry. 2008;69:266–273. doi: 10.4088/jcp.v69n0213. [DOI] [PubMed] [Google Scholar]
- Kollman DM, Brown TA, Liverant GI, Hofmann SG. A taxometric investigation of the latent structure of social anxiety disorder in outpatients with anxiety and mood disorders. Depression and Anxiety. 2006;23:190–199. doi: 10.1002/da.20158. [DOI] [PubMed] [Google Scholar]
- Kotov R, Schmidt NB, Lerew DR, Joiner TE, Jr, Ialongo NS. Latent structure of anxiety: taxometric exploration. Psychological Assessment. 2005;17:369–374. doi: 10.1037/1040-3590.17.3.369. [DOI] [PubMed] [Google Scholar]
- Latner JD, Clyne C. The diagnostic validity of the criteria for binge eating disorder. International Journal of Eating Disorders. 2008;41:1–14. doi: 10.1002/eat.20465. [DOI] [PubMed] [Google Scholar]
- Lilenfeld LR, Ringham R, Kalarchian MA, Marcus MD. A family history study of binge eating disorder. Comprehensive Psychiatry. 2008;49:247–254. doi: 10.1016/j.comppsych.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. The nature of body image disturbance in patients with binge eating disorder. International Journal of Eating Disorders. 2003;33:333–341. doi: 10.1002/eat.10139. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Rapid response predicts treatment outcomes in binge eating disorder: Implications for stepped care. Journal of Consulting and Clinical Psychology. 2007;75:639–644. doi: 10.1037/0022-006X.75.4.639. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Prognostic significance of two sub-categorization methods for the treatment of binge eating disorder: negative affect and overvaluation predict, but do not moderate, specific outcomes. Behaviour Research and Therapy. 2008;46:428–437. doi: 10.1016/j.brat.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehl PE. Bootstraps taxometrics. Solving the classification problem in psychopathology. American Psychologist. 1995;50:266–275. doi: 10.1037//0003-066x.50.4.266. [DOI] [PubMed] [Google Scholar]
- Meehl PE, Yonce LJ. Taxometric analysis: I. Detecting taxonicity with two quantitative indicators using means above and below a sliding cut (MAMBAC procedure) Psychological Reports. 1994;74:1059–1274. [Google Scholar]
- Mitchell JE, Crosby RD, Wonderlich SA, Hill L, le Grange D, Powers P, et al. Latent profile analysis of a cohort of patients with eating disorders not otherwise specified. International Journal of Eating Disorders. 2007;40(Suppl):S95–98. doi: 10.1002/eat.20459. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C. Recurrent binge eating with and without the “undue influence of weight or shape on self-evaluation”: Implications for the diagnosis of binge eating disorder. Behaviour Research and Therapy. 2007;45:929–938. doi: 10.1016/j.brat.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJ. Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behaviour Research and Therapy. 2004;42:551–567. doi: 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- Mussell MP, Mitchell JE, Weller CL, Raymond NC, Crow SJ, Crosby RD. Onset of binge eating, dieting, obesity, and mood disorders among subjects seeking treatment for binge eating disorder. International Journal of Eating Disorders. 17:395–401. doi: 10.1002/1098-108x(199505)17:4<395::aid-eat2260170412>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Peterson CB, Crosby RD, Wonderlich SA, Joiner T, Crow SJ, Mitchell JE, et al. Psychometric properties of the eating disorder examination-questionnaire: factor structure and internal consistency. International Journal of Eating Disorders. 2007;40:386–389. doi: 10.1002/eat.20373. [DOI] [PubMed] [Google Scholar]
- Peterson CB, Miller KB, Crow SJ, Thuras P, Mitchell JE. Subtypes of binge eating disorder based on psychiatric history. International Journal of Eating Disorders. 2005;38:273–276. doi: 10.1002/eat.20174. [DOI] [PubMed] [Google Scholar]
- Pike KM, Hilbert A, Wilfley DE, Fairburn CG, Dohm FA, Walsh BT, et al. Toward an understanding of risk factors for anorexia nervosa: a case-control study. Psychological Medicine. 2008;38:1443–1453. doi: 10.1017/S0033291707002310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reas DL, Grilo CM, Masheb RM. Reliability of the Eating Disorder Examination-Questionnaire in patients with binge eating disorder. Behaviour Research and Therapy. 2006;44:43–51. doi: 10.1016/j.brat.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Borkovec TD, Ruscio J. A taxometric investigation of the latent structure of worry. Journal of Abnormal Psychology. 2001;110:413–422. doi: 10.1037//0021-843x.110.3.413. [DOI] [PubMed] [Google Scholar]
- Ruscio J. Assigning cases to groups using taxometric results: An empirical comparison of classification techniques. Assessment. 2009;16:55–70. doi: 10.1177/1073191108320193. [DOI] [PubMed] [Google Scholar]
- Ruscio J, Brown TA, Meron Ruscio A. A taxometric investigation of DSM-IV major depression in a large outpatient sample: Interpretable structural results depend on the mode of assessment. Assessment. 2009;16:127–144. doi: 10.1177/1073191108330065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio J, Haslam N, Ruscio AM. Introduction to the Taxometric Method: A Practical Guide. Mahwah, NJ: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- Ruscio J, Marcus DK. Detecting small taxa using simulated comparison data: A reanalysis of Beach, Amir, and Bau’s (2005) data. Psychological Assessment. 2007;19:241–246. doi: 10.1037/1040-3590.19.2.241. [DOI] [PubMed] [Google Scholar]
