Abstract
Purpose
Low-dose theophylline has anti-inflammatory effects. The aim of this study was to evaluate the effects of adding theophylline compared with increasing the dose of inhaled corticosteroid (ICS) on symptomatic asthma.
Materials and Methods
The associated literature was acquired through deliberate searching and selected based on the established inclusion criteria for publications. The extracted data were further analyzed by a meta-analysis
Results
Four randomized, controlled, parallel studies were selected. Addition of theophylline produced a greater increase of forced expiratory volume in one second as %predicted (FEV1pred) by 2.49% [95% confidence interval (CI) 1.99-3.00; z = 9.70; p < 0.001], compared with increasing the dose of ICS. There was no difference between the two treatments in terms of peak expiratory flow (PEF).
Conclusion
Addition of theophylline to ICS has similar therapeutic effects on improving lung function as increasing the dose of ICS in the treatment of symptomatic asthma.
Keywords: Asthma, theophylline, inhaled corticosteroid, meta-analysis
INTRODUCTION
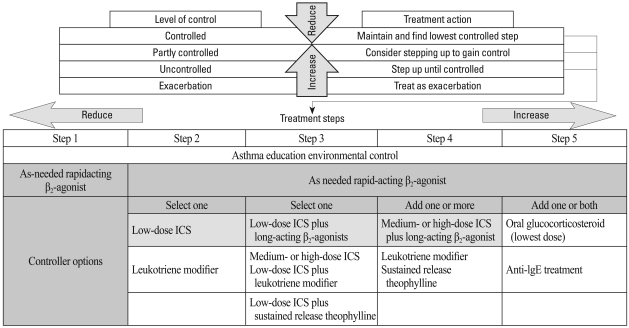
Asthma is a chronic inflammatory disorder of the airway induced by a variety of inflammatory cells. Anti-inflammatory therapy is the cornerstone of asthma therapy, and corticosteroids are the most efficacious anti-inflammatory drugs for asthma. Inhaled corticosteroid (ICS) has become a mainstay of asthma therapy. However, in many patients, asthma is not well controlled despite use of ICS. Global Initiative for Aathma (GINA) asthma guidelines1 recommend addition of long-acting β2-agonist (LABA) or increasing the dose of ICS in patients whose asthma is not adequately controlled by low dose ICS, with addition of LABA being the first choice (Fig. 1). A meta-analysis conducted by Shrewsbury, et al.2 showed that addition of salmeterol to ICS produced better lung function, better control of symptoms, less need for rescue medication and fewer exacerbations than increasing the dose of ICS. However, the safety of LABA has been questioned. Recent studies suggest that use of LABA increases the risk of serious asthma-related events and asthma mortality, despite the protective effect of ICS.3-5 However, this opinion remains controversial. Other studies have shown that LABA therapy was not associated with an increased risk of severe asthma exacerbation and asthma-related death.6,7 Addition of LABA and increasing the dose of ICS may also be expensive for patients, especially in developing countries.
Fig. 1.
GINA asthma guidelines: management approach based on control for children > 5 years of age, adolescents and adults. The best-documented treatment for controlling asthma is ICS. Low-dose ICS is recommended as the initial controller treatment at step 2, and low-dose ICS plus LABA is recommended at step 3. GINA, Global Initiative for Asthma; ICS, inhaled corticosteroid; LABA, long acting β2-agonist.
Many studies indicate that low-dose theophylline has anti-infammatory effects and it can reduce eosinophilic inflammation. As shown by two withdrawal studies, low-dose theophylline provided further improvement of asthma control in patients already treated with ICS.8,9 Several studies showed that addition of theophylline to a low or moderate dose of ICS and increasing the dose had similar therapeutic effects in terms of improving lung function and asthmatic symptoms, and reducing the need for rescue medication.10-13 The aim of this meta-analysis was to pool data from randomized, controlled, parallel trials to examine the effects of addition of theophylline to ICS compared with increasing the dose of ICS in treating symptomatic asthmatic patients.