- Ruscio J, Ruscio AM. Clarifying boundary issues in psychopathology: The role of taxometrics in a comprehensive program of structural research. Journal of Abnormal Psychology. 2004;113:24–38. doi: 10.1037/0021-843X.113.1.24. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Kotov R, Bernstein A, Zvolensky MJ, Joiner TE, Jr, Lewinsohn PM. Mixed anxiety depression: taxometric exploration of the validity of a diagnostic category in youth. Journal of Affective Disorders. 2007;98:83–89. doi: 10.1016/j.jad.2006.06.025. [DOI] [PubMed] [Google Scholar]
- Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Slade T, Grisham JR. A taxometric investigation of agoraphobia in a clinical and a community sample. Journal of Anxiety Disorders. 2009;23:799–805. doi: 10.1016/j.janxdis.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What’s driving the binge in binge eating disorder? A prospective examination of precursors and consequences. International Journal of Eating Disorders. 2007;40:195–203. doi: 10.1002/eat.20352. [DOI] [PubMed] [Google Scholar]
- Stice E, Davis K, Miller NP, Marti CN. Fasting increases risk for onset of binge eating and bulimic pathology: A 5-year prospective study. Journal of Abnormal Psychology. 2008;117:941–946. doi: 10.1037/a0013644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm FA, Wilfley DE, Pike KM, Bray NL, Kraemer HC, et al. Toward an understanding of health services use in women with binge eating disorder. Obesity Research. 2004;12:799–806. doi: 10.1038/oby.2004.96. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Franko DL. Should binge eating disorder be included in the DSM-V? A critical review of the state of the evidence. Annual Review of Clinical Psychology. 2008;4:305–324. doi: 10.1146/annurev.clinpsy.4.022007.141149. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Franko DL, Thompson D, Barton B, Schreiber GB, Daniels SR. An empirical study of the typology of bulimia nervosa and its spectrum variants. Psychological Medicine. 2005;35:1563–1572. doi: 10.1017/S0033291705006057. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Allison KC. Binge eating disorder: disorder or marker? International Journal of Eating Disorders. 2003;34(Suppl):S107–116. doi: 10.1002/eat.10210. [DOI] [PubMed] [Google Scholar]
- Svaldi J, Caffier D, Blechert J, Tuschen-Caffier B. Body-related film clip triggers desire to binge in women with binge eating disorder. Behaviour Research and Therapy. 2009;47:790–796. doi: 10.1016/j.brat.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Uebersax JS. Probit Latent Class Analysis with Dichotomous or Ordered Category Measures: Conditional Independence/Dependence Models. Applied Psychological Measurement. 1999;23:283–297. [Google Scholar]
- Wade TD, Crosby RD, Martin NG. Use of latent profile analysis to identify eating disorder phenotypes in an adult Australian twin cohort. Archives of General Psychiatry. 2006;63:1377–1384. doi: 10.1001/archpsyc.63.12.1377. [DOI] [PubMed] [Google Scholar]
- Waller NG, Meehl PE. Multivariate Taxometric Procedures: Distinguishing Types from Continua. Thousand Oaks: Sage; 1998. [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Weeks JW, Norton PJ, Heimberg RG. Exploring the latent structure of two cognitive components of social anxiety: Taxometric analyses of fears of negative and positive evaluation. Depression and Anxiety. 2009;26:E40–48. doi: 10.1002/da.20414. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Bishop ME, Wilson GT, Agras WS. Classification of eating disorders: Toward DSM-V. International Journal of Eating Disorders. 2007;40(Suppl):S123–129. doi: 10.1002/eat.20436. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Friedman MA, Dounchis JZ, Stein RI, Welch RR, Ball SA. Comorbid psychopathology in binge eating disorder: relation to eating disorder severity at baseline and following treatment. Journal of Consulting and Clinical Psychology. 2000;68:641–649. [PubMed] [Google Scholar]
- Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. International Journal of Eating Disorders. 2003;34(Suppl):S96–106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- Williamson DA, Womble LG, Smeets MA, Netemeyer RG, Thaw JM, Kutlesic V, et al. Latent structure of eating disorder symptoms: a factor analytic and taxometric investigation. American Journal of Psychiatry. 2002;159:412–418. doi: 10.1176/appi.ajp.159.3.412. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Archives of General Psychiatry. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engel SG. The validity and clinical utility of binge eating disorder. International Journal of Eating Disorders. 2009;42:687–705. doi: 10.1002/eat.20719. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Joiner TE, Jr, Keel PK, Williamson DA, Crosby RD. Eating disorder diagnoses: Empirical approaches to classification. American Psychologist. 2007;62:167–180. doi: 10.1037/0003-066X.62.3.167. [DOI] [PubMed] [Google Scholar]