MATERIALS AND METHODS
Search strategy and selection criteria
We performed a comprehensive search of the PubMed (1966-April 2010), EMBASE (1974-April 2010) and China National Knowledge Infrastructure (CNKI, 1994-April 2010) databases using the following keyword terms: theophylline AND asthma AND steroid or corticosteroid. Trials were not excluded on the basis of language. Reference lists were searched for additional articles.
Titles, abstracts, and citations were independently reviewed by two reviewers to assess their potential relevance for full review. From the full text, both reviewers independently assessed studies and procured the most relevant studies for inclusion based on our criteria. The following criteria were used for the literature selection for further meta-analysis: 1) The papers should be randomized, controlled, parallel trials; 2) Direct comparison between adding theophylline to ICS and increasing the current ICS dosage in adults with asthma; 3) Despite treatment with ICS, patients had asthmatic symptoms before the study or during the run-in period; 4) Data collection methods and analysis should be statistically acceptable. Accordingly, the following exclusion criteria were also used: 1) The design and definition of the trials were obviously different from those of selected papers; 2) Reviews and repeated literatures were also excluded; 3) Not offering the source of cases and controls and other essential information. We reviewed all papers in accordance with the criteria defined above for further analysis.
Data extraction and validity assessment
Data were extracted into contingency tables and entered into Ada database. Extraction was performed by two independent reviewers. When the results were presented only in graphs, these were digitized and then converted to numbers (DigitizeIt, version 1.5.7; DigitizeIt; Kŏln, Germany). In addition, we attempted to contact the investigators of the included studies to obtain further information for data extraction. Discrepancies were resolved by consensus. Primary study authors were requested to confirm data extraction and provide additional clarification or information for the review. The methodological quality of each trial was evaluated using the 5-point scale (0 = worst and 5 = best) described by Jadad, et al.14 This instrument assesses the adequacy of randomization, blinding, and the handling of withdrawals and drop outs.
Data analysis
For forced expiratory volume in one second as %predicted (FEV1pred), peak expiratory flow (PEF, recorded by patients twice daily, morning and evening, on diary cards), the measure of effect size is the difference in mean between baseline results and post-treatment results for both groups. We subtracted the results of increasing the ICS dose from the results of adding theophylline to obtain the net effect for all above measures. The net effects of each analysis were pooled using a random effect model or fixed-effect model for continuous outcomes, and a 95% confidence interval (CI) was calculated where appropriate. With pooled effects, heterogeneity was tested using the Chi-square-based Q statistic and measured additionally with the I2 test; I2 values of 25%, 50%, and 75% represent low, moderate, and high heterogeneity, respectively. Otherwise, a p value of less than 0.10 for Chi-square value using a two tailed test was considered significant. When heterogeneity was found, subgroup analyses were carried out in an attempt to explain the findings. The subgroup analyses were classified on duration of treatment. Sensitivity analysis was conducted on a statistical method of analysis (random vs fixed effects model). Meta-analysis was performed using Review Manager 4.2 (Cochrane Collaboration, Oxford, UK).
RESULTS
Literature search and meta-analysis databases
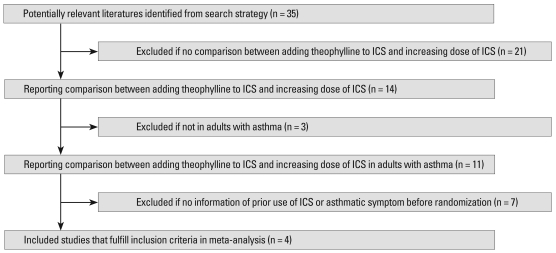
The flowchart of reviews shows the detailed selection process (Fig. 2). A total of 14 randomized controlled trials (RCT) reporting a comparison of addition of theophylline to ICS versus increasing the dose of ICS were identified, of which four studies were selected. Using the methods of Jadad, et al.14 three studies were found to have a Jadad score of 3-4, and one study reported by Wang, et al.13 had a Jadad score of 2. We established a database according to the extracted information from each paper.
Fig. 2.
The flowchart of the study selection process. ICS, inhaled corticosteroid.
Study characteristics and design
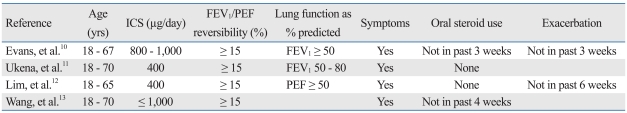
The inclusion criteria and study characteristics are given in Tables 1 and 2. All study designs were randomized, controlled and parallel groups, and three were double blind. The patients in all of the studies showed symptoms before randomized to treatment.
Table 1.
Inclusion Criteria from Individual Studies
The dose of ICS is the dose of inhaled beclometasone dipropionate (BDP) or equivalent dose of other ICS. Patients were asked to record presence (yes) or absence (no) of symptoms.
ICS, inhaled corticosteroid; FEV1, forced expiratory volume in one second; PEF, peak expiratory flow.
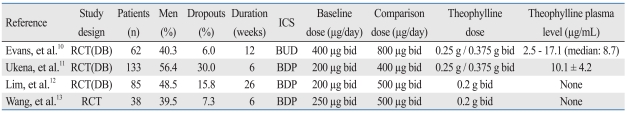
Table 2.
Characteristics and Study Design of Trials Included
ICS, inhaled corticosteroid; RCT, randomized controlled trial; DB, double blind; BDP, beclometasone dipropionate; BUD, budesonide; bid, twice daily.
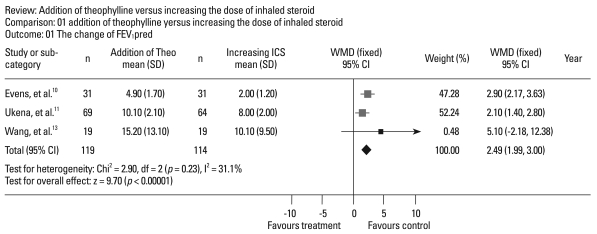
Primary outcomes
Spirometric testing: All trials examined forced expiratory volume in one second (FEV1) using spirometry, and three trials reported percentage change in FEV1pred (Fig. 3). Addition of theophylline produced a significantly greater increase by 2.49% [weighted means difference (WMD) = 2.49; 95% CI 1.99-3.00; z = 9.70; p < 0.00001] than increasing the dose of ICS in FEV1pred. There was no statistical heterogeneity between the trials (χ2 = 2.90; df = 2; p = 0.23; I2 = 31.1%).
Fig. 3.
Pooled WMD for the improvement of FEV1pred of eligible studies comparing the addition of theophylline (treatment) with increasing the dose of ICS (control). FEV1pred, forced expiratory volume in one second as %predicted; Theo, theophylline; ICS, inhaled corticosteroid; WMD, weighted mean difference; CI, confidence interval.
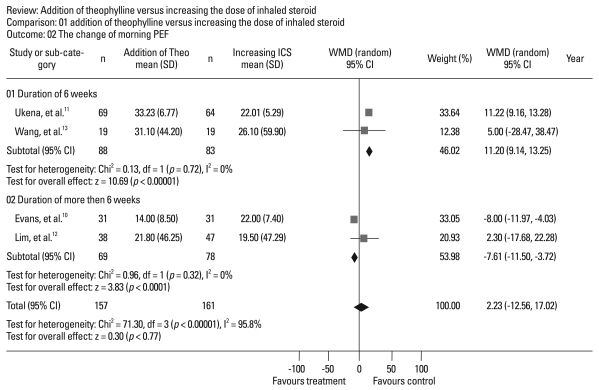
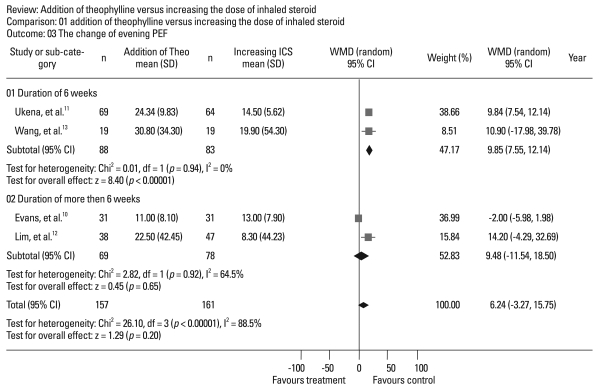
Home PEF: All trials reported mean morning and evening PEF. There was no difference between treatments in terms of morning (p = 0.77)(Fig. 4) or evening (p = 0.20) PEF (Fig. 5). Significant interstudy heterogeneity was found in morning (χ2 = 71.30; df = 3; p < 0.00001; I2 = 95.8%) and evening (χ2 = 26.10; df = 3; p < 0.00001; I2 = 88.5%) PEF. Using subgroup analysis based on treatment duration, we found that the increases in PEF with addition of theophylline were higher, by 11.20 liter/min (95% CI 9.14-13.25) in the morning and by 9.85 liter/min (95% CI 7.55-12.14) in the evening, than with increasing the dose of ICS for the strata of six-week duration. For the strata of duration longer than six weeks, evening PEF showed no difference, but the increase in morning PEF was in favor of increasing the dose of ICS by 7.61 liter/min (95% CI 3.72-11.50).
Fig. 4.
Pooled WMD for improvement of morning PEF in eligible studies comparing addition of theophylline (treatment) with increasing the dose of ICS (control). PEF, peak expiratory flow; Theo, theophylline; ICS, inhaled corticosteroid; WMD, weighted mean difference; CI, confidence interval.
Fig. 5.
Pooled WMD for the improvement of evening PEF of eligible studies comparing addition of theophylline (treatment) with increasing the dose of ICS (control). PEF, peak expiratory flow; Theo, theophylline; ICS, inhaled corticosteroid; WMD, weighted mean difference; CI, confidence interval.
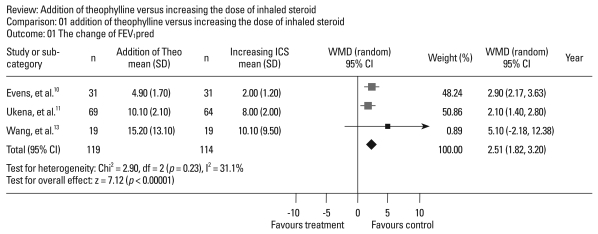
Sensitivity analysis
To evaluate the sensitivity of meta-analysis, we calculated the random effect model for FEV1pred. The random effect duramodel of FEV1pred showed a pooled WMD of 2.51 (95% CI 1.82-3.20)(Fig. 6), similar to the result (WMD = 2.49; 95% CI 1.99-3.00) obtained from the fixed-effect model.
Fig. 6.
Sensitivity analysis: Pooled WMD for improvement of FEV1pred in eligible studies comparing addition of theophylline (treatment) with increasing the dose of ICS (control) using the random effects model. FEV1pred, forced expiratory volume in one second as %predicted; Theo, theophylline; ICS, inhaled corticosteroid; WMD, weighted mean difference; CI, confidence interval.
Secondary outcomes
Rescue medication and symptom scores: All four trials revealed improvement of symptom scores and need for rescue medication in both groups, and there was no significant difference between the two treatments.
Plasma cortisol level: Two trials measured plasma cortisol level. Evans, et al.10 reported that the reduction of plasma cortisol level was observed only in the group given an increased dose of ICS after 12-week treatment. Wang, et al.13 found there was no significant reduction in plasma cortisol in both treatments.
Exacerbations: Two trials examined exacerbation rates due to asthma, and their results showed there were no statistical differences in exacerbation rates between the groups.10,12 Futhermore, Lim, et al.12 indicated that eight patients (5.2%) with an increase in ICS dose and three patients (1.9%) with addition of theophylline reported exacerbations, and that there was a trend towards fewer exacerbations with the addition of theophylline.
DISCUSSION
In past, theophylline has been applied worldwide for the treatment of asthma and is usually prescribed as bronchodilator therapy due to its inhibition of phosphodiesterase activities in airway smooth muscle. In recent years, theophylline has attracted greater attention because of its anti-inflammatory effects. In clinical trials, theophylline decreased eosinophil count and eosinophil cationic protein in sputum, blood and bronchoalveolar lavage15-17 and suppressed the late asthmatic response to nighttime antigen challenge.18 Theophylline also suppressed the expression of pro-inflammatory cytokines19,20 and restrained degranulation and release of inflammatory mediators.21-23 Recent studies show that theophylline has anti-inflammatory effects in the treatment of chronic obstructive pulmonary disease.24,25
In this study, our results demonstrated that, compared with increasing the dose of ICS, addition of theophylline led to a greater improvement of FEV1pred by 2.49%. There was no statistical heterogeneity, and the sensitivity analysis showed that the random and fixed effects models for FEV1pred had similar results. We also found no difference in PEF between the two treatments. However, statistically significant heterogeneity was found in the analysis of PEF. Subgroup analysis showed that addition of theophylline led to more improvement of PEF than increasing the dose of ICS for the strata of six-week treatment duration, but not for treatment duration of more than six weeks. Furthermore, the increase of morning PEF was in favor of increasing the dose of ICS for the strata of duration of more than 6 weeks. These results suggested that the addition of theophylline yielded a greater increase in PEF than increasing the dose of ICS, but only in short duration treatment. This result may be attributed to the bronchodilator activity of theophylline. Increasing the dose of ICS exerted an anti-inflammatory effect, resulting in similar or further improvement of PEF than the addition of theophylline in treatment of long duration. However, these results should be interpreted with caution because of the small sample of included studies and the possible presence of a publication bias.
Because most of the included studies provided insufficient information, we were not able to make a meta-analysis regarding symptom scores, rescue medication and exacerbation in the present study. However, all four studies revealed that addition of theophylline and increasing the dose of ICS had similar therapeutic effects in reducing symptom scores and need for rescue medication. Exacerbation is the primary outcome measure in asthma therapy. Two of the included trials examined exacerbation rates due to asthma, and the results showed that there were no statistical differences between the groups.10,12 Futhermore, a trial performed by Lim, et al.12 revealed a trend towards fewer exacerbations with the addition of theophylline. In addition, adrenal suppression of high-dose ICS becomes frequent. Masoli, et al.26 reported that fluticasone propionate (FP) had a minimal effect on adrenal function for routine prescription within the therapeutic dose-response range (50-500 µg/day). High-dose FP of 2,000 µg/day had similar adrenal suppression to oral prednisone of 10 mg/day.27 One study among those included reported that plasma cortisol levels reduced after 12 weeks of treatment with budesonide of 800 µg/day.10
Our study supports the use of theophylline as a steroid-sparing agent for the treatment of asthma. Adding theophylline to ICS may be a good choice for symptomatic asthma treated with low to moderate ICS. Theophylline fulfils many aspects of patient needs in treatment of asthma. It is a bronchodilator and may exert some anti-inflammatory effects.
There were several limitations in this meta-analysis. Several methodological weaknesses may limit its validity. First, of the four included studies, Wang, et al.13 was noted as open-label, whereas the other studies were double-blind. Obviously, the results from a double-blind study are more reliable than the results of an open-label study. However, our results demonstrated that the trials performed by Wang, et al.13 carried less weight than the other studies. Performance bias and measuring bias should be very low. Second, evidence of significant heterogeneity was noted in the analyses performed of PEF. However, the results were still reliable enough according to the random effects model, which accounted for heterogeneity. Third, the funnel plot was not created for evaluation of the publication bias because it is useless when the number of selected studies is too small. Moreover, it was possible that some related published or unpublished trials that may have met the inclusion criteria were missed. There was a possibility of publication bias in this meta-analysis. Fourth, we did not make a meta-analysis of adverse events. The evaluation of adverse effects was difficult to pool because there was no standardized reporting. As we know, theophylline has side effects that occur commonly, such as nausea, vomiting, and cardiac arrhythmias. However, low-dose theophylline, used in the four studies included, should cause fewer severe adverse events. Fifth, further observation should be required because of the small sample sizes and the small number of included studies. Despite these limitations, we believe that these pooled results provide valuable information.
In conclusion, adding theophylline to ICS has similar therapeutic effects in improving lung function to increasing the dose of ICS in the treatment of symptomatic asthmatic patients. Theophylline is also cheaper than either ICS or LABA. Addition of theophylline may be an appropriate treatment choice for symptomatic asthma patients currently taking ICS, especially in developing countries. More high quality, multicenter, controlled, double-blind trials are required due to our studies' limitations.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Global Initiative for Asthma (GINA) Global strategy for asthma management and prevention. 2009. [Google Scholar]
- 2.Shrewsbury S, Pyke S, Britton M. Meta-analysis of increased dose of inhaled steroid or addition of salmeterol in symptomatic asthma (MIASMA) BMJ. 2000;320:1368–1373. doi: 10.1136/bmj.320.7246.1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM SMART Study Group. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest. 2006;129:15–26. doi: 10.1378/chest.129.1.15. [DOI] [PubMed] [Google Scholar]
- 4.Weatherall M, Wijesinghe M, Perrin K, Harwood M, Beasley R. Meta-analysis of the risk of mortality with salmeterol and the effect of concomitant inhaled corticosteroid therapy. Thorax. 2010;65:39–43. doi: 10.1136/thx.2009.116608. [DOI] [PubMed] [Google Scholar]
- 5.Nelson H, Bonuccelli C, Radner F, Ottosson A, Carroll KJ, Andersson TL, et al. Safety of formoterol in patients with asthma: combined analysis of data from double-blind, randomized controlled trials. J Allergy Clin Immunol. 2010;125:390–396. doi: 10.1016/j.jaci.2009.11.036. [DOI] [PubMed] [Google Scholar]
- 6.Jaeschke R, O'Byrne PM, Mejza F, Nair P, Lesniak W, Brozek J, et al. The safety of long-acting beta-agonists among patients with asthma using inhaled corticosteroids: systematic review and meta-analysis. Am J Respir Crit Care Med. 2008;178:1009–1016. doi: 10.1164/rccm.200804-494OC. [DOI] [PubMed] [Google Scholar]
- 7.de Vries F, Setakis E, Zhang B, van Staa TP. Long-acting {beta}2-agonists in adult asthma and the pattern of risk of death and severe asthma outcomes: a study with the GPRD. Eur Respir J. 2010;36:494–502. doi: 10.1183/09031936.00124209. [DOI] [PubMed] [Google Scholar]
- 8.Minoguchi K, Kohno Y, Oda N, Wada K, Miyamoto M, Yokoe T, et al. Effect of theophylline withdrawal on airway inflammation in asthma. Clin Exp Allergy. 1998;28(Suppl 3):57–63. [PubMed] [Google Scholar]
- 9.Kidney J, Dominguez M, Taylor PM, Rose M, Chung KF, Barnes PJ. Immunomodulation by theophylline in asthma. Demonstration by withdrawal therapy. Am J Respir Crit Care Med. 1995;151:1907–1914. doi: 10.1164/ajrccm.151.6.7767539. [DOI] [PubMed] [Google Scholar]
- 10.Evans DJ, Taylor DA, Zetterstrom O, Chung KF, O'Connor BJ, Barnes PJ. A comparison of low-dose inhaled budesonide plus theophylline and high-dose inhaled budesonide for moderate asthma. N Engl J Med. 1997;337:1412–1418. doi: 10.1056/NEJM199711133372002. [DOI] [PubMed] [Google Scholar]
- 11.Ukena D, Harnest U, Sakalauskas R, Magyar P, Vetter N, Steffen H, et al. Comparison of addition of theophylline to inhaled steroid with doubling of the dose of inhaled steroid in asthma. Eur Respir J. 1997;10:2754–2760. doi: 10.1183/09031936.97.10122754. [DOI] [PubMed] [Google Scholar]
- 12.Lim S, Jatakanon A, Gordon D, Macdonald C, Chung KF, Barnes PJ. Comparison of high dose inhaled steroids, low dose inhaled steroids plus low dose theophylline, and low dose inhaled steroids alone in chronic asthma in general practice. Thorax. 2000;55:837–841. doi: 10.1136/thorax.55.10.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Y, Wang CZ, Lin KX, Qian GS, Zhuo WL, Li SP, et al. Comparison of inhaled corticosteroid combined with theophylline and double-dose inhaled corticosteroid in moderate to severe asthma. Respirology. 2005;10:189–195. doi: 10.1111/j.1440-1843.2005.00697.x. [DOI] [PubMed] [Google Scholar]
- 14.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan P, Bekir S, Jaffar Z, Page C, Jeffery P, Costello J. Anti-inflammatory effects of low-dose oral theophylline in atopic asthma. Lancet. 1994;343:1006–1008. doi: 10.1016/s0140-6736(94)90127-9. [DOI] [PubMed] [Google Scholar]
- 16.Tohda Y, Kubo H, Iwanaga T, Fukuoka M, Nakajima S. Influence of theophylline on activated lymphocytes and eosinophils in peripheral blood and sputum. J Int Med Res. 2001;29:528–536. doi: 10.1177/147323000102900610. [DOI] [PubMed] [Google Scholar]
- 17.Aizawa H, Iwanaga T, Inoue H, Takata S, Matsumoto K, Takahashi N, et al. Once-daily theophylline reduces serum eosinophil cationic protein and eosinophil levels in induced sputum of asthmatics. Int Arch Allergy Immunol. 2000;121:123–128. doi: 10.1159/000024307. [DOI] [PubMed] [Google Scholar]
- 18.Jarjour NN, Lacouture PG, Busse WW. Theophylline inhibits the late asthmatic response to nighttime antigen challenge in patients with mild atopic asthma. Ann Allergy Asthma Immunol. 1998;81:231–236. doi: 10.1016/S1081-1206(10)62817-7. [DOI] [PubMed] [Google Scholar]
- 19.Yao PL, Tsai MF, Lin YC, Wang CH, Liao WY, Chen JJ, et al. Global expression profiling of theophylline response genes in macrophages: evidence of airway anti-inflammatory regulation. Respir Res. 2005;6:89. doi: 10.1186/1465-9921-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shute JK, Tenor H, Church MK, Holgate ST. Theophylline inhibits the release of eosinophil survival cytokines--is Raf-1 the protein kinase A target? Clin Exp Allergy. 1998;28(Suppl 3):47–52. [PubMed] [Google Scholar]
- 21.Lim S, Tomita K, Caramori G, Jatakanon A, Oliver B, Keller A, et al. Low-dose theophylline reduces eosinophilic inflammation but not exhaled nitric oxide in mild asthma. Am J Respir Crit Care Med. 2001;164:273–276. doi: 10.1164/ajrccm.164.2.2006043. [DOI] [PubMed] [Google Scholar]
- 22.Horiguchi T, Tachikawa S, Kasahara J, Doi M, Shiga M, Miyazaki J, et al. Suppression of airway inflammation by theophylline in adult bronchial asthma. Respiration. 1999;66:124–127. doi: 10.1159/000029353. [DOI] [PubMed] [Google Scholar]
- 23.Kraft M, Torvik JA, Trudeau JB, Wenzel SE, Martin RJ. Theophylline: potential antiinflammatory effects in nocturnal asthma. J Allergy Clin Immunol. 1996;97:1242–1246. doi: 10.1016/s0091-6749(96)70191-4. [DOI] [PubMed] [Google Scholar]
- 24.Cosio BG, Iglesias A, Rios A, Noguera A, Sala E, Ito K, et al. Low-dose theophylline enhances the anti-inflammatory effects of steroids during exacerbations of COPD. Thorax. 2009;64:424–429. doi: 10.1136/thx.2008.103432. [DOI] [PubMed] [Google Scholar]
- 25.Iiboshi H, Ashitani J, Katoh S, Sano A, Matsumoto N, Mukae H, et al. Long-term treatment with theophylline reduces neutrophils, interleukin-8 and tumor necrosis factor-alpha in the sputum of patients with chronic obstructive pulmonary disease. Pulm Pharmacol Ther. 2007;20:46–51. doi: 10.1016/j.pupt.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Masoli M, Weatherall M, Holt S, Shirtcliffe P, Beasley R. Inhaled fluticasone propionate and adrenal effects in adult asthma: systematic review and meta-analysis. Eur Respir J. 2006;28:960–967. doi: 10.1183/09031936.06.00119305. [DOI] [PubMed] [Google Scholar]
- 27.Kellerman D, Stricker W, Howland W. Effects of inhaled fluticasone propionate (FP) on the HPA axis of patients with asthma. Eur Respir J. 1996;9(Suppl 23):162s. [Google Scholar]